-
PDF
- Split View
-
Views
-
Cite
Cite
Mingyang Wang, Xue Jiang, Jialu Geng, Shiqi Hui, Dongmei Li, Outcomes of Patients With Dysthyroid Optic Neuropathy Treated With Intravenous Corticosteroids and/or Orbital Decompression Surgery: A Systematic Review and Meta-analysis, The Journal of Clinical Endocrinology & Metabolism, Volume 108, Issue 10, October 2023, Pages 2717–2727, https://doi.org/10.1210/clinem/dgad211
Close - Share Icon Share
Abstract
The level of evidence is low for the treatment of patients with dysthyroid optic neuropathy (DON) and there is no consensus on the treatment of DON with intravenous high-dose glucocorticoids (ivGC) or direct surgical decompression.
To compare the efficacy of glucocorticoid treatment and orbital decompression (OD) in DON.
PubMed, EMBASE, and Cochrane Library were searched along with other sources.
A total of 17 studies met the inclusion criteria.
Standard methodological guidance of the Cochrane Handbook was used and data were independently extracted by multiple observers. The primary outcomes were the improvement of best corrected visual acuity (ΔBCVA). Secondary outcomes were proptosis reduction, change in diplopia, visual field defects, and intraocular pressure (IOP).
The ΔBCVA in the ivGC + OD group was improved 0.26 LogMAR more than in the ivGC group (P = .007). The ΔBCVA in the OD group was better than in the ivGC group (P = .008). Posttreatment proptosis in the ivGC + OD and OD groups were improved further by 3.54 mm and 3.00 mm, respectively, than in the ivGC group (P < .01). The mean deviation (MD) in the ivGC + OD group was improved by an additional 5.33 dB than in the ivGC group (P = .002). The IOP in the ivGC + OD group was improved further than in the ivGC group (P = .03).
Based on the results of the present meta-analysis, OD or ivGC + OD may be more effective in improving BCVA and MD and reducing proptosis compared with ivGC. Compared with ivGC alone, ivGC + OD is more effective in improving IOP than ivGC. Although this study improves the hierarchy of evidence in the treatment of DON, additional randomized controlled trials are needed to confirm this conclusion.
Dysthyroid optic neuropathy (DON) is a serious complication resulting from thyroid-associated ophthalmopathy (TAO) (1), in which crowding of the orbital apex or markedly increased adipogenesis leads to optic nerve compression with or without clinically significant exophthalmos, resulting in vision loss (2, 3). In addition to the common manifestations of TAO, other clinical manifestations of DON include deterioration in best corrected visual acuity (BCVA), anomalopia, presence of a relative afferent pupillary defect, visual field defects, visual evoked potential (VEP)-P100 anomalies, contrast sensitivity loss, optic disc changes, folded choroid, and orbital apex crowding, according to radiological evidence (4-6). Current treatment for DON mainly includes pharmacological decompression and surgical decompression. Steroids are most commonly used for pharmacological decompression (7). They can be used to reduce swelling of the orbital contents and orbital inflammation. Surgical decompression actively increases orbital volume to relieve compression of the optic nerve by removing orbital fat or bone walls to reduce the volume of ocular contents. Most current studies support initial treatment of DON with intravenous high-dose glucocorticoids (ivGC); urgent orbital decompression (OD) is necessary in the absence of response or poor response along with exacerbation of the BCVA or visual fields (8).
However, limited evidence supports the treatment of patients with DON (8). Further, there is no agreement on the use of ivGC or direct OD in DON treatment (9). This meta-analysis summarizes the currently available scientific evidence associated with the use of OD, steroids, and combinations thereof to treat DON.
Methods
Search Strategy
PubMed, EMBASE, and the Cochrane Library were searched for relevant publications from January 2002 to November 2022 using MeSH and Entry terms. The search was restricted to articles published in English, except for 1 article (10). The references of the manuscripts retrieved were also carefully searched manually. We conducted a systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (11). These studies were managed, and duplicates were deleted using Endnote X9.32.
Study Selection
Data were extracted by a single reviewer (M. Y. W.) and verified for precision by a second reviewer (X. J.). The eligibility of uncertain cases was judged by reviewing the full texts. Disagreements were resolved by discussion and finally resolved by the senior author (D. M. L.). Primary inclusion criteria for citations were (1) all randomized and nonrandomized controlled studies, as well as prospective or retrospective case series of at least 10 DON patients who were diagnosed with DON between the ages of 18 and 80 years; (2) studies that used purely surgical decompression or medical decompression with steroids or a combined approach; and (3) original articles including the primary outcome (improvement of BCVA) and 1 or more secondary outcome parameters of proptosis reduction, change in diplopia, intraocular pressure (IOP) reduction, improvement in visual field defects, and VEP-P100 after clinical follow-up of at least 1.8 months. The following studies were excluded: (1) studies that evaluated combined approaches and treatment by OD or steroids without a washout period earlier; (2) studies without relevant outcome or key statistical measures (mean ± SD); (3) studies that presented the statistics of patients with DON combined with those diagnosed with TAO who experienced vision loss; (4) studies with unstandardized surgical approaches or statistical variance; (5) studies containing OD but involving fewer than 10 patients with DON; and (6) reviews, conference abstracts, and duplicate publications. DON was defined as a combination of 2 or more of the following signs: abnormal color vision, increased latency in VEP, visual field loss compatible with optic nerve stretch or apical muscle crowding in radiological images, and presence of a relative afferent pupillary defect. Adverse outcomes were considered as complications of steroids or OD surgery.
Data Extraction and Quality Assessment
The study characteristics (eg, authors, country, study design, and year of publication), patient baseline characteristics (eg, study population, comparison group, and follow-up), and trial outcomes were extracted by independent reviewers. Instruments, such as the Cochrane risk of bias tool for trials and the Newcastle-Ottawa Scale (NOS) for observational studies, were also crosschecked by M. Y. W. and X. J. Quality was assessed using the Newcastle-Ottawa Scale and Cochrane risk of bias tool. The reliability of results was assessed by M. Y. W. and X. J. using GRADE (12). The International Prospective Registry of Systematic Reviews registration number was CRD42022367155.
Statistical Analysis
The meta-analysis was conducted using Review Manager 5.4 software. Statistical heterogeneity was estimated using the chi-square test (χ2), τ2, and I2 statistic. A fixed-effects model was used to obtain pooled estimates of mean ± SD of both the primary and secondary outcomes in studies with a control group, and the 95% CI was calculated. A random-effects model was used to generate pooled estimates of standardized mean difference of both the primary and secondary outcomes in a single-arm clinical trial. The 95% CI was calculated for each subgroup when at least 2 studies focused on the outcome. In addition, the impact of study quality on the results was evaluated based on sensitivity analysis. Egger's tests were used to assess potential publication bias.
Results
Characteristics of Eligible Studies in the Final Analysis
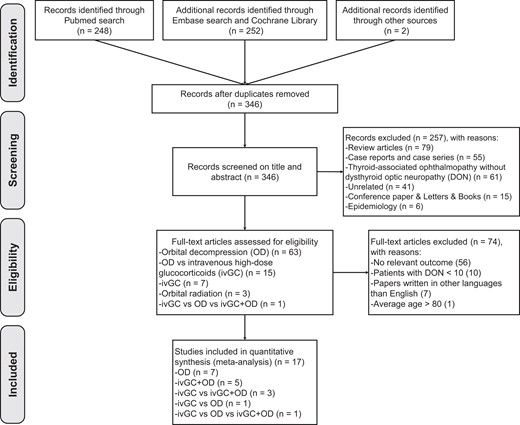
A total of 502 studies were retrieved via systematic search of bibliographic databases. After removing duplicates, 346 papers were eligible for screening of the title and abstract. A total of 89 studies were assessed for inclusion based on the full text. Finally, 17 eligible articles (2, 3, 5, 6, 9, 10, 13-23) were included in the systematic review. The flow diagram is depicted in Figure 1. The characteristics of 17 eligible articles are shown in Table 1. One randomized controlled trial, 2 prospective cohort studies, 9 retrospective studies, and 5 retrospective case series reporting OD surgery or steroid therapy were included. All included studies were written in English, except for 1 study (10) and were published between 2002 and 2022. A total of 500 patients (38.2% males and 61.8% females, 816 orbits) were recruited, which included 80 orbits treated with ivGC, 385 orbits managed via OD, and 305 orbits exposed to both ivGC and OD. Studies included in the ivGC group used similar therapy. Patients were treated with either 500 or 1000 mg pulse intravenous methylprednisolone administered daily for 3 consecutive days. The same cycle of treatment was repeated after 1 week. Steroids were tapered off either orally or intravenously in the following 4 months. The cumulative dose of methylprednisolone in all included studies was approximately 6 to 8 g but less than 10 g. For the OD group, surgical procedure included 2-wall (medial-lateral) (2, 3, 5, 6, 10, 13, 14, 16, 17, 20-23) or 3-wall (medial-lateral-inferior) (3, 9, 15, 17, 19, 22) orbital bony decompression and endoscopic trans-ethmoidal fat decompression (18). The follow-up periods ranged from 1.8 months to 5.33 years. Study characteristics are summarized in Table 1. Improvement in BCVA (ΔBCVA) was considered as the primary outcome in all included studies (Table 2). Secondary outcomes included posttreatment proptosis reduction (2, 3, 5, 6, 9, 10, 13-18, 21-23), change in diplopia (9, 10, 14, 16-18, 21-23), improvement of visual field defects (2, 5, 6, 14, 17, 19, 22, 23), IOP (2, 5, 6, 13, 14, 16, 21), and VEP-P100 (5, 14, 22) (Table 3).
