Abstract
Background
There is widespread recognition that research will be more impactful if it arises from partnerships between patients and researchers, but evidence on best practice for achieving this remains limited.
Methods
We convened workshops in three Australian cities involving 105 patients/caregivers and 43 clinicians/researchers. In facilitated breakout groups, participants discussed principles and strategies for effective patient involvement in chronic kidney disease research. Transcripts were analysed thematically
Results
Five major themes emerged. ‘Respecting consumer expertise and commitment’ involved valuing unique and diverse experiential knowledge, clarifying expectations and responsibilities, equipping for meaningful involvement and keeping patients ‘in the loop’. ‘Attuning to individual context’ required a preference-based multipronged approach to engagement, reducing the burden of involvement and being sensitive to the patient journey. ‘Harnessing existing relationships and infrastructure’ meant partnering with trusted clinicians, increasing research exposure in clinical settings, mentoring patient to patient and extending reach through established networks. ‘Developing a coordinated approach’ enabled power in the collective and united voice, a systematic approach for equitable inclusion and streamlining access to opportunities and trustworthy information. ‘Fostering a patient-centred culture’ encompassed building a community, facilitating knowledge exchange and translation, empowering health ownership, providing an opportunity to give back and cultivating trust through transparency.
Conclusions
Partnering with patients in research requires respect and recognition of their unique, diverse and complementary experiential expertise. Establishing a supportive, respectful research culture, responding to their individual context, coordinating existing infrastructure and centralizing the flow of information may facilitate patient involvement as active partners in research.
INTRODUCTION
Involving patients in research has emerged as a policy imperative to align research with patient priorities and thereby maximize the impact of research on practice and policy [1, 2]. This has spurred widespread efforts by global organizations to involve patients as active partners contributing across the research process from setting the research agenda through to design, dissemination and implementation [3–7].
Patient involvement can improve the relevance, quality and translation of research for improved outcomes [1, 7–11]. For example, patient involvement in the design of a clinical trial in cancer increased recruitment and retention rates [12–14]. Patient involvement in the Outcome Measures in Rheumatology initiative for the past 2 decades has led to increased focus and reporting of patient-centred outcomes such as fatigue and sleep [15, 16]. In nephrology, patient perspectives have ensured that the scope of clinical practice guidelines for polycystic kidney disease, renal biopsy and infectious diseases in patients on haemodialysis cover patient-relevant topics such as education and psychosocial support [17–19].
Patient involvement in research is particularly relevant in chronic kidney disease (CKD) as patients face a lifelong condition with mortality rates up to 100 times higher than the general population and impaired quality of life [20–22]. Yet there remains a substantial mismatch between the priorities of patients and research [10, 11]. A recent review indicated that 80% of clinical research did not address the top 10 research priorities identified by patients on or nearing dialysis [23, 24], and outcomes considered critically important to patients, such as fatigue and cardiovascular disease, are infrequently reported in trials [21, 25, 26].
Major steps have been taken towards empowering patients as partners in research [27, 28]. The Patient-Centered Outcomes Research Institute (PCORI) in the USA and INVOLVE in the UK were established to support patient-centred research and patient involvement across the research cycle [13, 29, 30]. The Kidney Health Initiative (a partnership between the American Society of Nephrology and the US Food and Drug Administration) has formed a Patient and Family Partnership Council, providing patients a voice to influence the development of drugs, treatments, devices and clinical trials [31]. Recently the Standardized Outcomes in Nephrology initiative was launched to bring together patients, caregivers and health professional to establish consensus-based core outcome sets for clinical trials [32].
However, there are barriers to involving patients in research [7, 33]. Patients may feel disempowered, uncertain about their role and overwhelmed by the burden of their disease and treatment [7, 34]. In the research community, there is scepticism about the value and impact of patient involvement and concerns about diminishing scientific rigour and the ‘representativeness’ of patient partners [1, 3, 35, 36]. Time and funding have also been identified as barriers [3, 4, 35]. Thus researchers remain uncertain about how to effectively communicate opportunities for involvement, provide necessary training and support or plan for meaningful involvement [35].
Systematic reviews [2, 28, 37–41] of methods for patient involvement focus on the stages (e.g. designing a trial) and roles (e.g. steering committee member) of patient involvement [7, 11, 27, 28, 33, 35, 36, 42, 43], yet sparse data exist to inform best practice on ‘how’ to engage and involve patients in research. While frameworks for involving patients in research exist [3, 6, 44–46], it can be difficult to translate these into tangible recommendations for practice. Further compounding this, and despite minimal evaluation of patient involvement initiatives [11], it is becoming known that practices previously viewed as empowering (e.g. one patient representative on a panel) are now viewed as disempowering and tokenistic by patients [35, 46].
Improved reporting and evaluation of effective methods for engagement and involvement, in conjunction with more data from the patient perspective, are needed to understand the potential for patients to impact and shape the future of health research [2, 3]. As part of the Better Evidence and Translation in Chronic Kidney Disease (BEAT-CKD) research programme, we aimed to understand and describe patient and health professional perspectives about patient involvement in research in CKD and to identify practical solutions to engage and involve patients across the spectrum of BEAT-CKD research initiatives. In this report we use the term ‘patient’ to refer to all persons with lived experience of CKD unless otherwise specified. Further definitions can be found in Box 1.
WORKSHOPS
Context and overview
BEAT-CKD is a collaborative research programme that aims to improve the lives of people with CKD by generating high-quality research evidence to inform health care decisions made by patients, health professionals and policymakers [47]. The programme supports research and translation platforms—Caring for Australasians with Renal Impairment clinical practice guidelines [48], Australasian Kidney Trials Network [49], Australian and New Zealand Dialysis and Transplant Registry (ANZDATA) [50] and Cochrane Kidney and Transplant [51]—and the scope of the research activity is global. To inform a patient involvement strategy, we convened three workshops with patients and health professionals about principles and strategies for patient involvement in research in kidney disease.
Attendees and contributors
The BEAT-CKD Management Committee and Kidney Health Australia invited patients and health professionals to attend through their networks and social media. In total, 105 people with lived experience, including 70 patients (CKD Stages 1–5 and non–dialysis dependent, on dialysis, with a kidney transplant), 28 caregivers (caregivers, parents and family members) and 7 who did not indicate their role and 43 health professionals (nephrologists, researchers, dieticians, nurses) attended the workshop.
Workshops
We conducted one workshop in Sydney, Adelaide and Brisbane, from August to December 2017. Following presentations about research, attendees participated in 1-h breakout discussions with 6–10 patients and health professionals per group to encourage the exchange of diverse perspectives (total 17 groups). Each group had a facilitator. Question guides were informed by literature on patient involvement in research (Supplementary data, File S1) to elicit perspectives on why and how patients want to be involved in research [2, 5, 13, 29, 40, 44, 46]. Shortly after the last workshop all participants received a brief narrative summary of the workshops (Supplementary data, File S2). The discussions were audio recorded and transcribed verbatim. T.G. coded the transcripts using HyperRESEARCH software (ResearchWare, Randolph, MA, USA) for qualitative data management [52]. Concepts relating to participants’ perspectives on patient involvement in research were identified and grouped into themes, which were reviewed by the facilitators and investigators to ensure all data were captured in the themes. All attendees and contributors were invited to provide feedback on the draft workshop report by e-mail, within a 2-week time frame. Comments and feedback were addressed and integrated into the final manuscript.
Summary of the discussions
The discussions across all workshops were synthesized into five themes: respecting patient expertise and commitment, attuning to individual context, harnessing existing relationships and infrastructure, developing a coordinated approach and fostering a patient-centred culture. The respective subthemes are described in the following section with reference to the patient or health professional group where relevant. Selected illustrative quotations are provided in Table 1. Figure 1 depicts a summary of the themes. Suggestions for practical approaches to involve patients in research are shown in Table 2.
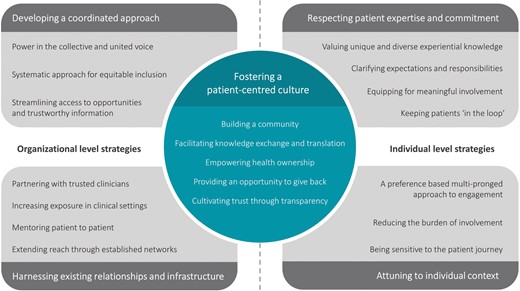
FIGURE 1
Strategies and principles for patient involvement in research. Workshop attendees identified strategies for patient involvement that could be addressed at an individual level (i.e. respecting patient expertise and commitment and attuning to individual context). However, some strategies may require collaborative efforts at organizational levels to instigate meaningful change (i.e. harnessing existing relationships and infrastructure and developing a coordinated approach). Underpinning these strategies were principles grounded in fostering a patient-centred culture and included building a community of patients and researchers for research partnership where both parties can learn and benefit from one another.
