-
PDF
- Split View
-
Views
-
Cite
Cite
Luuk B Hilbrands, Raphaël Duivenvoorden, Priya Vart, Casper F M Franssen, Marc H Hemmelder, Kitty J Jager, Lyanne M Kieneker, Marlies Noordzij, Michelle J Pena, Hanne de Vries, David Arroyo, Adrian Covic, Marta Crespo, Eric Goffin, Mahmud Islam, Ziad A Massy, Nuria Montero, João P Oliveira, Ana Roca Muñoz, J Emilio Sanchez, Sivakumar Sridharan, Rebecca Winzeler, Ron T Gansevoort, ERACODA Collaborators , COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration, Nephrology Dialysis Transplantation, Volume 35, Issue 11, November 2020, Pages 1973–1983, https://doi.org/10.1093/ndt/gfaa261
Close - Share Icon Share
Abstract
Background. Patients on kidney replacement therapy comprise a vulnerable population and may be at increased risk of death from coronavirus disease 2019 (COVID-19). Currently, only limited data are available on outcomes in this patient population.
Methods. We set up the ERACODA (European Renal Association COVID-19 Database) database, which is specifically designed to prospectively collect detailed data on kidney transplant and dialysis patients with COVID-19. For this analysis, patients were included who presented between 1 February and 1 May 2020 and had complete information available on the primary outcome parameter, 28-day mortality.
Results. Of the 1073 patients enrolled, 305 (28%) were kidney transplant and 768 (72%) dialysis patients with a mean age of 60 ± 13 and 67 ± 14 years, respectively. The 28-day probability of death was 21.3% [95% confidence interval (95% CI) 14.3–30.2%] in kidney transplant and 25.0% (95% CI 20.2–30.0%) in dialysis patients. Mortality was primarily associated with advanced age in kidney transplant patients, and with age and frailty in dialysis patients. After adjusting for sex, age and frailty, in-hospital mortality did not significantly differ between transplant and dialysis patients [hazard ratio (HR) 0.81, 95% CI 0.59–1.10, P = 0.18]. In the subset of dialysis patients who were a candidate for transplantation (n = 148), 8 patients died within 28 days, as compared with 7 deaths in 23 patients who underwent a kidney transplantation <1 year before presentation (HR adjusted for sex, age and frailty 0.20, 95% CI 0.07–0.56, P < 0.01).
Conclusions. The 28-day case-fatality rate is high in patients on kidney replacement therapy with COVID-19 and is primarily driven by the risk factors age and frailty. Furthermore, in the first year after kidney transplantation, patients may be at increased risk of COVID-19-related mortality as compared with dialysis patients on the waiting list for transplantation. This information is important in guiding clinical decision-making, and for informing the public and healthcare authorities on the COVID-19-related mortality risk in kidney transplant and dialysis patients.
What is already known about this subject?
studies in the general population have identified several risk factors for coronavirus disease 2019 (COVID-19)-related mortality, including age, male gender, obesity, hypertension, cardiovascular disease, diabetes mellitus, chronic lung disease, cancer and chronic kidney disease;
limited data are available on COVID-19-related mortality in dialysis and renal transplant patients, which are particularly vulnerable populations; and
we set up the ERACODA (European Renal Association COVID-19 Database) database to inform clinician, the public and healthcare authorities on the COVID-19-related mortality risk in kidney transplant and dialysis patients.
What this study adds?
the 28-day COVID-19-related mortality is 21.3% in kidney transplant and 25.0% in dialysis patients, which is markedly higher than what is observed in other populations;
age is the predominant risk factor in transplant patients, whereas in dialysis patients especially frailty is associated with mortality; and
the risk of mortality due to COVID-19 may be lower in dialysis patients on the waiting list for kidney transplantation than in patients who received a kidney transplant less than a year before. This finding needs confirmation in additional studies.
What impact this may have on practice or policy?
our data inform clinicians, patients, the general public and healthcare authorities that renal transplant and dialysis patients are at significant risk of death if they contract COVID-19. Preventive measures are therefore of great importance in these populations; and
we identified age and frailty as important risk factors for COVID-19-related mortality. We therefore propose that an assessment of frailty should be an essential part of risk assessment and clinical decision-making in transplant and dialysis patients with COVID-19.
INTRODUCTION
Since the start of the outbreak in China in December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread throughout the world at an alarming pace [1]. The severity of coronavirus disease 2019 (COVID-19) symptoms varies from mild complaints to serious life-threatening illness [2]. In the report of the Chinese Center for Disease Control on 44 672 confirmed COVID-19 patients, 19% of patients were found to develop severe symptoms and the case-fatality rate was 2.3% [2]. Reported case-fatality rates vary greatly per region owing to differences in demographics and case ascertainment [3].
Several studies have indicated that advanced age is the most important risk factor for mortality [4–8]. Patients older than 70 years have an >10-fold increased risk of death when compared with patients under 50 years of age [8]. Across all age groups, male sex was found to be associated with increased risk of mortality [4–8]. Furthermore, a number of underlying comorbidities and conditions have been associated with mortality, including obesity, hypertension, cardiovascular disease, diabetes mellitus, chronic lung disease and cancer [8–14]. Also, chronic kidney disease has been associated with increased risk of mortality [8, 9, 13].
Currently, only limited data are available on outcomes in patients treated with kidney replacement therapy [8, 9, 15–19]. Patients who have a kidney transplant or are on dialysis may be at particularly high risk of mortality as they are generally older and often have chronic underlying conditions such as hypertension, cardiovascular disease and diabetes mellitus [20]. In addition, kidney transplant patients are treated with immunosuppressive drugs, which may increase the risk of contracting SARS-CoV-2 infection and developing severe symptoms [8, 9, 15–19]. In response to the COVID-19 pandemic, a large European database (ERACODA, the European Renal Association COVID-19 Database) has been constructed to specifically investigate the course and outcome of COVID-19 in patients living with a kidney transplant or on maintenance dialysis therapy. Here we present the 28-day outcome in terms of hospital admission, intensive care unit (ICU) admission and mortality. We furthermore report associations of patient, disease and treatment characteristics with mortality and compare outcome in kidney transplant and dialysis patients where relevant.
MATERIALS AND METHODS
Data source
For the present study, we analysed information from the ERACODA database, which was established on 21 March 2020 and at present involves the cooperation of 170 physicians representing 98 centres in 26 countries, mainly in Europe and the northern part of the Mediterranean (Supplementary data, Table S1). This database is endorsed by the ERA-EDTA. It gathers data on adult (≥18 years old) patients with a functioning kidney allograft or on long-term dialysis treatment who are diagnosed to have COVID-19 based on a positive result on a real-time polymerase chain reaction (PCR) assay of nasal or pharyngeal swab specimens, and/or compatible findings on a computed tomography scan (CT scan) of the lungs. Data from outpatients as well as hospitalized patients are collected. Physicians responsible for the care of these patients can register voluntarily and are asked to enter data of all consecutive kidney transplant and long-term dialysis patients from their centre with COVID-19.
The ERACODA database is hosted at the University Medical Center Groningen, the Netherlands, and uses REDCap software (Research Electronic Data Capture, Vanderbilt University Medical Center, Nashville, TN, USA). Missing data are recovered and inconsistencies are corrected through online interaction. All patient identifiable information is stripped from each record and data are stored pseudonymized. The study was assessed by the Institutional Review Board of the University Medical Center Groningen, the Netherlands, which deemed the collection and analysis of data exempt from ethics review in the context of the Medical Research Involving Human Subjects Act (WMO). The database is compliant with European Union General Data Protection Regulation (GDPR, 2016/679).
Data collection
To be included for the present analysis, the date of presentation for evaluation of COVID-19 should be between 1 February and 1 May 2020, and information on vital status at Day 28 after presentation should be available. The primary outcome is mortality. Secondary outcomes are ICU admission, need for invasive ventilation, and need for kidney replacement therapy. Outcomes were recorded with the end of follow-up at Day 28, with the last follow-up data entered on 1 June 2020. Information is collected on patient characteristics (including demographics, frailty score referring to the clinical situation before the COVID-19 episode, comorbidities, primary kidney disease and medication use) and COVID-19-related characteristics (presenting symptoms, vital signs and laboratory test results) at presentation. Furthermore, the use of renin–angiotensin–aldosterone system (RAAS) inhibitors and immunosuppressive drugs, as well as changes in the dosing of these drugs during the first 48 h after hospital admission, and the start of anti-viral or anti-inflammatory therapy were recorded. In case subjects were initially not admitted but were on a second occasion, characteristics and treatment (changes) at second presentation were used for the present analyses. Tobacco use was scored as never, prior or current use, or unknown. Comorbidities were registered as derived from patient records, with obesity defined as a body mass index (BMI) >30 kg/m2. Frailty was scored on a scale of 1–9 according to the Clinical Frailty Scale (CFS), an easily applicable tool to stratify patients according to the level of vulnerability [21–23]. The CFS uses functional descriptors and pictographs. A score of 1 represents very fit, and 9 terminally ill [21–23]. Primary kidney disease was registered using the ERA-EDTA coding system [24].
Study oversight
Our observational study was designed by the ERACODA Working Group, which also runs the database assisted by a Management Team and an Advisory Board (members listed in the Acknowledgements). Details of authors' contributions are provided at the end of the article.
Statistical analysis
Continuous data are presented as mean with standard deviation (SD) or as median and interquartile range (IQR) in case of non-normal distribution. Categorical data are presented as percentages. Mortality was assessed as the probability of death using the Kaplan–Meier method or as a case-fatality rate. Because we had complete follow-up for all included patients, the Kaplan–Meier curves have no censoring for missing data. The 28-day case-fatality rate was calculated as the proportion of deaths from COVID-19 at Day 28 after presentation compared with the total number of people diagnosed with COVID-19 who had complete 28-day follow-up information available, expressed as a percentage. To identify independent risk factors for mortality, the associations of patient, disease and treatment variables with death were examined using Cox proportional hazard regression analysis. Hazard ratios (HRs) and corresponding 95% confidence intervals (95% CIs) refer to a per unit increase in a continuous variable. First, we tested the strength of univariable associations of characteristics with outcome, and secondly the strengths of these associations adjusted for age and sex. Thirdly, a multivariable regression model was obtained using a backward elimination procedure and excluding missing data list-wise. Variables associated with mortality after age and sex adjustment with a P-value <0.1 were entered in this model. The least significant variables were removed stepwise, until none met the criterion of P-value >0.05. Associations of patient and disease characteristics with mortality were tested in all patients. Since antiviral and anti-inflammatory treatments were started predominantly in patients admitted to hospital, we restricted testing of associations of treatment (changes) with mortality to the subset of patients admitted to hospital to minimize bias by indication. Cox proportional hazards assumptions were tested with Schoenfeld residuals, and no violations were detected. In the multivariable models, we assessed the significance of interactions of the remaining significant terms. The tables show only data for variables for which the association with mortality had a P-value <0.05.
To examine the robustness of the initial estimates, we performed a sensitivity analysis in which we repeated all tests in a subset of patients that is likely representative for all patients on kidney replacement therapy with COVID-19 by analysing data entered by physicians who responded in the questionnaire that they had completed records of all consecutive kidney transplant and dialysis patients with COVID-19 cared for by their centre.
Lastly, we were interested in mortality in patients who suffered from COVID-19 shortly after kidney transplantation. Therefore, we studied mortality risk separately for patients with an interval after transplantation of <1, 1–5 and >5 years, respectively, and compared the results with the mortality risk in dialysis patients who were on the waiting list for a transplantation or in preparation to be placed on the waiting list.
All analyses were performed with the statistical software SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). A two-sided P-value <0.05 indicated statistical significance. Because we judged Type 2 error to be a greater concern, the Type 1 error rate was quantified without adjustment for multiplicity of comparisons, implying that these results should be interpreted as exploratory.
RESULTS
Demographics and disease characteristics
As of 1 June 2020, a total of 1073 patients with COVID-19 and complete 28-day follow-up had been entered in the ERACODA database. Of the 1073 patients enrolled, 305 (28%) were kidney transplant patients and 768 (72%) were on dialysis, with a vast majority (96%) on haemodialysis and only 4% on peritoneal dialysis. The demographic and clinical characteristics according to the type of kidney replacement therapy and vital status at Day 28 are listed in Table 1 for the overall populations. Sex-specific data are shown in the Supplementary data, Table S2. Mean age was 60 ± 13 years in kidney transplant patients and 67 ± 14 years in dialysis patients, with a preponderance of males in both groups. The majority of patients suffered from one or more comorbidities, especially hypertension, diabetes mellitus and coronary artery disease. Frailty scores were 3.0 ± 1.6 AU in kidney transplant and 4.0 ± 1.8 AU in dialysis patients. The most commonly used immunosuppressive drugs in transplant patients were prednisone (84%), tacrolimus (77%) and mycophenolate (69%).
