-
PDF
- Split View
-
Views
-
Cite
Cite
G Nicholls, B Atkinson, K van Veldhoven, I Nicholls, M Coldwell, A Clarke, C J Atchison, A I Raja, A M Bennett, D Morgan, N Pearce, T Fletcher, E B Brickley, Y Chen, An outbreak of SARS-CoV-2 in a public-facing office in England, Occupational Medicine, Volume 74, Issue 7, October 2024, Pages 475–485, https://doi.org/10.1093/occmed/kqad100
Close - Share Icon Share
Abstract
An outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with an attack rate of 55% (22/40 workers) occurred at a public-facing office in England from August to September 2021. Published evidence regarding outbreaks in office workplaces remains limited.
To describe an investigation of workplace- and worker-related risk factors following an outbreak of SARS-CoV-2 in a public-facing office.
The COVID-19 (coronavirus disease 2019) Outbreak Investigation to Understand Transmission (COVID-OUT) study undertook an investigation of the outbreak. This included surface sampling, occupational environmental assessment, molecular and serological testing of workers, and detailed questionnaires.
Despite existing COVID-19 control measures, surface sampling conducted during a self-imposed 2-week temporary office closure identified viral contamination (10/60 samples, 17% positive), particularly in a small, shared security office (6/9, 67% positive) and on a window handle in one open-plan office. Targeted enhanced cleaning was, therefore, undertaken before the office reopened. Repeat surface sampling after this identified only one positive (2%) sample. Ventilation was deemed adequate using carbon dioxide monitoring (typically ≤1000 ppm). Twelve workers (30%) responded to the COVID-OUT questionnaire, and all had been vaccinated with two doses. One-third of respondents (4/12) reported direct physical or close contact with members of the public; of these, 75% (3/4) reported a divider/screen between themselves and members of the public.
The results highlight the potential utility of surface sampling to identify SARS-CoV-2 control deficiencies and the importance of evolving, site-specific risk assessments with layered COVID-19 mitigation strategies.
Introduction
Workplace outbreaks of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), in public-facing offices have rarely been reported in the literature, despite workers’ proximity to members of the public.
The COVID-19 Outbreak Investigation to Understand Transmission (COVID-OUT) study, part of the PROTECT COVID-19 National Core Study on transmission and environment [1], was established to contribute to a better understanding of workplace SARS-CoV-2 outbreaks and transmission risks across different work sectors. COVID-OUT has established a protocol under which relevant data can be collected in a consistent and systematic way, to enable individual outbreak investigations and comparisons across outbreaks [2]. The COVID-OUT study has previously reported investigations into outbreaks at two manufacturing sites [3, 4]. Here, we report an outbreak investigation of a cluster of SARS-CoV-2 cases at a public-facing office in England, UK. The COVID-OUT team was informed of the outbreak on 31st August 2021. At this time, most UK Government restrictions on social contact had been removed, and the economy was considered fully open [5]. While 78% of residents (aged ≥12 years) in the local community had received two doses of COVID-19 vaccines [6], rates of SARS-CoV-2 infections had been increasing slowly in the 2 months prior to this outbreak (Figure 1). Following the emergence of a cluster of SARS-CoV-2 at a public-facing office, the workplace voluntarily implemented a 2-week temporary office closure to minimize the risk to workers with all staff instructed to work from home. The outbreak, therefore, provided the COVID-OUT study with a valuable opportunity not only to investigate worker- and workplace-associated risk factors, but also to undertake surface sampling while the office was closed and provide timely advice to the workplace before reopening. This paper reports the results of this detailed investigation.
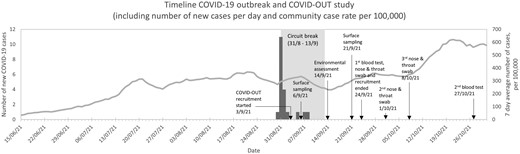
Timeline and epidemiological curve of a SARS-CoV-2 outbreak and the COVID-OUT investigation in a public-facing office, England, August to September 2021. Arrows indicate key dates of the outbreak and COVID-OUT study activities. The grey box indicates the self-imposed temporary office closer, which was implemented at the moment of identification of the initial cluster of cases. The bars represent the number of new COVID-19 cases reported to the site. The line chart represents the 7-day average case rate for the lower tier local authority area at which the company was based (publicly available from (https://coronavirus.data.gov.uk/); date of download 29 November 2023.
Workplaces are important when considering sites and routes for potential SARS-CoV-2 transmission.
Outbreaks of COVID-19 in public-facing offices are rarely reported or studied in the literature.
This study illustrates that public-facing office settings are vulnerable to acute SARS-CoV-2 outbreaks.
Undertaking a detailed voluntary research study during a workplace outbreak is challenging with interpretation hindered by numerous factors including gaining consent and access to site after the peak of the outbreak, and low workforce participation rates.
Our findings reinforce the value of environmental analysis, including surface sampling, for providing insights into potential infection control deficiencies; dissemination of these findings can assist other workplaces to maintain suitable control measures to maintain essential work and core societal functions.
Evolving, site-specific risk assessments with layered control strategies are imperative to mitigate against transmission of SARS-CoV-2 within workplaces.
These assessments require regular review to ensure suitability as a pandemic evolves, especially regarding changing infection rates within the local community.
Methods
A cluster of 11 SARS-CoV-2 cases among a workforce of 40 staff at a public-facing office was reported to the COVID-OUT team on 31st August 2021 by the organization. The COVID-OUT team undertook an outbreak investigation from 3rd September to 27th October 2021, using a previously described protocol [2]. The development of the protocol is described elsewhere [2] and the methodology is outlined below. The NHS North East Research Ethics Committee (Reference 20/NE/0282) provided ethical approval.
The building occupied by the organization reporting the outbreak was a public sector facility shared with other departments. There was minimal mixing of staff between departments, which occupied different wings of the building with just a shared entrance. The outbreak investigation was, therefore, restricted to the areas occupied by the reporting organization.
An environmental assessment was conducted when the facility reopened after the 2-week temporary office closure. This followed a previously developed framework, which included collecting information on the building layout, temperature, humidity, sound, observed work activities and COVID-19 control measures [7]. Ventilation was assessed using carbon dioxide (CO2) as a proxy; concentrations were determined by spot measurements during the visit and continuous measurements logged over the subsequent 2-week period. Monitoring locations were selected based on where workers might gather (e.g. canteen) and areas of particular interest, such as a small meeting room and a small security office with high occupancy prior to the outbreak. CO2 levels above 1500 ppm would be considered indicative of inadequate ventilation [8].
Two rounds of surface sampling were performed. One was undertaken during the 2-week temporary office closure sampling all areas; the other was undertaken 1 week after the workplace reopening and targeted areas of interest. The sampling used either Envirostik with Neutralising Buffer (Technical Service Consultants Ltd) or UTM swabs (Copan). Quantitative reverse transcription-polymerase chain reaction (qRT-PCR) for both ORF1ab and nucleocapsid (N) gene targets was performed in duplicate using the VIASURE SARS-CoV-2 Real-Time PCR Detection Kit (CerTest) in accordance with the manufacturer’s instructions [9,10]. The reportable detection limit was a crossing threshold (Ct) value of 38.0 as recommended by the manufacturer’s instructions. Confirmed positive samples were those with both replicates testing positive for at least one target, and suspected positive samples were those with a single replicate testing positive for at least one target. Samples with Ct values of <35 were further assessed by whole genome sequencing (WGS).
From 3rd to 24th September, workers from the site were invited to participate in the study. Participants completed a questionnaire at baseline obtaining information on work, lifestyle and health, in addition to potential risk factors such as use of personal protective equipment, job security and numbers of close contacts [11]. Two rounds of SARS-CoV-2 antibody testing in blood samples collected by phlebotomists were performed (baseline and Week 6), and three rounds of qRT-PCR (baseline, Week 2 and Week 3) [2]. Participants were also asked to complete a shorter follow-up questionnaire at the same time as testing at Weeks 2, 3 and 6 to collect data on recent symptoms and any changes to vaccination status. Confirmed cases were defined as participants who presented during the outbreak period with (i) real-time polymerase chain reaction (RT-PCR) evidence of a SARS-CoV-2 infection, (ii) N-specific seroconversion, or (iii) self-reporting of a positive test (i.e. by qRT-PCR or lateral flow device [LFD]) with positive N antibody results confirmed during COVID-OUT testing. Suspected cases were defined as participants who had no positive qRT-PCR or N antibody results from the COVID-OUT testing but who presented during the outbreak period with (i) a self-reported positive test (i.e. by qRT-PCR or LFD) or (ii) symptoms consistent with COVID-19 defined as (a) acute onset of fever (>37.8°C) and new continuous cough or (b) acute onset of any three or more symptoms of fever (>37.8°C), cough, shortness of breath, loss of taste or smell, runny nose, fatigue, sore throat, muscle or body aches, headache, nausea or vomiting, and/or diarrhoea.
Attack rates were calculated by dividing the total number of cases by the total number of workers [12] using company-supplied data. Fisher’s exact test was used to compare the attack rate for different job roles.
Results
From 30th August to 8th September, a total of 22 out of 40 workers (attack rate of 55%) were reported by the organization to have SARS-CoV-2 infections (Figure 1): 75% of cleaners (3/4), 50% of office staff (15/30) and 67% of security staff (4/6) tested positive. The attack rates observed for cleaners and security staff were not statistically significantly different from that of office staff (both P > 0.10).
An environmental assessment was conducted upon reopening after the 2-week temporary office closure (Figure 1). Each of the three floors had one or two large open-plan offices, low-occupancy offices, meeting rooms and toilets. In addition, there was a canteen/lunchroom on the second floor, and a small security office on the ground floor. Security and cleaning staff were subcontracted but were permanently assigned to the site. Security staff patrolled the facility on 30-minute rotating shifts and operated shared equipment in the 7.8-m2 security office. At the time of the outbreak, the maximum occupancy for the security office was two with security staff rotating positions regularly between this location and other areas within the building. Visitors had their own entrance on the ground floor, where they interacted with security staff, were booked in and were directed to their appointment. Office-based staff had up to 15 face-to-face meetings with visitors per day. Appointments took place at desks in the open-plan offices on the ground and first floors. Plastic screens separated the members of the public and office-based staff, and some desks were not in use to enable 2-m physical distancing. Office-based staff were allocated their own desk and did not share with colleagues. The surfaces of the desk, plastic screen and chair occupied by the member of the public were disinfected by cleaning staff between appointments.
