-
PDF
- Split View
-
Views
-
Cite
Cite
Soumia Brakta, Daria Lizneva, Kateryna Mykhalchenko, Adonis Imam, Walidah Walker, Michael P Diamond, Ricardo Azziz, Perspectives on Polycystic Ovary Syndrome: Is Polycystic Ovary Syndrome Research Underfunded?, The Journal of Clinical Endocrinology & Metabolism, Volume 102, Issue 12, 1 December 2017, Pages 4421–4427, https://doi.org/10.1210/jc.2017-01415
Close - Share Icon Share
Abstract
Polycystic ovary syndrome (PCOS) is a common endocrine-metabolic abnormality with a worldwide prevalence of 4% to 21%, depending on diagnostic criteria. The National Institutes of Health (NIH) is the largest single funding agency in the world; it invests nearly $30.0 billion annually in biomedical research.
Using the NIH Research Portfolio Online Reporting tool, we searched for all grants awarded by the NIH for PCOS and three other disorders with similar degrees of morbidity and similar or lower mortality and prevalence [rheumatoid arthritis (RA), tuberculosis (TB), and systemic lupus erythematosus (SLE)].
We compared funding by the NIH for PCOS, RA, TB, and SLE research for the years 2006 to 2015, inclusive.
PCOS, compared with RA, TB, and SLE, was relatively less funded (total mean 10-year funding was $215.12 million vs $454.39 million, $773.77 million, and $609.52 million, respectively). Funding for PCOS was largely provided by one NIH Institute/Center (ICs) vs at least two ICs for SLE and RA; more individual Research Project Grants were awarded for RA, SLE, and TB than for PCOS, whereas PCOS funding was more likely to be through General Clinical Research Centers Program or Specialized Centers Program awards. Our data suggest that PCOS research may be underfunded considering its prevalence, economic burden, metabolic morbidity, and negative impact on quality of life. Greater education of NIH leaders, including those at the National Heart, Lung, and Blood Institute and National Institutes of Diabetes and Digestive and Kidney Diseases; other federal and state agency leads; elected leaders; and the general public by professional societies, the scientific community, and patient advocates regarding this disorder is needed.
The polycystic ovary syndrome (PCOS) is a heterogeneous complex genetic disorder and the most common endocrine abnormality of reproductive-aged women, with a worldwide prevalence of 4% to 21%, depending on diagnostic criteria (1, 2). The cause remains unknown despite the syndrome's relatively high prevalence. In addition to hyperandrogenism and menstrual and ovulatory dysfunction, most patients also have metabolic dysfunction, resulting in an increased risk for type 2 diabetes mellitus, dyslipidemia, hypertension, and cerebrovascular disease, and possibly cardiovascular morbidity (3). Furthermore, women with PCOS are at increased risk for obstetrical complications, including gestational diabetes, pregnancy-induced hypertension, and preeclampsia (4). The estimated total annual burden, calculated for the United States and in reproductive years alone, and not considering the cost of obstetrical complications or the cost of metabolic morbidities in postmenopause, has been estimated to be $4.36 billion in 2004 figures (5).
The US National Institutes of Health (NIH) invests nearly $30.0 billion annually in medical research, providing competitive grants to >300,000 researchers, and is the largest single sponsor of biomedical research worldwide (6, 7). Consequently, to assess the relative extent of funding for research in PCOS, we assessed the degree of NIH funding for PCOS and three other disorders with similar degrees of morbidity and negative impact on quality of life (QOL), and similar or lower mortality and prevalence [rheumatoid arthritis (RA), tuberculosis (TB), and systemic lupus erythematosus (SLE)] (Supplemental Table 1) (8–17).
To estimate the NIH funding for PCOS in last 10 years, we used the NIH Research Portfolio Online Reporting tool (NIH RePorter) to extract information regarding all grants awarded by the NIH for PCOS, RA, TB, and SLE research between 2006 and 2015 (Supplemental Table 2). For each set of grants, titles and abstracts were reviewed separately by two investigators and categorized as relevant or irrelevant to the disease in review in accordance with the inclusion and exclusion criteria (Supplemental Table 3). We included grants that contained the reviewed disease in the title; studied human or animal models of the reviewed disease; studied pathogenesis and treatment of the reviewed disease; or supported education, meetings, and training grants of the reviewed disease.