| Theme
. | Illustrative quotations
. |
|---|
| Respecting patient expertise and commitment |
| Valuing unique and diverse experiential knowledge | Things like sleep or whether someone can go to work or someone’s quality of life or their mental well-being we’re just starting to measure. Patients probably could have told us 50 years ago that we should be measuring them, but they weren’t asked. (Female, Sydney, Health Professional) You do bring in knowledge that they don’t have. The reason people ask the wrong question is because they don’t have the experience of living with it. (Male, Sydney, Patient) It puts a human focus on it. It’s important to know who you’re working for, not just a group or a consumer but actual people and faces and lives and stories. (Female, Sydney, Health Professional)
|
| Clarifying expectations and responsibilities | One of the things that happens poorly is the explanation upfront as to why you’re doing what you’re doing, and what the potential benefits are, just the clarity of that. Because research can be kind of mystical, but it can also be really hands on and grounded if you explain it correctly. (Female, Adelaide, Health Professional) Maybe in the communication it could be about what it would mean in terms of the time that it would take to be involved? What the impact to our lives as a patient would be. (Female, Brisbane, Patient)
|
| Equipping for meaningful involvement | I was horrified to hear that gentleman say they had a consumer involved in one of the studies, and they pulled out because it was too technical. Was that a matter of we won’t replace the consumer because it’s too hard for consumers or was it just the wrong consumer? You simplify or train, or if it is going to be at that level then you select those consumers. Either way, don’t just go ‘it didn’t work’. (Female, Sydney, Patient) They’re talking about a separate group that would inform the other groups, just a consumer group, because you don’t want to get the ratio wrong either where you just have a whole bunch of doctors and then maybe one or two [patients]. (Female, Sydney, Patient) When you get more time to think about it, rather than closed in a room and put on the spot. (Female, Sydney, Patient)
|
| Keeping patients ‘in the loop’ | We’ve got to tell you about research that’s going on generally in the world. We probably have the duty to relay that. We currently don’t do that at all. And the duty to tell people about what’s going on, studies you can join, and then communicating the results of the work that you were engaged in as a person. I think we haven’t done that well. We’ve done it a bit through the KHA website. You probably don’t even know that. There should be a consumer summary. (Female, Brisbane, Health Professional) If I was going to contribute to things, I’d like there to be some way where you got to hear an end result or just progress. That’s a frustration for me. If there was some way to be connected to some sort of feedback that you don’t need a medical degree to understand. (Male, Sydney, Patient)
|
| Attuning to individual context |
| Preference-based, multipronged approach to engagement | I love the idea of a document that’s patient-written for patients about what the research is about. What’s going to work is a movie and one sheet of paper that summarizes what the benefit to me or the benefit to the kidney community in general is. (Female, Brisbane, Patient) It makes complete sense that this gentleman here would like to have a booklet or a pamphlet, whereas my daughter who’s 18 and just been diagnosed with a polycystic kidney disease is going to look at everything online, when she’s ready or when she’s interested. She’s not interested in the piece of paper. Being able to deliver that useful information in different forms. (Female, Adelaide, Patient)
|
| Reducing the burden of involvement | I used an annual leave day today. I don’t care, but if it was a regular, well I’m saving my annual leave for my transplant. (Male, Sydney, Patient) It’s the flexibility that will be the key. People need to be able to choose the level of engagement that they want to do. (Male, Sydney, Patient)
|
| Being sensitive to the patient journey | The sicker I became, the more vague I became. Your attention span is really affected. You can’t concentrate at all, focus. Whether that can be addressed in keeping notes very basic or something like that, rather than complicating. (Male, Sydney, Patient) They’ve got to have some sort of knowledge of when they hit you up for it [involvement]. Not when you’re at your worst. Also, if you’re on dialysis, you want to do it at home. You don’t want to sit there for another hour. You’ve chewed up enough of your day, you’ve lost enough of your life. (Female, Brisbane, Patient)
|
| Harnessing existing relationships and infrastructure |
| Partnering with trusted clinicians | Every kidney patient goes and sees a nephrologist or a kidney doctor, the kidney specialist can play a bigger role than they do about talking to the patient about research. (Male, Brisbane, Patient) It needs to come from the nephrologist first, even just to say there’s a website out there, or we’ve got this organization if you’re interested in research, because I think a lot of people probably don’t even think that there’s research going on. The idea needs to be put into their head first, that there is research going on in the area, and then they can pursue it if they are interested. (Female, Adelaide, Patient)
|
| Increasing research exposure in clinical settings | When I go to a hospital, you normally see a poster wall about the papers. I think there’s a volume of material already prepared, ready to be told to an audience, and you probably need to have some downscaling of the language in them to make them more suitable to the patients, and then you could put that in a newsletter. (Male, Brisbane, Patient) There’s a TV in the waiting area. Instead of running commercials, you just run your ads for research. (Male, Brisbane, Patient)
|
| Mentoring patient to patient | I found [the patient’s] talk very helpful, because he’s been through it. And he was able to talk to me about how it works. The more you hear about the process, the more you start to think, yeah, I could probably cope with that. (Male, Sydney, Patient) It’s just that if you do the patient to patient interactions though, you’ll have to mediate it really carefully. My experience with a lot of them is that they turn into misery pits. (Female, Sydney, Patient)
|
| Extending reach through established networks | If we could piggyback onto diabetes research, I think that might raise a lot of public awareness. (Female, Adelaide, Patient) I went to the hospital, they were set up in the foyer, kidney health week, we’ll take your blood pressure. I said people, you’re in the wrong spot. People who come into the hospital already know they’ve got high blood pressure. You should be outside at Bunnings [Hardware Store]. That’s exactly right. They said that’s not a bad idea. Where do you reckon they’ll be in March this year? Sitting in the hospital. (Male, Brisbane, Patient)
|
| Developing a coordinated approach |
| Power in the collective and united voice | There are so many not for profit organizations or bodies, but there doesn’t seem to be one umbrella organization that’s driving all the communications to the consumer, to the patient, so everyone knows where to look. I think everyone’s trying to do the right thing. There are so many of them that it’s diluting the power of the communication. (Male, Adelaide, Patient) If it’s not central or under one banner, you get competing priorities between organizations. (Male, Sydney, Health Professional) If you all get together, you’re all there for one common cause, but being separate, it’s not really helping anyone. (Female, Sydney, Patient)
|
| Systematic approach for equitable inclusion | You’re not increasing your pool if you keep on asking the same people over and over again, there are new patients being added all the time. There’s nothing upfront, a survey or whatever, to say are you interested, do you want to participate in this sort of thing? (Male, Brisbane, Patient) I know they have difficulty finding people to put themselves forward. In some cases it’s always the same person who puts themselves forward, and they may not necessarily be the right person, but because they’re on this treadmill of being on all these different things, then the true reflection of somebody with a passion to be on it doesn’t get on it. (Female, Adelaide, Patient) Why not? Why can’t we just have a kidney disease database? (Male, Brisbane, Patient) We really need to get a database of people and see whether they actually want to be contacted. (Male, Brisbane, Patient)
|
| Streamlining access to opportunities and trustworthy information | If you had a one stop shop. If there could be a tailored site where kidney-specific things could be put – perhaps research results, or trials or whatever. Something that ordinary people can understand, because we’re not all medically inclined. (Female, Brisbane, Patient) Almost like a dating site. You know what I mean. A Tinder trial site. (Female, Adelaide, Patient) There should be a central hub where you can find results, you can find organizations you can join, you can find research you can be involved in. (Male, Sydney, Patient)
|
| Fostering a patient-centred culture |
| Building a community | Our approach to communication becomes sanitized. The coffee group idea gives a sense of a relaxed atmosphere. Just having a group like that, where it’s just a general friendship group, and you’re not there for a purpose, you’re there just because you got commonalities. (Male, Adelaide, Health Professional) It’s about building a community first, is that right? (Female, Adelaide, Health Professional) Take the questions to the people where you know your groups are on the day, instead of you trying to say can you listen to us? (Female, Brisbane, Patient)
|
| Facilitating knowledge exchange and translation | Gaining information empowers you and that helps you to make decisions about how you can involve or improve your care. Gaining information gives you insight as to what type of research you might want to be interested in or involved in, and what capacity that you want to be. (Female, Brisbane, Health Professional) That’s really what we want [researchers to speak informally at patient meetings]. We had a transplant lady come and talk to us all about what they do with transplants. We would all come around, that was just fantastic. (Female, Adelaide, Patient)
|
| Empowering health ownership | We need to explain what’s in it for the patient, what’s the opportunity that it might present, what’s the potential benefit for the future, and why is it important for patients to get involved. If we make the messaging all speared towards why the consumer’s part of this is so important, we’ll get much better uptake. It’s spinning it around and not talking about the clinical stuff. It’s talking about the patient’s reasons of why it’s important. (Female, Brisbane, Health Professional) I believe in the power that we have as consumers to change what’s important to us, and make sure that we understand what’s going on in the research community. (Female, Brisbane, Patient)
|
| Providing an opportunity to give back | The way that I feel about it is that I got so much out from all the people, the doctors and the nurses who looked after me over the years. It’s been fantastic, really. I feel that anything I can contribute, I’d be very happy to have an opportunity to do anything. (Male, Sydney, Patient) Why would someone want to participate, it’s because they want to help other people. (Male, Adelaide, Patient)
|
| Cultivating trust through transparency | I just thought research was a waste of money up until today, because you never heard of an outcome. (Male, Adelaide, Patient) There’s sort of a them and us mentality. Most of these researchers, they’re in there as good guys. They have some bad habits, we all do, but they’re in there to help us, and we have to respect that as part of the process. Some of them are [there to get a degree], but it’s actually good to engage younger researchers and develop the culture of research as we move on in time. (Male, Sydney, Patient)
|
| Theme
. | Illustrative quotations
. |
|---|
| Respecting patient expertise and commitment |
| Valuing unique and diverse experiential knowledge | Things like sleep or whether someone can go to work or someone’s quality of life or their mental well-being we’re just starting to measure. Patients probably could have told us 50 years ago that we should be measuring them, but they weren’t asked. (Female, Sydney, Health Professional) You do bring in knowledge that they don’t have. The reason people ask the wrong question is because they don’t have the experience of living with it. (Male, Sydney, Patient) It puts a human focus on it. It’s important to know who you’re working for, not just a group or a consumer but actual people and faces and lives and stories. (Female, Sydney, Health Professional)
|
| Clarifying expectations and responsibilities | One of the things that happens poorly is the explanation upfront as to why you’re doing what you’re doing, and what the potential benefits are, just the clarity of that. Because research can be kind of mystical, but it can also be really hands on and grounded if you explain it correctly. (Female, Adelaide, Health Professional) Maybe in the communication it could be about what it would mean in terms of the time that it would take to be involved? What the impact to our lives as a patient would be. (Female, Brisbane, Patient)
|
| Equipping for meaningful involvement | I was horrified to hear that gentleman say they had a consumer involved in one of the studies, and they pulled out because it was too technical. Was that a matter of we won’t replace the consumer because it’s too hard for consumers or was it just the wrong consumer? You simplify or train, or if it is going to be at that level then you select those consumers. Either way, don’t just go ‘it didn’t work’. (Female, Sydney, Patient) They’re talking about a separate group that would inform the other groups, just a consumer group, because you don’t want to get the ratio wrong either where you just have a whole bunch of doctors and then maybe one or two [patients]. (Female, Sydney, Patient) When you get more time to think about it, rather than closed in a room and put on the spot. (Female, Sydney, Patient)
|