The workplace had a site-specific COVID-19 risk assessment based on a generic template provided by the parent organization. This had been tailored to the site and recently updated prior to the outbreak. Additional control measures included COVID-19 training for workers, commercial hand sanitizers and an enhanced cleaning regimen. In line with government guidance at the time, there was no requirement for staff to wear face coverings and no staff were observed wearing face coverings on the day of the environmental assessment. Ventilation was natural (i.e. manually opened windows) with some locally controlled air conditioning units and limited forced mechanical general ventilation. CO2 measurements were all ≤700 ppm in the open-plan office and canteen. Measurements in the security office and small meeting room were all ≤1000 ppm except for two spikes: one in each location, which peaked at 1200 ppm.
The first round of surface sampling was conducted approximately 1 week after the first identified case and during the 2-week temporary office closure (Figure 1). Out of 60 surfaces tested, 10 (17%) were confirmed positives and 1 (2%) was a suspected positive (Table 1). Five (8%) positive samples produced Ct values between 32.0 and 34.9. WGS was attempted on these five samples, but only a partial sequence was identified from a single sample (window handle, second-floor open-plan office). These data implied delta variant sequence but, as less than 50% of the genome was recovered, this could not be confirmed. The security office appeared to be a site of enhanced viral contamination with six of the nine (67%) samples from this location testing positive, including three in the 32.0–34.9 Ct bracket. Based on these initial findings, enhanced cleaning was performed prior to reopening, and routine cleaning procedures were updated to include disinfection of window handles; maximum occupancy and cleaning regimens in the security office were also reassessed. Repeat surface sampling performed ~1 week after reopening targeted the security office, sign-in area, and canteen/lunchroom as areas of interest. This identified only one positive (2%) and one suspected positive (2%) sample, both near the assay’s limit of detection (Table 1).
Data collected from two rounds of surface sampling in the COVID-OUT investigation of an outbreak of SARS-CoV-2 in an office-based workplace, England, August to September 2021
| Date . | Samples collected . | qRT-PCR result . | Level of RNA (base on Ct value) . | ||||
|---|---|---|---|---|---|---|---|
| Confirmed positive, n (%) . | Suspected positive, n (%) . | Negative, n (%) . | Moderate–high (Ct < 32.0), n (%) . | Low (Ct 32.0–34.9), n (%) . | Very low–None (Ct > 35.0a) n (%) . | ||
| 06/SEP/21 | 60 | 10 (17%) | 1 (2%) | 49 (82%) | 0 (0%) | 5 (8%) | 55 (92%) |
| 21/SEP/21 | 42 | 1 (2%) | 1 (2%) | 40 (95%) | 0 (0%) | 0 (0%) | 42 (100%) |
| Date . | Samples collected . | qRT-PCR result . | Level of RNA (base on Ct value) . | ||||
|---|---|---|---|---|---|---|---|
| Confirmed positive, n (%) . | Suspected positive, n (%) . | Negative, n (%) . | Moderate–high (Ct < 32.0), n (%) . | Low (Ct 32.0–34.9), n (%) . | Very low–None (Ct > 35.0a) n (%) . | ||
| 06/SEP/21 | 60 | 10 (17%) | 1 (2%) | 49 (82%) | 0 (0%) | 5 (8%) | 55 (92%) |
| 21/SEP/21 | 42 | 1 (2%) | 1 (2%) | 40 (95%) | 0 (0%) | 0 (0%) | 42 (100%) |
| Positive sample information . | |||||||
|---|---|---|---|---|---|---|---|
| Location Date . | Description . | Mean Ct Valueb . | Estimated copies per cm2c . | ||||
| Open-plan office (2nd floor) 06/SEP/21 | Window handle | 33.6 | 4589.9 | ||||
| Meeting room (1st floor) 06/SEP/21 | Air vent | 37.6 (suspectd) | 25.1 | ||||
| Meeting room (1st floor) 06/SEP/21 | Desk + chair | 37.4 | 7.0 | ||||
| Canteen 06/SEP/21 | Table + chair | 34.2 | 35.2 | ||||
| Security office 06/SEP/21 | Radio (two-way) | 36.7 | 12.8 | ||||
| Security office 06/SEP/21 | Telephone | 34.6 | 583.1 | ||||
| Security office 06/SEP/21 | Key press | 34.5 | 148.1 | ||||
| Security office 06/SEP/21 | Control panel | 34.2 | 229.4 | ||||
| Security office 06/SEP/21 | Telephone | 35.1 | 214.2 | ||||
| Security office 06/SEP/21 | Desk + chair | 37.7 | 19.5 | ||||
| Open-plan office (ground floor) 06/SEP/21 | Air conditioning unit | 37.6 | 13.1 | ||||
| Canteen 21/SEP/21 | Desk + chair | 37.6 (suspectd) | 1.1 | ||||
| Canteen 21/SEP/21 | Desk + chair | 37.2 | 1.7 | ||||
| Positive sample information . | |||||||
|---|---|---|---|---|---|---|---|
| Location Date . | Description . | Mean Ct Valueb . | Estimated copies per cm2c . | ||||
| Open-plan office (2nd floor) 06/SEP/21 | Window handle | 33.6 | 4589.9 | ||||
| Meeting room (1st floor) 06/SEP/21 | Air vent | 37.6 (suspectd) | 25.1 | ||||
| Meeting room (1st floor) 06/SEP/21 | Desk + chair | 37.4 | 7.0 | ||||
| Canteen 06/SEP/21 | Table + chair | 34.2 | 35.2 | ||||
| Security office 06/SEP/21 | Radio (two-way) | 36.7 | 12.8 | ||||
| Security office 06/SEP/21 | Telephone | 34.6 | 583.1 | ||||
| Security office 06/SEP/21 | Key press | 34.5 | 148.1 | ||||
| Security office 06/SEP/21 | Control panel | 34.2 | 229.4 | ||||
| Security office 06/SEP/21 | Telephone | 35.1 | 214.2 | ||||
| Security office 06/SEP/21 | Desk + chair | 37.7 | 19.5 | ||||
| Open-plan office (ground floor) 06/SEP/21 | Air conditioning unit | 37.6 | 13.1 | ||||
| Canteen 21/SEP/21 | Desk + chair | 37.6 (suspectd) | 1.1 | ||||
| Canteen 21/SEP/21 | Desk + chair | 37.2 | 1.7 | ||||
RNA, ribonucleic acid.
aIncludes samples with no SARS-CoV-2 RNA detected.
bMean Ct value for the N gene.
cExtrapolation from copies per reaction to copies per sample collected based on the dilution factor, then divided by recorded sampling area.
dA ‘suspected positive’ is one where only a single replicate is positive in at least one target.
Data collected from two rounds of surface sampling in the COVID-OUT investigation of an outbreak of SARS-CoV-2 in an office-based workplace, England, August to September 2021
| Date . | Samples collected . | qRT-PCR result . | Level of RNA (base on Ct value) . | ||||
|---|---|---|---|---|---|---|---|
| Confirmed positive, n (%) . | Suspected positive, n (%) . | Negative, n (%) . | Moderate–high (Ct < 32.0), n (%) . | Low (Ct 32.0–34.9), n (%) . | Very low–None (Ct > 35.0a) n (%) . | ||
| 06/SEP/21 | 60 | 10 (17%) | 1 (2%) | 49 (82%) | 0 (0%) | 5 (8%) | 55 (92%) |
| 21/SEP/21 | 42 | 1 (2%) | 1 (2%) | 40 (95%) | 0 (0%) | 0 (0%) | 42 (100%) |
| Date . | Samples collected . | qRT-PCR result . | Level of RNA (base on Ct value) . | ||||
|---|---|---|---|---|---|---|---|
| Confirmed positive, n (%) . | Suspected positive, n (%) . | Negative, n (%) . | Moderate–high (Ct < 32.0), n (%) . | Low (Ct 32.0–34.9), n (%) . | Very low–None (Ct > 35.0a) n (%) . | ||
| 06/SEP/21 | 60 | 10 (17%) | 1 (2%) | 49 (82%) | 0 (0%) | 5 (8%) | 55 (92%) |
| 21/SEP/21 | 42 | 1 (2%) | 1 (2%) | 40 (95%) | 0 (0%) | 0 (0%) | 42 (100%) |
| Positive sample information . | |||||||
|---|---|---|---|---|---|---|---|
| Location Date . | Description . | Mean Ct Valueb . | Estimated copies per cm2c . | ||||
| Open-plan office (2nd floor) 06/SEP/21 | Window handle | 33.6 | 4589.9 | ||||
| Meeting room (1st floor) 06/SEP/21 | Air vent | 37.6 (suspectd) | 25.1 | ||||
| Meeting room (1st floor) 06/SEP/21 | Desk + chair | 37.4 | 7.0 | ||||
| Canteen 06/SEP/21 | Table + chair | 34.2 | 35.2 | ||||
| Security office 06/SEP/21 | Radio (two-way) | 36.7 | 12.8 | ||||
| Security office 06/SEP/21 | Telephone | 34.6 | 583.1 | ||||
| Security office 06/SEP/21 | Key press | 34.5 | 148.1 | ||||
| Security office 06/SEP/21 | Control panel | 34.2 | 229.4 | ||||
| Security office 06/SEP/21 | Telephone | 35.1 | 214.2 | ||||
| Security office 06/SEP/21 | Desk + chair | 37.7 | 19.5 | ||||
| Open-plan office (ground floor) 06/SEP/21 | Air conditioning unit | 37.6 | 13.1 | ||||
| Canteen 21/SEP/21 | Desk + chair | 37.6 (suspectd) | 1.1 | ||||
| Canteen 21/SEP/21 | Desk + chair | 37.2 | 1.7 | ||||
| Positive sample information . | |||||||
|---|---|---|---|---|---|---|---|
| Location Date . | Description . | Mean Ct Valueb . | Estimated copies per cm2c . | ||||
| Open-plan office (2nd floor) 06/SEP/21 | Window handle | 33.6 | 4589.9 | ||||
| Meeting room (1st floor) 06/SEP/21 | Air vent | 37.6 (suspectd) | 25.1 | ||||
| Meeting room (1st floor) 06/SEP/21 | Desk + chair | 37.4 | 7.0 | ||||
| Canteen 06/SEP/21 | Table + chair | 34.2 | 35.2 | ||||
| Security office 06/SEP/21 | Radio (two-way) | 36.7 | 12.8 | ||||
| Security office 06/SEP/21 | Telephone | 34.6 | 583.1 | ||||
| Security office 06/SEP/21 | Key press | 34.5 | 148.1 | ||||
| Security office 06/SEP/21 | Control panel | 34.2 | 229.4 | ||||
| Security office 06/SEP/21 | Telephone | 35.1 | 214.2 | ||||
| Security office 06/SEP/21 | Desk + chair | 37.7 | 19.5 | ||||
| Open-plan office (ground floor) 06/SEP/21 | Air conditioning unit | 37.6 | 13.1 | ||||
| Canteen 21/SEP/21 | Desk + chair | 37.6 (suspectd) | 1.1 | ||||
| Canteen 21/SEP/21 | Desk + chair | 37.2 | 1.7 | ||||
RNA, ribonucleic acid.