Baseline characteristics of the patients with DON included in the meta-analysis
| Study . | Year . | Country . | Study design . | Patients (n) . | Sex (M/ F) . | Orbits (n) . | Mean age (y) . | Intervention . | OD (Orbits) . | Mean follow-up (mo) . |
|---|---|---|---|---|---|---|---|---|---|---|
| Wakelkamp et al (9) | 2005 | Netherlands | RCT | 15 | 2/13 | 15 | 52 | ivGC, OD | 3-walls | ivGC: 78 ± 15.5 OD: 64 ± 13 |
| Simon et al (13) | 2006 | Israel | RCS | 20 | 4/16 | 26 | 50.3 ± 15.7 | ivGC + OD | 2-walls: 6 | 17 ± 9 |
| Liao et al (14) | 2006 | Taiwan, China | RCS | 22 | 8/14 | 38 | 58.4 | ivGC + OD | 2-walls | 22.3 ± 12.8 |
| Lipski et al (15) | 2011 | Germany | RCS | 15 | 1/14 | 30 | 56.2 ± 10.88 | OD | 3-walls | 30 ± 13 |
| Wu et al (10) | 2011 | China | RCS | 29 | 10/19 | 45 | 44.8 ± 13.8 | OD | 2-walls | 17.4 ± 5.6 |
| Baril et al (16) | 2014 | Spain | RCS | 34 | 20/39 | 59 | 57.80 ± 11.89 | ivGC + OD | 2-walls | 132 |
| Korkmaz et al (17) | 2015 | Turkey | RCS | 42 | 25/17 | 68 | 53.5 | OD | 2-walls: 41 3-walls: 27 | 39.3 ± 15 |
| Lv et al (18) | 2015 | China | RCS | 43 | 12/31 | 72 | 45 | OD | fat decompression | 9 ± 3 |
| Kuebler et al (19) | 2020 | Germany | RA | 25 | 5/20 | 46 | ivGC: 62 ivGC + OD: 55 | ivGC, ivGC + OD | 3-walls | ivGC: 12 ± 12.55 ivGC + OD:10.1 ± 4.51 |
| Tagami et al (20) | 2020 | Japan | RCS | 44 | 15/29 | 70 | 53.4 ± 8.9 | OD | 2-walls | 40.9 ± 21.2 |
| Woods et al (21) | 2020 | Ireland | RA | 22 | 7/15 | 17 | 52 | ivGC + OD | 2-walls | 3 ± 0 |
| Xu et al (5) | 2020 | China | PCS | 23 | 15/8 | 46 | 58.3 ± 8.93 | ivGC, ivGC + OD | 2-walls | 3 ± 0 |
| Cheng et al (22) | 2021 | China | RCS | 37 | 9/28 | 52 | 48.27 ± 10.59 | OD | 2-walls:31 3-walls:21 | 22 ± 17 |
| Tu et al (23) | 2021 | China | RA | 42 | 24/18 | 74 | 57.30 ± 9.29 | OD | 2-walls | 6 ± 1.5 |
| Rezar-Dreindl et al (3) | 2022 | Austria | RA | 49 | 12/37 | 98 | 52 ± 14 | ivGC, OD, ivGC + OD | 2-walls:8 3-walls:30 | 49.2 ± 33.6 |
| Yun et al (2) | 2022 | Taiwan, China | RA | 11 | 9/2 | 16 | 60.1 ± 8.5 | ivGC + OD | 2-walls | 6 |
| Guo et al (6) | 2022 | China | PCS | 27 | 13/14 | 44 | 53.7 ± 8.8 | ivGC, ivGC + OD | 2-walls | ivGC: 1.8 ± 1.5 ivGC + OD: 2.6 ± 1.6 |
| Study . | Year . | Country . | Study design . | Patients (n) . | Sex (M/ F) . | Orbits (n) . | Mean age (y) . | Intervention . | OD (Orbits) . | Mean follow-up (mo) . |
|---|---|---|---|---|---|---|---|---|---|---|
| Wakelkamp et al (9) | 2005 | Netherlands | RCT | 15 | 2/13 | 15 | 52 | ivGC, OD | 3-walls | ivGC: 78 ± 15.5 OD: 64 ± 13 |
| Simon et al (13) | 2006 | Israel | RCS | 20 | 4/16 | 26 | 50.3 ± 15.7 | ivGC + OD | 2-walls: 6 | 17 ± 9 |
| Liao et al (14) | 2006 | Taiwan, China | RCS | 22 | 8/14 | 38 | 58.4 | ivGC + OD | 2-walls | 22.3 ± 12.8 |
| Lipski et al (15) | 2011 | Germany | RCS | 15 | 1/14 | 30 | 56.2 ± 10.88 | OD | 3-walls | 30 ± 13 |
| Wu et al (10) | 2011 | China | RCS | 29 | 10/19 | 45 | 44.8 ± 13.8 | OD | 2-walls | 17.4 ± 5.6 |
| Baril et al (16) | 2014 | Spain | RCS | 34 | 20/39 | 59 | 57.80 ± 11.89 | ivGC + OD | 2-walls | 132 |
| Korkmaz et al (17) | 2015 | Turkey | RCS | 42 | 25/17 | 68 | 53.5 | OD | 2-walls: 41 3-walls: 27 | 39.3 ± 15 |
| Lv et al (18) | 2015 | China | RCS | 43 | 12/31 | 72 | 45 | OD | fat decompression | 9 ± 3 |
| Kuebler et al (19) | 2020 | Germany | RA | 25 | 5/20 | 46 | ivGC: 62 ivGC + OD: 55 | ivGC, ivGC + OD | 3-walls | ivGC: 12 ± 12.55 ivGC + OD:10.1 ± 4.51 |
| Tagami et al (20) | 2020 | Japan | RCS | 44 | 15/29 | 70 | 53.4 ± 8.9 | OD | 2-walls | 40.9 ± 21.2 |
| Woods et al (21) | 2020 | Ireland | RA | 22 | 7/15 | 17 | 52 | ivGC + OD | 2-walls | 3 ± 0 |
| Xu et al (5) | 2020 | China | PCS | 23 | 15/8 | 46 | 58.3 ± 8.93 | ivGC, ivGC + OD | 2-walls | 3 ± 0 |
| Cheng et al (22) | 2021 | China | RCS | 37 | 9/28 | 52 | 48.27 ± 10.59 | OD | 2-walls:31 3-walls:21 | 22 ± 17 |
| Tu et al (23) | 2021 | China | RA | 42 | 24/18 | 74 | 57.30 ± 9.29 | OD | 2-walls | 6 ± 1.5 |
| Rezar-Dreindl et al (3) | 2022 | Austria | RA | 49 | 12/37 | 98 | 52 ± 14 | ivGC, OD, ivGC + OD | 2-walls:8 3-walls:30 | 49.2 ± 33.6 |
| Yun et al (2) | 2022 | Taiwan, China | RA | 11 | 9/2 | 16 | 60.1 ± 8.5 | ivGC + OD | 2-walls | 6 |
| Guo et al (6) | 2022 | China | PCS | 27 | 13/14 | 44 | 53.7 ± 8.8 | ivGC, ivGC + OD | 2-walls | ivGC: 1.8 ± 1.5 ivGC + OD: 2.6 ± 1.6 |
Abbreviations: DON, dysthyroid optic neuropathy; ivGC, intravenous high-dose glucocorticoids; OD, orbital decompression; PCS, prospective cohort study; RA, retrospective analysis; RCS, retrospective case studies; RCT, randomized controlled trial.
Baseline characteristics of the patients with DON included in the meta-analysis
| Study . | Year . | Country . | Study design . | Patients (n) . | Sex (M/ F) . | Orbits (n) . | Mean age (y) . | Intervention . | OD (Orbits) . | Mean follow-up (mo) . |
|---|---|---|---|---|---|---|---|---|---|---|
| Wakelkamp et al (9) | 2005 | Netherlands | RCT | 15 | 2/13 | 15 | 52 | ivGC, OD | 3-walls | ivGC: 78 ± 15.5 OD: 64 ± 13 |
| Simon et al (13) | 2006 | Israel | RCS | 20 | 4/16 | 26 | 50.3 ± 15.7 | ivGC + OD | 2-walls: 6 | 17 ± 9 |
| Liao et al (14) | 2006 | Taiwan, China | RCS | 22 | 8/14 | 38 | 58.4 | ivGC + OD | 2-walls | 22.3 ± 12.8 |
| Lipski et al (15) | 2011 | Germany | RCS | 15 | 1/14 | 30 | 56.2 ± 10.88 | OD | 3-walls | 30 ± 13 |
| Wu et al (10) | 2011 | China | RCS | 29 | 10/19 | 45 | 44.8 ± 13.8 | OD | 2-walls | 17.4 ± 5.6 |
| Baril et al (16) | 2014 | Spain | RCS | 34 | 20/39 | 59 | 57.80 ± 11.89 | ivGC + OD | 2-walls | 132 |
| Korkmaz et al (17) | 2015 | Turkey | RCS | 42 | 25/17 | 68 | 53.5 | OD | 2-walls: 41 3-walls: 27 | 39.3 ± 15 |
| Lv et al (18) | 2015 | China | RCS | 43 | 12/31 | 72 | 45 | OD | fat decompression | 9 ± 3 |
| Kuebler et al (19) | 2020 | Germany | RA | 25 | 5/20 | 46 | ivGC: 62 ivGC + OD: 55 | ivGC, ivGC + OD | 3-walls | ivGC: 12 ± 12.55 ivGC + OD:10.1 ± 4.51 |
| Tagami et al (20) | 2020 | Japan | RCS | 44 | 15/29 | 70 | 53.4 ± 8.9 | OD | 2-walls | 40.9 ± 21.2 |
| Woods et al (21) | 2020 | Ireland | RA | 22 | 7/15 | 17 | 52 | ivGC + OD | 2-walls | 3 ± 0 |
| Xu et al (5) | 2020 | China | PCS | 23 | 15/8 | 46 | 58.3 ± 8.93 | ivGC, ivGC + OD | 2-walls | 3 ± 0 |
| Cheng et al (22) | 2021 | China | RCS | 37 | 9/28 | 52 | 48.27 ± 10.59 | OD | 2-walls:31 3-walls:21 | 22 ± 17 |
| Tu et al (23) | 2021 | China | RA | 42 | 24/18 | 74 | 57.30 ± 9.29 | OD | 2-walls | 6 ± 1.5 |
| Rezar-Dreindl et al (3) | 2022 | Austria | RA | 49 | 12/37 | 98 | 52 ± 14 | ivGC, OD, ivGC + OD | 2-walls:8 3-walls:30 | 49.2 ± 33.6 |
| Yun et al (2) | 2022 | Taiwan, China | RA | 11 | 9/2 | 16 | 60.1 ± 8.5 | ivGC + OD | 2-walls | 6 |
| Guo et al (6) | 2022 | China | PCS | 27 | 13/14 | 44 | 53.7 ± 8.8 | ivGC, ivGC + OD | 2-walls | ivGC: 1.8 ± 1.5 ivGC + OD: 2.6 ± 1.6 |
| Study . | Year . | Country . | Study design . | Patients (n) . | Sex (M/ F) . | Orbits (n) . | Mean age (y) . | Intervention . | OD (Orbits) . | Mean follow-up (mo) . |
|---|---|---|---|---|---|---|---|---|---|---|
| Wakelkamp et al (9) | 2005 | Netherlands | RCT | 15 | 2/13 | 15 | 52 | ivGC, OD | 3-walls | ivGC: 78 ± 15.5 OD: 64 ± 13 |
| Simon et al (13) | 2006 | Israel | RCS | 20 | 4/16 | 26 | 50.3 ± 15.7 | ivGC + OD | 2-walls: 6 | 17 ± 9 |
| Liao et al (14) | 2006 | Taiwan, China | RCS | 22 | 8/14 | 38 | 58.4 | ivGC + OD | 2-walls | 22.3 ± 12.8 |
| Lipski et al (15) | 2011 | Germany | RCS | 15 | 1/14 | 30 | 56.2 ± 10.88 | OD | 3-walls | 30 ± 13 |
| Wu et al (10) | 2011 | China | RCS | 29 | 10/19 | 45 | 44.8 ± 13.8 | OD | 2-walls | 17.4 ± 5.6 |
| Baril et al (16) | 2014 | Spain | RCS | 34 | 20/39 | 59 | 57.80 ± 11.89 | ivGC + OD | 2-walls | 132 |
| Korkmaz et al (17) | 2015 | Turkey | RCS | 42 | 25/17 | 68 | 53.5 | OD | 2-walls: 41 3-walls: 27 | 39.3 ± 15 |
| Lv et al (18) | 2015 | China | RCS | 43 | 12/31 | 72 | 45 | OD | fat decompression | 9 ± 3 |
| Kuebler et al (19) | 2020 | Germany | RA | 25 | 5/20 | 46 | ivGC: 62 ivGC + OD: 55 | ivGC, ivGC + OD | 3-walls | ivGC: 12 ± 12.55 ivGC + OD:10.1 ± 4.51 |
| Tagami et al (20) | 2020 | Japan | RCS | 44 | 15/29 | 70 | 53.4 ± 8.9 | OD | 2-walls | 40.9 ± 21.2 |
| Woods et al (21) | 2020 | Ireland | RA | 22 | 7/15 | 17 | 52 | ivGC + OD | 2-walls | 3 ± 0 |
| Xu et al (5) | 2020 | China | PCS | 23 | 15/8 | 46 | 58.3 ± 8.93 | ivGC, ivGC + OD | 2-walls | 3 ± 0 |
| Cheng et al (22) | 2021 | China | RCS | 37 | 9/28 | 52 | 48.27 ± 10.59 | OD | 2-walls:31 3-walls:21 | 22 ± 17 |
| Tu et al (23) | 2021 | China | RA | 42 | 24/18 | 74 | 57.30 ± 9.29 | OD | 2-walls | 6 ± 1.5 |
| Rezar-Dreindl et al (3) | 2022 | Austria | RA | 49 | 12/37 | 98 | 52 ± 14 | ivGC, OD, ivGC + OD | 2-walls:8 3-walls:30 | 49.2 ± 33.6 |
| Yun et al (2) | 2022 | Taiwan, China | RA | 11 | 9/2 | 16 | 60.1 ± 8.5 | ivGC + OD | 2-walls | 6 |
| Guo et al (6) | 2022 | China | PCS | 27 | 13/14 | 44 | 53.7 ± 8.8 | ivGC, ivGC + OD | 2-walls | ivGC: 1.8 ± 1.5 ivGC + OD: 2.6 ± 1.6 |
Abbreviations: DON, dysthyroid optic neuropathy; ivGC, intravenous high-dose glucocorticoids; OD, orbital decompression; PCS, prospective cohort study; RA, retrospective analysis; RCS, retrospective case studies; RCT, randomized controlled trial.