| Keeping patients ‘in the loop’ | We’ve got to tell you about research that’s going on generally in the world. We probably have the duty to relay that. We currently don’t do that at all. And the duty to tell people about what’s going on, studies you can join, and then communicating the results of the work that you were engaged in as a person. I think we haven’t done that well. We’ve done it a bit through the KHA website. You probably don’t even know that. There should be a consumer summary. (Female, Brisbane, Health Professional) If I was going to contribute to things, I’d like there to be some way where you got to hear an end result or just progress. That’s a frustration for me. If there was some way to be connected to some sort of feedback that you don’t need a medical degree to understand. (Male, Sydney, Patient)
|
| Attuning to individual context |
| Preference-based, multipronged approach to engagement | I love the idea of a document that’s patient-written for patients about what the research is about. What’s going to work is a movie and one sheet of paper that summarizes what the benefit to me or the benefit to the kidney community in general is. (Female, Brisbane, Patient) It makes complete sense that this gentleman here would like to have a booklet or a pamphlet, whereas my daughter who’s 18 and just been diagnosed with a polycystic kidney disease is going to look at everything online, when she’s ready or when she’s interested. She’s not interested in the piece of paper. Being able to deliver that useful information in different forms. (Female, Adelaide, Patient)
|
| Reducing the burden of involvement | I used an annual leave day today. I don’t care, but if it was a regular, well I’m saving my annual leave for my transplant. (Male, Sydney, Patient) It’s the flexibility that will be the key. People need to be able to choose the level of engagement that they want to do. (Male, Sydney, Patient)
|
| Being sensitive to the patient journey | The sicker I became, the more vague I became. Your attention span is really affected. You can’t concentrate at all, focus. Whether that can be addressed in keeping notes very basic or something like that, rather than complicating. (Male, Sydney, Patient) They’ve got to have some sort of knowledge of when they hit you up for it [involvement]. Not when you’re at your worst. Also, if you’re on dialysis, you want to do it at home. You don’t want to sit there for another hour. You’ve chewed up enough of your day, you’ve lost enough of your life. (Female, Brisbane, Patient)
|
| Harnessing existing relationships and infrastructure |
| Partnering with trusted clinicians | Every kidney patient goes and sees a nephrologist or a kidney doctor, the kidney specialist can play a bigger role than they do about talking to the patient about research. (Male, Brisbane, Patient) It needs to come from the nephrologist first, even just to say there’s a website out there, or we’ve got this organization if you’re interested in research, because I think a lot of people probably don’t even think that there’s research going on. The idea needs to be put into their head first, that there is research going on in the area, and then they can pursue it if they are interested. (Female, Adelaide, Patient)
|
| Increasing research exposure in clinical settings | When I go to a hospital, you normally see a poster wall about the papers. I think there’s a volume of material already prepared, ready to be told to an audience, and you probably need to have some downscaling of the language in them to make them more suitable to the patients, and then you could put that in a newsletter. (Male, Brisbane, Patient) There’s a TV in the waiting area. Instead of running commercials, you just run your ads for research. (Male, Brisbane, Patient)
|
| Mentoring patient to patient | I found [the patient’s] talk very helpful, because he’s been through it. And he was able to talk to me about how it works. The more you hear about the process, the more you start to think, yeah, I could probably cope with that. (Male, Sydney, Patient) It’s just that if you do the patient to patient interactions though, you’ll have to mediate it really carefully. My experience with a lot of them is that they turn into misery pits. (Female, Sydney, Patient)
|
| Extending reach through established networks | If we could piggyback onto diabetes research, I think that might raise a lot of public awareness. (Female, Adelaide, Patient) I went to the hospital, they were set up in the foyer, kidney health week, we’ll take your blood pressure. I said people, you’re in the wrong spot. People who come into the hospital already know they’ve got high blood pressure. You should be outside at Bunnings [Hardware Store]. That’s exactly right. They said that’s not a bad idea. Where do you reckon they’ll be in March this year? Sitting in the hospital. (Male, Brisbane, Patient)
|
| Developing a coordinated approach |
| Power in the collective and united voice | There are so many not for profit organizations or bodies, but there doesn’t seem to be one umbrella organization that’s driving all the communications to the consumer, to the patient, so everyone knows where to look. I think everyone’s trying to do the right thing. There are so many of them that it’s diluting the power of the communication. (Male, Adelaide, Patient) If it’s not central or under one banner, you get competing priorities between organizations. (Male, Sydney, Health Professional) If you all get together, you’re all there for one common cause, but being separate, it’s not really helping anyone. (Female, Sydney, Patient)
|
| Systematic approach for equitable inclusion | You’re not increasing your pool if you keep on asking the same people over and over again, there are new patients being added all the time. There’s nothing upfront, a survey or whatever, to say are you interested, do you want to participate in this sort of thing? (Male, Brisbane, Patient) I know they have difficulty finding people to put themselves forward. In some cases it’s always the same person who puts themselves forward, and they may not necessarily be the right person, but because they’re on this treadmill of being on all these different things, then the true reflection of somebody with a passion to be on it doesn’t get on it. (Female, Adelaide, Patient) Why not? Why can’t we just have a kidney disease database? (Male, Brisbane, Patient) We really need to get a database of people and see whether they actually want to be contacted. (Male, Brisbane, Patient)
|
| Streamlining access to opportunities and trustworthy information | If you had a one stop shop. If there could be a tailored site where kidney-specific things could be put – perhaps research results, or trials or whatever. Something that ordinary people can understand, because we’re not all medically inclined. (Female, Brisbane, Patient) Almost like a dating site. You know what I mean. A Tinder trial site. (Female, Adelaide, Patient) There should be a central hub where you can find results, you can find organizations you can join, you can find research you can be involved in. (Male, Sydney, Patient)
|
| Fostering a patient-centred culture |
| Building a community | Our approach to communication becomes sanitized. The coffee group idea gives a sense of a relaxed atmosphere. Just having a group like that, where it’s just a general friendship group, and you’re not there for a purpose, you’re there just because you got commonalities. (Male, Adelaide, Health Professional) It’s about building a community first, is that right? (Female, Adelaide, Health Professional) Take the questions to the people where you know your groups are on the day, instead of you trying to say can you listen to us? (Female, Brisbane, Patient)
|
| Facilitating knowledge exchange and translation | Gaining information empowers you and that helps you to make decisions about how you can involve or improve your care. Gaining information gives you insight as to what type of research you might want to be interested in or involved in, and what capacity that you want to be. (Female, Brisbane, Health Professional) That’s really what we want [researchers to speak informally at patient meetings]. We had a transplant lady come and talk to us all about what they do with transplants. We would all come around, that was just fantastic. (Female, Adelaide, Patient)
|
| Empowering health ownership | We need to explain what’s in it for the patient, what’s the opportunity that it might present, what’s the potential benefit for the future, and why is it important for patients to get involved. If we make the messaging all speared towards why the consumer’s part of this is so important, we’ll get much better uptake. It’s spinning it around and not talking about the clinical stuff. It’s talking about the patient’s reasons of why it’s important. (Female, Brisbane, Health Professional) I believe in the power that we have as consumers to change what’s important to us, and make sure that we understand what’s going on in the research community. (Female, Brisbane, Patient)
|
| Providing an opportunity to give back | The way that I feel about it is that I got so much out from all the people, the doctors and the nurses who looked after me over the years. It’s been fantastic, really. I feel that anything I can contribute, I’d be very happy to have an opportunity to do anything. (Male, Sydney, Patient) Why would someone want to participate, it’s because they want to help other people. (Male, Adelaide, Patient)
|
| Cultivating trust through transparency | I just thought research was a waste of money up until today, because you never heard of an outcome. (Male, Adelaide, Patient) There’s sort of a them and us mentality. Most of these researchers, they’re in there as good guys. They have some bad habits, we all do, but they’re in there to help us, and we have to respect that as part of the process. Some of them are [there to get a degree], but it’s actually good to engage younger researchers and develop the culture of research as we move on in time. (Male, Sydney, Patient)
|
| Theme
. | Illustrative quotations
. |
|---|
| Respecting patient expertise and commitment |
| Valuing unique and diverse experiential knowledge | Things like sleep or whether someone can go to work or someone’s quality of life or their mental well-being we’re just starting to measure. Patients probably could have told us 50 years ago that we should be measuring them, but they weren’t asked. (Female, Sydney, Health Professional) You do bring in knowledge that they don’t have. The reason people ask the wrong question is because they don’t have the experience of living with it. (Male, Sydney, Patient) It puts a human focus on it. It’s important to know who you’re working for, not just a group or a consumer but actual people and faces and lives and stories. (Female, Sydney, Health Professional)
|
| Clarifying expectations and responsibilities | One of the things that happens poorly is the explanation upfront as to why you’re doing what you’re doing, and what the potential benefits are, just the clarity of that. Because research can be kind of mystical, but it can also be really hands on and grounded if you explain it correctly. (Female, Adelaide, Health Professional) Maybe in the communication it could be about what it would mean in terms of the time that it would take to be involved? What the impact to our lives as a patient would be. (Female, Brisbane, Patient)
|
| Equipping for meaningful involvement | I was horrified to hear that gentleman say they had a consumer involved in one of the studies, and they pulled out because it was too technical. Was that a matter of we won’t replace the consumer because it’s too hard for consumers or was it just the wrong consumer? You simplify or train, or if it is going to be at that level then you select those consumers. Either way, don’t just go ‘it didn’t work’. (Female, Sydney, Patient) They’re talking about a separate group that would inform the other groups, just a consumer group, because you don’t want to get the ratio wrong either where you just have a whole bunch of doctors and then maybe one or two [patients]. (Female, Sydney, Patient) When you get more time to think about it, rather than closed in a room and put on the spot. (Female, Sydney, Patient)
|
| Keeping patients ‘in the loop’ | We’ve got to tell you about research that’s going on generally in the world. We probably have the duty to relay that. We currently don’t do that at all. And the duty to tell people about what’s going on, studies you can join, and then communicating the results of the work that you were engaged in as a person. I think we haven’t done that well. We’ve done it a bit through the KHA website. You probably don’t even know that. There should be a consumer summary. (Female, Brisbane, Health Professional) If I was going to contribute to things, I’d like there to be some way where you got to hear an end result or just progress. That’s a frustration for me. If there was some way to be connected to some sort of feedback that you don’t need a medical degree to understand. (Male, Sydney, Patient)
|
| Attuning to individual context |
| Preference-based, multipronged approach to engagement | I love the idea of a document that’s patient-written for patients about what the research is about. What’s going to work is a movie and one sheet of paper that summarizes what the benefit to me or the benefit to the kidney community in general is. (Female, Brisbane, Patient) It makes complete sense that this gentleman here would like to have a booklet or a pamphlet, whereas my daughter who’s 18 and just been diagnosed with a polycystic kidney disease is going to look at everything online, when she’s ready or when she’s interested. She’s not interested in the piece of paper. Being able to deliver that useful information in different forms. (Female, Adelaide, Patient)
|
| Reducing the burden of involvement | I used an annual leave day today. I don’t care, but if it was a regular, well I’m saving my annual leave for my transplant. (Male, Sydney, Patient) It’s the flexibility that will be the key. People need to be able to choose the level of engagement that they want to do. (Male, Sydney, Patient)
|
| Being sensitive to the patient journey | The sicker I became, the more vague I became. Your attention span is really affected. You can’t concentrate at all, focus. Whether that can be addressed in keeping notes very basic or something like that, rather than complicating. (Male, Sydney, Patient) They’ve got to have some sort of knowledge of when they hit you up for it [involvement]. Not when you’re at your worst. Also, if you’re on dialysis, you want to do it at home. You don’t want to sit there for another hour. You’ve chewed up enough of your day, you’ve lost enough of your life. (Female, Brisbane, Patient)
|
| Harnessing existing relationships and infrastructure |
| Partnering with trusted clinicians | Every kidney patient goes and sees a nephrologist or a kidney doctor, the kidney specialist can play a bigger role than they do about talking to the patient about research. (Male, Brisbane, Patient) It needs to come from the nephrologist first, even just to say there’s a website out there, or we’ve got this organization if you’re interested in research, because I think a lot of people probably don’t even think that there’s research going on. The idea needs to be put into their head first, that there is research going on in the area, and then they can pursue it if they are interested. (Female, Adelaide, Patient)