aIncludes samples with no SARS-CoV-2 RNA detected.
bMean Ct value for the N gene.
cExtrapolation from copies per reaction to copies per sample collected based on the dilution factor, then divided by recorded sampling area.
dA ‘suspected positive’ is one where only a single replicate is positive in at least one target.
Between 3rd and 24th September 2021, 12 workers (30% response rate; 92% female; mean age 51 years, range 34–66 years; 100% office workers on regular day shift; 75% permanent contract) consented to participate in the COVID-OUT study. Of the 12 participants, 5 (42%) self-reported positive SARS-CoV-2 tests during the outbreak period; COVID-OUT serological testing confirmed all 5 were positive for both N- and S-specific antibodies against SARS-CoV-2 and 2 were positive by qRT-PCR from samples collected as part of the COVID-OUT study. No suspected cases were identified. The five non-cases who had undertaken COVID-OUT testing were positive for S- but not N-antibodies, confirming that they had been vaccinated but not previously infected (Table 2). Prior to the outbreak, all participants who responded to the questionnaire had received two doses of COVID-19 vaccines (date range of second dose: 4th May to 12th July in cases and 21st May to 30th July in non-cases; n = 2 [18%] with Pfizer/BioNTech, n = 9 [82%] with Oxford/AstraZeneca, and n = 1 did not report the vaccine type). All respondents reported a good supply of fresh air in the workplace (Table 3). Four participants (33%) reported direct physical or close contact with co-workers and members of the public. Of these, three workers (75%) reported a divider/screen between themselves and members of the public (Table 4). Most participants thought their pay would not change if they needed to self-isolate (n = 10, 83%) or if the workplace needed to close for 2 weeks due to COVID-19 (n = 10, 83%). When asked about infection control measures at work (Table 4), most (n = 11, 92%) reported receiving COVID-19 training (e.g. reading guidance or formal training). All reported having access to hand washing/sanitizing facilities at work and the majority (n = 10, 83%) reported wearing either a washable face mask/covering or a surgical/disposable mask at work. Contact patterns were similar between cases and non-cases (Table 5). Most reported some close contact with others in their workplace (n = 8, 73%), and just under half reported long close contact in their workplace lasting more than 1 hour (n = 5, 42%). Most reported close contact during non-work activities such as socializing (n = 8, 73%) and essential activities (e.g. food shopping) (n = 9, 82%). Just over half of respondents (n = 7, 58%; four non-cases and three cases) reported known contact with a COVID-19-positive individual. Of these, three (43%, two non-cases and one case) reported the positive contact was someone they worked with.
Characteristics, test results and clinical presentation of participants in the COVID-OUT study questionnaire and testing
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Characteristics | Sex | Male | 0 (0) | 1 (20) | 1 (8) |
| Female | 7 (100) | 4 (80) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Age | Mean (min–max) | 49 (34–66) | 54 (48–62) | 51 (34–66) | |
| Missing, n | 0 | 0 | 0 | ||
| BMI category | Normal weight (18.5–24.9) | 0 (0) | 0 (0) | 0 (0) | |
| Overweight (15.0–29.9) | 2 (33) | 4 (80) | 6 (55) | ||
| Obese (30+) | 4 (67) | 1 (20) | 5 (45) | ||
| Missing | 1 | 0 | 1 | ||
| Smoking status | No, never | 2 (40) | 3 (43) | 5 (42) | |
| No, ex-smoker | 2 (40) | 3 (43) | 5 (42) | ||
| Yes, current | 1 (20) | 1 (14) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| SARS-CoV-2 testing | Positive RT-PCRc | Yes | 0 (0) | 2 (100) | 2 (67) |
| Missing/invalid d | 3 | 3 | 6 | ||
| Positive anti-SARS-CoV-2 N (nucleocapsid) at any blood test | Yes | 0 (0) | 5 (100) | 5 (50) | |
| Missing e | 2 | 0 | 2 | ||
| Any self-reported positive test during outbreak period | Yes | 0 (0) | 5 (100) | 5 (42) | |
| None reported | 7 (100) | 0 (0) | 7 (58) | ||
| Signs and symptoms of COVID-19 | Reported during outbreak period | None reported | 7 (100) | 0 (0) | 7 (58) |
| Fever | 0 (0) | 3 (60) | 3 (25) | ||
| Dry cough | 0 (0) | 3 (60) | 3 (25) | ||
| Productive cough | 0 (0) | 3 (60) | 3 (25) | ||
| Shortness of breath | 0 (0) | 3 (60) | 3 (25) | ||
| Loss of taste or smell | 0 (0) | 4 (80) | 4 (33) | ||
| Vaccination | Vaccinated prior to outbreak start | Yes, two doses | 7 (100) | 5 (100) | 12 (100) |
| Missing | 0 | 0 | 0 | ||
| Vaccine type | Pfizer/BioNTech | 2 (29) | 0 (0) | 2 (18) | |
| Oxford/AstraZeneca | 5 (71) | 4 (100) | 9 (82) | ||
| Missing | 0 | 1 | 1 |
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Characteristics | Sex | Male | 0 (0) | 1 (20) | 1 (8) |
| Female | 7 (100) | 4 (80) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Age | Mean (min–max) | 49 (34–66) | 54 (48–62) | 51 (34–66) | |
| Missing, n | 0 | 0 | 0 | ||
| BMI category | Normal weight (18.5–24.9) | 0 (0) | 0 (0) | 0 (0) | |
| Overweight (15.0–29.9) | 2 (33) | 4 (80) | 6 (55) | ||
| Obese (30+) | 4 (67) | 1 (20) | 5 (45) | ||
| Missing | 1 | 0 | 1 | ||
| Smoking status | No, never | 2 (40) | 3 (43) | 5 (42) | |
| No, ex-smoker | 2 (40) | 3 (43) | 5 (42) | ||
| Yes, current | 1 (20) | 1 (14) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| SARS-CoV-2 testing | Positive RT-PCRc | Yes | 0 (0) | 2 (100) | 2 (67) |
| Missing/invalid d | 3 | 3 | 6 | ||
| Positive anti-SARS-CoV-2 N (nucleocapsid) at any blood test | Yes | 0 (0) | 5 (100) | 5 (50) | |
| Missing e | 2 | 0 | 2 | ||
| Any self-reported positive test during outbreak period | Yes | 0 (0) | 5 (100) | 5 (42) | |
| None reported | 7 (100) | 0 (0) | 7 (58) | ||
| Signs and symptoms of COVID-19 | Reported during outbreak period | None reported | 7 (100) | 0 (0) | 7 (58) |
| Fever | 0 (0) | 3 (60) | 3 (25) | ||
| Dry cough | 0 (0) | 3 (60) | 3 (25) | ||
| Productive cough | 0 (0) | 3 (60) | 3 (25) | ||
| Shortness of breath | 0 (0) | 3 (60) | 3 (25) | ||
| Loss of taste or smell | 0 (0) | 4 (80) | 4 (33) | ||
| Vaccination | Vaccinated prior to outbreak start | Yes, two doses | 7 (100) | 5 (100) | 12 (100) |
| Missing | 0 | 0 | 0 | ||
| Vaccine type | Pfizer/BioNTech | 2 (29) | 0 (0) | 2 (18) | |
| Oxford/AstraZeneca | 5 (71) | 4 (100) | 9 (82) | ||
| Missing | 0 | 1 | 1 |
BMI: body mass index; RT-PCR: real-time polymerase chain reaction.
aTwo out of seven controls did not undertake any testing as part of COVID-OUT and so are not confirmed negatives but classified as non-cases.
bOnly confirmed cases were identified. There were no suspected cases.
cAll RT-PCR tests were undertaken after the outbreak period.
dSix had missing/invalid tests for their first RT-PCR; nine had missing/invalid tests for their second RT-PCR; eight had missing/invalid tests for their third RT-PCR.
eFour were missing their first blood test; three were missing their second blood test.