Characteristics of kidney transplant and dialysis patients with COVID-19, overall and according to vital status at Day 28
| . | Kidney transplant patients . | Dialysis patients . | ||||
|---|---|---|---|---|---|---|
| . | Vital status at Day 28 . | . | Vital status at Day 28 . | |||
| All n = 305 . | Alive n = 240 . | Deceased n = 65 . | All n = 768 . | Alive n = 576 . | Deceased n = 192 . | |
| Characteristics . | ||||||
| Male sex, % | 62 | 64 | 54 | 60 | 59 | 64 |
| Age, years | 60 ± 13 | 56 ± 13 | 68 ± 11 | 67 ± 14 | 65 ± 14 | 72 ± 12 |
| BMI, kg/m2 | 27.0 ± 4.7 | 27.0 ± 4.8 | 27.0 ± 4.5 | 26.6 ± 5.7 | 26.5 ± 5.6 | 27.2 ± 5.9 |
| Race | ||||||
| Asian, % | 3 | 2 | 5 | 4 | 4 | 5 |
| Black or African descent, % | 7 | 8 | 3 | 5 | 6 | 3 |
| White or Caucasian, % | 81 | 81 | 78 | 82 | 80 | 85 |
| Other or unknown, % | 9 | 9 | 14 | 9 | 10 | 7 |
| Tobacco use | ||||||
| Current, % | 3 | 4 | 2 | 8 | 8 | 6 |
| Prior, % | 26 | 26 | 29 | 19 | 18 | 25 |
| Never, % | 52 | 50 | 57 | 39 | 41 | 31 |
| Unknown, % | 19 | 20 | 12 | 34 | 33 | 38 |
| CFS, AU | 3.0 ± 1.6 | 2.7 ± 1.4 | 3.8 ± 1.7 | 4.0 ± 1.8 | 3.6 ± 1.7 | 5.1 ± 1.8 |
| Comorbidities | ||||||
| Obesity, % | 23 | 22 | 25 | 23 | 21 | 28 |
| Hypertension, % | 83 | 84 | 80 | 82 | 85 | 77 |
| Diabetes mellitus, % | 32 | 28 | 45 | 42 | 42 | 48 |
| Coronary artery disease, % | 21 | 18 | 31 | 30 | 29 | 32 |
| Heart failure, % | 8 | 5 | 18 | 22 | 20 | 32 |
| Chronic lung disease, % | 9 | 8 | 14 | 13 | 13 | 16 |
| Active malignancy, % | 7 | 4 | 17 | 6 | 5 | 9 |
| Autoimmune disease, % | 5 | 5 | 3 | 4 | 4 | 4 |
| Primary kidney disease | ||||||
| Prim. glomerulonephritis, % | 20 | 22 | 10 | 16 | 17 | 10 |
| Pyelonephritis, % | 4 | 4 | 6 | 1 | 2 | 1 |
| Interstitial nephritis, % | 6 | 7 | 3 | 4 | 4 | 5 |
| Hereditary renal disease, % | 15 | 16 | 11 | 9 | 11 | 6 |
| Congenital diseases, % | 4 | 5 | 2 | 1 | 2 | 1 |
| Vascular diseases, % | 10 | 7 | 19 | 17 | 14 | 26 |
| Sec. glomerular disease, % | 5 | 6 | 2 | 10 | 10 | 10 |
| Diabetic kidney disease, % | 16 | 14 | 24 | 26 | 25 | 30 |
| Other, % | 5 | 3 | 10 | 5 | 5 | 5 |
| Unknown, % | 12 | 15 | 13 | 10 | 11 | 6 |
| Haemodialysis, % | NA | NA | NA | 96 | 96 | 95 |
| Peritoneal dialysis, % | NA | NA | NA | 4 | 4 | 5 |
| Residual diuresis ≥200 mL/day | NA | NA | NA | 33 | 36 | 26 |
| Transplant waiting list status | ||||||
| Active on waiting list, % | NA | NA | NA | 11 | 14 | 1 |
| In preparation, % | NA | NA | NA | 8 | 10 | 3 |
| Temporarily not on list, % | NA | NA | NA | 7 | 8 | 4 |
| Not transplantable, % | NA | NA | NA | 56 | 51 | 72 |
| Unknown, % | NA | NA | NA | 8 | 7 | 9 |
| Time since transplantation | ||||||
| <1 year, % | 7 | 7 | 11 | NA | NA | NA |
| 1–5 years, % | 31 | 34 | 21 | NA | NA | NA |
| >5 years, % | 60 | 58 | 66 | NA | NA | NA |
| Medication use | ||||||
| Use of RAAS inhibition | ||||||
| ACE inhibitors, % | 21 | 21 | 25 | 11 | 13 | 8 |
| ARB, % | 20 | 21 | 15 | 10 | 10 | 10 |
| Use of immunosuppressive medication | ||||||
| Prednisone, % | 84 | 83 | 88 | NA | NA | NA |
| Tacrolimus, % | 77 | 77 | 80 | NA | NA | NA |
| Cyclosporine, % | 10 | 10 | 12 | NA | NA | NA |
| Mycophenolate, % | 69 | 68 | 71 | NA | NA | NA |
| Azathioprine, % | 5 | 6 | 2 | NA | NA | NA |
| mTOR inhibitor, % | 14 | 15 | 12 | NA | NA | NA |
| Presenting symptoms | ||||||
| Sore throat, % | 15 | 16 | 11 | 11 | 11 | 10 |
| Cough, % | 67 | 65 | 77 | 45 | 43 | 50 |
| Shortness of breath, % | 46 | 39 | 72 | 32 | 26 | 49 |
| Fever, % | 75 | 74 | 81 | 54 | 49 | 67 |
| Headache, % | 15 | 17 | 10 | 8 | 8 | 8 |
| Nausea or vomiting, % | 17 | 17 | 17 | 9 | 9 | 11 |
| Diarrhea, % | 31 | 32 | 25 | 11 | 10 | 12 |
| Myalgia or arthralgia, % | 28 | 28 | 32 | 20 | 19 | 25 |
| Vital signs | ||||||
| Temperature, °C | 37.5 ± 1.1 | 37.5 ± 1.1 | 37.5 ± 1.0 | 37.5 ± 1.0 | 37.3 ± 1.0 | 37.8 ± 1.0 |
| Respiration rate, /min | 20.9 ± 7.0 | 19.7 ± 6.1 | 25.4 ± 8.1 | 18.8 ± 4.9 | 18.3 ± 4.5 | 20.5 ± 5.5 |
| O2 saturation room air, % | 93.6 ± 7.6 | 94.3 ± 6.9 | 91.0 ± 9.3 | 93.8 ± 5.1 | 94.4 ± 4.5 | 92.0 ± 5.1 |
| SBP, mmHg | 131 ± 20 | 130 ± 18 | 136 ± 24 | 137 ± 26 | 138 ± 24 | 133 ± 30 |
| DBP, mmHg | 76 ± 14 | 76 ± 13 | 77 ± 15 | 75 ± 15 | 76 ± 14 | 70 ± 17 |
| Pulse rate, BPM | 86 ± 17 | 86 ± 17 | 86 ± 16 | 83 ± 16 | 82 ± 15 | 88 ± 17 |
| Laboratory test results | ||||||
| Lymphocytes, ×1000/µL | 0.8 (0.5–1.3) | 0.9 (0.5–1.3) | 0.7 (0.4–1.0) | 0.9 (0.6–1.2) | 0.9 (0.6–1.3) | 0.7 (0.5–1.1) |
| eGFR, mL/min/1.73 m2 | 37 (21–51) | 39 (25–55) | 27 (18–43) | NA | NA | NA |
| CRP, mg/L | 52 (14-100) | 41 (10-89) | 85 (38-147) | 21 (5-70) | 19 (4–57) | 34 (12–114) |
| . | Kidney transplant patients . | Dialysis patients . | ||||
|---|---|---|---|---|---|---|
| . | Vital status at Day 28 . | . | Vital status at Day 28 . | |||
| All n = 305 . | Alive n = 240 . | Deceased n = 65 . | All n = 768 . | Alive n = 576 . | Deceased n = 192 . | |
| Characteristics . | ||||||
| Male sex, % | 62 | 64 | 54 | 60 | 59 | 64 |
| Age, years | 60 ± 13 | 56 ± 13 | 68 ± 11 | 67 ± 14 | 65 ± 14 | 72 ± 12 |
| BMI, kg/m2 | 27.0 ± 4.7 | 27.0 ± 4.8 | 27.0 ± 4.5 | 26.6 ± 5.7 | 26.5 ± 5.6 | 27.2 ± 5.9 |
| Race | ||||||
| Asian, % | 3 | 2 | 5 | 4 | 4 | 5 |
| Black or African descent, % | 7 | 8 | 3 | 5 | 6 | 3 |
| White or Caucasian, % | 81 | 81 | 78 | 82 | 80 | 85 |
| Other or unknown, % | 9 | 9 | 14 | 9 | 10 | 7 |
| Tobacco use | ||||||
| Current, % | 3 | 4 | 2 | 8 | 8 | 6 |
| Prior, % | 26 | 26 | 29 | 19 | 18 | 25 |
| Never, % | 52 | 50 | 57 | 39 | 41 | 31 |
| Unknown, % | 19 | 20 | 12 | 34 | 33 | 38 |
| CFS, AU | 3.0 ± 1.6 | 2.7 ± 1.4 | 3.8 ± 1.7 | 4.0 ± 1.8 | 3.6 ± 1.7 | 5.1 ± 1.8 |
| Comorbidities | ||||||
| Obesity, % | 23 | 22 | 25 | 23 | 21 | 28 |
| Hypertension, % | 83 | 84 | 80 | 82 | 85 | 77 |
| Diabetes mellitus, % | 32 | 28 | 45 | 42 | 42 | 48 |
| Coronary artery disease, % | 21 | 18 | 31 | 30 | 29 | 32 |
| Heart failure, % | 8 | 5 | 18 | 22 | 20 | 32 |
| Chronic lung disease, % | 9 | 8 | 14 | 13 | 13 | 16 |
| Active malignancy, % | 7 | 4 | 17 | 6 | 5 | 9 |
| Autoimmune disease, % | 5 | 5 | 3 | 4 | 4 | 4 |
| Primary kidney disease | ||||||
| Prim. glomerulonephritis, % | 20 | 22 | 10 | 16 | 17 | 10 |
| Pyelonephritis, % | 4 | 4 | 6 | 1 | 2 | 1 |
| Interstitial nephritis, % | 6 | 7 | 3 | 4 | 4 | 5 |
| Hereditary renal disease, % | 15 | 16 | 11 | 9 | 11 | 6 |
| Congenital diseases, % | 4 | 5 | 2 | 1 | 2 | 1 |
| Vascular diseases, % | 10 | 7 | 19 | 17 | 14 | 26 |
| Sec. glomerular disease, % | 5 | 6 | 2 | 10 | 10 | 10 |
| Diabetic kidney disease, % | 16 | 14 | 24 | 26 | 25 | 30 |
| Other, % | 5 | 3 | 10 | 5 | 5 | 5 |
| Unknown, % | 12 | 15 | 13 | 10 | 11 | 6 |
| Haemodialysis, % | NA | NA | NA | 96 | 96 | 95 |
| Peritoneal dialysis, % | NA | NA | NA | 4 | 4 | 5 |
| Residual diuresis ≥200 mL/day | NA | NA | NA | 33 | 36 | 26 |
| Transplant waiting list status | ||||||
| Active on waiting list, % | NA | NA | NA | 11 | 14 | 1 |
| In preparation, % | NA | NA | NA | 8 | 10 | 3 |
| Temporarily not on list, % | NA | NA | NA | 7 | 8 | 4 |
| Not transplantable, % | NA | NA | NA | 56 | 51 | 72 |
| Unknown, % | NA | NA | NA | 8 | 7 | 9 |
| Time since transplantation | ||||||
| <1 year, % | 7 | 7 | 11 | NA | NA | NA |
| 1–5 years, % | 31 | 34 | 21 | NA | NA | NA |
| >5 years, % | 60 | 58 | 66 | NA | NA | NA |
| Medication use | ||||||
| Use of RAAS inhibition | ||||||
| ACE inhibitors, % | 21 | 21 | 25 | 11 | 13 | 8 |
| ARB, % | 20 | 21 | 15 | 10 | 10 | 10 |
| Use of immunosuppressive medication | ||||||
| Prednisone, % | 84 | 83 | 88 | NA | NA | NA |
| Tacrolimus, % | 77 | 77 | 80 | NA | NA | NA |
| Cyclosporine, % | 10 | 10 | 12 | NA | NA | NA |
| Mycophenolate, % | 69 | 68 | 71 | NA | NA | NA |
| Azathioprine, % | 5 | 6 | 2 | NA | NA | NA |
| mTOR inhibitor, % | 14 | 15 | 12 | NA | NA | NA |
| Presenting symptoms | ||||||
| Sore throat, % | 15 | 16 | 11 | 11 | 11 | 10 |
| Cough, % | 67 | 65 | 77 | 45 | 43 | 50 |
| Shortness of breath, % | 46 | 39 | 72 | 32 | 26 | 49 |
| Fever, % | 75 | 74 | 81 | 54 | 49 | 67 |
| Headache, % | 15 | 17 | 10 | 8 | 8 | 8 |
| Nausea or vomiting, % | 17 | 17 | 17 | 9 | 9 | 11 |
| Diarrhea, % | 31 | 32 | 25 | 11 | 10 | 12 |
| Myalgia or arthralgia, % | 28 | 28 | 32 | 20 | 19 | 25 |
| Vital signs | ||||||
| Temperature, °C | 37.5 ± 1.1 | 37.5 ± 1.1 | 37.5 ± 1.0 | 37.5 ± 1.0 | 37.3 ± 1.0 | 37.8 ± 1.0 |
| Respiration rate, /min | 20.9 ± 7.0 | 19.7 ± 6.1 | 25.4 ± 8.1 | 18.8 ± 4.9 | 18.3 ± 4.5 | 20.5 ± 5.5 |
| O2 saturation room air, % | 93.6 ± 7.6 | 94.3 ± 6.9 | 91.0 ± 9.3 | 93.8 ± 5.1 | 94.4 ± 4.5 | 92.0 ± 5.1 |
| SBP, mmHg | 131 ± 20 | 130 ± 18 | 136 ± 24 | 137 ± 26 | 138 ± 24 | 133 ± 30 |
| DBP, mmHg | 76 ± 14 | 76 ± 13 | 77 ± 15 | 75 ± 15 | 76 ± 14 | 70 ± 17 |
| Pulse rate, BPM | 86 ± 17 | 86 ± 17 | 86 ± 16 | 83 ± 16 | 82 ± 15 | 88 ± 17 |
| Laboratory test results | ||||||
| Lymphocytes, ×1000/µL | 0.8 (0.5–1.3) | 0.9 (0.5–1.3) | 0.7 (0.4–1.0) | 0.9 (0.6–1.2) | 0.9 (0.6–1.3) | 0.7 (0.5–1.1) |
| eGFR, mL/min/1.73 m2 | 37 (21–51) | 39 (25–55) | 27 (18–43) | NA | NA | NA |
| CRP, mg/L | 52 (14-100) | 41 (10-89) | 85 (38-147) | 21 (5-70) | 19 (4–57) | 34 (12–114) |
Continuous variables are reported as mean ± SD or median (IQR). eGFR is calculated with the creatinine-based Chronic Kidney Disease Epidemiology Collaboration formula. Obesity is defined as BMI >30 kg/m2.
