-
PDF
- Split View
-
Views
-
Cite
Cite
Mickael Tordjman, Clara Pouchelon, Etienne Canouï, Manel Omri, Elisabeth Dion, Sternal mass caused by Mycobacterium tuberculosis in an immunocompetent young adult, Journal of Travel Medicine, Volume 28, Issue 6, August 2021, taab021, https://doi.org/10.1093/jtm/taab021
Close - Share Icon Share
A 24-year-old patient presented to our centre in July 2020, with a 2-month history of an anterior non-painful thoracic mass, measured at 9 cm, well limited, flexible (Figure 1A and B). The patient was a migrant from Sudan and lived in France for the past 4 months. He was tired and recently lost weight (about 10 kg in the last 2 months) but presented neither night sweat nor clinical lymphadenopathy. His medical history included malaria 5 years ago. His temperature was normal [36.4°C (97.5°F)] as well as the rest of his vital signs. A chest X-ray and ultrasound were performed, demonstrating an anterior mass adjacent to the sternum with no lytic bone lesion (Figure 1D). This mass was mostly cystic with intralesional walls vascularized using power Doppler ultrasound (Figure 1C). His biological examination showed a C-Reactive Protein (CRP) at 124 mg/L and 9.35 G/L leukocytes with 7.74 G/L neutrophils. Magnetic resonance imaging (MRI) and computed tomography (CT) scan were then performed. The sternal mass centred on the manubriosternal joint demonstrated low-signal intensity on T1-weighted images, with peripheral high T1 intensity on pre-contrast images, and high signal intensity on T2-weighted images as compared to adjacent muscles with peripheral enhancement after gadolinium chelates injection (Figure 1E–G). Manubriosternal joint presented small erosions on CT (Figure 1H) and no lytic or condensing bone lesion. Needle aspiration of the sternal mass found purulent fluid containing altered neutrophils and no malignant cell and was submitted for culture. The culture was positive for Mycobacterium tuberculosis with a final diagnosis of sternal tuberculosis. Acid-fast bacillus testing on sputum was examined to rule out open pulmonary tuberculosis and was negative. The M. tuberculosis was susceptible to all anti-tuberculosis drugs tested. Viral antibody tests including hepatitis B virus (HBV), hepatitis C virus (HCV) and human immunodeficiency virus (HIV) were negative. A thoraco-abdominopelvic CT scan demonstrated lung micronodules, mesenteric lymphadenopathies, bone (spine) and cerebral lesions compatible with abscesses. The patient was treated with anti-tuberculous therapy (isoniazid, rifampicin, pyrazinamide and ethambutol). He gained weight and is currently well after 3 months of treatment. The envisaged total time of treatment is 12 months.
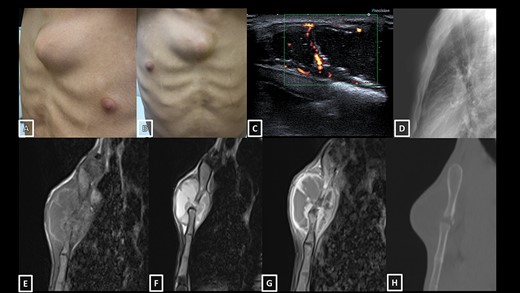
(A and B) Photographs show a medial sternal isolated mass with no cutaneous fistula; (C) Power Doppler ultrasound image showing mostly cystic mass with intralesional walls vascularization; (D) Lateral chest X-ray showing the sternal mass; (E) T1-weighted MRI of the sternal mass shows a slightly hyperintense rim; (F) T2-weighted image shows a heterogeneous cystic mass centred on the manubriosternal joint, compatible with an abscess (middle, arrow); (G) contrast-enhanced T1-weighted image shows enhancement of the walls (right, arrows) and (H) CT scan showing small erosions of the manubriosternal joint.
Sternal tuberculosis is an unusual entity and the presentation can be misleading because the sternum is an unusual location of infection and in particular of mycobacterial infections. Primary sternal tuberculosis accounts for approximately 0.3% of tubercular osteomyelitis locations.1 Differential diagnoses include malignant lesions such as sarcoma. Diagnosis is often delayed but imaging can orientate the diagnosis. In the previous cases described in the literature, patients were often immunocompetent.2,3 Patients with sternal tuberculosis often presented with a sternal abscess associated with osteomyelitis of the sternum. The sternoclavicular joint can also be involved.4 A few cases of sternal tuberculosis have been described after sternotomy.5 In our case, MRI showed a sternal collection centred on the manubriosternal joint with a slightly hyperintense rim on T1-weighted pre-contrast images, with enhancement after gadolinium injection, compatible with tuberculosis. Additional tuberculosis locations should be searched. In case of culture-negative tuberculosis (TB) abscess, microscopy of an acid-fast stained smear or Polymerase chain reaction (PCR) is diagnostic options.
Funding
None.
Conflict of interest
None declared.