Characteristics, test results and clinical presentation of participants in the COVID-OUT study questionnaire and testing
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Characteristics | Sex | Male | 0 (0) | 1 (20) | 1 (8) |
| Female | 7 (100) | 4 (80) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Age | Mean (min–max) | 49 (34–66) | 54 (48–62) | 51 (34–66) | |
| Missing, n | 0 | 0 | 0 | ||
| BMI category | Normal weight (18.5–24.9) | 0 (0) | 0 (0) | 0 (0) | |
| Overweight (15.0–29.9) | 2 (33) | 4 (80) | 6 (55) | ||
| Obese (30+) | 4 (67) | 1 (20) | 5 (45) | ||
| Missing | 1 | 0 | 1 | ||
| Smoking status | No, never | 2 (40) | 3 (43) | 5 (42) | |
| No, ex-smoker | 2 (40) | 3 (43) | 5 (42) | ||
| Yes, current | 1 (20) | 1 (14) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| SARS-CoV-2 testing | Positive RT-PCRc | Yes | 0 (0) | 2 (100) | 2 (67) |
| Missing/invalid d | 3 | 3 | 6 | ||
| Positive anti-SARS-CoV-2 N (nucleocapsid) at any blood test | Yes | 0 (0) | 5 (100) | 5 (50) | |
| Missing e | 2 | 0 | 2 | ||
| Any self-reported positive test during outbreak period | Yes | 0 (0) | 5 (100) | 5 (42) | |
| None reported | 7 (100) | 0 (0) | 7 (58) | ||
| Signs and symptoms of COVID-19 | Reported during outbreak period | None reported | 7 (100) | 0 (0) | 7 (58) |
| Fever | 0 (0) | 3 (60) | 3 (25) | ||
| Dry cough | 0 (0) | 3 (60) | 3 (25) | ||
| Productive cough | 0 (0) | 3 (60) | 3 (25) | ||
| Shortness of breath | 0 (0) | 3 (60) | 3 (25) | ||
| Loss of taste or smell | 0 (0) | 4 (80) | 4 (33) | ||
| Vaccination | Vaccinated prior to outbreak start | Yes, two doses | 7 (100) | 5 (100) | 12 (100) |
| Missing | 0 | 0 | 0 | ||
| Vaccine type | Pfizer/BioNTech | 2 (29) | 0 (0) | 2 (18) | |
| Oxford/AstraZeneca | 5 (71) | 4 (100) | 9 (82) | ||
| Missing | 0 | 1 | 1 |
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Characteristics | Sex | Male | 0 (0) | 1 (20) | 1 (8) |
| Female | 7 (100) | 4 (80) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Age | Mean (min–max) | 49 (34–66) | 54 (48–62) | 51 (34–66) | |
| Missing, n | 0 | 0 | 0 | ||
| BMI category | Normal weight (18.5–24.9) | 0 (0) | 0 (0) | 0 (0) | |
| Overweight (15.0–29.9) | 2 (33) | 4 (80) | 6 (55) | ||
| Obese (30+) | 4 (67) | 1 (20) | 5 (45) | ||
| Missing | 1 | 0 | 1 | ||
| Smoking status | No, never | 2 (40) | 3 (43) | 5 (42) | |
| No, ex-smoker | 2 (40) | 3 (43) | 5 (42) | ||
| Yes, current | 1 (20) | 1 (14) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| SARS-CoV-2 testing | Positive RT-PCRc | Yes | 0 (0) | 2 (100) | 2 (67) |
| Missing/invalid d | 3 | 3 | 6 | ||
| Positive anti-SARS-CoV-2 N (nucleocapsid) at any blood test | Yes | 0 (0) | 5 (100) | 5 (50) | |
| Missing e | 2 | 0 | 2 | ||
| Any self-reported positive test during outbreak period | Yes | 0 (0) | 5 (100) | 5 (42) | |
| None reported | 7 (100) | 0 (0) | 7 (58) | ||
| Signs and symptoms of COVID-19 | Reported during outbreak period | None reported | 7 (100) | 0 (0) | 7 (58) |
| Fever | 0 (0) | 3 (60) | 3 (25) | ||
| Dry cough | 0 (0) | 3 (60) | 3 (25) | ||
| Productive cough | 0 (0) | 3 (60) | 3 (25) | ||
| Shortness of breath | 0 (0) | 3 (60) | 3 (25) | ||
| Loss of taste or smell | 0 (0) | 4 (80) | 4 (33) | ||
| Vaccination | Vaccinated prior to outbreak start | Yes, two doses | 7 (100) | 5 (100) | 12 (100) |
| Missing | 0 | 0 | 0 | ||
| Vaccine type | Pfizer/BioNTech | 2 (29) | 0 (0) | 2 (18) | |
| Oxford/AstraZeneca | 5 (71) | 4 (100) | 9 (82) | ||
| Missing | 0 | 1 | 1 |
BMI: body mass index; RT-PCR: real-time polymerase chain reaction.
aTwo out of seven controls did not undertake any testing as part of COVID-OUT and so are not confirmed negatives but classified as non-cases.
bOnly confirmed cases were identified. There were no suspected cases.
cAll RT-PCR tests were undertaken after the outbreak period.
dSix had missing/invalid tests for their first RT-PCR; nine had missing/invalid tests for their second RT-PCR; eight had missing/invalid tests for their third RT-PCR.
eFour were missing their first blood test; three were missing their second blood test.
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Work factors | Good supply of fresh air in the workplace | No | 0 (0) | 0 (0) | 0 (0) |
| Yes, mechanical ventilation | 0 (0) | 1 (33) | 1 (11) | ||
| Yes, opening windows/doors | 6 (100) | 2 (67) | 8 (89) | ||
| Missing | 1 | 2 | 3 | ||
| Direct physical or close contact with co-workers or public | No | 5 (71) | 3 (60) | 8 (67) | |
| Yes, with co-workers and members of the public | 2 (29) | 2 (40) | 4 (33) | ||
| Missing | 0 | 0 | 0 | ||
| Need to talk loudly, or lean in to listen/speak | No | 2 (29) | 4 (80) | 6 (50) | |
| Yes, sometimes | 3 (43) | 1 (20) | 4 (33) | ||
| Yes, most of the time | 1 (14) | 0 (0) | 1 (8) | ||
| Yes, always | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Pay change due to self-isolation | No change | 6 (86) | 4 (80) | 10 (83) | |
| Don’t know | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Pay change due to work closure | No change | 6 (86) | 4 (80) | 10 (83) | |
| Don’t know | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Unemployment concerns due to self-isolation | No, not at all | 4 (57) | 3 (60) | 7 (58) | |
| No, not so much | 2 (29) | 0 (0) | 2 (17) | ||
| Yes, slightly | 0 (0) | 2 (40) | 2 (17) | ||
| Not sure | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 |
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Work factors | Good supply of fresh air in the workplace | No | 0 (0) | 0 (0) | 0 (0) |
| Yes, mechanical ventilation | 0 (0) | 1 (33) | 1 (11) | ||
| Yes, opening windows/doors | 6 (100) | 2 (67) | 8 (89) | ||
| Missing | 1 | 2 | 3 | ||
| Direct physical or close contact with co-workers or public | No | 5 (71) | 3 (60) | 8 (67) | |
| Yes, with co-workers and members of the public | 2 (29) | 2 (40) | 4 (33) | ||
| Missing | 0 | 0 | 0 | ||
| Need to talk loudly, or lean in to listen/speak | No | 2 (29) | 4 (80) | 6 (50) | |
| Yes, sometimes | 3 (43) | 1 (20) | 4 (33) | ||
| Yes, most of the time | 1 (14) | 0 (0) | 1 (8) | ||
| Yes, always | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Pay change due to self-isolation | No change | 6 (86) | 4 (80) | 10 (83) | |
| Don’t know | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Pay change due to work closure | No change | 6 (86) | 4 (80) | 10 (83) | |
| Don’t know | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Unemployment concerns due to self-isolation | No, not at all | 4 (57) | 3 (60) | 7 (58) | |
| No, not so much | 2 (29) | 0 (0) | 2 (17) | ||
| Yes, slightly | 0 (0) | 2 (40) | 2 (17) | ||
| Not sure | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 |
aTwo out of seven controls did not undertake any testing as part of COVID-OUT and so are not confirmed negatives but classified as non-cases.
bOnly confirmed cases were identified. There were no suspected cases.
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Work factors | Good supply of fresh air in the workplace | No | 0 (0) | 0 (0) | 0 (0) |
| Yes, mechanical ventilation | 0 (0) | 1 (33) | 1 (11) | ||
| Yes, opening windows/doors | 6 (100) | 2 (67) | 8 (89) | ||
| Missing | 1 | 2 | 3 | ||
| Direct physical or close contact with co-workers or public | No | 5 (71) | 3 (60) | 8 (67) | |
| Yes, with co-workers and members of the public | 2 (29) | 2 (40) | 4 (33) | ||
| Missing | 0 | 0 | 0 | ||
| Need to talk loudly, or lean in to listen/speak | No | 2 (29) | 4 (80) | 6 (50) | |
| Yes, sometimes | 3 (43) | 1 (20) | 4 (33) | ||
| Yes, most of the time | 1 (14) | 0 (0) | 1 (8) | ||
| Yes, always | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Pay change due to self-isolation | No change | 6 (86) | 4 (80) | 10 (83) | |
| Don’t know | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Pay change due to work closure | No change | 6 (86) | 4 (80) | 10 (83) | |
| Don’t know | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Unemployment concerns due to self-isolation | No, not at all | 4 (57) | 3 (60) | 7 (58) | |
| No, not so much | 2 (29) | 0 (0) | 2 (17) | ||
| Yes, slightly | 0 (0) | 2 (40) | 2 (17) | ||
| Not sure | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 |
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Work factors | Good supply of fresh air in the workplace | No | 0 (0) | 0 (0) | 0 (0) |
| Yes, mechanical ventilation | 0 (0) | 1 (33) | 1 (11) | ||
| Yes, opening windows/doors | 6 (100) | 2 (67) | 8 (89) | ||
| Missing | 1 | 2 | 3 | ||
| Direct physical or close contact with co-workers or public | No | 5 (71) | 3 (60) | 8 (67) | |
| Yes, with co-workers and members of the public | 2 (29) | 2 (40) | 4 (33) | ||
| Missing | 0 | 0 | 0 | ||
| Need to talk loudly, or lean in to listen/speak | No | 2 (29) | 4 (80) | 6 (50) | |
| Yes, sometimes | 3 (43) | 1 (20) | 4 (33) | ||
| Yes, most of the time | 1 (14) | 0 (0) | 1 (8) | ||
| Yes, always | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Pay change due to self-isolation | No change | 6 (86) | 4 (80) | 10 (83) | |
| Don’t know | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Pay change due to work closure | No change | 6 (86) | 4 (80) | 10 (83) | |
| Don’t know | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Unemployment concerns due to self-isolation | No, not at all | 4 (57) | 3 (60) | 7 (58) | |
| No, not so much | 2 (29) | 0 (0) | 2 (17) | ||
| Yes, slightly | 0 (0) | 2 (40) | 2 (17) | ||
| Not sure | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 |
aTwo out of seven controls did not undertake any testing as part of COVID-OUT and so are not confirmed negatives but classified as non-cases.
bOnly confirmed cases were identified. There were no suspected cases.