ACE, angiotensin-converting enzyme; ARB, angiotensin-II receptor blocker; AU, arbitrary units; CRP, C-reactive protein; DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; NA, not applicable; O2, oxygen; prim., primary; SBP, systolic blood pressure; sec., secondary.
Characteristics of kidney transplant and dialysis patients with COVID-19, overall and according to vital status at Day 28
| . | Kidney transplant patients . | Dialysis patients . | ||||
|---|---|---|---|---|---|---|
| . | Vital status at Day 28 . | . | Vital status at Day 28 . | |||
| All n = 305 . | Alive n = 240 . | Deceased n = 65 . | All n = 768 . | Alive n = 576 . | Deceased n = 192 . | |
| Characteristics . | ||||||
| Male sex, % | 62 | 64 | 54 | 60 | 59 | 64 |
| Age, years | 60 ± 13 | 56 ± 13 | 68 ± 11 | 67 ± 14 | 65 ± 14 | 72 ± 12 |
| BMI, kg/m2 | 27.0 ± 4.7 | 27.0 ± 4.8 | 27.0 ± 4.5 | 26.6 ± 5.7 | 26.5 ± 5.6 | 27.2 ± 5.9 |
| Race | ||||||
| Asian, % | 3 | 2 | 5 | 4 | 4 | 5 |
| Black or African descent, % | 7 | 8 | 3 | 5 | 6 | 3 |
| White or Caucasian, % | 81 | 81 | 78 | 82 | 80 | 85 |
| Other or unknown, % | 9 | 9 | 14 | 9 | 10 | 7 |
| Tobacco use | ||||||
| Current, % | 3 | 4 | 2 | 8 | 8 | 6 |
| Prior, % | 26 | 26 | 29 | 19 | 18 | 25 |
| Never, % | 52 | 50 | 57 | 39 | 41 | 31 |
| Unknown, % | 19 | 20 | 12 | 34 | 33 | 38 |
| CFS, AU | 3.0 ± 1.6 | 2.7 ± 1.4 | 3.8 ± 1.7 | 4.0 ± 1.8 | 3.6 ± 1.7 | 5.1 ± 1.8 |
| Comorbidities | ||||||
| Obesity, % | 23 | 22 | 25 | 23 | 21 | 28 |
| Hypertension, % | 83 | 84 | 80 | 82 | 85 | 77 |
| Diabetes mellitus, % | 32 | 28 | 45 | 42 | 42 | 48 |
| Coronary artery disease, % | 21 | 18 | 31 | 30 | 29 | 32 |
| Heart failure, % | 8 | 5 | 18 | 22 | 20 | 32 |
| Chronic lung disease, % | 9 | 8 | 14 | 13 | 13 | 16 |
| Active malignancy, % | 7 | 4 | 17 | 6 | 5 | 9 |
| Autoimmune disease, % | 5 | 5 | 3 | 4 | 4 | 4 |
| Primary kidney disease | ||||||
| Prim. glomerulonephritis, % | 20 | 22 | 10 | 16 | 17 | 10 |
| Pyelonephritis, % | 4 | 4 | 6 | 1 | 2 | 1 |
| Interstitial nephritis, % | 6 | 7 | 3 | 4 | 4 | 5 |
| Hereditary renal disease, % | 15 | 16 | 11 | 9 | 11 | 6 |
| Congenital diseases, % | 4 | 5 | 2 | 1 | 2 | 1 |
| Vascular diseases, % | 10 | 7 | 19 | 17 | 14 | 26 |
| Sec. glomerular disease, % | 5 | 6 | 2 | 10 | 10 | 10 |
| Diabetic kidney disease, % | 16 | 14 | 24 | 26 | 25 | 30 |
| Other, % | 5 | 3 | 10 | 5 | 5 | 5 |
| Unknown, % | 12 | 15 | 13 | 10 | 11 | 6 |
| Haemodialysis, % | NA | NA | NA | 96 | 96 | 95 |
| Peritoneal dialysis, % | NA | NA | NA | 4 | 4 | 5 |
| Residual diuresis ≥200 mL/day | NA | NA | NA | 33 | 36 | 26 |
| Transplant waiting list status | ||||||
| Active on waiting list, % | NA | NA | NA | 11 | 14 | 1 |
| In preparation, % | NA | NA | NA | 8 | 10 | 3 |
| Temporarily not on list, % | NA | NA | NA | 7 | 8 | 4 |
| Not transplantable, % | NA | NA | NA | 56 | 51 | 72 |
| Unknown, % | NA | NA | NA | 8 | 7 | 9 |
| Time since transplantation | ||||||
| <1 year, % | 7 | 7 | 11 | NA | NA | NA |
| 1–5 years, % | 31 | 34 | 21 | NA | NA | NA |
| >5 years, % | 60 | 58 | 66 | NA | NA | NA |
| Medication use | ||||||
| Use of RAAS inhibition | ||||||
| ACE inhibitors, % | 21 | 21 | 25 | 11 | 13 | 8 |
| ARB, % | 20 | 21 | 15 | 10 | 10 | 10 |
| Use of immunosuppressive medication | ||||||
| Prednisone, % | 84 | 83 | 88 | NA | NA | NA |
| Tacrolimus, % | 77 | 77 | 80 | NA | NA | NA |
| Cyclosporine, % | 10 | 10 | 12 | NA | NA | NA |
| Mycophenolate, % | 69 | 68 | 71 | NA | NA | NA |
| Azathioprine, % | 5 | 6 | 2 | NA | NA | NA |
| mTOR inhibitor, % | 14 | 15 | 12 | NA | NA | NA |
| Presenting symptoms | ||||||
| Sore throat, % | 15 | 16 | 11 | 11 | 11 | 10 |
| Cough, % | 67 | 65 | 77 | 45 | 43 | 50 |
| Shortness of breath, % | 46 | 39 | 72 | 32 | 26 | 49 |
| Fever, % | 75 | 74 | 81 | 54 | 49 | 67 |
| Headache, % | 15 | 17 | 10 | 8 | 8 | 8 |
| Nausea or vomiting, % | 17 | 17 | 17 | 9 | 9 | 11 |
| Diarrhea, % | 31 | 32 | 25 | 11 | 10 | 12 |
| Myalgia or arthralgia, % | 28 | 28 | 32 | 20 | 19 | 25 |
| Vital signs | ||||||
| Temperature, °C | 37.5 ± 1.1 | 37.5 ± 1.1 | 37.5 ± 1.0 | 37.5 ± 1.0 | 37.3 ± 1.0 | 37.8 ± 1.0 |
| Respiration rate, /min | 20.9 ± 7.0 | 19.7 ± 6.1 | 25.4 ± 8.1 | 18.8 ± 4.9 | 18.3 ± 4.5 | 20.5 ± 5.5 |
| O2 saturation room air, % | 93.6 ± 7.6 | 94.3 ± 6.9 | 91.0 ± 9.3 | 93.8 ± 5.1 | 94.4 ± 4.5 | 92.0 ± 5.1 |
| SBP, mmHg | 131 ± 20 | 130 ± 18 | 136 ± 24 | 137 ± 26 | 138 ± 24 | 133 ± 30 |
| DBP, mmHg | 76 ± 14 | 76 ± 13 | 77 ± 15 | 75 ± 15 | 76 ± 14 | 70 ± 17 |
| Pulse rate, BPM | 86 ± 17 | 86 ± 17 | 86 ± 16 | 83 ± 16 | 82 ± 15 | 88 ± 17 |
| Laboratory test results | ||||||
| Lymphocytes, ×1000/µL | 0.8 (0.5–1.3) | 0.9 (0.5–1.3) | 0.7 (0.4–1.0) | 0.9 (0.6–1.2) | 0.9 (0.6–1.3) | 0.7 (0.5–1.1) |
| eGFR, mL/min/1.73 m2 | 37 (21–51) | 39 (25–55) | 27 (18–43) | NA | NA | NA |
| CRP, mg/L | 52 (14-100) | 41 (10-89) | 85 (38-147) | 21 (5-70) | 19 (4–57) | 34 (12–114) |
| . | Kidney transplant patients . | Dialysis patients . | ||||
|---|---|---|---|---|---|---|
| . | Vital status at Day 28 . | . | Vital status at Day 28 . | |||
| All n = 305 . | Alive n = 240 . | Deceased n = 65 . | All n = 768 . | Alive n = 576 . | Deceased n = 192 . | |
| Characteristics . | ||||||
| Male sex, % | 62 | 64 | 54 | 60 | 59 | 64 |
| Age, years | 60 ± 13 | 56 ± 13 | 68 ± 11 | 67 ± 14 | 65 ± 14 | 72 ± 12 |
| BMI, kg/m2 | 27.0 ± 4.7 | 27.0 ± 4.8 | 27.0 ± 4.5 | 26.6 ± 5.7 | 26.5 ± 5.6 | 27.2 ± 5.9 |
| Race | ||||||
| Asian, % | 3 | 2 | 5 | 4 | 4 | 5 |
| Black or African descent, % | 7 | 8 | 3 | 5 | 6 | 3 |
| White or Caucasian, % | 81 | 81 | 78 | 82 | 80 | 85 |
| Other or unknown, % | 9 | 9 | 14 | 9 | 10 | 7 |
| Tobacco use | ||||||
| Current, % | 3 | 4 | 2 | 8 | 8 | 6 |
| Prior, % | 26 | 26 | 29 | 19 | 18 | 25 |
| Never, % | 52 | 50 | 57 | 39 | 41 | 31 |
| Unknown, % | 19 | 20 | 12 | 34 | 33 | 38 |
| CFS, AU | 3.0 ± 1.6 | 2.7 ± 1.4 | 3.8 ± 1.7 | 4.0 ± 1.8 | 3.6 ± 1.7 | 5.1 ± 1.8 |
| Comorbidities | ||||||
| Obesity, % | 23 | 22 | 25 | 23 | 21 | 28 |
| Hypertension, % | 83 | 84 | 80 | 82 | 85 | 77 |
| Diabetes mellitus, % | 32 | 28 | 45 | 42 | 42 | 48 |
| Coronary artery disease, % | 21 | 18 | 31 | 30 | 29 | 32 |
| Heart failure, % | 8 | 5 | 18 | 22 | 20 | 32 |
| Chronic lung disease, % | 9 | 8 | 14 | 13 | 13 | 16 |
| Active malignancy, % | 7 | 4 | 17 | 6 | 5 | 9 |
| Autoimmune disease, % | 5 | 5 | 3 | 4 | 4 | 4 |
| Primary kidney disease | ||||||
| Prim. glomerulonephritis, % | 20 | 22 | 10 | 16 | 17 | 10 |
| Pyelonephritis, % | 4 | 4 | 6 | 1 | 2 | 1 |
| Interstitial nephritis, % | 6 | 7 | 3 | 4 | 4 | 5 |
| Hereditary renal disease, % | 15 | 16 | 11 | 9 | 11 | 6 |
| Congenital diseases, % | 4 | 5 | 2 | 1 | 2 | 1 |
| Vascular diseases, % | 10 | 7 | 19 | 17 | 14 | 26 |
| Sec. glomerular disease, % | 5 | 6 | 2 | 10 | 10 | 10 |
| Diabetic kidney disease, % | 16 | 14 | 24 | 26 | 25 | 30 |
| Other, % | 5 | 3 | 10 | 5 | 5 | 5 |
| Unknown, % | 12 | 15 | 13 | 10 | 11 | 6 |
| Haemodialysis, % | NA | NA | NA | 96 | 96 | 95 |
| Peritoneal dialysis, % | NA | NA | NA | 4 | 4 | 5 |
| Residual diuresis ≥200 mL/day | NA | NA | NA | 33 | 36 | 26 |
| Transplant waiting list status | ||||||
| Active on waiting list, % | NA | NA | NA | 11 | 14 | 1 |
| In preparation, % | NA | NA | NA | 8 | 10 | 3 |
| Temporarily not on list, % | NA | NA | NA | 7 | 8 | 4 |
| Not transplantable, % | NA | NA | NA | 56 | 51 | 72 |
| Unknown, % | NA | NA | NA | 8 | 7 | 9 |
| Time since transplantation | ||||||
| <1 year, % | 7 | 7 | 11 | NA | NA | NA |
| 1–5 years, % | 31 | 34 | 21 | NA | NA | NA |
| >5 years, % | 60 | 58 | 66 | NA | NA | NA |
| Medication use | ||||||
| Use of RAAS inhibition | ||||||
| ACE inhibitors, % | 21 | 21 | 25 | 11 | 13 | 8 |
| ARB, % | 20 | 21 | 15 | 10 | 10 | 10 |
| Use of immunosuppressive medication | ||||||
| Prednisone, % | 84 | 83 | 88 | NA | NA | NA |
| Tacrolimus, % | 77 | 77 | 80 | NA | NA | NA |
| Cyclosporine, % | 10 | 10 | 12 | NA | NA | NA |
| Mycophenolate, % | 69 | 68 | 71 | NA | NA | NA |
| Azathioprine, % | 5 | 6 | 2 | NA | NA | NA |
| mTOR inhibitor, % | 14 | 15 | 12 | NA | NA | NA |
| Presenting symptoms | ||||||
| Sore throat, % | 15 | 16 | 11 | 11 | 11 | 10 |
| Cough, % | 67 | 65 | 77 | 45 | 43 | 50 |
| Shortness of breath, % | 46 | 39 | 72 | 32 | 26 | 49 |
| Fever, % | 75 | 74 | 81 | 54 | 49 | 67 |
| Headache, % | 15 | 17 | 10 | 8 | 8 | 8 |
| Nausea or vomiting, % | 17 | 17 | 17 | 9 | 9 | 11 |
| Diarrhea, % | 31 | 32 | 25 | 11 | 10 | 12 |
| Myalgia or arthralgia, % | 28 | 28 | 32 | 20 | 19 | 25 |
| Vital signs | ||||||
| Temperature, °C | 37.5 ± 1.1 | 37.5 ± 1.1 | 37.5 ± 1.0 | 37.5 ± 1.0 | 37.3 ± 1.0 | 37.8 ± 1.0 |
| Respiration rate, /min | 20.9 ± 7.0 | 19.7 ± 6.1 | 25.4 ± 8.1 | 18.8 ± 4.9 | 18.3 ± 4.5 | 20.5 ± 5.5 |
| O2 saturation room air, % | 93.6 ± 7.6 | 94.3 ± 6.9 | 91.0 ± 9.3 | 93.8 ± 5.1 | 94.4 ± 4.5 | 92.0 ± 5.1 |
| SBP, mmHg | 131 ± 20 | 130 ± 18 | 136 ± 24 | 137 ± 26 | 138 ± 24 | 133 ± 30 |
| DBP, mmHg | 76 ± 14 | 76 ± 13 | 77 ± 15 | 75 ± 15 | 76 ± 14 | 70 ± 17 |
| Pulse rate, BPM | 86 ± 17 | 86 ± 17 | 86 ± 16 | 83 ± 16 | 82 ± 15 | 88 ± 17 |
| Laboratory test results | ||||||
| Lymphocytes, ×1000/µL | 0.8 (0.5–1.3) | 0.9 (0.5–1.3) | 0.7 (0.4–1.0) | 0.9 (0.6–1.2) | 0.9 (0.6–1.3) | 0.7 (0.5–1.1) |
| eGFR, mL/min/1.73 m2 | 37 (21–51) | 39 (25–55) | 27 (18–43) | NA | NA | NA |
| CRP, mg/L | 52 (14-100) | 41 (10-89) | 85 (38-147) | 21 (5-70) | 19 (4–57) | 34 (12–114) |
Continuous variables are reported as mean ± SD or median (IQR). eGFR is calculated with the creatinine-based Chronic Kidney Disease Epidemiology Collaboration formula. Obesity is defined as BMI >30 kg/m2.
