-
PDF
- Split View
-
Views
-
Cite
Cite
Rasała Julia, Ciszewska Anna, Małgorzata Król, Mariusz Kusztal, Kościelska-Kasprzak Katarzyna, Andrzej Tukiendorf, Maciej Kanafa, Augustyniak-Bartosik Hanna, Oktawia Mazanowska, Krajewska Magdalena, MO162
IMPACT OF THE IMMUNOSUPPRESSIVE TREATMENT, X-RAY EXPOSITION AND RENAL PATHOLOGY ON OVARIAN RESERVE IN YOUNG WOMEN, Nephrology Dialysis Transplantation, Volume 36, Issue Supplement_1, May 2021, gfab092.0040, https://doi.org/10.1093/ndt/gfab092.0040Close - Share Icon Share
Abstract
Cyclophosphamide treatment and X-ray exposition in the area of the ovaries are proven to be the gonadotoxic factors in childbearing age women. Anti-Müllerian hormone (AMH) is regarded as a biomarker for ovarian reserve.
The study included 167 consecutive premenopausal women attending Nephrology Clinic who gave informed consent and met exclusion criteria (past ovarian surgical procedure, PCOS, eGFR <30ml/min, irregular menstrual cycles). Clinical (renal pathology, smoking, X-rays exposition, eGFR standardized MDRD4, contraceptives) and demographic characteristics, as well as previous and current immunosuppressive therapies were recorded. Serum AMH levels were measured by Beckman Coulter’s Gen II enzyme linked immunosorbent assay (ELISA) kit; AMH levels were classified as low or normal/above age-adjusted reference levels (published norms).
Statistical analysis included both regressive and non-regressive relationships between the studied clinical features. Due to the presumption of the remaining non-regression relationships between clinical factors, an original taxonomic method by Marczewski & Steinhaus was used instead of general linear modeling. Based on patient age, eGFR, renal pathology an ‘optimal’ segregation of patients was performed following the created classification tree (dendrogram).
Median age of the patients was 33 (range 18-44). Median AMH concentration was 2,66 ng/ml; AMH levels were classified in 64 females as low (median 1,015) and in 103 as normal/above age-adjusted reference (median 4,04). Sixty one patients were treated with cyclophosphamide in the past and 45 underwent kidney transplantation. 92 women suffered from glomerulonephritis, 44 from lupus nephritis, 12 from interstitial kidney disease, 5 from ADPKD and 14 from other kidney diseases.
Age, eGFR, pregnancies in the past as well as being the kidney transplant recipient were the coefficients strongly correlated with AMH level. Presence of lupus nephritis was correlated with lower levels of AMH in comparison to other renal diseases and in contrast to cyclophosphamide. X-ray exposition measured in cumulative lifetime dose was not correlated with AMH levels.
Although previous researchers suggested cyclophosphamide to be the strong gonadotoxic factor, our statistical analysis approach shows that lupus as the disease often treated with cyclophosphamide may be the lowering ovarian reserve factor itself. Further studies on this subject are still necessary.