Work and non-work COVID-19 control measures reported by participants in the COVID-OUT study questionnaire
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| COVID-19 control measures at work | COVID-19 training at work | No | 1 (14) | 0 (0) | 1 (8) |
| Yes | 6 (86) | 5 (100) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Hand washing or sanitizing facilities at work | No | 0 (0) | 0 (0) | 0 (0) | |
| Yes | 7 (100) | 5 (100) | 12 (100) | ||
| Missing | 0 | 0 | 0 | ||
| Good hand hygiene practice signage at work | No | 1 (14) | 0 (0) | 1 (8) | |
| Yes | 6 (86) | 5 (100) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Frequency of hand washing/sanitizing in a day | Never | 0 (0) | 0 (0) | 0 (0) | |
| 1-10 times | 1 (17) | 1 (20) | 2 (18) | ||
| 11 + times | 5 (83) | 4 (80) | 9 (82) | ||
| Missing | 1 | 0 | 1 | ||
| Wear gloves | Never | 4 (57) | 5 (100) | 9 (75) | |
| < half the time | 2 (29) | 0 (0) | 2 (17) | ||
| > half the time | 0 (0) | 0 (0) | 0 (0) | ||
| Nearly all the time | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Wear washable face mask/ face covering | Never | 0 (0) | 3 (60) | 3 (25) | |
| < half the time | 1 (14) | 0 (0) | 1 (8) | ||
| > half the time | 2 (29) | 0 (0) | 2 (17) | ||
| Nearly all the time | 4 (57) | 2 (40) | 6 (50) | ||
| Missing | 0 | 0 | 0 | ||
| Wear surgical mask/ disposable mask | Never | 1 (14) | 3 (60) | 4 (33) | |
| < half the time | 0 (0) | 0 (0) | 0 (0) | ||
| > half the time | 1 (14) | 0 (0) | 1 (8) | ||
| Nearly all the time | 5 (71) | 2 (40) | 7 (58) | ||
| Missing | 0 | 0 | 0 | ||
| Wear FFP2 or FFP3 | Never | 6 (100) | 5 (100) | 11 (100) | |
| Missing | 1 | 0 | 1 | ||
| Wear face shield | Never | 6 (100) | 5 (100) | 11 (100) | |
| Missing | 1 | 0 | 1 | ||
| Divider, colleagues | No | 2 (100) | 1 (50) | 3 (75) | |
| Yes | 0 (0) | 1 (50) | 1 (25) | ||
| Not applicable c | 5 | 3 | 8 | ||
| Missing | 0 | 0 | 0 | ||
| Divider, public | No | 1 (50) | 0 (0) | 1 (25) | |
| Yes | 1 (50) | 2 (100) | 3 (75) | ||
| Not applicable c | 5 | 3 | 8 | ||
| Missing | 0 | 0 | 0 | ||
| Social distancing, colleagues | Rarely able to maintain | 0 (0) | 0 (0) | 0 (0) | |
| Sometimes able to maintain | 1 (50) | 0 (0) | 1 (25) | ||
| Mostly able to maintain | 1 (50) | 2 (100) | 3 (75) | ||
| Always able to maintain | 0 (0) | 0 (0) | 0 (0) | ||
| Missing | 5 | 3 | 8 | ||
| Social distancing, public | Rarely able to maintain | 1 (14) | 0 (0) | 1 (8) | |
| Sometimes able to maintain | 0 (0) | 1 (20) | 1 (8) | ||
| Mostly able to maintain | 6 (86) | 4 (80) | 10 (83) | ||
| Always able to maintain | 0 (0) | 0 (0) | 0 (0) | ||
| Missing | 0 | 0 | 0 | ||
| COVID-19 control measures not at work | Wear washable face mask/ face covering | Never | 2 (33) | 1 (25) | 3 (30) |
| <half the time | 1 (17) | 1 (25) | 2 (20) | ||
| >half the time | 0 (0) | 0 (0) | 0 (0) | ||
| Nearly all the time | 3 (50) | 2 (50) | 5 (50) | ||
| Missing | 1 | 1 | 2 | ||
| Wear surgical mask/ disposable mask | Never | 2 (29) | 1 (25) | 3 (27) | |
| < half the time | 0 (0) | 0 (0) | 0 (0) | ||
| > half the time | 1 (14) | 1 (25) | 2 (18) | ||
| Nearly all the time | 4 (57) | 2 (20) | 6 (55) | ||
| Missing | 0 | 1 | 1 | ||
| Wear face shield | Never | 5 (100) | 4 (100) | 9 (100) | |
| Missing | 2 | 1 | 3 |
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| COVID-19 control measures at work | COVID-19 training at work | No | 1 (14) | 0 (0) | 1 (8) |
| Yes | 6 (86) | 5 (100) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Hand washing or sanitizing facilities at work | No | 0 (0) | 0 (0) | 0 (0) | |
| Yes | 7 (100) | 5 (100) | 12 (100) | ||
| Missing | 0 | 0 | 0 | ||
| Good hand hygiene practice signage at work | No | 1 (14) | 0 (0) | 1 (8) | |
| Yes | 6 (86) | 5 (100) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Frequency of hand washing/sanitizing in a day | Never | 0 (0) | 0 (0) | 0 (0) | |
| 1-10 times | 1 (17) | 1 (20) | 2 (18) | ||
| 11 + times | 5 (83) | 4 (80) | 9 (82) | ||
| Missing | 1 | 0 | 1 | ||
| Wear gloves | Never | 4 (57) | 5 (100) | 9 (75) | |
| < half the time | 2 (29) | 0 (0) | 2 (17) | ||
| > half the time | 0 (0) | 0 (0) | 0 (0) | ||
| Nearly all the time | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Wear washable face mask/ face covering | Never | 0 (0) | 3 (60) | 3 (25) | |
| < half the time | 1 (14) | 0 (0) | 1 (8) | ||
| > half the time | 2 (29) | 0 (0) | 2 (17) | ||
| Nearly all the time | 4 (57) | 2 (40) | 6 (50) | ||
| Missing | 0 | 0 | 0 | ||
| Wear surgical mask/ disposable mask | Never | 1 (14) | 3 (60) | 4 (33) | |
| < half the time | 0 (0) | 0 (0) | 0 (0) | ||
| > half the time | 1 (14) | 0 (0) | 1 (8) | ||
| Nearly all the time | 5 (71) | 2 (40) | 7 (58) | ||
| Missing | 0 | 0 | 0 | ||
| Wear FFP2 or FFP3 | Never | 6 (100) | 5 (100) | 11 (100) | |
| Missing | 1 | 0 | 1 | ||
| Wear face shield | Never | 6 (100) | 5 (100) | 11 (100) | |
| Missing | 1 | 0 | 1 | ||
| Divider, colleagues | No | 2 (100) | 1 (50) | 3 (75) | |
| Yes | 0 (0) | 1 (50) | 1 (25) | ||
| Not applicable c | 5 | 3 | 8 | ||
| Missing | 0 | 0 | 0 | ||
| Divider, public | No | 1 (50) | 0 (0) | 1 (25) | |
| Yes | 1 (50) | 2 (100) | 3 (75) | ||
| Not applicable c | 5 | 3 | 8 | ||
| Missing | 0 | 0 | 0 | ||
| Social distancing, colleagues | Rarely able to maintain | 0 (0) | 0 (0) | 0 (0) | |
| Sometimes able to maintain | 1 (50) | 0 (0) | 1 (25) | ||
| Mostly able to maintain | 1 (50) | 2 (100) | 3 (75) | ||
| Always able to maintain | 0 (0) | 0 (0) | 0 (0) | ||
| Missing | 5 | 3 | 8 | ||
| Social distancing, public | Rarely able to maintain | 1 (14) | 0 (0) | 1 (8) | |
| Sometimes able to maintain | 0 (0) | 1 (20) | 1 (8) | ||
| Mostly able to maintain | 6 (86) | 4 (80) | 10 (83) | ||
| Always able to maintain | 0 (0) | 0 (0) | 0 (0) | ||
| Missing | 0 | 0 | 0 | ||
| COVID-19 control measures not at work | Wear washable face mask/ face covering | Never | 2 (33) | 1 (25) | 3 (30) |
| <half the time | 1 (17) | 1 (25) | 2 (20) | ||
| >half the time | 0 (0) | 0 (0) | 0 (0) | ||
| Nearly all the time | 3 (50) | 2 (50) | 5 (50) | ||
| Missing | 1 | 1 | 2 | ||
| Wear surgical mask/ disposable mask | Never | 2 (29) | 1 (25) | 3 (27) | |
| < half the time | 0 (0) | 0 (0) | 0 (0) | ||
| > half the time | 1 (14) | 1 (25) | 2 (18) | ||
| Nearly all the time | 4 (57) | 2 (20) | 6 (55) | ||
| Missing | 0 | 1 | 1 | ||
| Wear face shield | Never | 5 (100) | 4 (100) | 9 (100) | |
| Missing | 2 | 1 | 3 |
aTwo out of seven controls did not undertake any testing as part of COVID-OUT and so are not confirmed negatives but classified as non-cases.
bOnly confirmed cases were identified. There were no suspected cases.
cNot applicable: participants did not report direct physical or close contract with co-workers or members of the public.