| Study . | Year . | Orbits (n) . | Best corrected visual acuity improvement (logMAR) . | Proptosis (mm) . | Diplopia . | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Reduction . | Report . | Comment . | |||
| ivGC | ||||||||||
| Wakelkamp et al (9) | 2005 | 9 | 0.3 ± 0.20 | 0.13 ± 0.44 | 0.17 ± 0.38 | 23 ± 2 | 20 ± 4 | 3 ± 3.46 | Yes | Unchange (n = 8) Aggravate (n = 1) |
| Kuebler et al (19) | 2020 | 16 | 0.3 ± 0.28 | 0.1 ± 0.19 | 0.2 ± 0.25 | NA | NA | NA | No | NA |
| Xu et al (5) | 2020 | 23 | 0.7 ± 0.51 | 0.5 ± 0.43 | 0.2 ± 0.34 | 19.2 ± 4.18 | 17.8 ± 3.84 | 1.4 ± 1.94 | No | NA |
| Rezar-Dreindl et al (3) | 2022 | 11 | 0.05 ± 0.5 | 0.05 ± 1.0 | 0 ± 0.87 | 23 ± 4 | 22 ± 5 | 1 ± 4.58 | Yes | Aggravate (n = 1) |
| Guo et al (6) | 2022 | 10 | 0.31 ± 0.35 | 0.35 ± 0.34 | −0.04 ± 0.35 | 21.6 ± 1.8 | 21.4 ± 1.7 | 0.2 ± 1.75 | No | NA |
| OD | ||||||||||
| Wakelkamp et al (9) | 2005 | 6 | 0.44 ± 0.18 | 0.05 ± 0.18 | 0.39 ± 0.18 | 24 ± 3 | 19 ± 2 | 5 ± 2.65 | Yes | Unchange (n = 5) aggravate (n = 1) |
| Lipski et al (15) | 2011 | 30 | 0.38 ± 0.25 | 0.14 ± 0.12 | 0.24 ± 0.22 | 22.4 ± 3.3 | 16.1 ± 2.6 | 6.4 ± 3 | No | NA |
| Wu et al (10) | 2011 | 45 | 0.65 ± 0.30 | 0.24 ± 0.22 | 0.54 ± 0.18 | 20.4 ± 1.9 | 13.4 ± 1.3 | 7.07 ± 1.59 | Yes | Unchange (n = 14) aggravate (n = 1) |
| Lv et al (18) | 2015 | 72 | 0.65 ± 0.3 | 0.25 ± 0.22 | 0.55 ± 0.17 | 19.4 ± 1.4 | 13.3 ± 0.7 | 6.2 ± 1.2 | Yes | Unchange (n = 23) Aggravate (n = 2) |
| Korkmaz et l (2-wall) (17) | 2015 | 41 | 0.64 ± 0.85 | 0.11 ± 0.28 | 0.52 ± 0.68 | 24.9 ± 3.4 | 19.8 ± 3.0 | 5.1 ± 1.3 | Yes | Aggravate (n = 8) |
| Korkmaz et al (3-wall) (17) | 2015 | 27 | 0.72 ± 0.88 | 0.02 ± 0.04 | 0.71 ± 0.86 | 28.1 ± 4.5 | 20.8 ± 3.6 | 7.2 ± 1.9 | Yes | Aggravate (n = 8) |
| Tagami et al (20) | 2020 | 24 | 0.73 ± 0.77 | 0.21 ± 0.43 | 0.52 ± 0.67 | NA | NA | NA | No | NA |
| Cheng et al (2-wall) (22) | 2020 | 31 | 0.94 ± 0.62 | 0.30 ± 0.52 | 0.64 ± 0.45 | 18.84 ± 2.72 | 13.68 ± 1.12 | 5.16 ± 2.34 | No | NA |
| Cheng et al (3-wall) (22) | 2020 | 21 | 0.70 ± 0.40 | 0.09 ± 0.15 | 0.61 ± 0.43 | 22.05 ± 3.24 | 14.52 ± 1.53 | 7.53 ± 3.40 | Yes | Unchange (n = 6) Aggravate (n = 1) |
| Tu et al (23) | 2021 | 74 | 0.70 ± 0.62 | 0.22 ± 0.33 | 0.48 ± 0.54 | 19.57 ± 3.38 | 16.35 ± 3.01 | 3.22 ± 3.21 | Yes | Improve (n = 8) Aggravate (n = 18) |
| Rezar-Dreindl et al (3) | 2022 | 7 | 0.1 ± 0.7 | 0.0 ± 1.0 | 0.1 ± 0.89 | 24 ± 2 | 19 ± 2 | 5 ± 2 | Yes | NA |
| ivGC + OD | ||||||||||
| Simon et al (13) | 2006 | 26 | 0.88 ± 0.59 | 0.2 ± 0.23 | 0.68 ± 0.52 | 26.4 ± 2.5 | 21.5 ± 2.1 | 4.9 ± 2.33 | No | NA |
| Liao et al (14) | 2006 | 38 | 1.08 ± 0.24 | 0.29 ± 0.18 | 0.79 ± 0.27 | 19.6 ± 1.8 | 15.9 ± 1.3 | 3.7 ± 1.6 | Yes | Unchange (n = 9) Aggravate (n = 5) |
| Baril et al (16) | 2014 | 59 | 0.54 ± 0.82 | 0.22 ± 0.25 | 0.32 ± 0.70 | 22.90 ± 3.26 | 18.09 ± 2.96 | 5.38 ± 3.69 | Yes | Aggravate (n = 18) |
| Kuebler et al (19) | 2020 | 30 | 0.6 ± 0.94 | 0.3 ± 0.54 | 0.3 ± 0.82 | NA | NA | NA | No | NA |
| Woods et al (21) | 2020 | 17 | 0.43 ± 0.49 | 0.11 ± 0.09 | 0.32 ± 0.45 | 25.59 ± 3.05 | 22.13 ± 3.30 | 3.46 ± 3.18 | Yes | Improve (n = 5) Aggravate (n = 2) |
| Xu et al (5) | 2020 | 23 | 1.3 ± 0.63 | 0.7 ± 0.54 | 0.5 ± 0.59 | 20.0 ± 4.24 | 15.7 ± 3.00 | 4.3 ± 2.52 | Yes | Aggravate (n = 4) |
| Rezar-Dreindl et al (3) | 2022 | 31 | 0.05 ± 0.5 | 0.1 ± 0.4 | −0.05 ± 0.46 | 23 ± 3 | 20 ± 3 | 3 ± 3.00 | No | NA |
| Yun et al (2) | 2022 | 16 | 0.38 ± 0.44 | 0.26 ± 0.42 | 0.12 ± 0.43 | 22.5 ± 3.0 | 17.7 ± 2.5 | 4.8 ± 2.78 | No | NA |
| Guo et al (6) | 2022 | 34 | 0.44 ± 0.38 | 0.26 ± 0.3 | 0.18 ± 0.35 | 21.7 ± 2.3 | 17.3 ± 2.2 | 4.4 ± 2.25 | No | NA |
| Study . | Year . | Orbits (n) . | Best corrected visual acuity improvement (logMAR) . | Proptosis (mm) . | Diplopia . | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Reduction . | Report . | Comment . | |||
| ivGC | ||||||||||
| Wakelkamp et al (9) | 2005 | 9 | 0.3 ± 0.20 | 0.13 ± 0.44 | 0.17 ± 0.38 | 23 ± 2 | 20 ± 4 | 3 ± 3.46 | Yes | Unchange (n = 8) Aggravate (n = 1) |
| Kuebler et al (19) | 2020 | 16 | 0.3 ± 0.28 | 0.1 ± 0.19 | 0.2 ± 0.25 | NA | NA | NA | No | NA |
| Xu et al (5) | 2020 | 23 | 0.7 ± 0.51 | 0.5 ± 0.43 | 0.2 ± 0.34 | 19.2 ± 4.18 | 17.8 ± 3.84 | 1.4 ± 1.94 | No | NA |
| Rezar-Dreindl et al (3) | 2022 | 11 | 0.05 ± 0.5 | 0.05 ± 1.0 | 0 ± 0.87 | 23 ± 4 | 22 ± 5 | 1 ± 4.58 | Yes | Aggravate (n = 1) |
| Guo et al (6) | 2022 | 10 | 0.31 ± 0.35 | 0.35 ± 0.34 | −0.04 ± 0.35 | 21.6 ± 1.8 | 21.4 ± 1.7 | 0.2 ± 1.75 | No | NA |
| OD | ||||||||||
| Wakelkamp et al (9) | 2005 | 6 | 0.44 ± 0.18 | 0.05 ± 0.18 | 0.39 ± 0.18 | 24 ± 3 | 19 ± 2 | 5 ± 2.65 | Yes | Unchange (n = 5) aggravate (n = 1) |
| Lipski et al (15) | 2011 | 30 | 0.38 ± 0.25 | 0.14 ± 0.12 | 0.24 ± 0.22 | 22.4 ± 3.3 | 16.1 ± 2.6 | 6.4 ± 3 | No | NA |
| Wu et al (10) | 2011 | 45 | 0.65 ± 0.30 | 0.24 ± 0.22 | 0.54 ± 0.18 | 20.4 ± 1.9 | 13.4 ± 1.3 | 7.07 ± 1.59 | Yes | Unchange (n = 14) aggravate (n = 1) |