|
| Increasing research exposure in clinical settings | When I go to a hospital, you normally see a poster wall about the papers. I think there’s a volume of material already prepared, ready to be told to an audience, and you probably need to have some downscaling of the language in them to make them more suitable to the patients, and then you could put that in a newsletter. (Male, Brisbane, Patient) There’s a TV in the waiting area. Instead of running commercials, you just run your ads for research. (Male, Brisbane, Patient)
|
| Mentoring patient to patient | I found [the patient’s] talk very helpful, because he’s been through it. And he was able to talk to me about how it works. The more you hear about the process, the more you start to think, yeah, I could probably cope with that. (Male, Sydney, Patient) It’s just that if you do the patient to patient interactions though, you’ll have to mediate it really carefully. My experience with a lot of them is that they turn into misery pits. (Female, Sydney, Patient)
|
| Extending reach through established networks | If we could piggyback onto diabetes research, I think that might raise a lot of public awareness. (Female, Adelaide, Patient) I went to the hospital, they were set up in the foyer, kidney health week, we’ll take your blood pressure. I said people, you’re in the wrong spot. People who come into the hospital already know they’ve got high blood pressure. You should be outside at Bunnings [Hardware Store]. That’s exactly right. They said that’s not a bad idea. Where do you reckon they’ll be in March this year? Sitting in the hospital. (Male, Brisbane, Patient)
|
| Developing a coordinated approach |
| Power in the collective and united voice | There are so many not for profit organizations or bodies, but there doesn’t seem to be one umbrella organization that’s driving all the communications to the consumer, to the patient, so everyone knows where to look. I think everyone’s trying to do the right thing. There are so many of them that it’s diluting the power of the communication. (Male, Adelaide, Patient) If it’s not central or under one banner, you get competing priorities between organizations. (Male, Sydney, Health Professional) If you all get together, you’re all there for one common cause, but being separate, it’s not really helping anyone. (Female, Sydney, Patient)
|
| Systematic approach for equitable inclusion | You’re not increasing your pool if you keep on asking the same people over and over again, there are new patients being added all the time. There’s nothing upfront, a survey or whatever, to say are you interested, do you want to participate in this sort of thing? (Male, Brisbane, Patient) I know they have difficulty finding people to put themselves forward. In some cases it’s always the same person who puts themselves forward, and they may not necessarily be the right person, but because they’re on this treadmill of being on all these different things, then the true reflection of somebody with a passion to be on it doesn’t get on it. (Female, Adelaide, Patient) Why not? Why can’t we just have a kidney disease database? (Male, Brisbane, Patient) We really need to get a database of people and see whether they actually want to be contacted. (Male, Brisbane, Patient)
|
| Streamlining access to opportunities and trustworthy information | If you had a one stop shop. If there could be a tailored site where kidney-specific things could be put – perhaps research results, or trials or whatever. Something that ordinary people can understand, because we’re not all medically inclined. (Female, Brisbane, Patient) Almost like a dating site. You know what I mean. A Tinder trial site. (Female, Adelaide, Patient) There should be a central hub where you can find results, you can find organizations you can join, you can find research you can be involved in. (Male, Sydney, Patient)
|
| Fostering a patient-centred culture |
| Building a community | Our approach to communication becomes sanitized. The coffee group idea gives a sense of a relaxed atmosphere. Just having a group like that, where it’s just a general friendship group, and you’re not there for a purpose, you’re there just because you got commonalities. (Male, Adelaide, Health Professional) It’s about building a community first, is that right? (Female, Adelaide, Health Professional) Take the questions to the people where you know your groups are on the day, instead of you trying to say can you listen to us? (Female, Brisbane, Patient)
|
| Facilitating knowledge exchange and translation | Gaining information empowers you and that helps you to make decisions about how you can involve or improve your care. Gaining information gives you insight as to what type of research you might want to be interested in or involved in, and what capacity that you want to be. (Female, Brisbane, Health Professional) That’s really what we want [researchers to speak informally at patient meetings]. We had a transplant lady come and talk to us all about what they do with transplants. We would all come around, that was just fantastic. (Female, Adelaide, Patient)
|
| Empowering health ownership | We need to explain what’s in it for the patient, what’s the opportunity that it might present, what’s the potential benefit for the future, and why is it important for patients to get involved. If we make the messaging all speared towards why the consumer’s part of this is so important, we’ll get much better uptake. It’s spinning it around and not talking about the clinical stuff. It’s talking about the patient’s reasons of why it’s important. (Female, Brisbane, Health Professional) I believe in the power that we have as consumers to change what’s important to us, and make sure that we understand what’s going on in the research community. (Female, Brisbane, Patient)
|
| Providing an opportunity to give back | The way that I feel about it is that I got so much out from all the people, the doctors and the nurses who looked after me over the years. It’s been fantastic, really. I feel that anything I can contribute, I’d be very happy to have an opportunity to do anything. (Male, Sydney, Patient) Why would someone want to participate, it’s because they want to help other people. (Male, Adelaide, Patient)
|
| Cultivating trust through transparency | I just thought research was a waste of money up until today, because you never heard of an outcome. (Male, Adelaide, Patient) There’s sort of a them and us mentality. Most of these researchers, they’re in there as good guys. They have some bad habits, we all do, but they’re in there to help us, and we have to respect that as part of the process. Some of them are [there to get a degree], but it’s actually good to engage younger researchers and develop the culture of research as we move on in time. (Male, Sydney, Patient)
|
| Theme
. | Illustrative quotations
. |
|---|
| Respecting patient expertise and commitment |
| Valuing unique and diverse experiential knowledge | Things like sleep or whether someone can go to work or someone’s quality of life or their mental well-being we’re just starting to measure. Patients probably could have told us 50 years ago that we should be measuring them, but they weren’t asked. (Female, Sydney, Health Professional) You do bring in knowledge that they don’t have. The reason people ask the wrong question is because they don’t have the experience of living with it. (Male, Sydney, Patient) It puts a human focus on it. It’s important to know who you’re working for, not just a group or a consumer but actual people and faces and lives and stories. (Female, Sydney, Health Professional)
|
| Clarifying expectations and responsibilities | One of the things that happens poorly is the explanation upfront as to why you’re doing what you’re doing, and what the potential benefits are, just the clarity of that. Because research can be kind of mystical, but it can also be really hands on and grounded if you explain it correctly. (Female, Adelaide, Health Professional) Maybe in the communication it could be about what it would mean in terms of the time that it would take to be involved? What the impact to our lives as a patient would be. (Female, Brisbane, Patient)
|
| Equipping for meaningful involvement | I was horrified to hear that gentleman say they had a consumer involved in one of the studies, and they pulled out because it was too technical. Was that a matter of we won’t replace the consumer because it’s too hard for consumers or was it just the wrong consumer? You simplify or train, or if it is going to be at that level then you select those consumers. Either way, don’t just go ‘it didn’t work’. (Female, Sydney, Patient) They’re talking about a separate group that would inform the other groups, just a consumer group, because you don’t want to get the ratio wrong either where you just have a whole bunch of doctors and then maybe one or two [patients]. (Female, Sydney, Patient) When you get more time to think about it, rather than closed in a room and put on the spot. (Female, Sydney, Patient)
|
| Keeping patients ‘in the loop’ | We’ve got to tell you about research that’s going on generally in the world. We probably have the duty to relay that. We currently don’t do that at all. And the duty to tell people about what’s going on, studies you can join, and then communicating the results of the work that you were engaged in as a person. I think we haven’t done that well. We’ve done it a bit through the KHA website. You probably don’t even know that. There should be a consumer summary. (Female, Brisbane, Health Professional) If I was going to contribute to things, I’d like there to be some way where you got to hear an end result or just progress. That’s a frustration for me. If there was some way to be connected to some sort of feedback that you don’t need a medical degree to understand. (Male, Sydney, Patient)
|
| Attuning to individual context |
| Preference-based, multipronged approach to engagement | I love the idea of a document that’s patient-written for patients about what the research is about. What’s going to work is a movie and one sheet of paper that summarizes what the benefit to me or the benefit to the kidney community in general is. (Female, Brisbane, Patient) It makes complete sense that this gentleman here would like to have a booklet or a pamphlet, whereas my daughter who’s 18 and just been diagnosed with a polycystic kidney disease is going to look at everything online, when she’s ready or when she’s interested. She’s not interested in the piece of paper. Being able to deliver that useful information in different forms. (Female, Adelaide, Patient)
|
| Reducing the burden of involvement | I used an annual leave day today. I don’t care, but if it was a regular, well I’m saving my annual leave for my transplant. (Male, Sydney, Patient) It’s the flexibility that will be the key. People need to be able to choose the level of engagement that they want to do. (Male, Sydney, Patient)
|
| Being sensitive to the patient journey | The sicker I became, the more vague I became. Your attention span is really affected. You can’t concentrate at all, focus. Whether that can be addressed in keeping notes very basic or something like that, rather than complicating. (Male, Sydney, Patient) They’ve got to have some sort of knowledge of when they hit you up for it [involvement]. Not when you’re at your worst. Also, if you’re on dialysis, you want to do it at home. You don’t want to sit there for another hour. You’ve chewed up enough of your day, you’ve lost enough of your life. (Female, Brisbane, Patient)
|
| Harnessing existing relationships and infrastructure |
| Partnering with trusted clinicians | Every kidney patient goes and sees a nephrologist or a kidney doctor, the kidney specialist can play a bigger role than they do about talking to the patient about research. (Male, Brisbane, Patient) It needs to come from the nephrologist first, even just to say there’s a website out there, or we’ve got this organization if you’re interested in research, because I think a lot of people probably don’t even think that there’s research going on. The idea needs to be put into their head first, that there is research going on in the area, and then they can pursue it if they are interested. (Female, Adelaide, Patient)
|
| Increasing research exposure in clinical settings | When I go to a hospital, you normally see a poster wall about the papers. I think there’s a volume of material already prepared, ready to be told to an audience, and you probably need to have some downscaling of the language in them to make them more suitable to the patients, and then you could put that in a newsletter. (Male, Brisbane, Patient) There’s a TV in the waiting area. Instead of running commercials, you just run your ads for research. (Male, Brisbane, Patient)
|
| Mentoring patient to patient | I found [the patient’s] talk very helpful, because he’s been through it. And he was able to talk to me about how it works. The more you hear about the process, the more you start to think, yeah, I could probably cope with that. (Male, Sydney, Patient) It’s just that if you do the patient to patient interactions though, you’ll have to mediate it really carefully. My experience with a lot of them is that they turn into misery pits. (Female, Sydney, Patient)
|
| Extending reach through established networks | If we could piggyback onto diabetes research, I think that might raise a lot of public awareness. (Female, Adelaide, Patient) I went to the hospital, they were set up in the foyer, kidney health week, we’ll take your blood pressure. I said people, you’re in the wrong spot. People who come into the hospital already know they’ve got high blood pressure. You should be outside at Bunnings [Hardware Store]. That’s exactly right. They said that’s not a bad idea. Where do you reckon they’ll be in March this year? Sitting in the hospital. (Male, Brisbane, Patient)
|
| Developing a coordinated approach |
| Power in the collective and united voice | There are so many not for profit organizations or bodies, but there doesn’t seem to be one umbrella organization that’s driving all the communications to the consumer, to the patient, so everyone knows where to look. I think everyone’s trying to do the right thing. There are so many of them that it’s diluting the power of the communication. (Male, Adelaide, Patient) If it’s not central or under one banner, you get competing priorities between organizations. (Male, Sydney, Health Professional) If you all get together, you’re all there for one common cause, but being separate, it’s not really helping anyone. (Female, Sydney, Patient)