ACE, angiotensin-converting enzyme; ARB, angiotensin-II receptor blocker; AU, arbitrary units; CRP, C-reactive protein; DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; NA, not applicable; O2, oxygen; prim., primary; SBP, systolic blood pressure; sec., secondary.
Ninety-three per cent of transplant patients and 96% of dialysis patients had a positive result on the SARS-CoV-2 PCR assay. The proportions of patients with a CT scan or X-ray showing COVID-19 compatible abnormalities were 92% and 88% in transplant patients and 74% and 69% in dialysis patients, respectively.
Hospital admission and treatment
Of the 305 transplant patients and 768 dialysis patients presenting with COVID-19, 89% and 70% were admitted to the hospital, respectively (Table 2). Six per cent of transplant and 4% of dialysis patients who were not admitted on initial presentation required hospital admission on a subsequent presentation. The mean time between onset of symptoms and hospital admission was 7 days in transplant patients and 3 days in dialysis patients. Of the admitted patients, 10% of transplant and 14% of dialysis patients were still admitted after 28 days of follow-up. A higher proportion of transplant than of dialysis patients was admitted to ICU and treated with invasive ventilation (21% versus 12% and 18% versus 10%, respectively) (Table 2; Supplementary data, Figure S1A). Patients admitted to the ICU had more severe signs of disease at presentation than those not requiring ICU admission (Supplementary data, Table S3).
| Characteristics . | Kidney transplant patients . | Dialysis patients . |
|---|---|---|
| All patients | n = 305 | n = 768 |
| Hospitalization, % | 89 | 70 |
| Reason for no hospital admission | ||
| No indication, % | 97 | 86 |
| Logistical reasons related to COVID-19, % | 0 | 2 |
| Patient/family preferred no admission, % | 3 | 12 |
| Admitted patients only | n = 271 | n = 538 |
| ICU admission, % | 21 | 12 |
| Reason for no ICU admission | ||
| No indication, % | 86 | 82 |
| Logistical reasons related to COVID-19, % | 4 | 1 |
| Patient/family preferred no admission, % | 1 | 1 |
| Prognosis was too bad, % | 9 | 16 |
| Ventilator support, % | 18 | 10 |
| Reason for no ventilator support | ||
| No indication, % | 86 | 83 |
| Logistical reasons related to COVID-19, % | 4 | 1 |
| Patient/family preferred no admission, % | 1 | 1 |
| Prognosis was too bad, % | 9 | 15 |
| Start of CVVH/haemodialysis, % | 11 | NA |
| Reason not to start CVVH/haemodialysis | ||
| No indication, % | 98 | NA |
| Logistical reasons related to COVID-19, % | 0 | NA |
| Patient/family preferred no admission, % | 0 | NA |
| Prognosis was too bad, % | 2 | NA |
| Continuing kidney replacement therapy during admission, % | NA | 95 |
| Increase in intensity kidney replacement therapy, % | NA | 8 |
| Reason for discontinuation of kidney replacement therapy | ||
| No indication, % | NA | 43 |
| Logistical reasons related to COVID-19, % | NA | 0 |
| Patient/family preferred no admission, % | NA | 0 |
| Prognosis was too bad, % | NA | 57 |
| Characteristics . | Kidney transplant patients . | Dialysis patients . |
|---|---|---|
| All patients | n = 305 | n = 768 |
| Hospitalization, % | 89 | 70 |
| Reason for no hospital admission | ||
| No indication, % | 97 | 86 |
| Logistical reasons related to COVID-19, % | 0 | 2 |
| Patient/family preferred no admission, % | 3 | 12 |
| Admitted patients only | n = 271 | n = 538 |
| ICU admission, % | 21 | 12 |
| Reason for no ICU admission | ||
| No indication, % | 86 | 82 |
| Logistical reasons related to COVID-19, % | 4 | 1 |
| Patient/family preferred no admission, % | 1 | 1 |
| Prognosis was too bad, % | 9 | 16 |
| Ventilator support, % | 18 | 10 |
| Reason for no ventilator support | ||
| No indication, % | 86 | 83 |
| Logistical reasons related to COVID-19, % | 4 | 1 |
| Patient/family preferred no admission, % | 1 | 1 |
| Prognosis was too bad, % | 9 | 15 |
| Start of CVVH/haemodialysis, % | 11 | NA |
| Reason not to start CVVH/haemodialysis | ||
| No indication, % | 98 | NA |
| Logistical reasons related to COVID-19, % | 0 | NA |
| Patient/family preferred no admission, % | 0 | NA |
| Prognosis was too bad, % | 2 | NA |
| Continuing kidney replacement therapy during admission, % | NA | 95 |
| Increase in intensity kidney replacement therapy, % | NA | 8 |
| Reason for discontinuation of kidney replacement therapy | ||
| No indication, % | NA | 43 |
| Logistical reasons related to COVID-19, % | NA | 0 |
| Patient/family preferred no admission, % | NA | 0 |
| Prognosis was too bad, % | NA | 57 |
CVVH, continuous venovenous haemofiltration; NA, not applicable.
| Characteristics . | Kidney transplant patients . | Dialysis patients . |
|---|---|---|
| All patients | n = 305 | n = 768 |
| Hospitalization, % | 89 | 70 |
| Reason for no hospital admission | ||
| No indication, % | 97 | 86 |
| Logistical reasons related to COVID-19, % | 0 | 2 |
| Patient/family preferred no admission, % | 3 | 12 |
| Admitted patients only | n = 271 | n = 538 |
| ICU admission, % | 21 | 12 |
| Reason for no ICU admission | ||
| No indication, % | 86 | 82 |
| Logistical reasons related to COVID-19, % | 4 | 1 |
| Patient/family preferred no admission, % | 1 | 1 |
| Prognosis was too bad, % | 9 | 16 |
| Ventilator support, % | 18 | 10 |
| Reason for no ventilator support | ||
| No indication, % | 86 | 83 |
| Logistical reasons related to COVID-19, % | 4 | 1 |
| Patient/family preferred no admission, % | 1 | 1 |
| Prognosis was too bad, % | 9 | 15 |
| Start of CVVH/haemodialysis, % | 11 | NA |
| Reason not to start CVVH/haemodialysis | ||
| No indication, % | 98 | NA |
| Logistical reasons related to COVID-19, % | 0 | NA |
| Patient/family preferred no admission, % | 0 | NA |
| Prognosis was too bad, % | 2 | NA |
| Continuing kidney replacement therapy during admission, % | NA | 95 |
| Increase in intensity kidney replacement therapy, % | NA | 8 |
| Reason for discontinuation of kidney replacement therapy | ||
| No indication, % | NA | 43 |
| Logistical reasons related to COVID-19, % | NA | 0 |
| Patient/family preferred no admission, % | NA | 0 |
| Prognosis was too bad, % | NA | 57 |
| Characteristics . | Kidney transplant patients . | Dialysis patients . |
|---|---|---|
| All patients | n = 305 | n = 768 |
| Hospitalization, % | 89 | 70 |
| Reason for no hospital admission | ||
| No indication, % | 97 | 86 |
| Logistical reasons related to COVID-19, % | 0 | 2 |
| Patient/family preferred no admission, % | 3 | 12 |
| Admitted patients only | n = 271 | n = 538 |
| ICU admission, % | 21 | 12 |
| Reason for no ICU admission | ||
| No indication, % | 86 | 82 |
| Logistical reasons related to COVID-19, % | 4 | 1 |
| Patient/family preferred no admission, % | 1 | 1 |
| Prognosis was too bad, % | 9 | 16 |
| Ventilator support, % | 18 | 10 |
| Reason for no ventilator support | ||
| No indication, % | 86 | 83 |
| Logistical reasons related to COVID-19, % | 4 | 1 |
| Patient/family preferred no admission, % | 1 | 1 |
| Prognosis was too bad, % | 9 | 15 |
| Start of CVVH/haemodialysis, % | 11 | NA |
| Reason not to start CVVH/haemodialysis | ||
| No indication, % | 98 | NA |
| Logistical reasons related to COVID-19, % | 0 | NA |
| Patient/family preferred no admission, % | 0 | NA |
| Prognosis was too bad, % | 2 | NA |
| Continuing kidney replacement therapy during admission, % | NA | 95 |
| Increase in intensity kidney replacement therapy, % | NA | 8 |
| Reason for discontinuation of kidney replacement therapy | ||
| No indication, % | NA | 43 |
| Logistical reasons related to COVID-19, % | NA | 0 |
| Patient/family preferred no admission, % | NA | 0 |
| Prognosis was too bad, % | NA | 57 |
CVVH, continuous venovenous haemofiltration; NA, not applicable.
More than 70% of hospitalized kidney transplant and dialysis patients received anti-viral treatment, which most often consisted of (hydroxy) chloroquine (Supplementary data, Table S4). While high-dose steroids were used in 18% of transplant patients and 11% of dialysis patients, the use of anti-inflammatory therapy with tocilizumab or anakinra was infrequent.
We documented changes in the doses of immunosuppressive drugs during the first 48 h after presentation in hospitalized kidney transplant patients (Supplementary data, Table S4). The dose of calcineurin inhibitors was reduced in 14%, with complete discontinuation in 15% of users. Mycophenolate was withdrawn in 54% of cases, whereas azathioprine and mechanistic target of rapamycin (mTOR) inhibitors were only infrequently reduced or withdrawn. The dose of prednisone was most often not changed or increased. Cessation of immunosuppressive medication occurred especially in patients with severe disease who required ICU admission.
Mortality
Probability of death within 28 days was 21.3% (95% CI 14.3–30.2%) in kidney transplant patients and 25.0% (95% CI 20.2–30.0%) in dialysis patients [Supplementary data, Figure S1B; unadjusted HR for the association of dialysis (versus transplant) with 28-day mortality was 1.23 (95% CI 0.93–1.63), P = 0.14]. To account for differences in disease severity, reflected in a higher admission rate in transplant patients and more COVID-19-related symptoms, the probability of death was separately analysed in hospitalized patients. In hospitalized transplant and dialysis patients, the 28-day probabilities of death were 23.6% (95% CI 15.8–32.3%) and 33.5% (95% CI 28.2–38.9%), respectively (HR 1.56, 95% CI 1.17–2.07, P = 0.002). However, after adjusting for sex, age and frailty, in-hospital mortality was similar in transplant and dialysis patients (HR 0.81, 95% CI 0.59–1.10, P = 0.18). Death rates in patients who required admission to the ICU were even higher (45% and 53%), respectively (Figure 1; Supplementary data, Table S3). The 28-day probability of death in patients who required mechanical ventilation was 53% and 59% in transplant and dialysis patients, respectively. Mortality in patients who were not admitted was low, with a 28-day case-fatality rate of 3% and 5% in kidney transplant and dialysis patients, respectively. Supplementary data, Figure S2 shows that the case-fatality rates increase sharply with higher age and frailty scores in kidney transplant as well as dialysis patients.