| Lv et al (18) | 2015 | 72 | 0.65 ± 0.3 | 0.25 ± 0.22 | 0.55 ± 0.17 | 19.4 ± 1.4 | 13.3 ± 0.7 | 6.2 ± 1.2 | Yes | Unchange (n = 23) Aggravate (n = 2) |
| Korkmaz et l (2-wall) (17) | 2015 | 41 | 0.64 ± 0.85 | 0.11 ± 0.28 | 0.52 ± 0.68 | 24.9 ± 3.4 | 19.8 ± 3.0 | 5.1 ± 1.3 | Yes | Aggravate (n = 8) |
| Korkmaz et al (3-wall) (17) | 2015 | 27 | 0.72 ± 0.88 | 0.02 ± 0.04 | 0.71 ± 0.86 | 28.1 ± 4.5 | 20.8 ± 3.6 | 7.2 ± 1.9 | Yes | Aggravate (n = 8) |
| Tagami et al (20) | 2020 | 24 | 0.73 ± 0.77 | 0.21 ± 0.43 | 0.52 ± 0.67 | NA | NA | NA | No | NA |
| Cheng et al (2-wall) (22) | 2020 | 31 | 0.94 ± 0.62 | 0.30 ± 0.52 | 0.64 ± 0.45 | 18.84 ± 2.72 | 13.68 ± 1.12 | 5.16 ± 2.34 | No | NA |
| Cheng et al (3-wall) (22) | 2020 | 21 | 0.70 ± 0.40 | 0.09 ± 0.15 | 0.61 ± 0.43 | 22.05 ± 3.24 | 14.52 ± 1.53 | 7.53 ± 3.40 | Yes | Unchange (n = 6) Aggravate (n = 1) |
| Tu et al (23) | 2021 | 74 | 0.70 ± 0.62 | 0.22 ± 0.33 | 0.48 ± 0.54 | 19.57 ± 3.38 | 16.35 ± 3.01 | 3.22 ± 3.21 | Yes | Improve (n = 8) Aggravate (n = 18) |
| Rezar-Dreindl et al (3) | 2022 | 7 | 0.1 ± 0.7 | 0.0 ± 1.0 | 0.1 ± 0.89 | 24 ± 2 | 19 ± 2 | 5 ± 2 | Yes | NA |
| ivGC + OD | ||||||||||
| Simon et al (13) | 2006 | 26 | 0.88 ± 0.59 | 0.2 ± 0.23 | 0.68 ± 0.52 | 26.4 ± 2.5 | 21.5 ± 2.1 | 4.9 ± 2.33 | No | NA |
| Liao et al (14) | 2006 | 38 | 1.08 ± 0.24 | 0.29 ± 0.18 | 0.79 ± 0.27 | 19.6 ± 1.8 | 15.9 ± 1.3 | 3.7 ± 1.6 | Yes | Unchange (n = 9) Aggravate (n = 5) |
| Baril et al (16) | 2014 | 59 | 0.54 ± 0.82 | 0.22 ± 0.25 | 0.32 ± 0.70 | 22.90 ± 3.26 | 18.09 ± 2.96 | 5.38 ± 3.69 | Yes | Aggravate (n = 18) |
| Kuebler et al (19) | 2020 | 30 | 0.6 ± 0.94 | 0.3 ± 0.54 | 0.3 ± 0.82 | NA | NA | NA | No | NA |
| Woods et al (21) | 2020 | 17 | 0.43 ± 0.49 | 0.11 ± 0.09 | 0.32 ± 0.45 | 25.59 ± 3.05 | 22.13 ± 3.30 | 3.46 ± 3.18 | Yes | Improve (n = 5) Aggravate (n = 2) |
| Xu et al (5) | 2020 | 23 | 1.3 ± 0.63 | 0.7 ± 0.54 | 0.5 ± 0.59 | 20.0 ± 4.24 | 15.7 ± 3.00 | 4.3 ± 2.52 | Yes | Aggravate (n = 4) |
| Rezar-Dreindl et al (3) | 2022 | 31 | 0.05 ± 0.5 | 0.1 ± 0.4 | −0.05 ± 0.46 | 23 ± 3 | 20 ± 3 | 3 ± 3.00 | No | NA |
| Yun et al (2) | 2022 | 16 | 0.38 ± 0.44 | 0.26 ± 0.42 | 0.12 ± 0.43 | 22.5 ± 3.0 | 17.7 ± 2.5 | 4.8 ± 2.78 | No | NA |
| Guo et al (6) | 2022 | 34 | 0.44 ± 0.38 | 0.26 ± 0.3 | 0.18 ± 0.35 | 21.7 ± 2.3 | 17.3 ± 2.2 | 4.4 ± 2.25 | No | NA |
Abbreviations: ivGC, intravenous high-dose glucocorticoids; NA, not available; OD, orbital decompression.
| Study . | Year . | Orbits (n) . | Best corrected visual acuity improvement (logMAR) . | Proptosis (mm) . | Diplopia . | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Reduction . | Report . | Comment . | |||
| ivGC | ||||||||||
| Wakelkamp et al (9) | 2005 | 9 | 0.3 ± 0.20 | 0.13 ± 0.44 | 0.17 ± 0.38 | 23 ± 2 | 20 ± 4 | 3 ± 3.46 | Yes | Unchange (n = 8) Aggravate (n = 1) |
| Kuebler et al (19) | 2020 | 16 | 0.3 ± 0.28 | 0.1 ± 0.19 | 0.2 ± 0.25 | NA | NA | NA | No | NA |
| Xu et al (5) | 2020 | 23 | 0.7 ± 0.51 | 0.5 ± 0.43 | 0.2 ± 0.34 | 19.2 ± 4.18 | 17.8 ± 3.84 | 1.4 ± 1.94 | No | NA |
| Rezar-Dreindl et al (3) | 2022 | 11 | 0.05 ± 0.5 | 0.05 ± 1.0 | 0 ± 0.87 | 23 ± 4 | 22 ± 5 | 1 ± 4.58 | Yes | Aggravate (n = 1) |
| Guo et al (6) | 2022 | 10 | 0.31 ± 0.35 | 0.35 ± 0.34 | −0.04 ± 0.35 | 21.6 ± 1.8 | 21.4 ± 1.7 | 0.2 ± 1.75 | No | NA |
| OD | ||||||||||
| Wakelkamp et al (9) | 2005 | 6 | 0.44 ± 0.18 | 0.05 ± 0.18 | 0.39 ± 0.18 | 24 ± 3 | 19 ± 2 | 5 ± 2.65 | Yes | Unchange (n = 5) aggravate (n = 1) |
| Lipski et al (15) | 2011 | 30 | 0.38 ± 0.25 | 0.14 ± 0.12 | 0.24 ± 0.22 | 22.4 ± 3.3 | 16.1 ± 2.6 | 6.4 ± 3 | No | NA |
| Wu et al (10) | 2011 | 45 | 0.65 ± 0.30 | 0.24 ± 0.22 | 0.54 ± 0.18 | 20.4 ± 1.9 | 13.4 ± 1.3 | 7.07 ± 1.59 | Yes | Unchange (n = 14) aggravate (n = 1) |
| Lv et al (18) | 2015 | 72 | 0.65 ± 0.3 | 0.25 ± 0.22 | 0.55 ± 0.17 | 19.4 ± 1.4 | 13.3 ± 0.7 | 6.2 ± 1.2 | Yes | Unchange (n = 23) Aggravate (n = 2) |
| Korkmaz et l (2-wall) (17) | 2015 | 41 | 0.64 ± 0.85 | 0.11 ± 0.28 | 0.52 ± 0.68 | 24.9 ± 3.4 | 19.8 ± 3.0 | 5.1 ± 1.3 | Yes | Aggravate (n = 8) |
| Korkmaz et al (3-wall) (17) | 2015 | 27 | 0.72 ± 0.88 | 0.02 ± 0.04 | 0.71 ± 0.86 | 28.1 ± 4.5 | 20.8 ± 3.6 | 7.2 ± 1.9 | Yes | Aggravate (n = 8) |
| Tagami et al (20) | 2020 | 24 | 0.73 ± 0.77 | 0.21 ± 0.43 | 0.52 ± 0.67 | NA | NA | NA | No | NA |
| Cheng et al (2-wall) (22) | 2020 | 31 | 0.94 ± 0.62 | 0.30 ± 0.52 | 0.64 ± 0.45 | 18.84 ± 2.72 | 13.68 ± 1.12 | 5.16 ± 2.34 | No | NA |
| Cheng et al (3-wall) (22) | 2020 | 21 | 0.70 ± 0.40 | 0.09 ± 0.15 | 0.61 ± 0.43 | 22.05 ± 3.24 | 14.52 ± 1.53 | 7.53 ± 3.40 | Yes | Unchange (n = 6) Aggravate (n = 1) |
| Tu et al (23) | 2021 | 74 | 0.70 ± 0.62 | 0.22 ± 0.33 | 0.48 ± 0.54 | 19.57 ± 3.38 | 16.35 ± 3.01 | 3.22 ± 3.21 | Yes | Improve (n = 8) Aggravate (n = 18) |
| Rezar-Dreindl et al (3) | 2022 | 7 | 0.1 ± 0.7 | 0.0 ± 1.0 | 0.1 ± 0.89 | 24 ± 2 | 19 ± 2 | 5 ± 2 | Yes | NA |
| ivGC + OD | ||||||||||