Work and non-work COVID-19 control measures reported by participants in the COVID-OUT study questionnaire
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| COVID-19 control measures at work | COVID-19 training at work | No | 1 (14) | 0 (0) | 1 (8) |
| Yes | 6 (86) | 5 (100) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Hand washing or sanitizing facilities at work | No | 0 (0) | 0 (0) | 0 (0) | |
| Yes | 7 (100) | 5 (100) | 12 (100) | ||
| Missing | 0 | 0 | 0 | ||
| Good hand hygiene practice signage at work | No | 1 (14) | 0 (0) | 1 (8) | |
| Yes | 6 (86) | 5 (100) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Frequency of hand washing/sanitizing in a day | Never | 0 (0) | 0 (0) | 0 (0) | |
| 1-10 times | 1 (17) | 1 (20) | 2 (18) | ||
| 11 + times | 5 (83) | 4 (80) | 9 (82) | ||
| Missing | 1 | 0 | 1 | ||
| Wear gloves | Never | 4 (57) | 5 (100) | 9 (75) | |
| < half the time | 2 (29) | 0 (0) | 2 (17) | ||
| > half the time | 0 (0) | 0 (0) | 0 (0) | ||
| Nearly all the time | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Wear washable face mask/ face covering | Never | 0 (0) | 3 (60) | 3 (25) | |
| < half the time | 1 (14) | 0 (0) | 1 (8) | ||
| > half the time | 2 (29) | 0 (0) | 2 (17) | ||
| Nearly all the time | 4 (57) | 2 (40) | 6 (50) | ||
| Missing | 0 | 0 | 0 | ||
| Wear surgical mask/ disposable mask | Never | 1 (14) | 3 (60) | 4 (33) | |
| < half the time | 0 (0) | 0 (0) | 0 (0) | ||
| > half the time | 1 (14) | 0 (0) | 1 (8) | ||
| Nearly all the time | 5 (71) | 2 (40) | 7 (58) | ||
| Missing | 0 | 0 | 0 | ||
| Wear FFP2 or FFP3 | Never | 6 (100) | 5 (100) | 11 (100) | |
| Missing | 1 | 0 | 1 | ||
| Wear face shield | Never | 6 (100) | 5 (100) | 11 (100) | |
| Missing | 1 | 0 | 1 | ||
| Divider, colleagues | No | 2 (100) | 1 (50) | 3 (75) | |
| Yes | 0 (0) | 1 (50) | 1 (25) | ||
| Not applicable c | 5 | 3 | 8 | ||
| Missing | 0 | 0 | 0 | ||
| Divider, public | No | 1 (50) | 0 (0) | 1 (25) | |
| Yes | 1 (50) | 2 (100) | 3 (75) | ||
| Not applicable c | 5 | 3 | 8 | ||
| Missing | 0 | 0 | 0 | ||
| Social distancing, colleagues | Rarely able to maintain | 0 (0) | 0 (0) | 0 (0) | |
| Sometimes able to maintain | 1 (50) | 0 (0) | 1 (25) | ||
| Mostly able to maintain | 1 (50) | 2 (100) | 3 (75) | ||
| Always able to maintain | 0 (0) | 0 (0) | 0 (0) | ||
| Missing | 5 | 3 | 8 | ||
| Social distancing, public | Rarely able to maintain | 1 (14) | 0 (0) | 1 (8) | |
| Sometimes able to maintain | 0 (0) | 1 (20) | 1 (8) | ||
| Mostly able to maintain | 6 (86) | 4 (80) | 10 (83) | ||
| Always able to maintain | 0 (0) | 0 (0) | 0 (0) | ||
| Missing | 0 | 0 | 0 | ||
| COVID-19 control measures not at work | Wear washable face mask/ face covering | Never | 2 (33) | 1 (25) | 3 (30) |
| <half the time | 1 (17) | 1 (25) | 2 (20) | ||
| >half the time | 0 (0) | 0 (0) | 0 (0) | ||
| Nearly all the time | 3 (50) | 2 (50) | 5 (50) | ||
| Missing | 1 | 1 | 2 | ||
| Wear surgical mask/ disposable mask | Never | 2 (29) | 1 (25) | 3 (27) | |
| < half the time | 0 (0) | 0 (0) | 0 (0) | ||
| > half the time | 1 (14) | 1 (25) | 2 (18) | ||
| Nearly all the time | 4 (57) | 2 (20) | 6 (55) | ||
| Missing | 0 | 1 | 1 | ||
| Wear face shield | Never | 5 (100) | 4 (100) | 9 (100) | |
| Missing | 2 | 1 | 3 |
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| COVID-19 control measures at work | COVID-19 training at work | No | 1 (14) | 0 (0) | 1 (8) |
| Yes | 6 (86) | 5 (100) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Hand washing or sanitizing facilities at work | No | 0 (0) | 0 (0) | 0 (0) | |
| Yes | 7 (100) | 5 (100) | 12 (100) | ||
| Missing | 0 | 0 | 0 | ||
| Good hand hygiene practice signage at work | No | 1 (14) | 0 (0) | 1 (8) | |
| Yes | 6 (86) | 5 (100) | 11 (92) | ||
| Missing | 0 | 0 | 0 | ||
| Frequency of hand washing/sanitizing in a day | Never | 0 (0) | 0 (0) | 0 (0) | |
| 1-10 times | 1 (17) | 1 (20) | 2 (18) | ||
| 11 + times | 5 (83) | 4 (80) | 9 (82) | ||
| Missing | 1 | 0 | 1 | ||
| Wear gloves | Never | 4 (57) | 5 (100) | 9 (75) | |
| < half the time | 2 (29) | 0 (0) | 2 (17) | ||
| > half the time | 0 (0) | 0 (0) | 0 (0) | ||
| Nearly all the time | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Wear washable face mask/ face covering | Never | 0 (0) | 3 (60) | 3 (25) | |
| < half the time | 1 (14) | 0 (0) | 1 (8) | ||
| > half the time | 2 (29) | 0 (0) | 2 (17) | ||
| Nearly all the time | 4 (57) | 2 (40) | 6 (50) | ||
| Missing | 0 | 0 | 0 | ||
| Wear surgical mask/ disposable mask | Never | 1 (14) | 3 (60) | 4 (33) | |
| < half the time | 0 (0) | 0 (0) | 0 (0) | ||
| > half the time | 1 (14) | 0 (0) | 1 (8) | ||
| Nearly all the time | 5 (71) | 2 (40) | 7 (58) | ||
| Missing | 0 | 0 | 0 | ||
| Wear FFP2 or FFP3 | Never | 6 (100) | 5 (100) | 11 (100) | |
| Missing | 1 | 0 | 1 | ||
| Wear face shield | Never | 6 (100) | 5 (100) | 11 (100) | |
| Missing | 1 | 0 | 1 | ||
| Divider, colleagues | No | 2 (100) | 1 (50) | 3 (75) | |
| Yes | 0 (0) | 1 (50) | 1 (25) | ||
| Not applicable c | 5 | 3 | 8 | ||
| Missing | 0 | 0 | 0 | ||
| Divider, public | No | 1 (50) | 0 (0) | 1 (25) | |
| Yes | 1 (50) | 2 (100) | 3 (75) | ||
| Not applicable c | 5 | 3 | 8 | ||
| Missing | 0 | 0 | 0 | ||
| Social distancing, colleagues | Rarely able to maintain | 0 (0) | 0 (0) | 0 (0) | |
| Sometimes able to maintain | 1 (50) | 0 (0) | 1 (25) | ||
| Mostly able to maintain | 1 (50) | 2 (100) | 3 (75) | ||
| Always able to maintain | 0 (0) | 0 (0) | 0 (0) | ||
| Missing | 5 | 3 | 8 | ||
| Social distancing, public | Rarely able to maintain | 1 (14) | 0 (0) | 1 (8) | |
| Sometimes able to maintain | 0 (0) | 1 (20) | 1 (8) | ||
| Mostly able to maintain | 6 (86) | 4 (80) | 10 (83) | ||
| Always able to maintain | 0 (0) | 0 (0) | 0 (0) | ||
| Missing | 0 | 0 | 0 | ||
| COVID-19 control measures not at work | Wear washable face mask/ face covering | Never | 2 (33) | 1 (25) | 3 (30) |
| <half the time | 1 (17) | 1 (25) | 2 (20) | ||
| >half the time | 0 (0) | 0 (0) | 0 (0) | ||
| Nearly all the time | 3 (50) | 2 (50) | 5 (50) | ||
| Missing | 1 | 1 | 2 | ||
| Wear surgical mask/ disposable mask | Never | 2 (29) | 1 (25) | 3 (27) | |
| < half the time | 0 (0) | 0 (0) | 0 (0) | ||
| > half the time | 1 (14) | 1 (25) | 2 (18) | ||
| Nearly all the time | 4 (57) | 2 (20) | 6 (55) | ||
| Missing | 0 | 1 | 1 | ||
| Wear face shield | Never | 5 (100) | 4 (100) | 9 (100) | |
| Missing | 2 | 1 | 3 |
aTwo out of seven controls did not undertake any testing as part of COVID-OUT and so are not confirmed negatives but classified as non-cases.
bOnly confirmed cases were identified. There were no suspected cases.
cNot applicable: participants did not report direct physical or close contract with co-workers or members of the public.