|
| Systematic approach for equitable inclusion | You’re not increasing your pool if you keep on asking the same people over and over again, there are new patients being added all the time. There’s nothing upfront, a survey or whatever, to say are you interested, do you want to participate in this sort of thing? (Male, Brisbane, Patient) I know they have difficulty finding people to put themselves forward. In some cases it’s always the same person who puts themselves forward, and they may not necessarily be the right person, but because they’re on this treadmill of being on all these different things, then the true reflection of somebody with a passion to be on it doesn’t get on it. (Female, Adelaide, Patient) Why not? Why can’t we just have a kidney disease database? (Male, Brisbane, Patient) We really need to get a database of people and see whether they actually want to be contacted. (Male, Brisbane, Patient)
|
| Streamlining access to opportunities and trustworthy information | If you had a one stop shop. If there could be a tailored site where kidney-specific things could be put – perhaps research results, or trials or whatever. Something that ordinary people can understand, because we’re not all medically inclined. (Female, Brisbane, Patient) Almost like a dating site. You know what I mean. A Tinder trial site. (Female, Adelaide, Patient) There should be a central hub where you can find results, you can find organizations you can join, you can find research you can be involved in. (Male, Sydney, Patient)
|
| Fostering a patient-centred culture |
| Building a community | Our approach to communication becomes sanitized. The coffee group idea gives a sense of a relaxed atmosphere. Just having a group like that, where it’s just a general friendship group, and you’re not there for a purpose, you’re there just because you got commonalities. (Male, Adelaide, Health Professional) It’s about building a community first, is that right? (Female, Adelaide, Health Professional) Take the questions to the people where you know your groups are on the day, instead of you trying to say can you listen to us? (Female, Brisbane, Patient)
|
| Facilitating knowledge exchange and translation | Gaining information empowers you and that helps you to make decisions about how you can involve or improve your care. Gaining information gives you insight as to what type of research you might want to be interested in or involved in, and what capacity that you want to be. (Female, Brisbane, Health Professional) That’s really what we want [researchers to speak informally at patient meetings]. We had a transplant lady come and talk to us all about what they do with transplants. We would all come around, that was just fantastic. (Female, Adelaide, Patient)
|
| Empowering health ownership | We need to explain what’s in it for the patient, what’s the opportunity that it might present, what’s the potential benefit for the future, and why is it important for patients to get involved. If we make the messaging all speared towards why the consumer’s part of this is so important, we’ll get much better uptake. It’s spinning it around and not talking about the clinical stuff. It’s talking about the patient’s reasons of why it’s important. (Female, Brisbane, Health Professional) I believe in the power that we have as consumers to change what’s important to us, and make sure that we understand what’s going on in the research community. (Female, Brisbane, Patient)
|
| Providing an opportunity to give back | The way that I feel about it is that I got so much out from all the people, the doctors and the nurses who looked after me over the years. It’s been fantastic, really. I feel that anything I can contribute, I’d be very happy to have an opportunity to do anything. (Male, Sydney, Patient) Why would someone want to participate, it’s because they want to help other people. (Male, Adelaide, Patient)
|
| Cultivating trust through transparency | I just thought research was a waste of money up until today, because you never heard of an outcome. (Male, Adelaide, Patient) There’s sort of a them and us mentality. Most of these researchers, they’re in there as good guys. They have some bad habits, we all do, but they’re in there to help us, and we have to respect that as part of the process. Some of them are [there to get a degree], but it’s actually good to engage younger researchers and develop the culture of research as we move on in time. (Male, Sydney, Patient)
|
Table 2Suggestions for effective engagement and involvement
| Domain
. | Considerations and suggestions from workshop participants for patient/caregiver involvement
. |
|---|
| Engagement and selection | Plan and budget for patient/caregiver involvement at the earliest stage of the research project. Clearly define role (i.e. level of involvement, stage of research, specific responsibilities), required commitment (i.e. time, financial, emotional) and expected impact (i.e. directly on a specific project, on the wider kidney community agenda or expected benefits for future generations) with ‘terms of reference’ document, allow time for reflection and questions. Roles may vary by project and/or research stage and can range from consultation to partnership. Consider the potential benefits for the patient/caregiver and clearly explain these (e.g. developing new skills, greater understanding of disease, contributing to research for future generations). Consider the cross section of patients/caregivers involved (e.g. urban versus rural, experienced versus new, older versus younger, well versus unwell) and structure projects to enable broad participation (e.g. join from remote locations, schedule meetings outside of business hours). Select patients/caregivers for whom your project is most relevant and whose expertise is best suited (e.g. target peritoneal dialysis patients for projects/interventions designed for peritoneal dialysis patients). Use engagement methods preferred by target population (e.g. phone/letter for older patients, social media for younger patients, in clinic/centre for haemodialysis patients). Advertise opportunities in waiting rooms (e.g. videos, pamphlets, posters). Work with physicians and nurses to engage patients/caregivers. Ask patients to suggest new patients to be involved; consider having patient mentors to induct new patients into research projects.
|
| Training, support and education | Provide education for patient/caregiver partners (e.g. current research activities, kidney disease). Provide training in research methods (e.g. study design, academic writing, critical appraisal, recruitment). Consider psychological, mental and physical demands of involvement: ensure environment is accessible and can accommodate for patient needs (e.g. place to do peritoneal dialysis, elevator access); use communication strategies and simple language to reduce cognitive burden of involvement on patients; have referrals available in case of distress (e.g. social worker); offer flexible meeting options (e.g. videoconferencing, regular breaks, time for questions); andwhere possible, embed opportunities into routine care (e.g. transplant clinics). Financial reimbursement/aid may assist patients/caregiver to become involved: consider financial burden/sacrifice of involvement on patients/caregivers, and at a minimum, cover costs incurred (e.g. travel expenses, time off work); consider implementing a ‘jury duty’ system to reimburse patients/caregivers for their time; consider budgeting for paid patient/caregiver research partner position/s.
|
| Empowering the patient voice | Appoint more than one patient representative on a steering committee/working group. Consider forming a diverse patient advisory group to oversee research activities. Produce induction packets with relevant materials (e.g. glossary of terms/acronyms, background reading, helpful resources, videos). Use lay language where possible and explain technical/medical terminology when necessary. Allow time before or after meetings for patients/caregivers to consider their responses/opinions (e.g. send meeting agenda with topics to be discussed, follow-up post-meeting). Involve across all stages of the research; however, early involvement, before the grant stage, allows patient/caregiver contributions to be more easily integrated. Partner patient/caregiver with experienced research ‘buddy’ whom they can reach out to with any problems, questions or suggestions.
|
| Connection and community | Establish and expand a database to contact patients. Consider building a patient-dedicated research showcase portal/hub with lay language summaries of research and impacts, and opportunities for involvement to connect patients with researchers with potential for patients/caregivers to customize their profiles (interests, experience, CKD stage, etc.). Keep communications open with regular updates via newsletters, e-mails, texts and/or social media, even if no formal results are available. Collaborate with patient/caregiver and community organizations (e.g. present at patient support groups) to raise awareness of kidney disease, encourage knowledge exchange and advertise opportunities for involvement. Establish relationships with other research organizations to pool resources for patient/caregiver engagement to mitigate competing priorities, leverage collective goals and streamline communications to patients/caregivers. Disseminate research findings in plain language and informal settings to patients/caregivers to educate them about the outcomes and impact of research (including the impact of their involvement), build trust with the research community and encourage future involvement.
|
| Domain
. | Considerations and suggestions from workshop participants for patient/caregiver involvement
. |
|---|
| Engagement and selection | Plan and budget for patient/caregiver involvement at the earliest stage of the research project. Clearly define role (i.e. level of involvement, stage of research, specific responsibilities), required commitment (i.e. time, financial, emotional) and expected impact (i.e. directly on a specific project, on the wider kidney community agenda or expected benefits for future generations) with ‘terms of reference’ document, allow time for reflection and questions. Roles may vary by project and/or research stage and can range from consultation to partnership. Consider the potential benefits for the patient/caregiver and clearly explain these (e.g. developing new skills, greater understanding of disease, contributing to research for future generations). Consider the cross section of patients/caregivers involved (e.g. urban versus rural, experienced versus new, older versus younger, well versus unwell) and structure projects to enable broad participation (e.g. join from remote locations, schedule meetings outside of business hours). Select patients/caregivers for whom your project is most relevant and whose expertise is best suited (e.g. target peritoneal dialysis patients for projects/interventions designed for peritoneal dialysis patients). Use engagement methods preferred by target population (e.g. phone/letter for older patients, social media for younger patients, in clinic/centre for haemodialysis patients). Advertise opportunities in waiting rooms (e.g. videos, pamphlets, posters). Work with physicians and nurses to engage patients/caregivers. Ask patients to suggest new patients to be involved; consider having patient mentors to induct new patients into research projects.
|
| Training, support and education | Provide education for patient/caregiver partners (e.g. current research activities, kidney disease). Provide training in research methods (e.g. study design, academic writing, critical appraisal, recruitment). Consider psychological, mental and physical demands of involvement: ensure environment is accessible and can accommodate for patient needs (e.g. place to do peritoneal dialysis, elevator access); use communication strategies and simple language to reduce cognitive burden of involvement on patients; have referrals available in case of distress (e.g. social worker); offer flexible meeting options (e.g. videoconferencing, regular breaks, time for questions); andwhere possible, embed opportunities into routine care (e.g. transplant clinics). Financial reimbursement/aid may assist patients/caregiver to become involved: consider financial burden/sacrifice of involvement on patients/caregivers, and at a minimum, cover costs incurred (e.g. travel expenses, time off work); consider implementing a ‘jury duty’ system to reimburse patients/caregivers for their time; consider budgeting for paid patient/caregiver research partner position/s.
|
| Empowering the patient voice | Appoint more than one patient representative on a steering committee/working group. Consider forming a diverse patient advisory group to oversee research activities. Produce induction packets with relevant materials (e.g. glossary of terms/acronyms, background reading, helpful resources, videos). Use lay language where possible and explain technical/medical terminology when necessary. Allow time before or after meetings for patients/caregivers to consider their responses/opinions (e.g. send meeting agenda with topics to be discussed, follow-up post-meeting). Involve across all stages of the research; however, early involvement, before the grant stage, allows patient/caregiver contributions to be more easily integrated. Partner patient/caregiver with experienced research ‘buddy’ whom they can reach out to with any problems, questions or suggestions.
|
| Connection and community | Establish and expand a database to contact patients. Consider building a patient-dedicated research showcase portal/hub with lay language summaries of research and impacts, and opportunities for involvement to connect patients with researchers with potential for patients/caregivers to customize their profiles (interests, experience, CKD stage, etc.). Keep communications open with regular updates via newsletters, e-mails, texts and/or social media, even if no formal results are available. Collaborate with patient/caregiver and community organizations (e.g. present at patient support groups) to raise awareness of kidney disease, encourage knowledge exchange and advertise opportunities for involvement. Establish relationships with other research organizations to pool resources for patient/caregiver engagement to mitigate competing priorities, leverage collective goals and streamline communications to patients/caregivers. Disseminate research findings in plain language and informal settings to patients/caregivers to educate them about the outcomes and impact of research (including the impact of their involvement), build trust with the research community and encourage future involvement.