| Simon et al (13) | 2006 | 26 | 0.88 ± 0.59 | 0.2 ± 0.23 | 0.68 ± 0.52 | 26.4 ± 2.5 | 21.5 ± 2.1 | 4.9 ± 2.33 | No | NA |
| Liao et al (14) | 2006 | 38 | 1.08 ± 0.24 | 0.29 ± 0.18 | 0.79 ± 0.27 | 19.6 ± 1.8 | 15.9 ± 1.3 | 3.7 ± 1.6 | Yes | Unchange (n = 9) Aggravate (n = 5) |
| Baril et al (16) | 2014 | 59 | 0.54 ± 0.82 | 0.22 ± 0.25 | 0.32 ± 0.70 | 22.90 ± 3.26 | 18.09 ± 2.96 | 5.38 ± 3.69 | Yes | Aggravate (n = 18) |
| Kuebler et al (19) | 2020 | 30 | 0.6 ± 0.94 | 0.3 ± 0.54 | 0.3 ± 0.82 | NA | NA | NA | No | NA |
| Woods et al (21) | 2020 | 17 | 0.43 ± 0.49 | 0.11 ± 0.09 | 0.32 ± 0.45 | 25.59 ± 3.05 | 22.13 ± 3.30 | 3.46 ± 3.18 | Yes | Improve (n = 5) Aggravate (n = 2) |
| Xu et al (5) | 2020 | 23 | 1.3 ± 0.63 | 0.7 ± 0.54 | 0.5 ± 0.59 | 20.0 ± 4.24 | 15.7 ± 3.00 | 4.3 ± 2.52 | Yes | Aggravate (n = 4) |
| Rezar-Dreindl et al (3) | 2022 | 31 | 0.05 ± 0.5 | 0.1 ± 0.4 | −0.05 ± 0.46 | 23 ± 3 | 20 ± 3 | 3 ± 3.00 | No | NA |
| Yun et al (2) | 2022 | 16 | 0.38 ± 0.44 | 0.26 ± 0.42 | 0.12 ± 0.43 | 22.5 ± 3.0 | 17.7 ± 2.5 | 4.8 ± 2.78 | No | NA |
| Guo et al (6) | 2022 | 34 | 0.44 ± 0.38 | 0.26 ± 0.3 | 0.18 ± 0.35 | 21.7 ± 2.3 | 17.3 ± 2.2 | 4.4 ± 2.25 | No | NA |
| Study . | Year . | Orbits (n) . | Best corrected visual acuity improvement (logMAR) . | Proptosis (mm) . | Diplopia . | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Reduction . | Report . | Comment . | |||
| ivGC | ||||||||||
| Wakelkamp et al (9) | 2005 | 9 | 0.3 ± 0.20 | 0.13 ± 0.44 | 0.17 ± 0.38 | 23 ± 2 | 20 ± 4 | 3 ± 3.46 | Yes | Unchange (n = 8) Aggravate (n = 1) |
| Kuebler et al (19) | 2020 | 16 | 0.3 ± 0.28 | 0.1 ± 0.19 | 0.2 ± 0.25 | NA | NA | NA | No | NA |
| Xu et al (5) | 2020 | 23 | 0.7 ± 0.51 | 0.5 ± 0.43 | 0.2 ± 0.34 | 19.2 ± 4.18 | 17.8 ± 3.84 | 1.4 ± 1.94 | No | NA |
| Rezar-Dreindl et al (3) | 2022 | 11 | 0.05 ± 0.5 | 0.05 ± 1.0 | 0 ± 0.87 | 23 ± 4 | 22 ± 5 | 1 ± 4.58 | Yes | Aggravate (n = 1) |
| Guo et al (6) | 2022 | 10 | 0.31 ± 0.35 | 0.35 ± 0.34 | −0.04 ± 0.35 | 21.6 ± 1.8 | 21.4 ± 1.7 | 0.2 ± 1.75 | No | NA |
| OD | ||||||||||
| Wakelkamp et al (9) | 2005 | 6 | 0.44 ± 0.18 | 0.05 ± 0.18 | 0.39 ± 0.18 | 24 ± 3 | 19 ± 2 | 5 ± 2.65 | Yes | Unchange (n = 5) aggravate (n = 1) |
| Lipski et al (15) | 2011 | 30 | 0.38 ± 0.25 | 0.14 ± 0.12 | 0.24 ± 0.22 | 22.4 ± 3.3 | 16.1 ± 2.6 | 6.4 ± 3 | No | NA |
| Wu et al (10) | 2011 | 45 | 0.65 ± 0.30 | 0.24 ± 0.22 | 0.54 ± 0.18 | 20.4 ± 1.9 | 13.4 ± 1.3 | 7.07 ± 1.59 | Yes | Unchange (n = 14) aggravate (n = 1) |
| Lv et al (18) | 2015 | 72 | 0.65 ± 0.3 | 0.25 ± 0.22 | 0.55 ± 0.17 | 19.4 ± 1.4 | 13.3 ± 0.7 | 6.2 ± 1.2 | Yes | Unchange (n = 23) Aggravate (n = 2) |
| Korkmaz et l (2-wall) (17) | 2015 | 41 | 0.64 ± 0.85 | 0.11 ± 0.28 | 0.52 ± 0.68 | 24.9 ± 3.4 | 19.8 ± 3.0 | 5.1 ± 1.3 | Yes | Aggravate (n = 8) |
| Korkmaz et al (3-wall) (17) | 2015 | 27 | 0.72 ± 0.88 | 0.02 ± 0.04 | 0.71 ± 0.86 | 28.1 ± 4.5 | 20.8 ± 3.6 | 7.2 ± 1.9 | Yes | Aggravate (n = 8) |
| Tagami et al (20) | 2020 | 24 | 0.73 ± 0.77 | 0.21 ± 0.43 | 0.52 ± 0.67 | NA | NA | NA | No | NA |
| Cheng et al (2-wall) (22) | 2020 | 31 | 0.94 ± 0.62 | 0.30 ± 0.52 | 0.64 ± 0.45 | 18.84 ± 2.72 | 13.68 ± 1.12 | 5.16 ± 2.34 | No | NA |
| Cheng et al (3-wall) (22) | 2020 | 21 | 0.70 ± 0.40 | 0.09 ± 0.15 | 0.61 ± 0.43 | 22.05 ± 3.24 | 14.52 ± 1.53 | 7.53 ± 3.40 | Yes | Unchange (n = 6) Aggravate (n = 1) |
| Tu et al (23) | 2021 | 74 | 0.70 ± 0.62 | 0.22 ± 0.33 | 0.48 ± 0.54 | 19.57 ± 3.38 | 16.35 ± 3.01 | 3.22 ± 3.21 | Yes | Improve (n = 8) Aggravate (n = 18) |
| Rezar-Dreindl et al (3) | 2022 | 7 | 0.1 ± 0.7 | 0.0 ± 1.0 | 0.1 ± 0.89 | 24 ± 2 | 19 ± 2 | 5 ± 2 | Yes | NA |
| ivGC + OD | ||||||||||
| Simon et al (13) | 2006 | 26 | 0.88 ± 0.59 | 0.2 ± 0.23 | 0.68 ± 0.52 | 26.4 ± 2.5 | 21.5 ± 2.1 | 4.9 ± 2.33 | No | NA |
| Liao et al (14) | 2006 | 38 | 1.08 ± 0.24 | 0.29 ± 0.18 | 0.79 ± 0.27 | 19.6 ± 1.8 | 15.9 ± 1.3 | 3.7 ± 1.6 | Yes | Unchange (n = 9) Aggravate (n = 5) |
| Baril et al (16) | 2014 | 59 | 0.54 ± 0.82 | 0.22 ± 0.25 | 0.32 ± 0.70 | 22.90 ± 3.26 | 18.09 ± 2.96 | 5.38 ± 3.69 | Yes | Aggravate (n = 18) |
| Kuebler et al (19) | 2020 | 30 | 0.6 ± 0.94 | 0.3 ± 0.54 | 0.3 ± 0.82 | NA | NA | NA | No | NA |
| Woods et al (21) | 2020 | 17 | 0.43 ± 0.49 | 0.11 ± 0.09 | 0.32 ± 0.45 | 25.59 ± 3.05 | 22.13 ± 3.30 | 3.46 ± 3.18 | Yes | Improve (n = 5) Aggravate (n = 2) |
| Xu et al (5) | 2020 | 23 | 1.3 ± 0.63 | 0.7 ± 0.54 | 0.5 ± 0.59 | 20.0 ± 4.24 | 15.7 ± 3.00 | 4.3 ± 2.52 | Yes | Aggravate (n = 4) |
| Rezar-Dreindl et al (3) | 2022 | 31 | 0.05 ± 0.5 | 0.1 ± 0.4 | −0.05 ± 0.46 | 23 ± 3 | 20 ± 3 | 3 ± 3.00 | No | NA |
| Yun et al (2) | 2022 | 16 | 0.38 ± 0.44 | 0.26 ± 0.42 | 0.12 ± 0.43 | 22.5 ± 3.0 | 17.7 ± 2.5 | 4.8 ± 2.78 | No | NA |
| Guo et al (6) | 2022 | 34 | 0.44 ± 0.38 | 0.26 ± 0.3 | 0.18 ± 0.35 | 21.7 ± 2.3 | 17.3 ± 2.2 | 4.4 ± 2.25 | No | NA |
Abbreviations: ivGC, intravenous high-dose glucocorticoids; NA, not available; OD, orbital decompression.