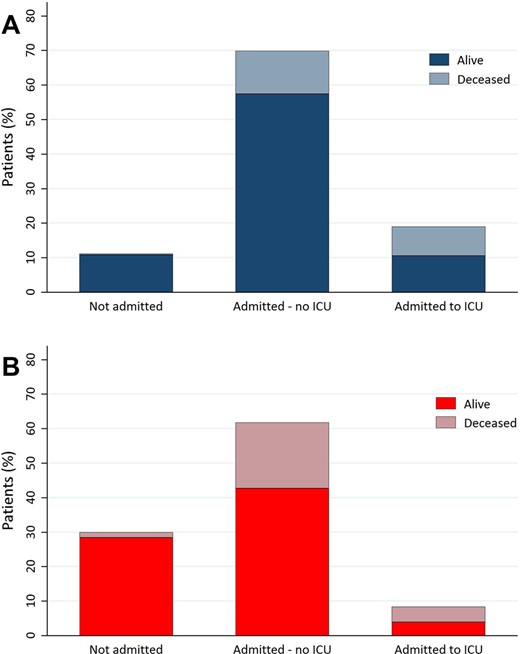
Vital status at Day 28 after presentation with COVID-19 of (A) kidney transplant (n = 305) and (B) haemodialysis patients (n = 768).
By univariable and multivariable analyses, we identified age as the most important risk factor for mortality in kidney transplant patients, and age and frailty in dialysis patients (Table 3). In Figure 2, we show the association between age, frailty and case-fatality rates, indicating that when these risk factors accumulate, mortality increases. In dialysis patients ≥75 years with a frailty score of 5 or higher, the 28-day case-fatality rate was 44%. In transplant patients, other risk factors remaining significant in multivariable analysis were higher respiration rate, decreased kidney function and use of prednisone (all at presentation). For dialysis patients, a higher risk of death was found for obesity, dyspnoea, high body temperature, high pulse rate and elevated liver enzymes at presentation. We did not find male sex, hypertension, chronic lung disease, coronary artery disease or diabetes mellitus to be major risk factors for mortality in transplant and dialysis patients (Figure 3). Repeating our analyses in hospitalized patients only and in a subset of patients that was likely representative for all patients on kidney replacement therapy with COVID-19 yielded similar results (Supplementary data, Tables S5 and S6).
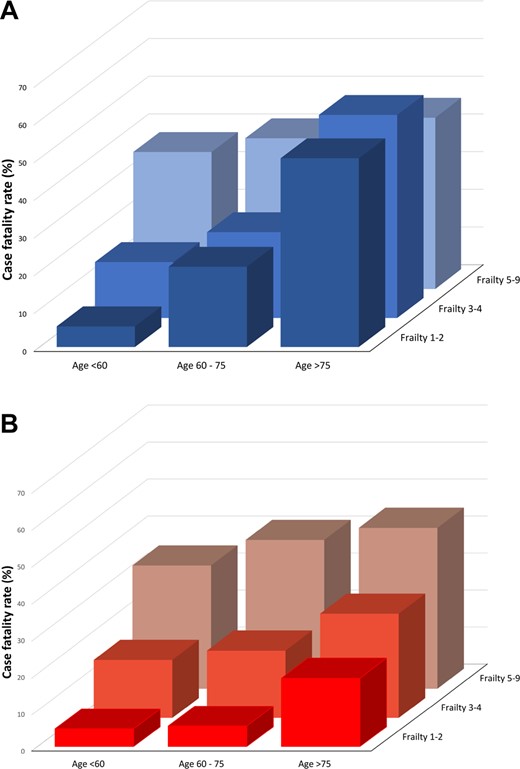
Relationship between age, clinical frailty score and 28-day case-fatality rate in (A) kidney transplant and (B) dialysis patients with COVID-19. Age and clinical frailty scores are subdivided into three clinical classes.
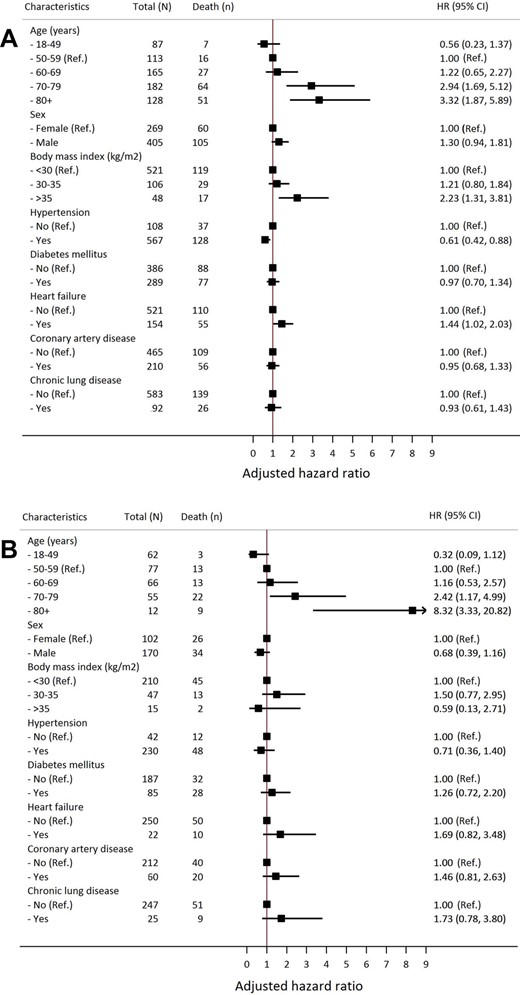
Association of demographic factors, major cardiovascular disease risk factors and chronic lung disease with 28-day mortality in dialysis and kidney transplant patients with COVID-19. Results are shown for a full adjusted multivariate model that includes the covariates shown in the graphs to allow comparison with data from the literature. Panel (A) shows results for patients on dialysis. Panel (B) shows results for patients living with a kidney transplant.
Univariable and multivariable Cox regression analysis of patient and disease-related factors at a presentation associated with a 28-day case-fatality rate in all kidney transplant (n = 305) and dialysis (n = 768) patients with COVID-19
| Characteristics . | Age and sex adjusted . | Multivariable . | ||||
|---|---|---|---|---|---|---|
| HRa . | 95% CI . | P-value . | HRa . | 95% CI . | P-value . | |
| Kidney transplant patients | ||||||
| Age, years | 1.08 | 1.06–1.11 | <0.001 | 1.07 | 1.04–1.10 | <0.001 |
| eGFR, mL/min/1.73 m2 | 0.98 | 0.97–1.00 | 0.03 | |||
| Primary kidney disease, yes versus no | ||||||
| Primary glomerulonephritis | 0.42 | 0.18–0.97 | 0.04 | |||
| Vascular disease | 2.03 | 1.0–3.83 | 0.03 | |||
| Comorbidity, yes versus no | ||||||
| Active malignancy | 2.00 | 1.02–3.93 | 0.04 | |||
| O2 saturation, % | 0.97 | 0.95–1.00 | 0.02 | |||
| Respiratory rate, /min | 1.08 | 1.05–1.12 | <0.001 | 1.07 | 1.03–1.11 | <0.001 |
| Log lymphocyte count | 0.72 | 0.54–0.96 | 0.03 | |||
| Log CRP | 1.48 | 1.17–1.86 | <0.001 | |||
| Dyspnoea, yes versus no | 2.77 | 1.60–4.79 | <0.001 | |||
| >25% higher creatinine, yes versus no | 2.10 | 1.27–3.50 | 0.004 | 1.89 | 1.05–3.40 | 0.03 |
| Use of prednisone, yes versus no | 2.09 | 0.95–4.59 | 0.07 | 2.88 | 1.03–8.03 | 0.04 |
| Dialysis patients | ||||||
| Age, year | 1.04 | 1.03–1.05 | <0.001 | 1.03 | 1.01–1.04 | 0.006 |
| Frailty, AU | 1.41 | 1.29–1.55 | <0.001 | 1.28 | 1.13–1.46 | <0.001 |
| Smoking status, versus never | ||||||
| Prior | 1.54 | 0.02–2.32 | 0.04 | |||
| Primary kidney disease, yes versus no | ||||||
| Vascular diseases | 1.49 | 1.06–2.09 | 0.02 | |||
| Comorbidity, yes versus no | ||||||
| Obesity | 1.49 | 1.06–2.10 | 0.02 | 1.87 | 1.18–2.95 | 0.007 |
| Hypertension | 0.61 | 0.44–0.85 | 0.004 | |||
| Heart failure | 1.39 | 1.02–1.89 | 0.04 | |||
| Status waiting list, versus not transplantable | ||||||
| Active or in prep for wait list | 0.19 | 0.09–0.40 | <0.001 | |||
| Temporary not on wait list | 0.42 | 0.20–0.91 | 0.03 | |||
| Temperature, °C | 1.54 | 1.31–1.80 | <0.001 | 1.61 | 1.30–1.98 | <0.001 |
| Respiratory rate, /min | 1.06 | 1.03–1.09 | <0.001 | |||
| O2 saturation, % | 0.94 | 0.92–0.97 | <0.001 | |||
| DBP, mmHg | 0.98 | 0.97–1.00 | 0.01 | |||
| Pulse, beats per min | 1.02 | 1.01–1.03 | <0.001 | 1.01 | 1.00–1.03 | 0.008 |
| Log lymphocyte count | 0.71 | 0.56–0.91 | 0.007 | |||
| Log CRP | 1.26 | 1.13–1.41 | <0.001 | |||
| Dyspnoea, yes versus no | 2.63 | 1.93–3.60 | <0.001 | 2.11 | 1.37–3.27 | <0.001 |
| Fever, yes versus no | 2.61 | 1.80–3.80 | <0.001 | |||
| Myalgia, yes versus no | 1.52 | 1.08–2.14 | 0.01 | |||
| Elevated liver transaminases, yes versus no | 1.97 | 1.17–3.34 | 0.01 | 2.81 | 1.55–5.08 | <0.001 |
| New HF or abnormal ECG, yes versus no | 1.86 | 1.19–2.90 | 0.006 | |||
| Characteristics . | Age and sex adjusted . | Multivariable . | ||||
|---|---|---|---|---|---|---|
| HRa . | 95% CI . | P-value . | HRa . | 95% CI . | P-value . | |
| Kidney transplant patients | ||||||
| Age, years | 1.08 | 1.06–1.11 | <0.001 | 1.07 | 1.04–1.10 | <0.001 |
| eGFR, mL/min/1.73 m2 | 0.98 | 0.97–1.00 | 0.03 | |||
| Primary kidney disease, yes versus no | ||||||
| Primary glomerulonephritis | 0.42 | 0.18–0.97 | 0.04 | |||
| Vascular disease | 2.03 | 1.0–3.83 | 0.03 | |||
| Comorbidity, yes versus no | ||||||
| Active malignancy | 2.00 | 1.02–3.93 | 0.04 | |||
| O2 saturation, % | 0.97 | 0.95–1.00 | 0.02 | |||
| Respiratory rate, /min | 1.08 | 1.05–1.12 | <0.001 | 1.07 | 1.03–1.11 | <0.001 |
| Log lymphocyte count | 0.72 | 0.54–0.96 | 0.03 | |||
| Log CRP | 1.48 | 1.17–1.86 | <0.001 | |||
| Dyspnoea, yes versus no | 2.77 | 1.60–4.79 | <0.001 | |||
| >25% higher creatinine, yes versus no | 2.10 | 1.27–3.50 | 0.004 | 1.89 | 1.05–3.40 | 0.03 |
| Use of prednisone, yes versus no | 2.09 | 0.95–4.59 | 0.07 | 2.88 | 1.03–8.03 | 0.04 |
| Dialysis patients | ||||||
| Age, year | 1.04 | 1.03–1.05 | <0.001 | 1.03 | 1.01–1.04 | 0.006 |
| Frailty, AU | 1.41 | 1.29–1.55 | <0.001 | 1.28 | 1.13–1.46 | <0.001 |
| Smoking status, versus never | ||||||
| Prior | 1.54 | 0.02–2.32 | 0.04 | |||
| Primary kidney disease, yes versus no | ||||||
| Vascular diseases | 1.49 | 1.06–2.09 | 0.02 | |||
| Comorbidity, yes versus no | ||||||
| Obesity | 1.49 | 1.06–2.10 | 0.02 | 1.87 | 1.18–2.95 | 0.007 |
| Hypertension | 0.61 | 0.44–0.85 | 0.004 | |||
| Heart failure | 1.39 | 1.02–1.89 | 0.04 | |||
| Status waiting list, versus not transplantable | ||||||
| Active or in prep for wait list | 0.19 | 0.09–0.40 | <0.001 | |||
| Temporary not on wait list | 0.42 | 0.20–0.91 | 0.03 | |||
| Temperature, °C | 1.54 | 1.31–1.80 | <0.001 | 1.61 | 1.30–1.98 | <0.001 |
| Respiratory rate, /min | 1.06 | 1.03–1.09 | <0.001 | |||
| O2 saturation, % | 0.94 | 0.92–0.97 | <0.001 | |||
| DBP, mmHg | 0.98 | 0.97–1.00 | 0.01 | |||
| Pulse, beats per min | 1.02 | 1.01–1.03 | <0.001 | 1.01 | 1.00–1.03 | 0.008 |
| Log lymphocyte count | 0.71 | 0.56–0.91 | 0.007 | |||
| Log CRP | 1.26 | 1.13–1.41 | <0.001 | |||
| Dyspnoea, yes versus no | 2.63 | 1.93–3.60 | <0.001 | 2.11 | 1.37–3.27 | <0.001 |
| Fever, yes versus no | 2.61 | 1.80–3.80 | <0.001 | |||
| Myalgia, yes versus no | 1.52 | 1.08–2.14 | 0.01 | |||
| Elevated liver transaminases, yes versus no | 1.97 | 1.17–3.34 | 0.01 | 2.81 | 1.55–5.08 | <0.001 |
| New HF or abnormal ECG, yes versus no | 1.86 | 1.19–2.90 | 0.006 | |||
Number of deaths in kidney transplant = 65 and in dialysis patients = 192.