|
Table 2Suggestions for effective engagement and involvement
| Domain
. | Considerations and suggestions from workshop participants for patient/caregiver involvement
. |
|---|
| Engagement and selection | Plan and budget for patient/caregiver involvement at the earliest stage of the research project. Clearly define role (i.e. level of involvement, stage of research, specific responsibilities), required commitment (i.e. time, financial, emotional) and expected impact (i.e. directly on a specific project, on the wider kidney community agenda or expected benefits for future generations) with ‘terms of reference’ document, allow time for reflection and questions. Roles may vary by project and/or research stage and can range from consultation to partnership. Consider the potential benefits for the patient/caregiver and clearly explain these (e.g. developing new skills, greater understanding of disease, contributing to research for future generations). Consider the cross section of patients/caregivers involved (e.g. urban versus rural, experienced versus new, older versus younger, well versus unwell) and structure projects to enable broad participation (e.g. join from remote locations, schedule meetings outside of business hours). Select patients/caregivers for whom your project is most relevant and whose expertise is best suited (e.g. target peritoneal dialysis patients for projects/interventions designed for peritoneal dialysis patients). Use engagement methods preferred by target population (e.g. phone/letter for older patients, social media for younger patients, in clinic/centre for haemodialysis patients). Advertise opportunities in waiting rooms (e.g. videos, pamphlets, posters). Work with physicians and nurses to engage patients/caregivers. Ask patients to suggest new patients to be involved; consider having patient mentors to induct new patients into research projects.
|
| Training, support and education | Provide education for patient/caregiver partners (e.g. current research activities, kidney disease). Provide training in research methods (e.g. study design, academic writing, critical appraisal, recruitment). Consider psychological, mental and physical demands of involvement: ensure environment is accessible and can accommodate for patient needs (e.g. place to do peritoneal dialysis, elevator access); use communication strategies and simple language to reduce cognitive burden of involvement on patients; have referrals available in case of distress (e.g. social worker); offer flexible meeting options (e.g. videoconferencing, regular breaks, time for questions); andwhere possible, embed opportunities into routine care (e.g. transplant clinics). Financial reimbursement/aid may assist patients/caregiver to become involved: consider financial burden/sacrifice of involvement on patients/caregivers, and at a minimum, cover costs incurred (e.g. travel expenses, time off work); consider implementing a ‘jury duty’ system to reimburse patients/caregivers for their time; consider budgeting for paid patient/caregiver research partner position/s.
|
| Empowering the patient voice | Appoint more than one patient representative on a steering committee/working group. Consider forming a diverse patient advisory group to oversee research activities. Produce induction packets with relevant materials (e.g. glossary of terms/acronyms, background reading, helpful resources, videos). Use lay language where possible and explain technical/medical terminology when necessary. Allow time before or after meetings for patients/caregivers to consider their responses/opinions (e.g. send meeting agenda with topics to be discussed, follow-up post-meeting). Involve across all stages of the research; however, early involvement, before the grant stage, allows patient/caregiver contributions to be more easily integrated. Partner patient/caregiver with experienced research ‘buddy’ whom they can reach out to with any problems, questions or suggestions.
|
| Connection and community | Establish and expand a database to contact patients. Consider building a patient-dedicated research showcase portal/hub with lay language summaries of research and impacts, and opportunities for involvement to connect patients with researchers with potential for patients/caregivers to customize their profiles (interests, experience, CKD stage, etc.). Keep communications open with regular updates via newsletters, e-mails, texts and/or social media, even if no formal results are available. Collaborate with patient/caregiver and community organizations (e.g. present at patient support groups) to raise awareness of kidney disease, encourage knowledge exchange and advertise opportunities for involvement. Establish relationships with other research organizations to pool resources for patient/caregiver engagement to mitigate competing priorities, leverage collective goals and streamline communications to patients/caregivers. Disseminate research findings in plain language and informal settings to patients/caregivers to educate them about the outcomes and impact of research (including the impact of their involvement), build trust with the research community and encourage future involvement.
|
| Domain
. | Considerations and suggestions from workshop participants for patient/caregiver involvement
. |
|---|
| Engagement and selection | Plan and budget for patient/caregiver involvement at the earliest stage of the research project. Clearly define role (i.e. level of involvement, stage of research, specific responsibilities), required commitment (i.e. time, financial, emotional) and expected impact (i.e. directly on a specific project, on the wider kidney community agenda or expected benefits for future generations) with ‘terms of reference’ document, allow time for reflection and questions. Roles may vary by project and/or research stage and can range from consultation to partnership. Consider the potential benefits for the patient/caregiver and clearly explain these (e.g. developing new skills, greater understanding of disease, contributing to research for future generations). Consider the cross section of patients/caregivers involved (e.g. urban versus rural, experienced versus new, older versus younger, well versus unwell) and structure projects to enable broad participation (e.g. join from remote locations, schedule meetings outside of business hours). Select patients/caregivers for whom your project is most relevant and whose expertise is best suited (e.g. target peritoneal dialysis patients for projects/interventions designed for peritoneal dialysis patients). Use engagement methods preferred by target population (e.g. phone/letter for older patients, social media for younger patients, in clinic/centre for haemodialysis patients). Advertise opportunities in waiting rooms (e.g. videos, pamphlets, posters). Work with physicians and nurses to engage patients/caregivers. Ask patients to suggest new patients to be involved; consider having patient mentors to induct new patients into research projects.
|
| Training, support and education | Provide education for patient/caregiver partners (e.g. current research activities, kidney disease). Provide training in research methods (e.g. study design, academic writing, critical appraisal, recruitment). Consider psychological, mental and physical demands of involvement: ensure environment is accessible and can accommodate for patient needs (e.g. place to do peritoneal dialysis, elevator access); use communication strategies and simple language to reduce cognitive burden of involvement on patients; have referrals available in case of distress (e.g. social worker); offer flexible meeting options (e.g. videoconferencing, regular breaks, time for questions); andwhere possible, embed opportunities into routine care (e.g. transplant clinics). Financial reimbursement/aid may assist patients/caregiver to become involved: consider financial burden/sacrifice of involvement on patients/caregivers, and at a minimum, cover costs incurred (e.g. travel expenses, time off work); consider implementing a ‘jury duty’ system to reimburse patients/caregivers for their time; consider budgeting for paid patient/caregiver research partner position/s.
|
| Empowering the patient voice | Appoint more than one patient representative on a steering committee/working group. Consider forming a diverse patient advisory group to oversee research activities. Produce induction packets with relevant materials (e.g. glossary of terms/acronyms, background reading, helpful resources, videos). Use lay language where possible and explain technical/medical terminology when necessary. Allow time before or after meetings for patients/caregivers to consider their responses/opinions (e.g. send meeting agenda with topics to be discussed, follow-up post-meeting). Involve across all stages of the research; however, early involvement, before the grant stage, allows patient/caregiver contributions to be more easily integrated. Partner patient/caregiver with experienced research ‘buddy’ whom they can reach out to with any problems, questions or suggestions.
|
| Connection and community | Establish and expand a database to contact patients. Consider building a patient-dedicated research showcase portal/hub with lay language summaries of research and impacts, and opportunities for involvement to connect patients with researchers with potential for patients/caregivers to customize their profiles (interests, experience, CKD stage, etc.). Keep communications open with regular updates via newsletters, e-mails, texts and/or social media, even if no formal results are available. Collaborate with patient/caregiver and community organizations (e.g. present at patient support groups) to raise awareness of kidney disease, encourage knowledge exchange and advertise opportunities for involvement. Establish relationships with other research organizations to pool resources for patient/caregiver engagement to mitigate competing priorities, leverage collective goals and streamline communications to patients/caregivers. Disseminate research findings in plain language and informal settings to patients/caregivers to educate them about the outcomes and impact of research (including the impact of their involvement), build trust with the research community and encourage future involvement.
|
Respecting patient expertise and commitment
‘The power of people’s lived experience is immense’—Health professional.
‘Valuing unique and diverse experiential knowledge’: Health professionals acknowledged that patients could identify important outcomes for research such as sleep and quality of life, and that having patients actively involved ‘puts a human focus’ on research and reminded them of the ‘reason you’re doing it all’. Patients emphasized that all lived experience should be valued and to include caregivers who were ‘a goldmine of information’. Some patients were unsure about how they could contribute to research or thought that their opinion ‘doesn’t count’ because they did not have a medical background. Others believed their experience provided complementary expertise—‘You do bring in knowledge that [health professionals] don’t have…the reason people ask the wrong question is because they don’t have the experience of living with it’.
‘Clarifying expectations and responsibilities’: Research could be ‘kind of mystical’ for patients, and health professionals recognized that ‘one of the things that happens poorly is the explanation [of what is required] upfront’. They suggested to clarify the patient’s role, expected commitments and potential impact of their involvement to encourage patient research partners.
‘Equipping for meaningful involvement’: Patients wanted health professionals to use ‘plain simple English’ to provide adequate education and training and to avoid putting patients ‘on the spot’ by giving them time and resources to prepare before meetings and opportunities to respond afterwards. Patients thought that involving one patient on a steering group of health professionals was tokenistic and overwhelming for the patient and suggested that ‘at least three’ patients were needed to give them confidence in voicing their opinions and to convey diverse perspectives. They suggested that involving patients based on relevant expertise would enable meaningful contribution and that financial reimbursement may allow a more diverse group of patients to be involved.
‘Keeping patients “in the loop”’: To maintain interest, motivation and engagement in research, patients explained that they wanted to be included in regular communications and information ‘that you don’t need a medical degree to understand’. Contributing to research was ‘a two-way street’ and patients believed they should receive updates on projects they had been involved in even if the results were not yet available. Health professionals agreed that efforts to maintain communication with patients would serve to sustain relationships for longer-term and meaningful involvement in research.
Attuning to individual context
‘Once the patient is happy and healthy, then they’ll be able to go on and do research’—Patient
‘Preference-based multipronged approach to engagement’: Considering patients’ preferences for communication and tailoring the approach accordingly was suggested. Some older patients asked to be contacted by telephone or letter, while some younger patients preferred social media. Patients thought that innovative visual methods of communication such as infographics and YouTube videos would be an effective way to deliver potentially complicated research information.
‘Reducing the burden of involvement’: For patients, it was necessary to have flexibility, given their health and life priorities. One patient could not commit to research activities that required him to take annual leave, as he was saving this for his transplant, while another remarked that dialysis has ‘already chewed up enough of your day, you’ve already lost enough of your life’.
‘Being sensitive to the patient journey’: Patients urged researchers to ‘not hit you up for it [involvement] when you’re at your worst’ and to demonstrate sensitivity to each individual’s CKD journey. Some patients were ‘overwhelmed’ at diagnosis and not in the ‘right frame of mind’ to be involved in research. For patients on dialysis, the treatment burden was ‘all-consuming’ and it would be difficult to be involved in research when commencing dialysis. Fatigue and poor concentration could also constrain the patient’s ability to be involved.
Harnessing existing relationships and infrastructure
‘If we could piggyback onto diabetes research, that might raise public awareness’—Patient
‘Partnering with trusted clinicians’: Nephrologists and dialysis nurses that already had established relationships with patients were thought to be best placed to induct patients into research opportunities, and health professionals agreed that their networks of clinician colleagues could be further utilized to reach more patients.
‘Increasing research exposure in clinical settings’: Patients ‘had time to kill’ and suggested showing videos about research opportunities while waiting for appointments in the clinic. Patients thought ‘posters are really good’ to share opportunities for involvement in research.
‘Mentoring patient to patient’: Some believed that patients with previous research experience would be the best people to engage new patients ‘because they’ve been through it. The more you hear about the process, the more you start to think “I could probably cope with that”’. Patients thought they were uniquely placed to reach new patients in their own networks, including those residing in rural/remote areas. Some health professionals thought moderating peer interactions may be needed.