| Study . | Year . | Orbits (n) . | Visual field (MD) . | Intraocular pressure (mm Hg) . | Visual evoked potential-P100 . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Improvement . | Amplitude (uV) . | Latency (ms) . | |||||||
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Improvement . | |||||||||
| ivGC | ||||||||||||||
| Kuebler et al (19) | 2020 | 16 | −10.2 ± 9.95 | −3.1 ± 4.97 | 7.1 ± 8.62 | 17.50 ± 2.25 | NA | NA | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 23 | −12.8 ± 7.45 | −9.4 ± 6.98 | 3.4 ± 5.02 | 18.5 ± 4.80 | 18.5 ± 7.24 | 0.0 ± 5.71 | 7.7 ± 4.39 | 7.3 ± 6.19 | −0.1 ± 5.51 | 137.8 ± 39.00 | 141.1 ± 36.36 | −3.3 ± 10.17 |
| Guo et al (6) | 2022 | 10 | −13.4 ± 7.5 | −15.8 ± 12.4 | −2.4 ± 10.82 | 18.7 ± 3.3 | 18 ± 4 | 0.7 ± 3.7 | NA | NA | NA | NA | NA | NA |
| OD | ||||||||||||||
| Korkmaz et al (2-wall) (7) | 2015 | 41 | −13.6 ± 6.8 | −3.6 ± 2.5 | 10.0 ± 5.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Korkmaz et al (3-wall) (7) | 2015 | 27 | −17.4 ± 8.0 | −3.2 ± 2.2 | 14.3 ± 7.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cheng et al (2-wall) (22) | 2020 | 31 | −13.73 ± 9.15 | −6.79 ± 6.95 | 6.94 ± 6.82 | NA | NA | NA | 4.22 ± 3.01 | 6.52 ± 2.17 | 2.30 ± 2.26 | 118.33 ± 16.41 | 112.17 ± 9.47 | 6.16 ± 13.04 |
| Cheng et al (3-wall) (22) | 2020 | 21 | −9.45 ± 6.85 | −3.68 ± 3.44 | 5.77 ± 6.15 | NA | NA | NA | 4.62 ± 2.26 | 9.51 ± 3.79 | 4.89 ± 4.67 | 115.89 ± 8.70 | 108.87 ± 7.91 | 7.02 ± 10.06 |
| Tu et al (23) | 2021 | 74 | −13.73 ± 9.22 | −7.23 ± 7.04 | 6.5 ± 8.35 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| ivGC + OD | ||||||||||||||
| Simon et al (13) | 2006 | 26 | NA | NA | NA | 19.6 ± 6.4 | 17.5 ± 4.3 | 2.1 ± 5.65 | NA | NA | NA | NA | NA | NA |
| Liao et al (14) | 2006 | 38 | −13.6 ± 8.6 | −4.2 ± 2.0 | 9.4 ± 8.2 | NA | NA | NA | NA | NA | NA | 134.8 ± 22.1 | 107.3 ± 4.0 | 27.5 ± 20.1 |
| Baril et al (16) | 2014 | 59 | NA | NA | NA | 19.83 ± 4.44 | 17.26 ± 3.61 | 2.56 ± 3.98 | NA | NA | NA | NA | NA | NA |
| Kuebler et al (19) | 2020 | 30 | −7.2 ± 15.27 | −2.3 ± 3.75 | 4.9 ± 13.78 | 17.00 ± 3.25 | NA | NA | NA | NA | NA | NA | NA | NA |
| Woods et al (21) | 2020 | 17 | NA | NA | NA | 20.35 ± 3.28 | 16.06 ± 3.58 | 4.29 ± 3.44 | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 23 | −19.8 ± 9.90 | −11.7 ± 8.82 | 8.1 ± 7.72 | 20.5 ± 6.21 | 16.1 ± 4.43 | 4.4 ± 6.79 | 3.8 ± 3.58 | 6.3 ± 4.05 | 2.5 ± 3.97 | 166.3 ± 38.98 | 138.2 ± 37.08 | 28.1 ± 29.93 |
| Yun et al (2) | 2022 | 16 | −8.95 ± 5.37 | −5.25 ± 4.46 | 3.7 ± 4.98 | 24.6 ± 6.0 | 16.7 ± 4.0 | 7.9 ± 5.29 | NA | NA | NA | NA | NA | NA |
| Guo et al (6) | 2022 | 34 | −11.1 ± 8.3 | −5.9 ± 6.5 | 5.2 ± 7.56 | 18.9 ± 5.1 | 17.6 ± 4.2 | 1.3 ± 4.72 | NA | NA | NA | NA | NA | NA |
| Study . | Year . | Orbits (n) . | Visual field (MD) . | Intraocular pressure (mm Hg) . | Visual evoked potential-P100 . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Improvement . | Amplitude (uV) . | Latency (ms) . | |||||||
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Improvement . | |||||||||
| ivGC | ||||||||||||||
| Kuebler et al (19) | 2020 | 16 | −10.2 ± 9.95 | −3.1 ± 4.97 | 7.1 ± 8.62 | 17.50 ± 2.25 | NA | NA | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 23 | −12.8 ± 7.45 | −9.4 ± 6.98 | 3.4 ± 5.02 | 18.5 ± 4.80 | 18.5 ± 7.24 | 0.0 ± 5.71 | 7.7 ± 4.39 | 7.3 ± 6.19 | −0.1 ± 5.51 | 137.8 ± 39.00 | 141.1 ± 36.36 | −3.3 ± 10.17 |
| Guo et al (6) | 2022 | 10 | −13.4 ± 7.5 | −15.8 ± 12.4 | −2.4 ± 10.82 | 18.7 ± 3.3 | 18 ± 4 | 0.7 ± 3.7 | NA | NA | NA | NA | NA | NA |
| OD | ||||||||||||||
| Korkmaz et al (2-wall) (7) | 2015 | 41 | −13.6 ± 6.8 | −3.6 ± 2.5 | 10.0 ± 5.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Korkmaz et al (3-wall) (7) | 2015 | 27 | −17.4 ± 8.0 | −3.2 ± 2.2 | 14.3 ± 7.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cheng et al (2-wall) (22) | 2020 | 31 | −13.73 ± 9.15 | −6.79 ± 6.95 | 6.94 ± 6.82 | NA | NA | NA | 4.22 ± 3.01 | 6.52 ± 2.17 | 2.30 ± 2.26 | 118.33 ± 16.41 | 112.17 ± 9.47 | 6.16 ± 13.04 |
| Cheng et al (3-wall) (22) | 2020 | 21 | −9.45 ± 6.85 | −3.68 ± 3.44 | 5.77 ± 6.15 | NA | NA | NA | 4.62 ± 2.26 | 9.51 ± 3.79 | 4.89 ± 4.67 | 115.89 ± 8.70 | 108.87 ± 7.91 | 7.02 ± 10.06 |
| Tu et al (23) | 2021 | 74 | −13.73 ± 9.22 | −7.23 ± 7.04 | 6.5 ± 8.35 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| ivGC + OD | ||||||||||||||
| Simon et al (13) | 2006 | 26 | NA | NA | NA | 19.6 ± 6.4 | 17.5 ± 4.3 | 2.1 ± 5.65 | NA | NA | NA | NA | NA | NA |
| Liao et al (14) | 2006 | 38 | −13.6 ± 8.6 | −4.2 ± 2.0 | 9.4 ± 8.2 | NA | NA | NA | NA | NA | NA | 134.8 ± 22.1 | 107.3 ± 4.0 | 27.5 ± 20.1 |
| Baril et al (16) | 2014 | 59 | NA | NA | NA | 19.83 ± 4.44 | 17.26 ± 3.61 | 2.56 ± 3.98 | NA | NA | NA | NA | NA | NA |
| Kuebler et al (19) | 2020 | 30 | −7.2 ± 15.27 | −2.3 ± 3.75 | 4.9 ± 13.78 | 17.00 ± 3.25 | NA | NA | NA | NA | NA | NA | NA | NA |
| Woods et al (21) | 2020 | 17 | NA | NA | NA | 20.35 ± 3.28 | 16.06 ± 3.58 | 4.29 ± 3.44 | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 23 | −19.8 ± 9.90 | −11.7 ± 8.82 | 8.1 ± 7.72 | 20.5 ± 6.21 | 16.1 ± 4.43 | 4.4 ± 6.79 | 3.8 ± 3.58 | 6.3 ± 4.05 | 2.5 ± 3.97 | 166.3 ± 38.98 | 138.2 ± 37.08 | 28.1 ± 29.93 |
| Yun et al (2) | 2022 | 16 | −8.95 ± 5.37 | −5.25 ± 4.46 | 3.7 ± 4.98 | 24.6 ± 6.0 | 16.7 ± 4.0 | 7.9 ± 5.29 | NA | NA | NA | NA | NA | NA |
| Guo et al (6) | 2022 | 34 | −11.1 ± 8.3 | −5.9 ± 6.5 | 5.2 ± 7.56 | 18.9 ± 5.1 | 17.6 ± 4.2 | 1.3 ± 4.72 | NA | NA | NA | NA | NA | NA |
Abbreviation: ivGC, intravenous high-dose glucocorticoids; MD, mean deviation; NA, not available; OD, orbital decompression.
| Study . | Year . | Orbits (n) . | Visual field (MD) . | Intraocular pressure (mm Hg) . | Visual evoked potential-P100 . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Improvement . | Amplitude (uV) . | Latency (ms) . | |||||||
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Improvement . | |||||||||
| ivGC | ||||||||||||||
| Kuebler et al (19) | 2020 | 16 | −10.2 ± 9.95 | −3.1 ± 4.97 | 7.1 ± 8.62 | 17.50 ± 2.25 | NA | NA | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 23 | −12.8 ± 7.45 | −9.4 ± 6.98 | 3.4 ± 5.02 | 18.5 ± 4.80 | 18.5 ± 7.24 | 0.0 ± 5.71 | 7.7 ± 4.39 | 7.3 ± 6.19 | −0.1 ± 5.51 | 137.8 ± 39.00 | 141.1 ± 36.36 | −3.3 ± 10.17 |
| Guo et al (6) | 2022 | 10 | −13.4 ± 7.5 | −15.8 ± 12.4 | −2.4 ± 10.82 | 18.7 ± 3.3 | 18 ± 4 | 0.7 ± 3.7 | NA | NA | NA | NA | NA | NA |
| OD | ||||||||||||||
| Korkmaz et al (2-wall) (7) | 2015 | 41 | −13.6 ± 6.8 | −3.6 ± 2.5 | 10.0 ± 5.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Korkmaz et al (3-wall) (7) | 2015 | 27 | −17.4 ± 8.0 | −3.2 ± 2.2 | 14.3 ± 7.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cheng et al (2-wall) (22) | 2020 | 31 | −13.73 ± 9.15 | −6.79 ± 6.95 | 6.94 ± 6.82 | NA | NA | NA | 4.22 ± 3.01 | 6.52 ± 2.17 | 2.30 ± 2.26 | 118.33 ± 16.41 | 112.17 ± 9.47 | 6.16 ± 13.04 |
| Cheng et al (3-wall) (22) | 2020 | 21 | −9.45 ± 6.85 | −3.68 ± 3.44 | 5.77 ± 6.15 | NA | NA | NA | 4.62 ± 2.26 | 9.51 ± 3.79 | 4.89 ± 4.67 | 115.89 ± 8.70 | 108.87 ± 7.91 | 7.02 ± 10.06 |