Is PCOS Research Underfunded?
The mean (± standard deviation) yearly funding during the 10-year study period for PCOS, RA, TB, and SLE was $215.12 million vs $454.39 million, $609.52 million, and $773.77 million, respectively, a significant difference (P ≤ 0.001) (Fig. 1). All three comparator disorders received between 2- and 3.5-fold greater funding than did PCOS during the period of study. During the study period, funding for PCOS research tended to decline (P = 0.066), as did funding for RA and SLE (although these trends did not reach significance), whereas funding for TB increased 2.4-fold (P < 0.0001) (Fig. 2). In general, our data indicate that research in PCOS during the study period (2006 to 2015) was relatively less funded when compared with research for RA, TB, and SLE, despite the syndrome's significantly higher disease prevalence (∼10% vs 1%, <1%, and <0.01%, respectively).
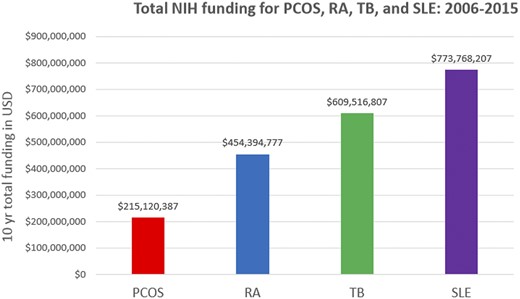
Total NIH funding for PCOS, RA, TB, and SLE: 2006 to 2015. USD, US dollars.

NIH funding per year for PCOS, RA, TB, and SLE: 2006 to 2015. USD, US dollars.
Why Is PCOS Research Funded Less?
Why does PCOS research receive less funding? The answer to this query will be critical to formulate policies and strategies that will ensure significant and definitive progress in understanding the causes, heritability, prevention, and treatment of this pervasive and morbid disorder.
Diseases of women, in general, tend to be underfunded, although more recently there has been substantial progress to address this deficiency, at least in the United States, in the past 2 decades (18). However, underfunding for PCOS may also be the result of limited interest in the disorder by the various Institutes/Centers (ICs) of the NIH. For example, we noted that 68.4% of NIH funding for PCOS research was provided by one institute of the NIH, the National Institutes of Child Health and Development (NICHD), whereas SLE and RA (but not TB), research was largely funded by at least two separate NIH ICs each (Fig. 3). The general lack of funding for PCOS research by ICs such as the National Heart, Lung, and Blood Institute (NHLBI) or National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) is surprising considering the extensive data noting the pathophysiologic relationship of the disorder with metabolic and vascular dysfunction (3, 19).
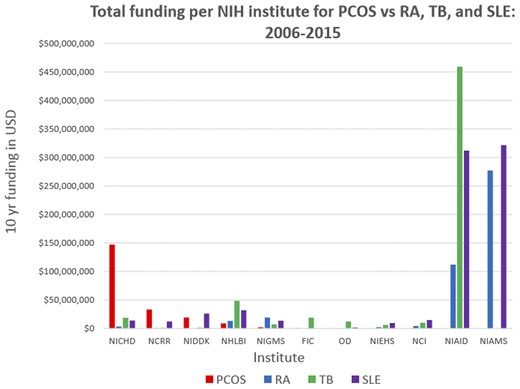
Total funding per NIH institute for PCOS, RA, TB, and SLE: 2006 to 2015. FIC, Fogarty International Center; NCCR, National Center for Research Resources; NCI, National Cancer Institute; NIAMS, National Institute of Arthritis and Musculoskeletal and Skin Diseases; NIEHS, National Institute of Environmental Health Sciences; NIGMS, National Institute of General Medical Sciences; OD, Office of the Director; USD, US dollars.
The disadvantage of PCOS research being primarily funded by the NICHD is likely further amplified by the fact that this IC is one of the lowest-funded within the NIH. For example, in 2015 the budgets of the eight ICs funded to a greater degree than the NICHD totaled almost 65% of the entire NIH budget [in order of the largest budget: National Cancer Institute, National Institute of Allergy and Infectious Diseases (NIAID), NHLBI, National Institute of General Medical Sciences, NIDDK, National Institute of Neurologic Disorders and Stroke, and National Institute of Mental Health] (7). In contrast, the NICHD received only 6.53% of the total 2015 NIH budget. TB, RA, and SLE all were significantly funded by the NIAID, the second best-funded institute of the NIH, which receives almost four times the budget of the NICHD. In addition, SLE and RA are also funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, a smaller institute.