For continuous variables, HR refers to per unit increase in a given variable.
AU, arbitrary units; CRP, C-reactive protein; eGFR, estimated glomerular filtration rate; O2, oxygen; DBP, diastolic blood pressure, HF, heart failure; ECG, electrocardiogram.
Univariable and multivariable Cox regression analysis of patient and disease-related factors at a presentation associated with a 28-day case-fatality rate in all kidney transplant (n = 305) and dialysis (n = 768) patients with COVID-19
| Characteristics . | Age and sex adjusted . | Multivariable . | ||||
|---|---|---|---|---|---|---|
| HRa . | 95% CI . | P-value . | HRa . | 95% CI . | P-value . | |
| Kidney transplant patients | ||||||
| Age, years | 1.08 | 1.06–1.11 | <0.001 | 1.07 | 1.04–1.10 | <0.001 |
| eGFR, mL/min/1.73 m2 | 0.98 | 0.97–1.00 | 0.03 | |||
| Primary kidney disease, yes versus no | ||||||
| Primary glomerulonephritis | 0.42 | 0.18–0.97 | 0.04 | |||
| Vascular disease | 2.03 | 1.0–3.83 | 0.03 | |||
| Comorbidity, yes versus no | ||||||
| Active malignancy | 2.00 | 1.02–3.93 | 0.04 | |||
| O2 saturation, % | 0.97 | 0.95–1.00 | 0.02 | |||
| Respiratory rate, /min | 1.08 | 1.05–1.12 | <0.001 | 1.07 | 1.03–1.11 | <0.001 |
| Log lymphocyte count | 0.72 | 0.54–0.96 | 0.03 | |||
| Log CRP | 1.48 | 1.17–1.86 | <0.001 | |||
| Dyspnoea, yes versus no | 2.77 | 1.60–4.79 | <0.001 | |||
| >25% higher creatinine, yes versus no | 2.10 | 1.27–3.50 | 0.004 | 1.89 | 1.05–3.40 | 0.03 |
| Use of prednisone, yes versus no | 2.09 | 0.95–4.59 | 0.07 | 2.88 | 1.03–8.03 | 0.04 |
| Dialysis patients | ||||||
| Age, year | 1.04 | 1.03–1.05 | <0.001 | 1.03 | 1.01–1.04 | 0.006 |
| Frailty, AU | 1.41 | 1.29–1.55 | <0.001 | 1.28 | 1.13–1.46 | <0.001 |
| Smoking status, versus never | ||||||
| Prior | 1.54 | 0.02–2.32 | 0.04 | |||
| Primary kidney disease, yes versus no | ||||||
| Vascular diseases | 1.49 | 1.06–2.09 | 0.02 | |||
| Comorbidity, yes versus no | ||||||
| Obesity | 1.49 | 1.06–2.10 | 0.02 | 1.87 | 1.18–2.95 | 0.007 |
| Hypertension | 0.61 | 0.44–0.85 | 0.004 | |||
| Heart failure | 1.39 | 1.02–1.89 | 0.04 | |||
| Status waiting list, versus not transplantable | ||||||
| Active or in prep for wait list | 0.19 | 0.09–0.40 | <0.001 | |||
| Temporary not on wait list | 0.42 | 0.20–0.91 | 0.03 | |||
| Temperature, °C | 1.54 | 1.31–1.80 | <0.001 | 1.61 | 1.30–1.98 | <0.001 |
| Respiratory rate, /min | 1.06 | 1.03–1.09 | <0.001 | |||
| O2 saturation, % | 0.94 | 0.92–0.97 | <0.001 | |||
| DBP, mmHg | 0.98 | 0.97–1.00 | 0.01 | |||
| Pulse, beats per min | 1.02 | 1.01–1.03 | <0.001 | 1.01 | 1.00–1.03 | 0.008 |
| Log lymphocyte count | 0.71 | 0.56–0.91 | 0.007 | |||
| Log CRP | 1.26 | 1.13–1.41 | <0.001 | |||
| Dyspnoea, yes versus no | 2.63 | 1.93–3.60 | <0.001 | 2.11 | 1.37–3.27 | <0.001 |
| Fever, yes versus no | 2.61 | 1.80–3.80 | <0.001 | |||
| Myalgia, yes versus no | 1.52 | 1.08–2.14 | 0.01 | |||
| Elevated liver transaminases, yes versus no | 1.97 | 1.17–3.34 | 0.01 | 2.81 | 1.55–5.08 | <0.001 |
| New HF or abnormal ECG, yes versus no | 1.86 | 1.19–2.90 | 0.006 | |||
| Characteristics . | Age and sex adjusted . | Multivariable . | ||||
|---|---|---|---|---|---|---|
| HRa . | 95% CI . | P-value . | HRa . | 95% CI . | P-value . | |
| Kidney transplant patients | ||||||
| Age, years | 1.08 | 1.06–1.11 | <0.001 | 1.07 | 1.04–1.10 | <0.001 |
| eGFR, mL/min/1.73 m2 | 0.98 | 0.97–1.00 | 0.03 | |||
| Primary kidney disease, yes versus no | ||||||
| Primary glomerulonephritis | 0.42 | 0.18–0.97 | 0.04 | |||
| Vascular disease | 2.03 | 1.0–3.83 | 0.03 | |||
| Comorbidity, yes versus no | ||||||
| Active malignancy | 2.00 | 1.02–3.93 | 0.04 | |||
| O2 saturation, % | 0.97 | 0.95–1.00 | 0.02 | |||
| Respiratory rate, /min | 1.08 | 1.05–1.12 | <0.001 | 1.07 | 1.03–1.11 | <0.001 |
| Log lymphocyte count | 0.72 | 0.54–0.96 | 0.03 | |||
| Log CRP | 1.48 | 1.17–1.86 | <0.001 | |||
| Dyspnoea, yes versus no | 2.77 | 1.60–4.79 | <0.001 | |||
| >25% higher creatinine, yes versus no | 2.10 | 1.27–3.50 | 0.004 | 1.89 | 1.05–3.40 | 0.03 |
| Use of prednisone, yes versus no | 2.09 | 0.95–4.59 | 0.07 | 2.88 | 1.03–8.03 | 0.04 |
| Dialysis patients | ||||||
| Age, year | 1.04 | 1.03–1.05 | <0.001 | 1.03 | 1.01–1.04 | 0.006 |
| Frailty, AU | 1.41 | 1.29–1.55 | <0.001 | 1.28 | 1.13–1.46 | <0.001 |
| Smoking status, versus never | ||||||
| Prior | 1.54 | 0.02–2.32 | 0.04 | |||
| Primary kidney disease, yes versus no | ||||||
| Vascular diseases | 1.49 | 1.06–2.09 | 0.02 | |||
| Comorbidity, yes versus no | ||||||
| Obesity | 1.49 | 1.06–2.10 | 0.02 | 1.87 | 1.18–2.95 | 0.007 |
| Hypertension | 0.61 | 0.44–0.85 | 0.004 | |||
| Heart failure | 1.39 | 1.02–1.89 | 0.04 | |||
| Status waiting list, versus not transplantable | ||||||
| Active or in prep for wait list | 0.19 | 0.09–0.40 | <0.001 | |||
| Temporary not on wait list | 0.42 | 0.20–0.91 | 0.03 | |||
| Temperature, °C | 1.54 | 1.31–1.80 | <0.001 | 1.61 | 1.30–1.98 | <0.001 |
| Respiratory rate, /min | 1.06 | 1.03–1.09 | <0.001 | |||
| O2 saturation, % | 0.94 | 0.92–0.97 | <0.001 | |||
| DBP, mmHg | 0.98 | 0.97–1.00 | 0.01 | |||
| Pulse, beats per min | 1.02 | 1.01–1.03 | <0.001 | 1.01 | 1.00–1.03 | 0.008 |
| Log lymphocyte count | 0.71 | 0.56–0.91 | 0.007 | |||
| Log CRP | 1.26 | 1.13–1.41 | <0.001 | |||
| Dyspnoea, yes versus no | 2.63 | 1.93–3.60 | <0.001 | 2.11 | 1.37–3.27 | <0.001 |
| Fever, yes versus no | 2.61 | 1.80–3.80 | <0.001 | |||
| Myalgia, yes versus no | 1.52 | 1.08–2.14 | 0.01 | |||
| Elevated liver transaminases, yes versus no | 1.97 | 1.17–3.34 | 0.01 | 2.81 | 1.55–5.08 | <0.001 |
| New HF or abnormal ECG, yes versus no | 1.86 | 1.19–2.90 | 0.006 | |||
Number of deaths in kidney transplant = 65 and in dialysis patients = 192.
For continuous variables, HR refers to per unit increase in a given variable.
AU, arbitrary units; CRP, C-reactive protein; eGFR, estimated glomerular filtration rate; O2, oxygen; DBP, diastolic blood pressure, HF, heart failure; ECG, electrocardiogram.
In kidney transplant recipients, we specifically addressed the incidence of severe forms of acute kidney injury. Loss of kidney function, necessitating the start of dialysis or continuous haemo(dia)filtration, occurred in 11% of hospitalized transplant patients (Table 2). Although mortality was not increased in patients within 1 year after transplantation (n = 23) as compared with those who were between 1 and 5 years after transplantation (n = 96), we explored how this risk relates to mortality in dialysis patients who were eligible for transplantation. The risk of mortality in dialysis patients who were on the waiting list for kidney transplantation (n = 85), or in work-up to be placed on the waiting list for transplantation (n = 63), was significantly lower compared with that in transplant patients who were in the first year after transplantation. In the subset of hospitalized patients, similar results were obtained (Table 4).
Risk of 28-day mortality in patients on the waiting list for kidney transplantation or in work-up to be placed on the waiting list for transplantation (n = 148, events = 8) versus those who received a transplant within 1 year before date of presentation (n = 23, events = 7) (presented are HRs from Cox proportional hazard model)
| Cox proportional hazard model . | HR . | 95% CI . | P-value . |
|---|---|---|---|
| In total study population | |||
| Crude | 0.16 | 0.06–0.46 | 0.001 |
| Age, sex and frailty adjusted | 0.20 | 0.07–0.56 | 0.002 |
| In those admitted to hospital | |||
| Crude | 0.17 | 0.06–0.50 | 0.001 |
| Age, sex and frailty adjusted | 0.20 | 0.06–0.61 | 0.004 |
| Cox proportional hazard model . | HR . | 95% CI . | P-value . |
|---|---|---|---|
| In total study population | |||
| Crude | 0.16 | 0.06–0.46 | 0.001 |
| Age, sex and frailty adjusted | 0.20 | 0.07–0.56 | 0.002 |
| In those admitted to hospital | |||
| Crude | 0.17 | 0.06–0.50 | 0.001 |
| Age, sex and frailty adjusted | 0.20 | 0.06–0.61 | 0.004 |
Risk of 28-day mortality in patients on the waiting list for kidney transplantation or in work-up to be placed on the waiting list for transplantation (n = 148, events = 8) versus those who received a transplant within 1 year before date of presentation (n = 23, events = 7) (presented are HRs from Cox proportional hazard model)
| Cox proportional hazard model . | HR . | 95% CI . | P-value . |
|---|---|---|---|
| In total study population | |||
| Crude | 0.16 | 0.06–0.46 | 0.001 |
| Age, sex and frailty adjusted | 0.20 | 0.07–0.56 | 0.002 |
| In those admitted to hospital | |||
| Crude | 0.17 | 0.06–0.50 | 0.001 |
| Age, sex and frailty adjusted | 0.20 | 0.06–0.61 | 0.004 |
| Cox proportional hazard model . | HR . | 95% CI . | P-value . |
|---|---|---|---|
| In total study population | |||
| Crude | 0.16 | 0.06–0.46 | 0.001 |
| Age, sex and frailty adjusted | 0.20 | 0.07–0.56 | 0.002 |
| In those admitted to hospital | |||
| Crude | 0.17 | 0.06–0.50 | 0.001 |
| Age, sex and frailty adjusted | 0.20 | 0.06–0.61 | 0.004 |
DISCUSSION
The ERACODA database is a large European data set containing detailed individual patient data, facilitating well-powered analyses of risk factors for mortality in dialysis and transplant patients with COVID-19. The results of our study show that mortality in kidney transplant and dialysis patients with COVID-19 is high and primarily associated with advanced age and frailty, while hypertension, diabetes mellitus, coronary artery disease, heart failure and chronic lung disease did not emerge as independent risk factors in our analysis. After adjusting for age, sex and frailty, we observed no significant difference in in-hospital mortality between kidney transplant and dialysis patients.
For kidney transplant patients, our study shows a 28-day probability of death of 21.3%. Several small case series with varying patient selection and duration of follow-up reported case-fatality rates in kidney transplant patients ranging from 6% to 28% [15–17]. Previous studies of COVID-19 in the general population have also reported a wide range of death rates due to differences in demographics and selection of patients [4–8]. Reported in-hospital case-fatality rates were 10.2%, 15.6% and 20.3% in cohorts from the general population with median ages of 62, 61 and 63 years, respectively [4–6]. In comparison, our finding of 23.6% in-hospital case-fatality rate in a cohort with a mean age of 60 ± 13 years suggests that the COVID-19-related mortality rate of transplant patients is higher than in the general population. A similar view emerges when we compare our data to age-group-specific case-fatality rates reported in European countries. For all age groups, mortality is substantially higher in transplant and dialysis patients as compared with the general population (Table 5). It is important to note that case-fatality rates of the general population and our cohort must be compared with caution, since demographics, case ascertainment as well as follow-up periods differ. We noticed that mortality was very low in transplant and dialysis patients who were not hospitalized, indicating that clinical judgment at presentation correctly identified those patients who could be safely managed at home.