| Tu et al (23) | 2021 | 74 | −13.73 ± 9.22 | −7.23 ± 7.04 | 6.5 ± 8.35 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| ivGC + OD | ||||||||||||||
| Simon et al (13) | 2006 | 26 | NA | NA | NA | 19.6 ± 6.4 | 17.5 ± 4.3 | 2.1 ± 5.65 | NA | NA | NA | NA | NA | NA |
| Liao et al (14) | 2006 | 38 | −13.6 ± 8.6 | −4.2 ± 2.0 | 9.4 ± 8.2 | NA | NA | NA | NA | NA | NA | 134.8 ± 22.1 | 107.3 ± 4.0 | 27.5 ± 20.1 |
| Baril et al (16) | 2014 | 59 | NA | NA | NA | 19.83 ± 4.44 | 17.26 ± 3.61 | 2.56 ± 3.98 | NA | NA | NA | NA | NA | NA |
| Kuebler et al (19) | 2020 | 30 | −7.2 ± 15.27 | −2.3 ± 3.75 | 4.9 ± 13.78 | 17.00 ± 3.25 | NA | NA | NA | NA | NA | NA | NA | NA |
| Woods et al (21) | 2020 | 17 | NA | NA | NA | 20.35 ± 3.28 | 16.06 ± 3.58 | 4.29 ± 3.44 | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 23 | −19.8 ± 9.90 | −11.7 ± 8.82 | 8.1 ± 7.72 | 20.5 ± 6.21 | 16.1 ± 4.43 | 4.4 ± 6.79 | 3.8 ± 3.58 | 6.3 ± 4.05 | 2.5 ± 3.97 | 166.3 ± 38.98 | 138.2 ± 37.08 | 28.1 ± 29.93 |
| Yun et al (2) | 2022 | 16 | −8.95 ± 5.37 | −5.25 ± 4.46 | 3.7 ± 4.98 | 24.6 ± 6.0 | 16.7 ± 4.0 | 7.9 ± 5.29 | NA | NA | NA | NA | NA | NA |
| Guo et al (6) | 2022 | 34 | −11.1 ± 8.3 | −5.9 ± 6.5 | 5.2 ± 7.56 | 18.9 ± 5.1 | 17.6 ± 4.2 | 1.3 ± 4.72 | NA | NA | NA | NA | NA | NA |
| Study . | Year . | Orbits (n) . | Visual field (MD) . | Intraocular pressure (mm Hg) . | Visual evoked potential-P100 . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Improvement . | Amplitude (uV) . | Latency (ms) . | |||||||
| Pretreatment . | Posttreatment . | Improvement . | Pretreatment . | Posttreatment . | Improvement . | |||||||||
| ivGC | ||||||||||||||
| Kuebler et al (19) | 2020 | 16 | −10.2 ± 9.95 | −3.1 ± 4.97 | 7.1 ± 8.62 | 17.50 ± 2.25 | NA | NA | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 23 | −12.8 ± 7.45 | −9.4 ± 6.98 | 3.4 ± 5.02 | 18.5 ± 4.80 | 18.5 ± 7.24 | 0.0 ± 5.71 | 7.7 ± 4.39 | 7.3 ± 6.19 | −0.1 ± 5.51 | 137.8 ± 39.00 | 141.1 ± 36.36 | −3.3 ± 10.17 |
| Guo et al (6) | 2022 | 10 | −13.4 ± 7.5 | −15.8 ± 12.4 | −2.4 ± 10.82 | 18.7 ± 3.3 | 18 ± 4 | 0.7 ± 3.7 | NA | NA | NA | NA | NA | NA |
| OD | ||||||||||||||
| Korkmaz et al (2-wall) (7) | 2015 | 41 | −13.6 ± 6.8 | −3.6 ± 2.5 | 10.0 ± 5.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Korkmaz et al (3-wall) (7) | 2015 | 27 | −17.4 ± 8.0 | −3.2 ± 2.2 | 14.3 ± 7.5 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cheng et al (2-wall) (22) | 2020 | 31 | −13.73 ± 9.15 | −6.79 ± 6.95 | 6.94 ± 6.82 | NA | NA | NA | 4.22 ± 3.01 | 6.52 ± 2.17 | 2.30 ± 2.26 | 118.33 ± 16.41 | 112.17 ± 9.47 | 6.16 ± 13.04 |
| Cheng et al (3-wall) (22) | 2020 | 21 | −9.45 ± 6.85 | −3.68 ± 3.44 | 5.77 ± 6.15 | NA | NA | NA | 4.62 ± 2.26 | 9.51 ± 3.79 | 4.89 ± 4.67 | 115.89 ± 8.70 | 108.87 ± 7.91 | 7.02 ± 10.06 |
| Tu et al (23) | 2021 | 74 | −13.73 ± 9.22 | −7.23 ± 7.04 | 6.5 ± 8.35 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| ivGC + OD | ||||||||||||||
| Simon et al (13) | 2006 | 26 | NA | NA | NA | 19.6 ± 6.4 | 17.5 ± 4.3 | 2.1 ± 5.65 | NA | NA | NA | NA | NA | NA |
| Liao et al (14) | 2006 | 38 | −13.6 ± 8.6 | −4.2 ± 2.0 | 9.4 ± 8.2 | NA | NA | NA | NA | NA | NA | 134.8 ± 22.1 | 107.3 ± 4.0 | 27.5 ± 20.1 |
| Baril et al (16) | 2014 | 59 | NA | NA | NA | 19.83 ± 4.44 | 17.26 ± 3.61 | 2.56 ± 3.98 | NA | NA | NA | NA | NA | NA |
| Kuebler et al (19) | 2020 | 30 | −7.2 ± 15.27 | −2.3 ± 3.75 | 4.9 ± 13.78 | 17.00 ± 3.25 | NA | NA | NA | NA | NA | NA | NA | NA |
| Woods et al (21) | 2020 | 17 | NA | NA | NA | 20.35 ± 3.28 | 16.06 ± 3.58 | 4.29 ± 3.44 | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 23 | −19.8 ± 9.90 | −11.7 ± 8.82 | 8.1 ± 7.72 | 20.5 ± 6.21 | 16.1 ± 4.43 | 4.4 ± 6.79 | 3.8 ± 3.58 | 6.3 ± 4.05 | 2.5 ± 3.97 | 166.3 ± 38.98 | 138.2 ± 37.08 | 28.1 ± 29.93 |
| Yun et al (2) | 2022 | 16 | −8.95 ± 5.37 | −5.25 ± 4.46 | 3.7 ± 4.98 | 24.6 ± 6.0 | 16.7 ± 4.0 | 7.9 ± 5.29 | NA | NA | NA | NA | NA | NA |
| Guo et al (6) | 2022 | 34 | −11.1 ± 8.3 | −5.9 ± 6.5 | 5.2 ± 7.56 | 18.9 ± 5.1 | 17.6 ± 4.2 | 1.3 ± 4.72 | NA | NA | NA | NA | NA | NA |
Abbreviation: ivGC, intravenous high-dose glucocorticoids; MD, mean deviation; NA, not available; OD, orbital decompression.
Heterogeneity Test Results and Analysis
Studies with short- and long-term follow-up were analyzed separately.
Short-term follow-up (≤ 6 months) (2, 5, 6, 21, 23): The ΔBCVA in the ivGC + OD group was improved by 0.26 (95% CI, 0.07–0.44, P = .007) LogMAR compared with the ivGC group (Z = 2.71, I2 = 0) (Fig. 2). Proptosis in the ivGC + OD group was improved by 3.54 mm (95% CI, 2.61–4.47, P < .00001) compared with the ivGC group (Z = 7.48, I2 = 47%) (Fig. 3). The mean deviation (MD) in the ivGC + OD group was improved by 5.33 dB (95% CI, 1.99–8.66, P = .002) than in the ivGC group (Z = 3.13, I2 = 0%) (Fig. 3). Results of subgroup analysis showed no statistically significant difference between the ivGC + OD and OD groups in terms of MD (Z = 4.69, P = .37), I2 = 0% [Supplementary Fig. S1 (24)]. The IOP in the ivGC + OD group was improved better than in the ivGC group (Z = 2.70, P = .03, I2 = 79.7%) (Fig. 4).
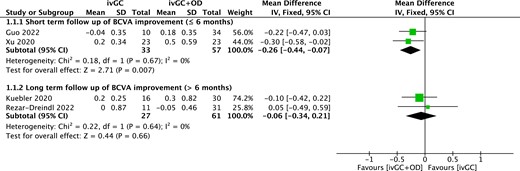
Forest plot of BCVA improvement (logMAR) compared ivGC with ivGC + OD. Abbreviations: BCVA, best corrected visual acuity; ivGC, intravenous high-dose glucocorticoids; OD, orbital decompression.
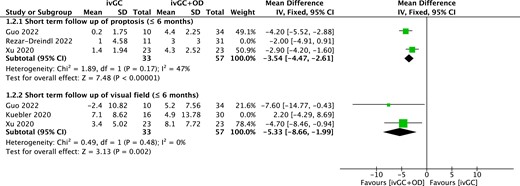
Forest plot of secondary outcomes compared ivGC with ivGC + OD. Abbreviations: ivGC, intravenous high-dose glucocorticoids; OD, orbital decompression.
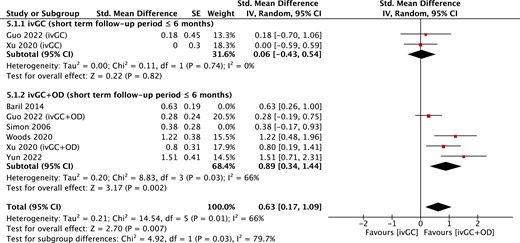
Forest plot of IOP (mmHg) compared between ivGC with ivGC + OD. Abbreviations: IOP, intraocular pressure; ivGC, intravenous high-dose glucocorticoids; OD, orbital decompression.
Long-term follow-up (> 6 months) (3, 9, 10, 13-18, 19, 20, 22): In terms of the ΔBCVA, no statistically significant difference was found between the ivGC and the ivGC + OD groups (Z = 0.44, P = .66), I2 = 0 (Fig. 2). No statistically significant difference was found between the 3-wall and the 2-wall OD groups [Z = 0.31, P = .76), I2 = 0 (Fig. 5)]. Subgroup analysis showed that the ΔBCVA in the OD group was better than in the ivGC group [P = .008, Z = 7.66, I2 = 85.6%) (Supplementary Fig. S2 (24)]. No statistically significant difference was found between the ivGC + OD group and OD group (Z = 5.78, P = .93), I2 = 0 [Supplementary Fig. S3 (24)].
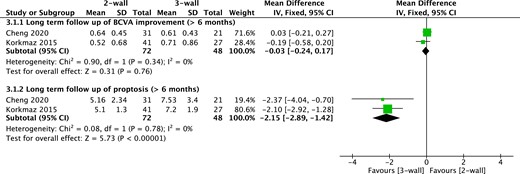
Forest plot of primary and secondary outcomes compared 2-wall vs 3-wall.
Posttreatment proptosis in the OD group was improved by 3.00 mm (95% CI, 0.82–5.19, P = .007) more than in the ivGC group (Z = 2.69, I2 = 0%) (Fig. 6); proptosis in the 3-wall OD group was improved 2.15 mm (95% CI, 1.42–2.89, P < .00001) more than in the 2-wall OD group (Z = 5.73, I2 = 0) (Fig. 5). Subgroup analysis showed no statistically significant difference between the ivGC + OD group and OD group (Z = 7.48, P = .05), I2 = 73.7% (Supplementary Fig. S4 (24)).
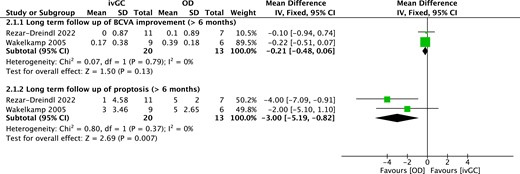
Forest plot of primary and secondary outcomes compared ivGC with OD. Abbreviations: ivGC, intravenous high-dose glucocorticoids; OD, orbital decompression.