The disadvantage of having the NICHD primarily fund most of the research in PCOS may also stem from discordance between the mission of that institute and the pathophysiology of the disorder. The NICHD’s stated mission is to “ensure that every person is born healthy and wanted, that women suffer no harmful effects from reproductive processes, and that all children have the chance to achieve their full potential for healthy and productive lives, free from disease or disability, and to ensure the health, productivity, independence, and well-being of all people through optimal rehabilitation.” Thus, research funded by this Institute will be more focused on the reproductive consequences of a disorder. However, as noted PCOS is also a metabolic disorder, with substantial and well-documented metabolic origins and metabolic and cardiovascular morbidity (3, 19), which are not areas of interest to the NICHD. In fact, those areas of research fall, at a minimum, within the scope of the missions of the NHLBI and the NIDDK, which fund very little of PCOS research.
It is also possible that the specific granting mechanism used to fund PCOS research may play a role in the relative underfunding of PCOS research. For example, considerably more Research Project Grants (R01s) were awarded for RA, SLE, and TB than for PCOS, whereas PCOS funding was more likely to be through General Clinical Research Centers Program (M01) or Specialized Center Program (P50) awards (Fig. 4). In fact, PCOS researchers receive more of their support from P50 or M01 grants combined than from R01 grants. Notably, funding for individual projects from these sources (P50, M01) provide smaller grants than do individual R01 grants.
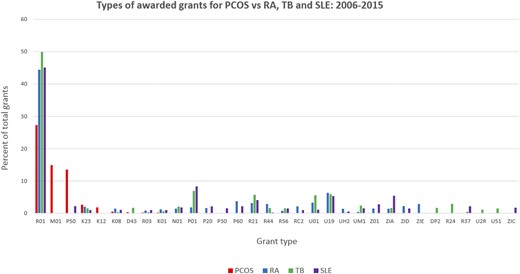
Types of awarded grants for PCOS, RA, TB, and SLE: 2006 to 2015.
Why PCOS research funded by the NIH is more often funded through M01 and P50 grants is not readily evident. Research in PCOS should not be more likely to benefit from group or consortia science than would research for RA or SLE, and certainly should be less so than that of TB. Hence, perhaps this anomaly reflects internal NICHD policy, whereby funds are preferably allocated to consortia and multicenter efforts rather than individual research grants. Assessing the total number of P50 grants per IC awarded between 2006 and 2015, we observed that the NICHD ranked 10th among NIH ICs (data not shown). However, the NICHD was only one of three ICs (along with the National Institute on Alcohol Abuse and Alcoholism and the NIAID) to increase the number of P50 grants awarded during the study period, doing so the most of any of the three (the number of P50 awards increased by 8, 2, and 6 from 2006 to 2015, respectively). Consequently, is it possible that an emphasis on P50 grant awards results from deliberate strategy by the NICHD during the study period to foster greater intercenter collaboration and team science among its investigators.
Finally, we must acknowledge that our analysis has a few limitations. First, our decision to contrast PCOS funding to that of SLE, RA, and TB does not represent an exhaustive comparison, although these disorders do have similar morbidity and impact on QOL and similar or even lower mortality and prevalence. We also recognize that we assessed funding by only one entity, the NIH, although the NIH remains the largest single provider of biomedical research grants worldwide.
Second, the lesser funding for PCOS research may result from a smaller pool of applications or applications of lesser quality. To attempt to determine whether there were differences in the funding rates of PCOS research grants versus that of other disorders, we requested data from the NIH eRA Information for Management, Planning, Analysis, and Coordination (IMPAC) II database. Although these data are solely for use of NIH staff and obtaining access would require a targeted ‘Freedom of Information Act (FOIA)’ request to the NIH, NIH staff did provide unofficial aggregated and de-identified figures regarding all funded and non-funded unsolicited competing R01 applications to the various NIH ICs for PCOS, TB, RA, and SLE, for 2006 through 2015 inclusive. In order to control for variations in IC funding rates for female reproductive disorders, they also provided funding rates for endometriosis and uterine leiomyomas (ULMs). Of note, the data did not include data on other type of grant applications, including program projects.