Case-fatality rates in the ERACODA database and the European general population overall, across both sexes and across age groups.
| . | ERACODA . | General . | |
|---|---|---|---|
| Characteristics . | Transplantation (%) . | Dialysis (%) . | Population (%) . |
| All | 21.6 | 25.6 | 11.4 |
| Sex | |||
| Males | 18.9 | 27.4 | 15.0 |
| Females | 26.0 | 23.0 | 8.3 |
| Age (years) | |||
| 30–40 | 14.3 | 9.1 | 0.3 |
| 40–50 | 5.7 | 6.5 | 1.1 |
| 50–60 | 14.9 | 16.8 | 2.8 |
| 60–70 | 17.5 | 18.8 | 9.4 |
| 70–80 | 38.6 | 34.8 | 21.8 |
| 80–90 | 71.4 | 39.5 | 29.0 |
| . | ERACODA . | General . | |
|---|---|---|---|
| Characteristics . | Transplantation (%) . | Dialysis (%) . | Population (%) . |
| All | 21.6 | 25.6 | 11.4 |
| Sex | |||
| Males | 18.9 | 27.4 | 15.0 |
| Females | 26.0 | 23.0 | 8.3 |
| Age (years) | |||
| 30–40 | 14.3 | 9.1 | 0.3 |
| 40–50 | 5.7 | 6.5 | 1.1 |
| 50–60 | 14.9 | 16.8 | 2.8 |
| 60–70 | 17.5 | 18.8 | 9.4 |
| 70–80 | 38.6 | 34.8 | 21.8 |
| 80–90 | 71.4 | 39.5 | 29.0 |
The data shown in this table are average data for the 10 countries that added most patients to the database (Spain 200, the Netherlands 167, Romania 127, Italy 104, Switzerland 95, Turkey 81, Belgium 56, UK 41, Portugal 39 and Poland 22 patients). The data for the general population are obtained from these 10 countries (average weighted for the number of patients added to ERACODA). Data for the general population of these countries were derived on 8 June 2020 from https://en.wikipedia.org/wiki/COVID-19_pandemic_in_Europe.
Case-fatality rates in the ERACODA database and the European general population overall, across both sexes and across age groups.
| . | ERACODA . | General . | |
|---|---|---|---|
| Characteristics . | Transplantation (%) . | Dialysis (%) . | Population (%) . |
| All | 21.6 | 25.6 | 11.4 |
| Sex | |||
| Males | 18.9 | 27.4 | 15.0 |
| Females | 26.0 | 23.0 | 8.3 |
| Age (years) | |||
| 30–40 | 14.3 | 9.1 | 0.3 |
| 40–50 | 5.7 | 6.5 | 1.1 |
| 50–60 | 14.9 | 16.8 | 2.8 |
| 60–70 | 17.5 | 18.8 | 9.4 |
| 70–80 | 38.6 | 34.8 | 21.8 |
| 80–90 | 71.4 | 39.5 | 29.0 |
| . | ERACODA . | General . | |
|---|---|---|---|
| Characteristics . | Transplantation (%) . | Dialysis (%) . | Population (%) . |
| All | 21.6 | 25.6 | 11.4 |
| Sex | |||
| Males | 18.9 | 27.4 | 15.0 |
| Females | 26.0 | 23.0 | 8.3 |
| Age (years) | |||
| 30–40 | 14.3 | 9.1 | 0.3 |
| 40–50 | 5.7 | 6.5 | 1.1 |
| 50–60 | 14.9 | 16.8 | 2.8 |
| 60–70 | 17.5 | 18.8 | 9.4 |
| 70–80 | 38.6 | 34.8 | 21.8 |
| 80–90 | 71.4 | 39.5 | 29.0 |
The data shown in this table are average data for the 10 countries that added most patients to the database (Spain 200, the Netherlands 167, Romania 127, Italy 104, Switzerland 95, Turkey 81, Belgium 56, UK 41, Portugal 39 and Poland 22 patients). The data for the general population are obtained from these 10 countries (average weighted for the number of patients added to ERACODA). Data for the general population of these countries were derived on 8 June 2020 from https://en.wikipedia.org/wiki/COVID-19_pandemic_in_Europe.
A potential explanation for the relatively high mortality in kidney transplant patients is the high prevalence of impaired kidney function, which has been demonstrated to be a strong risk factor for mortality in patients with COVID-19 [7–9, 12]. In accordance with a previous study, we found that also a worsening of kidney function at presentation was independently associated with mortality [12]. Other factors at presentation associated with 28-day case-fatality in kidney transplant patients were age, respiration rate and use of prednisone prior to admission. The association between prednisone use prior to admission and outcome should be more closely examined in future studies.
We observed that in the hospitalized kidney transplant patients in our cohort, mycophenolate and tacrolimus were often reduced or discontinued and prednisone was often increased, in accordance with published opinion-based guidelines [24]. Our data did not allow evaluation of whether higher doses of corticosteroids had beneficial effects, as was recently demonstrated for short-term dexamethasone treatment in patients with COVID-19 receiving oxygen with or without invasive mechanical ventilation [25]. Cessation of immunosuppressive medication occurred especially in patients with severe disease who required ICU admission. Future studies should evaluate whether this strategy is effective for improving outcomes in COVID-19 and whether it is safe with respect to graft function and transplant rejection.
We observed that the 28-day mortality of kidney transplant patients within their first year after transplantation was higher than that of dialysis patients who were on the kidney transplant waiting list or in preparation for placement on the waiting list. While this might impact the decision to undergo transplantation during the COVID-19 pandemic, several aspects need consideration when interpreting this observation. First, this observation was based on a relatively small subset of patients with only 15 events. Secondly, the risk of dying from COVID-19 largely depends on the risk of contracting a SARS-CoV-2 infection, which can vary widely at different stages of the pandemic and across regions, and may differ between transplant and dialysis patients. Thirdly, long-term outcomes have to be taken into account since chronic dialysis treatment is associated with an increased risk of morbidity and mortality. Finally, the availability of resources to provide adequate care to transplant and dialysis patients and individual patient factors such as age, frailty, the need for lymphocyte depleting induction therapy and the urgency of a kidney transplantation should be assessed. In our opinion, the risk for mortality in the first year after kidney transplantation may not exceed the risk associated with the continuation of dialysis when the prevalence of SARS-CoV-2 infection in the general population is low.
In dialysis patients, COVID-19-related 28-day case-fatality rate was 25.0% for all patients in our study and 33.5% for patients who were admitted in hospital. A recent report from the COVID-19 registry of the Spanish Society of Nephrology showed a case-fatality rate of 24.9% in nearly 600 dialysis patients, although follow-up was limited to <3 weeks in the majority of patients [19]. In dialysis patients who died in our study, only a minority was admitted to the ICU, suggesting the presence of advanced care planning in this population.
In dialysis patients, the clinical frailty score at presentation was the strongest predictor of mortality. In multivariable analysis, the association between frailty and mortality was even stronger than the association between age and mortality, which was opposite to the situation in kidney transplant patients. Although this finding may be explained by a power issue (there are more dialysis patients with a wider range in clinical frailty scores as compared with kidney transplant patients), it could also be that in every age category the least frail dialysis patients receive a kidney transplant, so that frailty will be more strongly associated with outcome in dialysis than in kidney transplant patients. Whatever the explanation of this finding may be, this indicates that the easy-to-use clinical frailty score rather than chronological age should be used to guide treatment decisions in dialysis patients with COVID-19 requiring critical care organ support and in advanced care planning.
Our study has limitations. The database may not include all patients with COVID-19 in the participating centres, which can lead to selection bias. However, when we limited our analyses to the subsets of patients that were likely representative for an unselected population of COVID-19 patients, similar results were obtained. In addition, patients may have contracted SARS-CoV-2 infection without contacting a medical centre. Theoretically, patients with no or mild symptoms may therefore be underrepresented in our database. Such bias is not expected to be important, because kidney transplant and dialysis patients are in general under close medical follow-up, and therefore will likely present themselves when having complaints. Some patients were still in hospital after 28 days of follow-up. It is unclear whether they are still at risk of dying or whether they have passed the critical disease stage and are in a recovery phase. However, the Kaplan–Meier curve visualizes that the majority of deaths occur within the first 2 weeks after presentation. The present 28-day vital status data will therefore be only a minor underestimation of the final case-fatality rate. Lastly, although our database contains a wealth of granular individual patient-level information, a confounding effect of other unmeasured parameters cannot be excluded.
The major strengths of the ERACODA database are that it prospectively collects data from many centres across Europe, and that it is specifically dedicated to gathering information on patients with kidney disease. It encompasses a large multi-centre dataset with granular information on individual patient, disease as well as treatment characteristics which allows detailed analyses. In addition to mortality, we also report on ICU admission, need for ventilator support and need for renal replacement therapy. The dataset includes information on frailty, a factor that is considered important for clinical decision-making, but only rarely collected in COVID-19 registries. Moreover, kidney transplant as well as dialysis patients are included, which makes it possible to compare risk in these two patient groups.
In summary, 28-day case-fatality rate was high in kidney transplant and dialysis patients, especially in those admitted in hospital. Mortality was primarily associated with advanced age in kidney transplant patients and with age and frailty in dialysis patients. Our findings are important in guiding clinical decision-making, and for informing the public and healthcare authorities on the COVID-19-related mortality risk in kidney transplant and dialysis patients.
SUPPLEMENTARY DATA
Supplementary data are available at ndt online.
ACKNOWLEDGEMENTS
The ERACODA collaboration is an initiative to study prognosis and risk factors for mortality due to COVID-19 in patients with a kidney transplant or on dialysis that is endorsed by the ERA-EDTA. ERACODA is an acronym for European Renal Association COVID-19 Database. The organizational structure contains a Working Group assisted by a Data Management Team and Advisory Board. The ‘ERACODA Working Group’ members are C.F.M.F. (Lead Dialysis Subdatabase), R.T.G. (ERA-EDTA Council Member and Overall Coordination), M.H.H. (Director Dutch Renal Registry), L.B.H. (Lead Transplant Subdatabase) and K.J.J. (Director ERA-EDTA Registry). The ‘ERACODA Data Management Team’ members are L.M.K. (Lead Study Coordinator and Epidemiologist), M.J.P. (Epidemiologist) and H.d.V. (Study Coordinator). The ‘ERACODA Advisory Board’ members are D. Abramowicz, C. Basile, A.C., M.C., Z.A.M. (Co-chair), S. Mitra and J.E.S. (Co-chair). Collaborators that entered data in ERACODA remain the owner of these data. The database can therefore not be disclosed to any third party without the prior written consent of all data providers, but the database will be made available to the Editorial office of the Nephrology Dialysis Transplantation. Research proposals can be submitted to the Working Group via [email protected]. If deemed of interest and methodological sound by the Working Group, Advisory Board and User Panel, the analyses needed for the proposal will be carried out by the Data Management Team. We thank all people that entered information in the ERACODA database for their participation, and especially all healthcare workers that have taken care of the included COVID-19 patients.
ERACODA Collaborating Authors
Affiliations and names of collaborative authors, and the number of records entered in the ERACODA database between brackets.
Albert Schweitzer Hospital, Dordrecht, the Netherlands (3)
- Jeroen B. van der Net, M.D., Ph.D.
Ambroise Pare Hospital, APHP Paris-Saclay University, Boulogne Billancourt, France (8)
- Marie Essig, M.D., Ph.D.
Amphia Hospital, Breda, the Netherlands (11)
- Peggy W.G. du Buf-Vereijken, M.D., Ph.D.
- Betty van Ginneken
- Nanda Maas
Amsterdam UMC, Amsterdam, the Netherlands (26)
- Liffert Vogt, M.D., Ph.D.
- Birgit C. van Jaarsveld, M.D, Ph.D.
- Frederike J. Bemelman, M.D, Ph.D.
- Farah Klingenberg-Salahova, M.D.
- Frederiek Heenan-Vos, M.D., Ph.D.
- Marc G. Vervloet M.D., Ph.D.
- Azam Nurmohamed, M.D., Ph.D.
Antwerp University Hospital, Antwerp, Belgium (10)
- Daniel Abramowicz, M.D., Ph.D.
- Sabine Verhofstede
Avicennes Military Hospital, Faculty of Medicine, Cadi Ayyad University , Marrakech Morocco (2)
- Omar Maoujoud, M.D., Ph.D.
B. Braun Avitum, Litomerice, Czech Republic (1)
- Jana Fialova, M.D.
Bellvitge University Hospital, Hospitalet de Llobregat, Barcelona, Spain (31)
- Edoardo Melilli, M.D., Ph.D.
- Alex Favà, M.D.
- Josep M. Cruzado
Bernhoven Hospital, Uden, the Netherlands (14)
- Joy Lips, M.D.
Catharina Hospital, Eindhoven, the Netherlands (18)
- Maaike Hengst, MSc.
Centre of Postgraduate Medical Education, Poland (1)
- Ryszard Gellert
Central Clinical Hospital of the Ministry of Interior, Warsaw, Poland (20)
- Andrzej Rydzewski, M.D., Ph.D.
Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal (3)
- Daniela G. Alferes, M.D.
Charles University, Prague, Czech Republic (1)
- Ivan Rychlik, M.D., Ph.D
City Hospital n.a. S.P. Botkin, Moscow, Russia (2)
- Elena V. Zakharova, M.D., Ph.D.
City Hospital Waid, Zürich, Switzerland (92)
- Patrice Max Ambuehl
Claude Galien Hospital Ramsay santé, Quincy-sous-Sénart, France (29)
- Fanny Lepeytre, M.D.
- Clémentine Rabaté, M.D.
- Guy Rostoker, M.D., Ph.D.
Clínica de Hemodiálise de Felgueiras, Felgueiras, Portugal (3)
- Sofia Marques, M.D.
Clinical Centre of Vojvodina, Novi Sad, Serbia (3)
- Tijana Azasevac, M.D.