‘Extending reach through established networks’: Patients were frustrated by the lack of public awareness about kidney disease, compared with cancer and diabetes for example. They urged more ‘marketing’, ‘promotion’ and ‘education’ to ‘raise the profile’ of kidney disease in the community and not just in hospital settings. One patient noted, ‘[The kidney information booth] was set up in the [hospital] foyer for kidney health week, saying we’ll take your blood pressure…People who come to the hospital already know they’ve got high blood pressure. You should be outside Bunnings [hardware store]’.
Developing a coordinated approach
‘If you all get together, you’re there for one common cause, but being separate, it’s not really helping anyone’—Patient
‘Power in the collective and united voice’: One patient explained that researchers are ‘diluting the power of their communication’ as ‘there doesn’t appear to be one umbrella organisation that is driving communication [about research] to the consumer’. They agreed that a collective message would be more effective in reaching patients to get them involved in research.
‘Systematic approach for equitable inclusion’: Some patients were concerned that many patients may never be approached, while others become stuck on ‘this treadmill of being on all these different things’. Patients were confused and frustrated with privacy laws that prevented researchers contacting them through existing registries (e.g. ANZDATA), as they felt this denied them the opportunity to be involved. They suggested patients be presented with an opportunity to be involved in research through an opt-out registry for involvement in research for all patients with kidney disease—‘Why can’t we just have a kidney disease database [for researchers]?’
‘Streamlining access to opportunities for involvement and trustworthy information’: A comprehensive and reliable information platform covering all nephrology research in Australia, ‘a one-stop shop’ such as an online ‘hub’ or ‘portal’, would give patients access to opportunities for involvement and connect researchers to patients who want to be involved.
Fostering a patient-centred culture
‘It’s about spinning it around and not talking about the clinical stuff. It’s talking about the patient’s reasons of why it’s important, what’s in it for the patient’—Health professional
‘Building a community’: Patients, particularly those on home dialysis, often felt isolated and viewed involvement in research as an opportunity to connect with other patients and the research community through shared goals and experiences. Engaging patients in research could be improved if researchers facilitated the development of a community for research involvement and ‘took research to the patients’ on their own terms in a convenient, informal and unintimidating environment (e.g. patient support groups). This could provide opportunities for social interactions and educational discussions about kidney disease and research and establish connections for future relationships between patients and researchers.
‘Facilitating knowledge exchange and translation’: Patients believed they would be motivated to become involved in research if they knew about current research in nephrology and understood how research and their involvement could improve care. They often felt that they lacked knowledge and information about their illness and valued opportunities to learn more about their disease from health professionals. Dissemination of research findings to patients could be an effective method of engagement in research.
‘Empowering health ownership’: Patients faced uncertainties with their prognoses and treatments and therefore viewed their contributions to shaping and directing research as gaining ownership over their health. While they may not glean benefits directly from being involved, they wanted opportunities to assert their priorities and preferences—‘I believe in the power we have as consumers to change what’s important to us’.
‘Providing an opportunity to give back’: Helping future generations, paying forward the benefit they have received from others and giving something back to the community of health professionals who have cared for them motivated patients to become involved in research.
‘Cultivating trust through transparency’: A culture of communication and transparency could address mistrust of the research community among patients, particularly regarding distribution and prioritization of funding and researchers’ motivations. Patients identified a lack of involvement in grants and funding decisions resulting in resources being directed to research ‘contrary to what the patient might have picked’. Some believed researchers were ‘in there to get a degree’ or were ‘led kicking and screaming’ by mandates to involve patients. Being involved in all stages of the research cycle from applying for grants to disseminating findings and evaluating programmes would serve to allay these fears and allow for trust to develop between the research and patient communities, encouraging more involvement in research.
DISCUSSION
Patients and health professionals believed that involving patients as research partners required respect and recognition of the unique and complementary expertise of patients, consideration for the individual context, leveraging clinical and community networks for increased research exposure and streamlined, systematic approaches that unify research silos to foster a patient-centred culture for research. To enact these, practical approaches were suggested that covered selection and engagement; training, support and education; empowering the patient voice; and connection and community (Table 2).
These workshops support previous findings suggesting the engagement and selection of patients for involvement across the research cycle requires a plan for diversity [1, 7, 36]. Attendees suggested that strategies should support the inclusion of a broad range of experiences through involving multiple patient partners in different capacities and different stages (i.e. advisory group, co-investigator). However, the notion that patients need to be ‘representative’ to be able to make a meaningful contribution to research was challenged. It was argued that the intrinsic value of the unique expertise and lived experience that patients bring as research partners can serve to ground research in real-world applications, resulting in research that is relevant and important to all stakeholders, supporting both the moralistic and consequentialist arguments previously raised for involving patients in research [3, 35, 53].
Consistent with existing patient involvement frameworks from organizations such as PCORI and INVOLVE, patient partners can be better supported to make meaningful contributions through the provision of education and training in research methods to help contextualize their role and strengthen their capacity to contribute [5, 6, 45, 54]. Novel to these workshops was recognition of the need to consider the individual context of the patient and the impact this might have on their capacity for involvement. Awareness and sensitivity to the patient’s competing personal, professional and health-related priorities was expected to support respectful engagement by avoiding adding to overwhelming burdens at difficult times in the patient journey.
Empowering patients to contribute meaningfully is well recognized with increasing understanding that approaches such as having one patient on a steering committee can be tokenistic and disempowering [15]. A multipronged approach may be necessary to enable patients to confidently voice their needs and concerns, and detailed suggestions are available in Table 2.
Also distinct to these workshops was the concept of establishing a nationwide community of patients and health professionals for research partnership. Patients identified an opportunity to combat isolation and build trust with the research community by connecting patients and researchers in informal and social environments where they can learn and gain from each other. Of note, attendees acknowledged the need for a systematic way to engage patients in research. They viewed current ethics laws preventing researchers from using existing databases to contact patients with opportunities for involvement as a hindrance, denying them opportunities to shape the future of kidney research and therefore their own health outcomes. This highlights opportunities to draw from principles of participant-centred initiatives that leverage advances in technology and use social media to address consent and privacy concerns, while establishing long-term interactive partnerships [55].
While we were as inclusive as was feasible to obtain a broad range of perspectives, we note it is not possible to include a completely ‘representative’ group of patients (or health professionals), as they are contributing based on their individual experience and knowledge [56, 57]. We acknowledge that the transferability of the findings to other settings is uncertain.
Partnering with patients in research requires respect and recognition of their unique, diverse and complementary experiential expertise. Multiple and flexible approaches are necessary to consider the patient circumstances, stage in their CKD journey and existing burdens of their illness and treatment. Harnessing relationships with trusted clinicians and community organizations may help to broaden patient involvement and raise awareness of research in kidney disease, while innovative infrastructure to streamline the way patients engage with the research community can be further explored. Robust tools and frameworks to evaluate patient involvement in research are also needed [10, 11, 36].
SUPPLEMENTARY DATA
Supplementary data are available at ndt online.
ACKNOWLEDGEMENTS
We thank all the workshop investigators who volunteered their time and expertise to contribute to the workshops. We give a special mention to patient and research partner, the late Neville Fazulla, who made an important contribution to these workshops prior to his death.
Workshop facilitators and co-facilitators (not listed in the main authorship): Yeoungjee Cho, Margie Conley, Phil Clayton, Josephine Forbes, Angela Henson, Nikky Isbel, Laura James, Angela Ju, Pamela Lopez-Vargas, David Mudge, Lisa Shanahan, Matthew Sypek, Anita Van Zwieten and Andrea Viecelli. Workshop participants (patients/caregivers and health professionals), Sydney: Jane Beech-Allen, Mukesh Chandra, Helen Coolican, Judith Cornell, Clive Cornish, Vanessa Cullen, David Ellis, Jullianne Ellis, Esparanzo Evans, Jason Fisher, Paul Gilligan, Sandra Hesford, Tevor Hesford, Therese Hoogesteger, Colin Jones, Bruce Lin, Phillip McCready, Sherry Mead, Harry Michael, Rhonda Michael, Phillip Noble, Susan Noble, Michael Pennacchio, Peter Ramshaw, Lisa Richardson, Meral Senol, Tugba Senol and Tim Simpson. Workshop participants (patients/caregivers and health professionals), Adelaide: Sydney Aidinis, Ainslie Bolton, Alla Bondaruk, Lydia Bondaruk, Beryl Brearton, Paolo Cardelli, Michael Clark, John Dennis, Lois Ellery, Neville Fazulla, Rosalind Fulwood, Michael Geesing, John Griffith, Lynda Hall, Rob Hall, Chris Harrison, Greg Harward, Bronwyn Hockley, Patricia Ireland, Marina Karidis, Richard Le Leu, Marie Ludlow, Lindsay Lugg, George Majarian, Fabian Marsden, Tom Mayer, Tom Mayer Jr., Amritha Amalraj, Debbie Newton, Garrie Newton, Tamara Paget, Wayne Riches, David Roberts, Joy Roberts, Bronte Sterk, Barbara Stopp, Andrew Taylor, Maureen Taylor, Peter Taylor, Polly Taylor, Ann Tejada, Sandra Turner, Diana Voss, Amber Watt, Patricia Waxman and Trevor Wynne. Workshop participants (patients/caregivers and health professionals), Brisbane: Carlyn Ames, Neville Arkinstall, Gwen Arkinstall, Jenny Best, Jill Biedermann, Andrew Biedermann, Colin Brown, Anne Cameron, Phillip Carswell, Martin Chambers, Loraine Chambers, Frances Cowper, Jenevieve Dooley, Tony Dunning, Sue-Ann Dunning, Kerry Dwyer, Donna Felschow, Bernard Goan, Kate Greenup, Laurie Hindom, Linda Hindom, Wendy Hoy, Gaye Jennings, Sofia Kudlak, Mark Luchterhand, Amy Luchterhand, Irene Mewburn, Russell Morgan, Anthony Nester, Veronica Oliver, Carl Pedersen, Chris Sandford, Lloyd Smith, Andrea Viecelli, Julie Walker, Ralph Walker and Richard White.
FUNDING
T.G. is supported by a scholarship through the National Health and Medical Research Council (NHMRC) BEAT-CKD Programme (grant APP1092957). A.T. is supported by a NHMRC Fellowship (APP1106716).
AUTHORS’ CONTRIBUTIONS
T.G., A.T., M.H., K.D., C.M.H., J.C.C., S.J., J.R.C., D.W.J., L.M., D.R., S.C., E.D., S.M., N.S.R., A.W. and S.M. were involved in the research idea and study design. T.G., A.T., M.H., K.D., C.M.H., S.J., D.R., A.W. and S.M. were involved in data acquisition. T.G., A.T., M.H., K.D., C.M.H., J.C.C., S.J., J.R.C., D.W.J., L.M., D.R., S.C., E.D., S.M., N.S.R., A.W. and S.M. analysed and interpreted the data. A.T., J.C.C., S.J. and S.M were involved in supervision or mentorship. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest relevant to this article to disclose. The results presented in this article have not been published previously in whole or part, except in abstract format.