The results are telling. In the time period studied, there were a significantly greater number of applications for TB, SLE and RA (1460, 742 and 985, respectively) than for PCOS, endometriosis, and ULMs (126, 118, and 68). The overall funding rates was lowest for PCOS vs. endometriosis, ULM, SLE, RA, and TB (12.7% vs. 16.9%, 17.6%, 19.9%, 16.2%, and 17.5%, respectively), although the differences did not reach significance. However, careful examination of funding rates by IC revealed that for PCOS, endometriosis and ULMs, funding principally arose from one ‘principal’ IC (i.e. NICHD), and that the funding rates for these three disorders were very similar (16.5%, 16.2% and 16.4%, respectively) for this IC. Alternatively, SLE, RA and TB received significant funding (≥20 funded grants) from at least two ‘principal’ ICs (i.e. NIAID and NIAMS for SLE and RA, and NIAID, NIGMS, and NHLBI for TB), with aggregate funding rates for each of these disorders within these ICs of 20%, 15.9%, and 17.7%, respectively.
Funding rates for ICs outside of these ‘principal’ funding ICs was lowest for PCOS versus endometriosis, ULM, SLE, RA, and TB (6.8% vs. 26.7%, 40.0%, 21.5%, and 24.6%, respectively). Of note, funding rates for ‘non-principal’ ICs were higher than for ‘principal’ ICs for all disorders except PCOS, where it was lower than the funding rate afforded by the NICHD. The effect of the lower funding rate for PCOS by ‘non-principal’ ICs was magnified by the fact that PCOS also had the highest proportion of applications submitted to ‘non-principal’ ICs compared to all others disorders studied (37.3% vs. 9.5-20.7%, respectively). Finally, and most concerning, was the change in the number of submitted applications over the period studied, which decreased 42% for PCOS between 2006-10 and 2011-15 (from 74 to 43 applications, respectively), compared to a decrease of 11% for ULMs, no change for SLE, and increases of 16-18% for all others during the same period.
Overall, these data confirm the conclusions of the primary analysis, suggesting that PCOS is funded at a lower rate compared to other disorders studied, including other reproductive disorders. Further, while the data does not reveal a significant difference in funding rates by their principal funding IC, it does indicate that for PCOS, endometriosis and ULMs there is only one principal IC (NICHD) compared to two or three for SLE, RA and TB. Magnifying the discrepancy in funding rates between ‘principal’ and ‘non-principal’ funding ICs was the fact that PCOS had more than one-third of its applications submitted to ICs other than the NICHD, consistent with its recognized metabolic and vascular impact, but these ICs provided very low rates of funding.
Finally, and quite worrisome is the fact that the number of applications submitted dropped by almost 50% from the beginning to the end of the period studied, a degree of reduction not observed for any of the other disorders studied. These data suggest that we are losing PCOS investigators at the exact time when the clinical and public health relevance of the disorder is being increasingly recognized.
Other issues that may also affect NIH funding for PCOS research by ICs other than the NICHD includes failure to consider as reproductive and/or metabolic such outcomes variables as general adiposity and body fat distribution. It also may reflect a paucity of basic science; assessing the MD-to-PhD ratio among grant applicants or awardees may be revealing. Furthermore, a lack of PCOS may mirror the size of the academic pool because this research is primarily carried out by pediatric, medical, and reproductive endocrinologists, which are generally part of small units and whose workforce is often engaged in addressing other consuming clinical issues (growth disorders, diabetes, thyroid dysfunction, obesity, and infertility). Nonetheless, it may be argued that the number of practitioners dealing with SLE or RA in any academic setting is also relatively small. Finally, a real or perceived reduction in funding for PCOS may, in turn, discourage investigators from pursuing research in the field, leading to a vicious cycle impeding research in this critical area. Our analysis of trends in the number of unsolicited competing R01 applications provided further support for this important concern.
PCOS Research Funding: Where to From Here?