Nine studies (5, 9, 14, 16-18, 21-23) reported posttreatment complications (Table 4). The most common complication in the ivGC group was Cushing's syndrome (n = 11). Other complications of ivGC included newly developed diplopia (n = 4), hyperglycemia (n = 6), and cardiovascular symptoms (n = 1). The most common complication in the OD group was newly developed diplopia (n = 40). Other complications of OD included epistaxis (n = 10), infraorbital nerve hypoesthesia (n = 4), sinusitis (n = 2), decrease in extraocular muscle motility (n = 1), and central retinal artery occlusion (n = 1). The most common complication in the ivGC + OD group was newly developed diplopia (n = 25). Other complications of ivGC + OD included palpebral expansion (n = 17), sinusitis (n = 2), and cerebrospinal fluid leakage (n = 2).
| Study . | Year . | Newly developed diplopia . | Cushing . | Sinusitis . | Hyperglycaemia . | Cardio-vascular symptoms . | Infraorbital nerve hypoesthesia . | Decrease in extraocular muscle motility . | Epistaxis . | CRAO . | Cerebrospinal fluid leak . | Palpebral expansion . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ivGC | ||||||||||||
| Wakelkamp et al (9) | 2005 | NA | 9 | NA | 6 | 1 | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 4 | 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| OD | ||||||||||||
| Wakelkamp et al (9) | 2005 | NA | NA | NA | NA | NA | 4 | 1 | NA | NA | NA | NA |
| Lv et al (18) | 2015 | 5 | NA | NA | NA | NA | NA | NA | 10 | NA | NA | NA |
| Korkmaz et al (17) | 2015 | 16 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cheng et al (22) | 2020 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Tu et al (23) | 2021 | 18 | NA | 2 | NA | NA | NA | NA | NA | 1 | NA | NA |
| ivGC + OD | ||||||||||||
| Liao et al (14) | 2006 | 5 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Baril et al (16) | 2014 | 18 | NA | 2 | NA | NA | NA | NA | NA | NA | 2 | 17 |
| Woods et al (21) | 2020 | 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Study . | Year . | Newly developed diplopia . | Cushing . | Sinusitis . | Hyperglycaemia . | Cardio-vascular symptoms . | Infraorbital nerve hypoesthesia . | Decrease in extraocular muscle motility . | Epistaxis . | CRAO . | Cerebrospinal fluid leak . | Palpebral expansion . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ivGC | ||||||||||||
| Wakelkamp et al (9) | 2005 | NA | 9 | NA | 6 | 1 | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 4 | 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| OD | ||||||||||||
| Wakelkamp et al (9) | 2005 | NA | NA | NA | NA | NA | 4 | 1 | NA | NA | NA | NA |
| Lv et al (18) | 2015 | 5 | NA | NA | NA | NA | NA | NA | 10 | NA | NA | NA |
| Korkmaz et al (17) | 2015 | 16 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cheng et al (22) | 2020 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Tu et al (23) | 2021 | 18 | NA | 2 | NA | NA | NA | NA | NA | 1 | NA | NA |
| ivGC + OD | ||||||||||||
| Liao et al (14) | 2006 | 5 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Baril et al (16) | 2014 | 18 | NA | 2 | NA | NA | NA | NA | NA | NA | 2 | 17 |
| Woods et al (21) | 2020 | 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
Abbreviations: CRAO, central retinal artery occlusion; ivGC, intravenous high-dose glucocorticoids; NA, not available; OD, orbital decompression.
| Study . | Year . | Newly developed diplopia . | Cushing . | Sinusitis . | Hyperglycaemia . | Cardio-vascular symptoms . | Infraorbital nerve hypoesthesia . | Decrease in extraocular muscle motility . | Epistaxis . | CRAO . | Cerebrospinal fluid leak . | Palpebral expansion . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ivGC | ||||||||||||
| Wakelkamp et al (9) | 2005 | NA | 9 | NA | 6 | 1 | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 4 | 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| OD | ||||||||||||
| Wakelkamp et al (9) | 2005 | NA | NA | NA | NA | NA | 4 | 1 | NA | NA | NA | NA |
| Lv et al (18) | 2015 | 5 | NA | NA | NA | NA | NA | NA | 10 | NA | NA | NA |
| Korkmaz et al (17) | 2015 | 16 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cheng et al (22) | 2020 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Tu et al (23) | 2021 | 18 | NA | 2 | NA | NA | NA | NA | NA | 1 | NA | NA |
| ivGC + OD | ||||||||||||
| Liao et al (14) | 2006 | 5 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Baril et al (16) | 2014 | 18 | NA | 2 | NA | NA | NA | NA | NA | NA | 2 | 17 |
| Woods et al (21) | 2020 | 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Study . | Year . | Newly developed diplopia . | Cushing . | Sinusitis . | Hyperglycaemia . | Cardio-vascular symptoms . | Infraorbital nerve hypoesthesia . | Decrease in extraocular muscle motility . | Epistaxis . | CRAO . | Cerebrospinal fluid leak . | Palpebral expansion . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ivGC | ||||||||||||
| Wakelkamp et al (9) | 2005 | NA | 9 | NA | 6 | 1 | NA | NA | NA | NA | NA | NA |
| Xu et al (5) | 2020 | 4 | 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| OD | ||||||||||||
| Wakelkamp et al (9) | 2005 | NA | NA | NA | NA | NA | 4 | 1 | NA | NA | NA | NA |
| Lv et al (18) | 2015 | 5 | NA | NA | NA | NA | NA | NA | 10 | NA | NA | NA |
| Korkmaz et al (17) | 2015 | 16 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cheng et al (22) | 2020 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Tu et al (23) | 2021 | 18 | NA | 2 | NA | NA | NA | NA | NA | 1 | NA | NA |
| ivGC + OD | ||||||||||||
| Liao et al (14) | 2006 | 5 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Baril et al (16) | 2014 | 18 | NA | 2 | NA | NA | NA | NA | NA | NA | 2 | 17 |
| Woods et al (21) | 2020 | 2 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
Abbreviations: CRAO, central retinal artery occlusion; ivGC, intravenous high-dose glucocorticoids; NA, not available; OD, orbital decompression.
Sensitivity Analysis and Publication Bias
We evaluated the effects of each of these studies via sensitivity analysis. All effects were in accordance with our main results. Egger's test suggested absence of publication bias in this study (Supplementary Figs. S5–S8).
Discussion
We divided the included studies into the following three groups: ivGC group, OD group, and ivGC combined with OD group. The most common clinical features before treatment were decline in BCVA, proptosis, and visual field defects. This meta-analysis revealed that OD or ivGC + OD may be more effective than ivGC in improving BCVA and visual field defects and reducing proptosis.
Improvement in posttreatment BCVA was reported in all studies except for Rezar-Dreindl (3). The ΔBCVA in the ivGC + OD group (short-term follow-up) and OD group (long-term follow-up) were both improved more than in the ivGC group, indicating that OD or ivGC + OD has greater efficacy in improving BCVA among patients with DON. Studies indicated that many factors played a more important role than inflammation in the pathogenesis of DON, such as venous stasis, orbital congestion, and anatomic factors, suggesting that steroids alone may not be effective in permanently treating DON (25, 26). Meanwhile, improvement of visual function after OD in patients with DON has been widely demonstrated (14, 27). Therefore, OD is indicated in some patients with DON initially for effective long-term improvement in BCVA.
Reduction of proptosis is another important measure of treatment efficacy. Previous studies have reported that ivGC was not better than placebo or nonsurgical treatment in relieving exophthalmos (28). However, studies reported that OD is effective in correcting exposure keratopathy (29). In this meta-analysis, proptosis in the ivGC + OD group (short-term follow-up) and OD group (long-term follow-up) was improved by more than 3.54 mm and 3.00 mm compared with the ivGC group, respectively. Although the safety and efficacy of 2-wall and 3-wall OD have been established in DON treatment (17), our study showed that the 3-wall OD group showed an improvement of 2.15 mm more than in the 2-wall OD group (long-term follow-up), which indicates that 3-wall decompression was apparently more appropriate for DON. Since the enlargement of extraocular muscles in patients with DON showed an extra volume effect that negatively affected the degree of retropulsion after OD surgery, the 3-wall OD may be more effective in cases of severe proptosis, which resulted in higher eyeball retropulsion and better cosmesis.
Visual function tests including perimetry and VEP are also important in the diagnosis of DON (30). Several studies have shown the beneficial effects of OD in improving the MD of patients with DON (14, 27, 31). Two studies (14, 17) have shown that the MD value can be significantly increased by OD, with an average increase of 9.4 to 10.0 dB. In this meta-analysis, the MD in the ivGC + OD group improved by an extra 5.33 dB than in the ivGC group (short-term follow-up). Meanwhile, higher mean IOP and 24 hours IOP fluctuation might be risk factors for DON (32). The fluctuation in 24 hours mean ocular perfusion pressure may induce ischemia of the optic nerve head, which was significantly associated with the MD of the visual field and was the most important risk factor for visual field defects in patients with TAO (32). Our meta-analysis revealed that the IOP in the ivGC + OD group was better than in the ivGC group (short-term follow-up). This illustrates that OD can improve visual field by decreasing intraorbital pressure and reduced the risk factors of DON by decreasing intraocular pressure. VEP is an objective visual electrophysiological analysis that facilitates the detection of early optic neuropathy. The reduction of VEP amplitude suggests that a torsional effect or mechanical compression of optic nerve (33) may lead to axonal degeneration, and abnormal optic nerve conduction is reflected by prolonged latency. The latency of VEP-P100 can be improved by OD (22); however, studies were insufficient for further analysis.
Cushing's syndrome was the most common complication of steroid therapy. Other common syndromes included newly developed diplopia, hyperglycemia, and cardiovascular symptoms. A study shows that potentially serious side effects can be avoided by excluding patients with severe systemic diseases from taking steroids (26). The incidence of side effects of glucocorticoids is related to the cumulative dose or the existence of complications (34, 35). Therefore, it is very important to control the cumulative dose and monitor blood glucose and cardiovascular function during the treatment in an effort to reduce posttreatment complications associated with steroid therapy. In the ivGC + OD and OD groups, the most common complication was newly developed diplopia. A few studies have reported sinusitis, infraorbital nerve hypoesthesia, epistaxis, central retinal artery occlusion, cerebrospinal fluid leakage, palpebral expansion, and decrease in extraocular muscle motility. Wen (36) reported that 20.0% of patients were relieved of double vision after ivGC therapy, which indicates that steroid therapy was more effective in improving pretreatment diplopia, while OD therapy increased the risk of posttreatment diplopia.
The meta-analysis has certain limitations. First, the retrospective analysis and case series had no control group, which may have reduced the reliability of subgroup analysis and increased the risk of bias. Second, the subgroup analysis was performed on the basis of aggregate data, which masked the diversity at the individual level and interaction between factors. Third, the baseline of each clinical feature was not completely identical in each group, which may have led to bias when comparing the efficacy in the 2 groups. Fourth, the comprehensive search was based on a limited number of publications in several bibliographic databases, which might have resulted in missing potential eligible studies.
In conclusion, this meta-analysis revealed that OD or ivGC + OD was more effective in improving postoperative vision (BCVA and MD) and relieving exophthalmos than ivGC alone. Although this study improves the hierarchy of evidence in the treatment of DON, additional randomized controlled trials are needed to confirm this conclusion.
Funding
This study was supported by the National Natural Science Foundation of China (No. 82071005).
Disclosures
The authors have nothing to disclose.
Data Availability
All data analyzed during this study are included in this published article.