Croatian Society of Nephrology, Dialysis and Transplantation, Croatia (5)
- Dajana Katicic, M.D.
CWZ Nijmegen, Nijmegen, the Netherlands (2)
- Marc ten Dam
DaVita Geilenkirchen, Geilenkirchen, Germany (2)
- Thilo Krüger, M.D., Ph.D.
Dianet Dialysis Center, Utrecht, the Netherlands (5)
- Susan J.J. Logtenberg, M.D., Ph.D.
Dialysis Center Bochum, Bochum, Germany (2)
- Lutz Fricke, M.D., Ph.D.
Deventer Ziekenhuis, Deventer, the Netherlands (2)
- A.L. van Zanen
Elyse Klinieken voor Nierzorg, Kerkrade, the Netherlands (4)
- Jeroen J.P. Slebe, M.D.
Erasme Hospital, Brussels, Belgium (11)
- Delphine Kemlin
Erasmus Medical Center, Rotterdam, the Netherlands (5)
- Jacqueline van de Wetering, M.D., Ph.D.
Faculty of Medicine in Pilsen, Charles University, Pilsen, Czech Republic (1)
- Jaromir Eiselt
- Lukas Kielberger
Faculty of Medicine-Alexandria University, Alexandria, Egypt (7)
- Hala S. El-Wakil, M.D., Ph.D.
Epidemiology department - High Institute of Public Health - Alexandria University – Egypt (1)
- Samar Abd ElHafeez, MD, Dr.PH
Fundación Jiménez Díaz, Madrid, Spain (6)
- Christina Canal, M.D., Ph.D.
- Carme Facundo, M.D., Ph.D.
- Ana M. Ramos, M.D., Ph.D.
Gdansk Medical University, Gdansk, Poland (10)
- Alicja Debska-Slizien, M.D., Ph.D.
Gelre Hospital, Apeldoorn, the Netherlands (1)
- Nicoline M.H. Veldhuizen, M.D.
General University Hospital of Alexandroupolis, Alexandroupolis, Greece (2)
- Stylianos Panagoutsos
Grigore T Popa University of Medicine and Pharmacy, Iasi, Romania / Dr Ci Parhon Hospital, Iasi, Romania (165)
- Irina Matceac, M.D.
- Ionut Nistor, M.D., Ph.D.
- Monica Cordos, M.D.
Haaglanden Medisch Centrum, the Hague, the Netherlands (5)
- J.H.M. Groeneveld, M.D.
Haga Hospital, the Hague, the Netherlands (2)
- Marjolijn van Buren, M.D., Ph.D.
Hospital Clínic de Barcelona, Barcelona, Spain (1)
- Fritz Diekmann
Hospital Curry Cabral - Central Lisbon University Hospital Center, Lisbon, Portugal (9)
- Ana C. Ferreira, M.D.
HC-UFMG, CMN Contagem-MG, Unimed-BH, Brazil (1)
- Augusto Cesar S. Santos Jr., M.D., Ph.D.
Hospital del Mar, Barcelona, Spain (35)
- Carlos Arias-Cabrales, M.D.
- Laura Llinàs-Mallol, MSc.
- Anna Buxeda, M.D.
- Carla Burballa Tàrrega, M.D.
- Dolores Redondo-Pachon, M.D., Ph.D.
- Maria Dolores Arenas Jimenez, M.D.
Hospital Gelderse Vallei, Ede, the Netherlands (1)
- Julia M. Hofstra, M.D., Ph.D.
Hospital General of Alicante, Alicante, Spain (5)
- Antonio Franco
Hospital General Universitario Gregorio Marañón, Madrid, Spain (71)
- María L. Rodríguez-Ferrero, M.D.
Hospital Obispo Polanco, Salud Aragón, Spain (4)
- Sagrario Balda Manzanos, M.D., Ph.D.
Hospital Universitario de Guadalajara, Guadalajara, Spain (15)
- Gabriel de Arriba, M.D., Ph.D.
Hospital Universitario Ramón y Cajal, Madrid, Spain (1)
- R. Haridian Sosa Barrios, M.D. MSc
Isala, Zwolle, the Netherlands (5)
- Karlijn Bartelet, M.D.
Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey (28)
- Erol Demir, M.D.
Jeroen Bosch Ziekenhuis, Den Bosch, the Netherlands (8)
- Daan A.M.J. Hollander, M.D., Ph.D.
- Angele Kerckhoffs, M.D., Ph.D.
Klinikum Aschaffenburg-Alzenau, Aschaffenburg, Germany (2)
- Stefan Büttner, M.D.
Leiden University Medical Center, Leiden, the Netherlands (15)
- Aiko P.J. de Vries, M.D., Ph.D.
- Soufian Meziyerh, M.D.
- Danny van der Helm, M.Sc.
- Marlies Reinders, M.D., Ph.D.
- Hanneke Bouwsma, M.D.
Lithuanian University of Health Sciences, Lithuania (6)
- Kristina Petruliene, M.D., Ph.D.
Luzerner Kantonsspital, Luzern, Switzerland (1)
- Sharon Maloney
Maasstad Ziekenhuis, Rotterdam, the Netherlands (1)
- Iris Verberk
Marche Nord Hospital, Pesaro, Italy (19)
- Marina Di Luca, M.D., Ph.D.
Marmara University School of Medicine, Istanbul, Turkey (19)
- Serhan Z. Tuğlular, M.D.
Maxima Medisch Centrum, Veldhoven, the Netherlands (5)
- Charles Beerenhout
Meander Medisch Centrum, Amersfoort, the Netherlands (3)
- Peter T. Luik, M.D., Ph.D.
Medical University Innsbruck, Innsbruck, Austria (4)
- Julia Kerschbaum, M.D.
- Martin Tiefenthaler
Medical University of Vienna, Vienna, Austria (3)
- Bruno Watschinger, M.D.
Medisch Centrum Leeuwarden, Leeuwarden, the Netherlands (3)
- Aaltje Y. Adema, M.D., Ph.D.
Moscow Regional Research and Clinical Institute, Moscow, Russia (23)
- Vadim A. Stepanov, M.D., Ph.D.
- Alexey B. Zulkarnaev, M.D., Ph.D.
Necmettin Erbakan University Meram School of Medicine, Konya, Turkey (6)
- Kultigin Turkmen, M.D.
Nephrology and Dialysis - AUSL Modena, Modena, Italy (1)
- Bonucchi Decenzio
Nierenzentrum Reutlingen-Tübingen, Reutlingen, Germany (11)
- Anselm Fliedner, M.D.
Okinawa chubu hospital, Japan (1)
- Hitoshi Miyasato
The Norwegian Renal Registry, Oslo University Hospital – Rikshospitalet, Olso, Norway (28)
- Anders Åsberg, Ph.D.
- Geir Mjoen, Ph.D.
Padua University Hospital, Padua, Italy (3)
- Stefano Pini, M.D.
Radboud University Medical Center, Nijmegen, the Netherlands (15)
- Consuelo de Biase, M.D.
- Anne Els van de Logt
- Rutger Maas
Regional clinical hospital, Yaroslavl, Russia (26)
- Olga Lebedeva, M.D.
Regional Hospital of Malaga, Malaga, Spain (2)
- Veronica Lopez, M.D., Ph.D.
Rijnstate Hospital, Arnhem, the Netherlands (8)
- Louis J.M. Reichert, M.D., Ph.D.
- Jacobien Verhave, M.D., Ph.D.
RUDN university, Russia (6)
- Denis Titov
Saint-Petersburg State University Hospital, Saint-Petersburg, Russia (11)
- Ekaterina V. Parshina, M.D.
Sint Antonius Ziekenhuis, Nieuwegein, the Netherlands (2)
- Liesbeth E.A. van Gils-Verrij, drs.
Slingeland Ziekenhuis, Doetinchem, Netherlands (2)
- Charlotte J.R. de Bruin, M.D.
Southern Health and Social Care Trust, Newry, Northern Ireland (4)
- John C. Harty, M.D.
Spaarne Gasthuis, Haarlem, the Netherlands (6)
- Marleen Meurs, M.D.
SPWSZ Hospital, Szczecinie, Poland (8)
- Marek Myslak
St. Anna University Hospital, Ferrara, Italy (6)
- Yuri Battaglia, M.D., Ph.D.
St. Bassiano Hospital, Bassano del Grappo, Italy (7)
- Paolo Lentini, M.D., Ph.D.
Streekziekenhuis Koningin Beatrix, Winterswijk, the Netherlands (1)
- Edwin den Deurwaarder
Tehran university of medical sciences, Theran, Iran (5)
- Hormat Rahimzadeh, M.D.
Tergooi, Hilversum, the Netherlands (1)
- Marcel Schouten, M.D., Ph.D.
Toledo University Hospital, Toledo, Spain (49)
- Carlos J. Cabezas-Reina, M.D.
University Clinical Hospital of Santiago de Compostela, Santiago de Compostela, Spain (3)
- Anabel Diaz-Mareque, M.D.
University Clinical Hospital of Valladolid, Valladolid, Spain (14)
- Armando Coca, M.D., Ph.D.
University Hospital Leuven, Leuven, Belgium (12)
- Björn K.I. Meijers, M.D., Ph.D.
- Maarten Naesens, M.D., Ph.D.
- Dirk Kuypers, M.D., Ph.D.
- Bruno Desschans
University Hospital Brussels, Brussels, Belgium (1)
- Annelies Tonnerlier
- Karl M. Wissing
University Hospital Martin and Jessenius Faculty of Medicine Comenius University, Martin, Slovakia (3)
- Ivana Dedinska, M.D., Ph.D.
University Hospital Medical Center Verona, Verona, Italy (7)
- Giuseppina Pessolano, M.D.
University Hospital of Maastricht, Maastricht, the Netherlands (10)
- Frank M. van der Sande, M.D., Ph.D.
- Maarten H.L Christiaans, M.D., Ph.D.
University Hospital Parma, Parma, Italy (4)
- Ilaria Gandolfini, M.D.
- Umberto Maggiore
University Hospital UC Louvain, Cliniques Universitaires Saint-Luc, Brussels, Belgium (45)
- Nada Kanaan, M.D.
- Laura Labriola, M.D.
- Arnaud Devresse, M.D.
University Hospitals of Coventry and Warwickshire NHS Trust, Coventry, United Kingdom (1)
- Shafi Malik, M.D.
University Medical Center Groningen, Groningen, the Netherlands (16)
- Stefan P. Berger, M.D., Ph.D.
- Esther Meijer, M.D., Ph.D.
- Jan Stephan F. Sanders, M.D., Ph.D.
University Medical Center Ljubljana, Ljubljana, Slovenia (7)
- Jadranka Buturović Ponikvar, M.D., Ph.D.
University Medical Center Utrecht, Utrecht, the Netherlands (18)
- Alferso C. Abrahams, M.D., Ph.D.
- Femke M. Molenaar, M.D.
- Arjan D. van Zuilen, M.D., Ph.D.
- S.C.A. Meijvis
- Helma Dolmans
San Marco Hospital, University of Catania, Catania, Italy (2)
- Luca Zanoli, M.D., Ph.D.
- Carmelita Marcantoni, M.D.
University of Genoa, Genoa, Italy (9)
- Pasquale Esposito, M.D., Ph.D.
University of Liège, Liège, Belgium (3)
- Jean-Marie Krzesinski, M.D., Ph.D.
- Jean Damacène Barahira, MPH
University of Milan, Milan, Italy (18)
- Maurizio Gallieni, M.D.
- Gianmarco Sabiu, M.D. University of Navarra Clinic, Pamplona, Spain (1)
- Paloma Leticia Martin-Moreno
University of Piemonte Orientale, Novara, Italy (25)
- Gabriele Guglielmetti, M.D.
Valais Hospital, Sion, Switzerland (7)
- Gabriella Guzzo, M.D.
VieCuri Medical Centre, Venlo, the Netherlands (13)
- Antinus J. Luik, M.D., Ph.D.
- Willi H.M. van Kuijk, M.D., Ph.D.
- Lonneke W.H. Stikkelbroeck, M.D.
- Marc M.H. Hermans, M.D., Ph.D.
Vilnius University, Vilnius, Lithuania (5)
- Laurynas Rimsevicius, M.D., Ph.D.
Vimercate Hospital, Vimercate, Italy (12)
- Marco Righetti, M.D.
Zuyderland Medical Center, Geleen and Heerlen, the Netherlands (10)
- Nicole Heitink-ter Braak
FUNDING
The ERACODA Consortium is financially supported by unrestricted grants from the ERA-EDTA, the Dutch Kidney Foundation, Baxter and Sandoz. None of these organizations had any role in the design or execution of the study, nor in writing of the manuscript.
AUTHORS’ CONTRIBUTIONS
All authors contributed to data collection, study design, data analysis, interpretation and drafting of this article. The data were analysed by three of the authors (L.M.K., M.J.P. and P.V.), who vouch for the analysis. Ten of the authors vouch for the accuracy of the data (L.B.H., R.D., P.V., C.F.M.F., M.H.H., K.J.J., L.M.K., M.J.P., H.d.V. and R.T.G.). The first, second and last authors (L.B.H., R.D. and R.T.G) prepared the first draft of the manuscript. All authors had full access to the data and were responsible for the decision to submit the manuscript for publication.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
COVID-19 Cases and Case Fatality Rate by age. https://ec.europa.eu/knowledge4policy/sites/know4pol/files/jrc120420_covid_risk_and_age.pdf (6 October 2020, date last accessed)
GBD Chronic Kidney Disease Collaboration.
Clinical Frailty Scale. https://www.nice.org.uk/guidance/ng159/resources/clinical-frailty-scale-pdf-8712262765 (1 September 2020, date last accessed)
Author notes
Additional ERACODA Collaborators are listed in the Acknowledgements.





Comments