Work and non-work contact patterns reported by participants in the COVID-OUT study questionnaire
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Number of close contactsc | Household | None | 0 (0) | 1 (20) | 1 (8) |
| 1–2 | 2 (29) | 4 (80) | 6 (50) | ||
| 3–5 | 5 (71) | 0 (0) | 5 (42) | ||
| Missing | 0 | 0 | 0 | ||
| Work | None | 1 (14) | 2 (50) | 3 (27) | |
| 1–2 | 2 (29) | 0 (0) | 2 (18) | ||
| 3–5 | 0 (0) | 0 (0) | 0 (0) | ||
| 6–20 | 2 (29) | 2 (50) | 4 (36) | ||
| 21–100 | 2 (29) | 0 (0) | 2 (18) | ||
| Missing | 0 | 1 | 1 | ||
| Commute | None | 6 (86) | 4 (100) | 10 (91) | |
| 1–2 | 1 (14) | 0 (0) | 1 (9) | ||
| Missing | 0 | 1 | 1 | ||
| Social | None | 1 (17) | 2 (40) | 3 (27) | |
| 1–2 | 0 (0) | 0 (0) | 0 (0) | ||
| 3–5 | 1 (17) | 1 (20) | 2 (18) | ||
| 6–20 | 3 (50) | 2 (40) | 5 (45) | ||
| 21–100 | 1 (17) | 0 (0) | 1 (9) | ||
| Missing | 1 | 0 | 1 | ||
| Essential | None | 1 (14) | 1 (25) | 2 (18) | |
| 1–2 | 1 (14) | 1 (25) | 2 (18) | ||
| 3–5 | 0 (0) | 1 (25) | 1 (9) | ||
| 6–20 | 1 (14) | 1 (25) | 2 (18) | ||
| 21–100 | 4 (57) | 0 (0) | 4 (36) | ||
| Missing | 0 | 1 | 1 | ||
| Contact with a positive individual in the last 14 days | No | 1 (14) | 1 (20) | 2 (17) | |
| Yes, live with | 1 (14) | 1 (20) | 2 (17) | ||
| Yes, work with | 1 (14) | 1 (20) | 2 (17) | ||
| Yes, live and work with | 1 (14) | 0 (0) | 1 (8) | ||
| Yes, do not live and work with | 1 (14) | 1 (20) | 2 (17) | ||
| Not sure | 2 (29) | 1 (20) | 3 (25) | ||
| Long close contacts (>1 hour in same space) | Non-household | Never | 2 (29) | 3 (60) | 5 (42) |
| <1/day | 3 (43) | 0 (0) | 3 (25) | ||
| 1/day | 2 (29) | 0 (0) | 2 (17) | ||
| >1/day | 0 (0) | 2 (40) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Work | Never | 4 (57) | 3 (60) | 7 (58) | |
| <1/day | 2 (29) | 0 (0) | 2 (17) | ||
| 1/day | 0 (0) | 1 (20) | 1 (8) | ||
| >1/day | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Commute | Never | 6 (86) | 5 (100) | 11 (92) | |
| <1/day | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Social | Never | 3 (50) | 3 (60) | 6 (55) | |
| <1/day | 3 (50) | 1 (20) | 4 (36) | ||
| 1/day | 0 (0) | 1 (20) | 1 (9) | ||
| Missing | 1 | 0 | 1 | ||
| Essential | Never | 3 (43) | 2 (50) | 5 (45) | |
| <1/day | 2 (29) | 2 (50) | 4 (36) | ||
| 1/day | 0 (0) | 0 (0) | 0 (0) | ||
| >1/day | 2 (29) | 0 (0) | 2 (18) | ||
| Missing | 0 | 1 | 1 |
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Number of close contactsc | Household | None | 0 (0) | 1 (20) | 1 (8) |
| 1–2 | 2 (29) | 4 (80) | 6 (50) | ||
| 3–5 | 5 (71) | 0 (0) | 5 (42) | ||
| Missing | 0 | 0 | 0 | ||
| Work | None | 1 (14) | 2 (50) | 3 (27) | |
| 1–2 | 2 (29) | 0 (0) | 2 (18) | ||
| 3–5 | 0 (0) | 0 (0) | 0 (0) | ||
| 6–20 | 2 (29) | 2 (50) | 4 (36) | ||
| 21–100 | 2 (29) | 0 (0) | 2 (18) | ||
| Missing | 0 | 1 | 1 | ||
| Commute | None | 6 (86) | 4 (100) | 10 (91) | |
| 1–2 | 1 (14) | 0 (0) | 1 (9) | ||
| Missing | 0 | 1 | 1 | ||
| Social | None | 1 (17) | 2 (40) | 3 (27) | |
| 1–2 | 0 (0) | 0 (0) | 0 (0) | ||
| 3–5 | 1 (17) | 1 (20) | 2 (18) | ||
| 6–20 | 3 (50) | 2 (40) | 5 (45) | ||
| 21–100 | 1 (17) | 0 (0) | 1 (9) | ||
| Missing | 1 | 0 | 1 | ||
| Essential | None | 1 (14) | 1 (25) | 2 (18) | |
| 1–2 | 1 (14) | 1 (25) | 2 (18) | ||
| 3–5 | 0 (0) | 1 (25) | 1 (9) | ||
| 6–20 | 1 (14) | 1 (25) | 2 (18) | ||
| 21–100 | 4 (57) | 0 (0) | 4 (36) | ||
| Missing | 0 | 1 | 1 | ||
| Contact with a positive individual in the last 14 days | No | 1 (14) | 1 (20) | 2 (17) | |
| Yes, live with | 1 (14) | 1 (20) | 2 (17) | ||
| Yes, work with | 1 (14) | 1 (20) | 2 (17) | ||
| Yes, live and work with | 1 (14) | 0 (0) | 1 (8) | ||
| Yes, do not live and work with | 1 (14) | 1 (20) | 2 (17) | ||
| Not sure | 2 (29) | 1 (20) | 3 (25) | ||
| Long close contacts (>1 hour in same space) | Non-household | Never | 2 (29) | 3 (60) | 5 (42) |
| <1/day | 3 (43) | 0 (0) | 3 (25) | ||
| 1/day | 2 (29) | 0 (0) | 2 (17) | ||
| >1/day | 0 (0) | 2 (40) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Work | Never | 4 (57) | 3 (60) | 7 (58) | |
| <1/day | 2 (29) | 0 (0) | 2 (17) | ||
| 1/day | 0 (0) | 1 (20) | 1 (8) | ||
| >1/day | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Commute | Never | 6 (86) | 5 (100) | 11 (92) | |
| <1/day | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Social | Never | 3 (50) | 3 (60) | 6 (55) | |
| <1/day | 3 (50) | 1 (20) | 4 (36) | ||
| 1/day | 0 (0) | 1 (20) | 1 (9) | ||
| Missing | 1 | 0 | 1 | ||
| Essential | Never | 3 (43) | 2 (50) | 5 (45) | |
| <1/day | 2 (29) | 2 (50) | 4 (36) | ||
| 1/day | 0 (0) | 0 (0) | 0 (0) | ||
| >1/day | 2 (29) | 0 (0) | 2 (18) | ||
| Missing | 0 | 1 | 1 |
aTwo out of seven controls did not undertake any testing as part of COVID-OUT and so are not confirmed negatives but classified as non-cases.
bOnly confirmed cases were identified. There were no suspected cases.
c‘Close Contact’ defined as: typically spending more than 15 minutes within 2 m of someone.
Work and non-work contact patterns reported by participants in the COVID-OUT study questionnaire
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Number of close contactsc | Household | None | 0 (0) | 1 (20) | 1 (8) |
| 1–2 | 2 (29) | 4 (80) | 6 (50) | ||
| 3–5 | 5 (71) | 0 (0) | 5 (42) | ||
| Missing | 0 | 0 | 0 | ||
| Work | None | 1 (14) | 2 (50) | 3 (27) | |
| 1–2 | 2 (29) | 0 (0) | 2 (18) | ||
| 3–5 | 0 (0) | 0 (0) | 0 (0) | ||
| 6–20 | 2 (29) | 2 (50) | 4 (36) | ||
| 21–100 | 2 (29) | 0 (0) | 2 (18) | ||
| Missing | 0 | 1 | 1 | ||
| Commute | None | 6 (86) | 4 (100) | 10 (91) | |
| 1–2 | 1 (14) | 0 (0) | 1 (9) | ||
| Missing | 0 | 1 | 1 | ||
| Social | None | 1 (17) | 2 (40) | 3 (27) | |
| 1–2 | 0 (0) | 0 (0) | 0 (0) | ||
| 3–5 | 1 (17) | 1 (20) | 2 (18) | ||
| 6–20 | 3 (50) | 2 (40) | 5 (45) | ||
| 21–100 | 1 (17) | 0 (0) | 1 (9) | ||
| Missing | 1 | 0 | 1 | ||
| Essential | None | 1 (14) | 1 (25) | 2 (18) | |
| 1–2 | 1 (14) | 1 (25) | 2 (18) | ||
| 3–5 | 0 (0) | 1 (25) | 1 (9) | ||
| 6–20 | 1 (14) | 1 (25) | 2 (18) | ||
| 21–100 | 4 (57) | 0 (0) | 4 (36) | ||
| Missing | 0 | 1 | 1 | ||
| Contact with a positive individual in the last 14 days | No | 1 (14) | 1 (20) | 2 (17) | |
| Yes, live with | 1 (14) | 1 (20) | 2 (17) | ||
| Yes, work with | 1 (14) | 1 (20) | 2 (17) | ||
| Yes, live and work with | 1 (14) | 0 (0) | 1 (8) | ||
| Yes, do not live and work with | 1 (14) | 1 (20) | 2 (17) | ||
| Not sure | 2 (29) | 1 (20) | 3 (25) | ||
| Long close contacts (>1 hour in same space) | Non-household | Never | 2 (29) | 3 (60) | 5 (42) |
| <1/day | 3 (43) | 0 (0) | 3 (25) | ||
| 1/day | 2 (29) | 0 (0) | 2 (17) | ||
| >1/day | 0 (0) | 2 (40) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Work | Never | 4 (57) | 3 (60) | 7 (58) | |
| <1/day | 2 (29) | 0 (0) | 2 (17) | ||
| 1/day | 0 (0) | 1 (20) | 1 (8) | ||
| >1/day | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Commute | Never | 6 (86) | 5 (100) | 11 (92) | |
| <1/day | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Social | Never | 3 (50) | 3 (60) | 6 (55) | |
| <1/day | 3 (50) | 1 (20) | 4 (36) | ||
| 1/day | 0 (0) | 1 (20) | 1 (9) | ||
| Missing | 1 | 0 | 1 | ||
| Essential | Never | 3 (43) | 2 (50) | 5 (45) | |
| <1/day | 2 (29) | 2 (50) | 4 (36) | ||
| 1/day | 0 (0) | 0 (0) | 0 (0) | ||
| >1/day | 2 (29) | 0 (0) | 2 (18) | ||
| Missing | 0 | 1 | 1 |
| . | . | . | Non-casesa (n = 7), n (%) . | Confirmed casesb (n = 5), n (%) . | Total (n = 12), n (%) . |
|---|---|---|---|---|---|
| Number of close contactsc | Household | None | 0 (0) | 1 (20) | 1 (8) |
| 1–2 | 2 (29) | 4 (80) | 6 (50) | ||
| 3–5 | 5 (71) | 0 (0) | 5 (42) | ||
| Missing | 0 | 0 | 0 | ||
| Work | None | 1 (14) | 2 (50) | 3 (27) | |
| 1–2 | 2 (29) | 0 (0) | 2 (18) | ||
| 3–5 | 0 (0) | 0 (0) | 0 (0) | ||
| 6–20 | 2 (29) | 2 (50) | 4 (36) | ||
| 21–100 | 2 (29) | 0 (0) | 2 (18) | ||
| Missing | 0 | 1 | 1 | ||
| Commute | None | 6 (86) | 4 (100) | 10 (91) | |
| 1–2 | 1 (14) | 0 (0) | 1 (9) | ||
| Missing | 0 | 1 | 1 | ||
| Social | None | 1 (17) | 2 (40) | 3 (27) | |
| 1–2 | 0 (0) | 0 (0) | 0 (0) | ||
| 3–5 | 1 (17) | 1 (20) | 2 (18) | ||
| 6–20 | 3 (50) | 2 (40) | 5 (45) | ||
| 21–100 | 1 (17) | 0 (0) | 1 (9) | ||
| Missing | 1 | 0 | 1 | ||
| Essential | None | 1 (14) | 1 (25) | 2 (18) | |
| 1–2 | 1 (14) | 1 (25) | 2 (18) | ||
| 3–5 | 0 (0) | 1 (25) | 1 (9) | ||
| 6–20 | 1 (14) | 1 (25) | 2 (18) | ||
| 21–100 | 4 (57) | 0 (0) | 4 (36) | ||
| Missing | 0 | 1 | 1 | ||
| Contact with a positive individual in the last 14 days | No | 1 (14) | 1 (20) | 2 (17) | |
| Yes, live with | 1 (14) | 1 (20) | 2 (17) | ||
| Yes, work with | 1 (14) | 1 (20) | 2 (17) | ||
| Yes, live and work with | 1 (14) | 0 (0) | 1 (8) | ||
| Yes, do not live and work with | 1 (14) | 1 (20) | 2 (17) | ||
| Not sure | 2 (29) | 1 (20) | 3 (25) | ||
| Long close contacts (>1 hour in same space) | Non-household | Never | 2 (29) | 3 (60) | 5 (42) |
| <1/day | 3 (43) | 0 (0) | 3 (25) | ||
| 1/day | 2 (29) | 0 (0) | 2 (17) | ||