Box 1. Definition of patient, involvement and engagement
Patient/consumer: refers to a patient, caregiver or family member with lived experience of chronic kidney disease.
Involvement: refers to a sustained and meaningful contribution to the research process as more than a research subject or participant and can range from consultation to partnership.
Engagement: refers to the establishment of a relationship between patients and researchers and is the first step of involvement.
REFERENCES
1Boote
J
, Telford
R
, Cooper
C.
Consumer involvement in health research: a review and research agenda
.
Health Policy
2002
;
61
:
213
–
236
2Shippee
ND
, Domecq Garces
JP
, Prutsky Lopez
GJ
et al.
Patient and service user engagement in research: a systematic review and synthesized framework
.
Health Expect
2015
;
18
:
1151
–
1166
3Duffett
L.
Patient engagement: what partnering with patient in research is all about
.
Thromb Res
2017
;
150
:
113
–
120
4Harris
J
, Graue
M
, Dunning
T
et al.
Involving people with diabetes and the wider community in diabetes research: a realist review protocol
.
Syst Rev
2015
;
4
:
146
5INVOLVE.
Briefing Notes for Researchers: Involving the Public in NHS, Public Health and Social Care Research
.
Eastleigh, UK
:
INVOLVE
,
2012
6Can-SOLVE.
Engaging Patients in the Research Process—A toolkit for project leads
.
Vancouver, BC, Canada
:
Can-SOLVE
,
2017
7Vat
LE
, Ryan
D
, Etchegary
H.
Recruiting patients as partners in health research: a qualitative descriptive study
.
Res Involv Engagem
2017
;
3
:
15
8Ashcroft
J
, Wykes
T
, Taylor
J
et al.
Impact on the individual: what do patients and carers gain, lose and expect from being involved in research?
J Ment Health
2016
;
25
:
28
–
35
9Chalmers
I.
What do I want from health research and researchers when I am a patient?
BMJ
1995
;
310
:
1315
–
1318
12Donovan
J
, Little
P
, Mills
N
et al.
Quality improvement report: improving design and conduct of randomised trials by embedding them in qualitative research: ProtecT (prostate testing for cancer and treatment) study. Commentary: presenting unbiased information to patients can be difficult
.
Br Med J
2002
;
325
:
766
–
770
13Staley
K
.
Exploring Impact: Public Involvement in NHS, Public Health and Social Care Research
.
Eastleigh, UK
:
INVOLVE
,
2009
14Langston
AL
, Mccallum
M
, Campbell
MK
et al.
An integrated approach to consumer representation and involvement in a multicentre randomized controlled trial
.
J Soc Clin Trials
2005
;
2
:
80
–
87
15de Wit
MP
, Koelewijn-van Loon
MS
, Collins
S
et al.
“If I wasn’t this robust”: Patients’ expectations and experiences at the Outcome Measures in Rheumatology Conference 2010
.
Patient
2013
;
6
:
179
–
187
16de Wit
M
, Kirwan
JR
, Tugwell
P
et al.
Successful stepwise development of patient research partnership: 14 years’ experience of actions and consequences in Outcome Measures in Rheumatology (OMERACT)
.
Patient
2017
;
10
:
141
–
152
17Gutman
T
, Lopez‐Vargas
P
, Manera
KE
et al.
Identifying and integrating patient and caregiver perspectives in clinical practice guidelines for percutaneous renal biopsy
.
Nephrology
2019
;
24
:
395
–
404
18Miller
HM
, Tong
A
, Tunnicliffe
DJ
et al.
Identifying and integrating patient and caregiver perspectives for clinical practice guidelines on the screening and management of infectious microorganisms in hemodialysis units
.
Hemodial Int
2017
;
21
:
213
–
223
19Tong
A
, Tunnicliffe
DJ
, Lopez‐Vargas
P
et al.
Identifying and integrating consumer perspectives in clinical practice guidelines on autosomal‐dominant polycystic kidney disease
.
Nephrology
2016
;
21
:
122
–
132
20Robinson
BM
, Zhang
J
, Morgenstern
H
et al.
Worldwide, mortality risk is high soon after initiation of hemodialysis
.
Kidney Int
2014
;
85
:
158
–
165
21Wyld
M
, Morton
RL
, Hayen
A
et al.
A systematic review and meta-analysis of utility-based quality of life in chronic kidney disease treatments
.
PLoS Med
2012
;
9
:
e1001307
22Levin
A
, Tonelli
M
, Bonventre
J
et al.
Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy
.
Lancet
2017
;
390
:
1888
–
1917
23Jun
M
, Manns
B
, Laupacis
A
et al.
Assessing the extent to which current clinical research is consistent with patient priorities: a scoping review using a case study in patients on or nearing dialysis
.
Can J Kidney Health Dis
2015
;
2
:
35
24Manns
B
, Hemmelgarn
B
, Lillie
E
et al.
Setting research priorities for patients on or nearing dialysis
.
Clin J Am Soc Nephrol
2014
;
9
:
1813
–
1821
25Evangelidis
N
, Tong
A
, Manns
B
et al.
Developing a set of core outcomes for trials in hemodialysis: an international Delphi survey
.
Am J Kidney Dis
2017
;
70
:
464
–
475
26Sautenet
B
, Tong
A
, Williams
G
et al.
Scope and consistency of outcomes reported in randomized trials conducted in adults receiving hemodialysis: a systematic review
.
Am J Kidney Dis
2018
;
72
:
62
–
74
27Crocker
JC
, Boylan
AM
, Bostock
J
et al.
Is it worth it? Patient and public views on the impact of their involvement in health research and its assessment: a UK‐based qualitative interview study
.
Health Expect
2017
;
20
:
519
–
528
28Domecq
JP
, Prutsky
G
, Elraiyah
T
et al.
Patient engagement in research: a systematic review
.
BMC Health Serv Res
2014
;
14
:
89
29Fleurence
R
, Selby
JV
, Odom-Walker
K
et al.
How the Patient-Centered Outcomes Research Institute is engaging patients and others in shaping its research agenda
.
Health Aff
2013
;
32
:
393
–
400
30INVOLVE.
Supporting Public Involvement in NHS, Public Health and Social Care Research
.
Eastleigh, UK
:
INVOLVE
,
2018
.
http://www.invo.org.uk/ 32Tong
A
, Manns
B
, Hemmelgarn
B
et al.
Standardised outcomes in nephrology–haemodialysis (SONG-HD): study protocol for establishing a core outcome set in haemodialysis
.
Trials
2015
;
16
:
364
33McKenzie
A
, Alpers
K
, Heyworth
J
et al.
Consumer and community involvement in health and medical research: evaluation by online survey of Australian training workshops for researchers
.
Res Involv Engagem
2016
;
2
:
16
34Locock
L
, Boylan
AM
, Snow
R
et al.
The power of symbolic capital in patient and public involvement in health research
.
Health Expect
2017
;
20
:
836
–
844
35Dudley
L
, Gamble
C
, Preston
J
et al.
What difference does patient and public involvement make and what are its pathways to impact? Qualitative study of patients and researchers from a cohort of randomised clinical trials
.
PLoS One
2015
;
10
:
e0128817
36Snape
D
, Kirkham
J
, Britten
N
et al.
Exploring perceived barriers, drivers, impacts and the need for evaluation of public involvement in health and social care research: a modified Delphi study
.
BMJ Open
2014
;
4
:
e004943
37Boote
J
, Baird
W
, Beecroft
C.
Public involvement at the design stage of primary health research: a narrative review of case examples
.
Health Policy
2010
;
95
:
10
–
23
38Brett
J
, Staniszewska
S
, Mockford
C
et al.
Mapping the impact of patient and public involvement on health and social care research: a systematic review
.
Health Expect
2014
;
17
:
637
–
650
39Concannon
TW
, Fuster
M
, Saunders
T
et al.
A systematic review of stakeholder engagement in comparative effectiveness and patient-centered outcomes research
.
J Gen Intern Med
2014
;
29
:
1692
–
1701
40Nilsen
ES
, Myrhaug
HT
, Johansen
M
et al.
Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material
.
Cochrane Database Syst Rev
2006
;
3
:
CD004563
41Oliver
S
, Clarke-Jones
L
, Rees
R
et al.
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach
.
Health Technol Assess
2004
;
8
:
1
–
136
42Dennis
BK.
Understanding participant experiences: reflections of a novice research participant
.
Int J Qual Methods
2014
;
13
:
395
–
410
43Kirwan
JR
, de Wit
M
, Frank
L
et al.
Emerging guidelines for patient engagement in research
.
Value Health
2017
;
20
:
481
–
486
44Hewlett
S
, de Wit
M
, Richards
P
et al.
Patients and professionals as research partners: challenges, practicalities, and benefits
.
Arthritis Rheum
2006
;
55
:
676
–
680
45Telford
R
, Boote
JD
, Cooper
CL.
What does it mean to involve consumers successfully in NHS research? A consensus study
.
Health Expect
2004
;
7
:
209
–
220
46National Health and Medical Research Council.
Statement on Consumer and Community Involvement in Health and Medical Research
.
Canberra
:
National Health and Medical Research Council
,
2016
47BEAT-CKD.
Better Evidence and Translation in Chronic Kidney Disease
.
www.beatckd.org (10 October 2018, date last accessed)
48KHA-CARI.
Kidney Health Australia—Caring for Australasians with Renal Impairment
.
http://www.cari.org.au/ (10 October 2018, date last accessed)
49Australasian Kidney Trials Network. Homepage. aktn.org.au (10 October 2018, date last accessed)
50Australia and New Zealand Dialysis and Transplant Registry.
ANZDATA and ANZOD
.
http://www.anzdata.org.au (10 October 2018, date last accessed)
52Glaser
BG
, Strauss
AL.
Discovery of Grounded Theory: Strategies for Qualitative Research
.
London, UK
:
Routledge
,
2017
53Boote
J
, Wong
R
, Booth
A.
‘
Talking the talk or walking the walk?’A bibliometric review of the literature on public involvement in health research published between 1995 and 2009
.
Health Expect
2015
;
18
:
44
–
57
55Kaye
J
, Curren
L
, Anderson
N
et al.
From patients to partners: participant-centric initiatives in biomedical research
.
Nat Rev Genet
2012
;
13
:
371
56Edelman
N
, Barron
D.
Evaluation of public involvement in research: time for a major re-think?
J Health Serv Res Policy
2016
;
21
:
209
–
211
57Lander
J
, Langhof
H
, Dierks
M-L.
Involving patients and the public in medical and health care research studies: An exploratory survey on participant recruiting and representativeness from the perspective of study authors
.
PLoS One
2019
;
14
:
e0204187
Author notes
© The Author(s) 2019. Published by Oxford University Press on behalf of ERA-EDTA. All rights reserved.
PDF
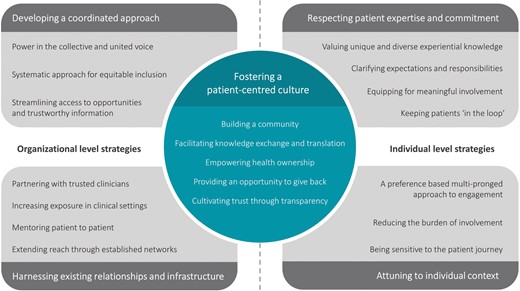





Comments