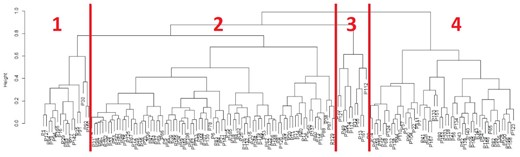
Classification tree (dendrogram) of patients with clusters
Characteristics of patients in clusters (mean±st. dev. and %) with p-values (<0.05)
| Clinical factor . | Cluster1 . | Cluster2 . | Cluster3 . | Cluster4 . | p-value . |
|---|---|---|---|---|---|
| Age | 30.6±2.5 | 37.8±3.9 | 33.9±6.6 | 23.2±3.8 | 0.0000 |
| Kidney transplant | 71% | 39% | 45% | 19% | 0.0012 |
| eGFR (MDRD4) | 38.4±10.1 | 66.7±21.8 | 9.0±3.3 | 91.8±23.7 | 0.0000 |
| Renal pathology (lupus vs. other) | 12% | 38% | 9% | 15% | 0.0051 |
| Born children | 0.2±0.4 | 0.8±0.8 | 0.8±1.4 | 0.3±0.7 | 0.0010 |
| AMH | 3.22±2.16 | 2.37±1.95 | 3.51±3.37 | 4.66±3.16 | 0.0000 |
| Clinical factor . | Cluster1 . | Cluster2 . | Cluster3 . | Cluster4 . | p-value . |
|---|---|---|---|---|---|
| Age | 30.6±2.5 | 37.8±3.9 | 33.9±6.6 | 23.2±3.8 | 0.0000 |
| Kidney transplant | 71% | 39% | 45% | 19% | 0.0012 |
| eGFR (MDRD4) | 38.4±10.1 | 66.7±21.8 | 9.0±3.3 | 91.8±23.7 | 0.0000 |
| Renal pathology (lupus vs. other) | 12% | 38% | 9% | 15% | 0.0051 |
| Born children | 0.2±0.4 | 0.8±0.8 | 0.8±1.4 | 0.3±0.7 | 0.0010 |
| AMH | 3.22±2.16 | 2.37±1.95 | 3.51±3.37 | 4.66±3.16 | 0.0000 |
Characteristics of patients in clusters (mean±st. dev. and %) with p-values (<0.05)
| Clinical factor . | Cluster1 . | Cluster2 . | Cluster3 . | Cluster4 . | p-value . |
|---|---|---|---|---|---|
| Age | 30.6±2.5 | 37.8±3.9 | 33.9±6.6 | 23.2±3.8 | 0.0000 |
| Kidney transplant | 71% | 39% | 45% | 19% | 0.0012 |
| eGFR (MDRD4) | 38.4±10.1 | 66.7±21.8 | 9.0±3.3 | 91.8±23.7 | 0.0000 |
| Renal pathology (lupus vs. other) | 12% | 38% | 9% | 15% | 0.0051 |
| Born children | 0.2±0.4 | 0.8±0.8 | 0.8±1.4 | 0.3±0.7 | 0.0010 |
| AMH | 3.22±2.16 | 2.37±1.95 | 3.51±3.37 | 4.66±3.16 | 0.0000 |
| Clinical factor . | Cluster1 . | Cluster2 . | Cluster3 . | Cluster4 . | p-value . |
|---|---|---|---|---|---|
| Age | 30.6±2.5 | 37.8±3.9 | 33.9±6.6 | 23.2±3.8 | 0.0000 |
| Kidney transplant | 71% | 39% | 45% | 19% | 0.0012 |
| eGFR (MDRD4) | 38.4±10.1 | 66.7±21.8 | 9.0±3.3 | 91.8±23.7 | 0.0000 |
| Renal pathology (lupus vs. other) | 12% | 38% | 9% | 15% | 0.0051 |
| Born children | 0.2±0.4 | 0.8±0.8 | 0.8±1.4 | 0.3±0.7 | 0.0010 |
| AMH | 3.22±2.16 | 2.37±1.95 | 3.51±3.37 | 4.66±3.16 | 0.0000 |
- polycystic ovary syndrome
- pregnancy
- smoking
- kidney diseases
- renal transplantation
- informed consent
- diagnostic radiologic examination
- roentgen rays
- glomerulonephritis
- immunosuppressive agents
- enzyme-linked immunosorbent assay
- systemic lupus erythematosus
- cyclophosphamide
- discoid lupus erythematosus
- hormones
- biological markers
- child
- contraceptive agents
- demography
- lupus nephritis
- nephrology
- polycystic kidney, autosomal dominant
- premenopause
- signs and symptoms
- trees (plant)
- kidney
- lupus erythematosus
- ovary
- pathology
- mullerian-inhibiting hormone
- menstrual cycle, irregular
- ovarian surgery
- impact
- ovarian reserve





Comments