| >1/day | 0 (0) | 2 (40) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Work | Never | 4 (57) | 3 (60) | 7 (58) | |
| <1/day | 2 (29) | 0 (0) | 2 (17) | ||
| 1/day | 0 (0) | 1 (20) | 1 (8) | ||
| >1/day | 1 (14) | 1 (20) | 2 (17) | ||
| Missing | 0 | 0 | 0 | ||
| Commute | Never | 6 (86) | 5 (100) | 11 (92) | |
| <1/day | 1 (14) | 0 (0) | 1 (8) | ||
| Missing | 0 | 0 | 0 | ||
| Social | Never | 3 (50) | 3 (60) | 6 (55) | |
| <1/day | 3 (50) | 1 (20) | 4 (36) | ||
| 1/day | 0 (0) | 1 (20) | 1 (9) | ||
| Missing | 1 | 0 | 1 | ||
| Essential | Never | 3 (43) | 2 (50) | 5 (45) | |
| <1/day | 2 (29) | 2 (50) | 4 (36) | ||
| 1/day | 0 (0) | 0 (0) | 0 (0) | ||
| >1/day | 2 (29) | 0 (0) | 2 (18) | ||
| Missing | 0 | 1 | 1 |
aTwo out of seven controls did not undertake any testing as part of COVID-OUT and so are not confirmed negatives but classified as non-cases.
bOnly confirmed cases were identified. There were no suspected cases.
c‘Close Contact’ defined as: typically spending more than 15 minutes within 2 m of someone.
Discussion
In late August 2021, a public-facing office in England, with adherence to governmental COVID-19 control guidance and high vaccination coverage, experienced an outbreak of SARS-CoV-2 affecting 55% of the workforce. At the time of this outbreak, governmental guidance for workplaces in England prioritized policies for risk assessments, adequate ventilation, frequent cleaning, self-isolation and communication/training; however, social distancing and face-covering usage were no longer compulsory [13]. On 16th August 2021, 2 weeks before the outbreak, government guidance was amended, so fully vaccinated people did not need to self-isolate if they were identified as a close contact with someone with COVID-19 [13].
Despite existing COVID-19 control measures implemented by the organization, surface sampling identified potential deficiencies in routine disinfection procedures that informed targeted strengthening of infection control practices to support workplace reopening following the 2-week closure. Similar to other SARS-CoV-2 outbreak studies, relatively low-level contamination was identified even in locations associated with recent occupancy of symptomatic people [3,14–19]. No positive surface sample yielded a complete genome sequence suggesting degradation of the viral genome and a lack of transmission potential at the time of sampling. Similar investigations imply Ct values of less than 30 correlate with the presence of infectious virus [20].
The attack rate was higher among cleaners and security staff (75% and 67%, respectively) compared to office staff (50%); however, these differences were not statistically significant, probably due to the small numbers involved. Additionally, no cleaners or security staff participated in the study meaning it is difficult to interpret why attack rates were higher for workers in these job roles compared to others. However, it is noteworthy that the security office was identified as a site of enhanced viral contamination through surface sampling.
CO2 measurements indicated that, although largely by natural means, ventilation conformed with current guidance [8] and did not exceed 1500 ppm at any location sampled including the security office. However, since occupancy levels for the security office and security staff rotation patterns were modified upon reopening, the CO2 levels measured in the security office may not be representative of the levels at the time of the outbreak. Other areas were not affected by the change in working practices, so their CO2 levels should be indicative of those during the outbreak.
While vaccines remain effective for preventing severe COVID-19 illness and death, SARS-CoV-2 infections among fully vaccinated individuals in this outbreak are consistent with previous reports [21]. This reinforces the importance of workplaces using a layered SARS-CoV-2 transmission mitigation strategy prioritizing risk assessment-informed interventions, such as testing, social distancing, use of face coverings, adequate ventilation, and reduced occupancy levels even when vaccination uptake is high among the workforce.
The limitations of this study warrant consideration. Surface sampling and participant testing performed closer to the peak of cases could yield a more representative indication of viral contamination within the facility and facilitate more informative genomic sequencing and epidemiological assessment [22]. Although workplace transmission appears likely, given the clustering of cases in some areas and positive environmental sampling, we were unable to clarify chains of transmission and determine whether cases may have been independently introduced from community sources. It was also not possible to follow up with members of the public who may have visited the offices and had interviews with staff in the days preceding the outbreak to understand whether they too developed COVID-19 or indeed seeded the outbreak. Notably, the worker participation rate in COVID-OUT was 30%, with an underrepresentation of male workers as well as cleaning and security staff. The small sample size and potential for selection bias limit the ability to evaluate individual risk factors within this workplace. In addition, differences in behaviours reported by participants compared to those observed by the COVID-OUT team (e.g. wearing face coverings while at work), suggests that social desirability bias could be overestimating reported adherence to infection control measures.
Surface sampling techniques were used to identify areas of contamination that may be linked to control measure deficiencies. Additionally, the identification of viable virus and WGS may have provided evidence for fomite transmission, especially if these sequences could be linked with sequences from positive workers [23]. The absence of WGS in surface samples does not necessarily infer the absence of fomite transmission in this outbreak or other workplace outbreaks. Although identifying the contribution of fomite transmission of SARS-CoV-2 is complex [24], an association between hand/surface positive samples and transmission has been observed in households [25]. The utility of air sampling may also be considered in the future; however, such sampling has limited benefits in large environments and air sampling does not regularly detect viable virus in hospital rooms of patients with COVID-19 [26] likely due to both a small quantity of infectious virus in a large volume of air and the resulting dilution factor from downstream processing.
Maintaining core societal functions during future pandemics is of utmost importance, and thus the ability to rapidly investigate infectious disease outbreaks and implement data-informed transmission mitigation measures will be required. This is particularly relevant to workplaces with public-facing elements that have a dynamic population with an elevated risk of virus introduction and onward transmission. This study highlights the challenges involved in conducting a voluntary outbreak investigation such as COVID-OUT. Mechanisms to encourage workplaces to report potential outbreaks as early as practicable and engage with research studies, like the one presented here, should be prioritized to further our understanding of transmission and to provide safer work environments.
Overall, our findings highlight the need for evolving, site-specific risk assessments that adapt to changes in local community infection rates and recognize heterogeneity within a workplace in the risks associated with different workspaces (e.g. rooms with high occupancy) and worker roles (e.g. desk-based versus circulating staff). For public-facing workplaces, these assessments must inform suitable control measures to minimize potential close interactions of staff members with co-workers and visitors.
Funding
This work was funded by the Partnership for Research in Occupational, Transport and Environmental COVID Transmission COVID-19 National Core Study on Transmission and Environment and managed by the Health and Safety Executive on behalf of HM Government.
Acknowledgements
The authors wish to acknowledge Antony Spencer, Vince Sandys, Joan Cooke, Gary Dobbin, Hannah Higgins, Chris Keen, Alice Graham and Helen Collins for their efforts in recruitment and data collection supporting the COVID-OUT project. The authors further acknowledge the assistance of the UKHSA Genomics Team at UKHSA Porton Down for sequencing samples of interest from this study.
Competing interests
The contents of this paper, including any opinions and/or conclusions expressed, are those of the authors alone and do not necessarily reflect Health and Safety Executive or UK Health Security Agency policy.
Copyright
© Crown copyright (2023), Health and Safety Executive. This is an open access article distributed under the terms of the Open Government Licence v3.0, which permits re-use, distribution, reproduction, and adaptation, provided the original work is properly cited.