First, subsequent studies need to attempt to determine whether the science in the proposals for PCOS research is of the same high quality as that for other disorders that garner higher levels of funding. These studies will be helpful in determining the direction and emphasis of research in PCOS.
Second, an obvious factor that can be addressed now is that PCOS seems to be exclusively funded through only one institute, the NICHD, which itself is primarily focused on reproductive outcomes. Consequently, better education of NHLBI and NIDDK leaders, and other related institutes, by professional societies, the scientific community, and patient advocates regarding PCOS, its economic burden, and its metabolic origin and consequences is needed.
Third, it is clear that greater advocacy, targeting the public and our elected representatives, is needed by these same groups to raise awareness of this pervasive and highly prevalent disease.
Importantly, many women with PCOS experience delayed diagnosis and inadequate information. Gibson-Helm and colleagues (24) carried out a large cross-sectional study to assess the diagnostic experiences, information obtained, main concerns, and support needs of women with PCOS, primarily from North America and Europe. A total of 1385 women from 48 different countries responded to the questionnaires. Nearly half of the participants had seen three or more health professionals before PCOS was diagnosed, and in one third of patients this process was over 2 years. In addition, only one third were satisfied with their diagnosis experience, and only 15% were satisfied with the information about PCOS provided at the time of their diagnosis. Dokras and colleagues (25) conducted a large-scale PCOS survey to identify gaps in PCOS knowledge and practice pattern among physicians in North America. Of the 630 surveys completed, 70% were from obstetrician-gynecologists, and slightly less than half of these were reproductive endocrinologists. The results revealed that 28% respondents did not know which PCOS criteria they used, one third associated “cysts on ovaries” with PCOS, and few were aware of the associated risk for depression and anxiety disorders and reduced QOL of these patients. Current misperceptions by clinicians regarding the pathophysiology of PCOS need to be corrected through better medical education to not only reduce worldwide patient dissatisfactions with PCOS-related health care but also to improve PCOS research in the future.
Summary
In summary, our data suggest that PCOS research may be relatively underfunded, at least by the NIH, considering its prevalence, morbidity, and negative impact on QOL, when compared with other chronic diseases with similar morbidity, albeit lower prevalence (at least in the United States). Greater education of NIH leaders, including those at the NHLBI and NIDDK, other federal and state agency leads, elected leaders, and the general public, by professional societies, the scientific community, and patient advocates regarding this disorder is likely needed. Because PCOS is a highly prevalent disorder affecting multiple aspects of women’s overall health, evidence from research on gender policies and women’s health suggests that policies intended to support women and families are associated with improved health outcomes for women or diminished sex inequalities in health (26).
Abbreviations:
- IC
Institute/Center
- NHLBI
National Heart, Lung, and Blood Institute
- NIAID
National Institute of Allergy and Infectious Diseases
- NICHD
National Institutes of Child Health and Development
- NIDDK
National Institute of Diabetes and Digestive and Kidney Diseases
- NIH
National Institutes of Health
- PCOS
polycystic ovary syndrome
- QOL
quality of life
- RA
rheumatoid arthritis
- SLE
systemic lupus erythematosus
- TB
tuberculosis
- ULM
uterine leiomyomas.
Acknowledgments
We are grateful to Dr. Louis DePaolo, Chief of the Fertility and Infertility Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, for his insights and for assisting in identifying some of the data utilized in this analysis.
Disclosure Summary: M.P.D. is on the Board of Directors and a stockholder of Advanced Reproductive Care and has Augusta University contracts with AbbVie and Bayer. R.A. is consultant for Ansh Laboratories, Latitude Capital, and Bayer Pharmaceuticals and advisor to GlobalPet Imaging. The remaining authors have nothing to disclose.
References
National Institutes of Health. Budget. Available at: https://www.nih.gov/about-nih/what-we-do/budget. Accessed May 20, 2017.
US Department of Health and Human Services. HHS FY2015 budget in brief. Available at: http://www.hhs.gov/about/budget/fy2015/budget-in-brief/nih/index.html. Accessed May 20, 2017.
Institute of Medicine. Women’s health research: progress, pitfalls, and promise. 2010. Available at: https://www.nap.edu/read/12908/chapter/1. Accessed May 20, 2017.



