-
PDF
- Split View
-
Views
-
Cite
Cite
R O’Donnell, A Amos, S W Turner, L Adams, T Henderson, S Lyttle, S Mitchell, S Semple, ‘They only smoke in the house when I’m not in’: understanding the limited effectiveness of a smoke-free homes intervention, Journal of Public Health, Volume 43, Issue 3, September 2021, Pages 647–654, https://doi.org/10.1093/pubmed/fdaa042
Close - Share Icon Share
Abstract
Children’s second-hand smoke (SHS) exposure in the home is highest in socio-economically disadvantaged areas. Personalized household air-quality measurements can promote changes in smoking that reduce SHS exposure. The ‘First Steps 2 Smoke-free’ (FS2SF) intervention is the first to trial this approach delivered as part of health professionals’ routine work. This paper reports the findings of qualitative interviews with participants that explored their experiences of the intervention and why outcomes varied.
120 women were recruited from the NHS First Steps Programme, which supports disadvantaged mothers. They received either personalized feedback on their home air quality and advice on reducing SHS or standard SHS advice. Qualitative interviews with 15 mothers were analyzed thematically using the Capability, Opportunity, Motivation, Behaviour (COM-B) model.
The intervention increased women’s capability to change home-smoking behaviour, through increasing awareness and salience of SHS risks to their children, and motivation to act. However, taking effective action was constrained by their limited social and environmental opportunities, including others’ smoking in the home.
The FS2SF intervention was ineffective as it was unable to fully address the precarious, complex life circumstances that make creating a smoke-free home particularly difficult for women experiencing intersecting dimensions of disadvantage.
Introduction
Exposure to second-hand smoke (SHS) in the home causes adverse health outcomes in children and adults.1,2,3 The proportion of children exposed to SHS in the home has declined in the UK, but there is continuing inequality in exposure levels.4,5 In Scotland, under 1% of children in the most affluent areas report regular SHS home exposure, compared to 15% of childrenje in the most deprived areas.5 Disadvantaged parents can face challenges in creating and maintaining a smoke-free home, particularly when sole caring for young children in accommodation with limited access to suitable space to smoke outside.6,7,8,9
A range of interventions have been developed to promote smoke-free homes, for example using counselling approaches, feedback of a biological measure of children’s SHS exposure, school-based strategies, nicotine-replacement therapy and educational materials. However, reviews of interventions to reduce SHS in households with children have concluded that there is insufficient evidence to recommend any specific approach.10,11,12
Two British studies using personalized measurements of air quality in disadvantaged households have shown promise. The REFRESH 13 feasibility study involved smoking mothers in Scotland. It compared changes in home air quality, measured by airborne concentrations of fine particulate matter < 2.5 μm in size (PM2.5) and smoking in the homes of mothers who received personalized home air-quality data as part of a motivational interview with those who received only the motivational interview. REFRESH showed reductions in PM2.5 levels, with women motivated to protect their children because of their new knowledge about their home SHS levels.13,14 The second intervention15,16 used a similar approach, but included nicotine replacement therapy (NRT) for temporary abstinence and involved women with children under 5 years from socio-economically disadvantaged communities in England. This RCT found significant reductions in the intervention compared to the control group in home SHS levels at 12 weeks follow-up.16
In both studies, women reported that personalized feedback was the key motivating factor for changing smoking in the home. However, these interventions used labour-intensive recruitment16 and delivery methods,13 involving staff with dedicated time for delivery. The feasibility of health professionals delivering similar interventions as part of routine practice remains uncertain, particularly given declining resources for tobacco-control work.17
The NHS Lanarkshire First Steps Programme (FSP) provides home-based, one-to-one support for vulnerable women in socio-economically disadvantaged areas of South Lanarkshire. It works with mothers of pre-school children and pregnant women to develop parenting skills and encourage play and healthy lifestyles. At the time of the study, over 30% of clients smoked with 48% of homes having one or more smoking-adult resident. The ‘First Steps to Smoke Free’ (FS2SF) study aimed to test whether personalized air-quality feedback could be delivered by First Steps (FS) workers as part of their routine work and whether this reduced home SHS levels. An asset-based approach guided study development, considering women’s own resources, networks and skills alongside their needs.18,19 The FS2SF quantitative results are reported elsewhere.20 In summary, there was no statistical difference between the standard and enhanced intervention groups’ 1- and 6-month PM2.5 measurements. To understand why FS2SF had no effect, this paper reports the findings of qualitative interviews with women who received the enhanced intervention, which explored their experiences of the intervention and why behaviour change outcomes varied.
Methods
Study sample
FSP clients who were over 16 and smoked or lived with smokers could participate. FS workers invited eligible women to participate in the study, provided information sheets and gained written informed consent. Project home visits were built into the existing weekly visits. Full engagement over the 6-month intervention period involved nine visits. 171 women were invited to take part, of which 120 agreed (response rate 70.2%).
Design
Seventeen FS workers received a half-day course on the health effects of SHS, using the air-quality monitor and discussing the measurements with participants to encourage them to make their homes smoke free. Participants were randomized to Group A or B. A Dylos DC1700 air-quality monitor was installed in the home by the participant’s FS workers to measure PM2.5 for 3–7 days at baseline, +1 month and +6 months. An FS administrator downloaded data from air-quality instruments and prepared personalized feedback graphs. Group A received standard NHS Lanarkshire advice on the harmful effects of SHS after the baseline visit. Group B received standard advice plus personalized air-quality feedback at the baseline, +1 month and + 6 month measurements. Fig. 1 shows a hypothetical example of the air-quality feedback graph and information on home air quality that Group B participants received. Questionnaires assessed smoking and household rules at baseline, 1- and 6-month follow-up.
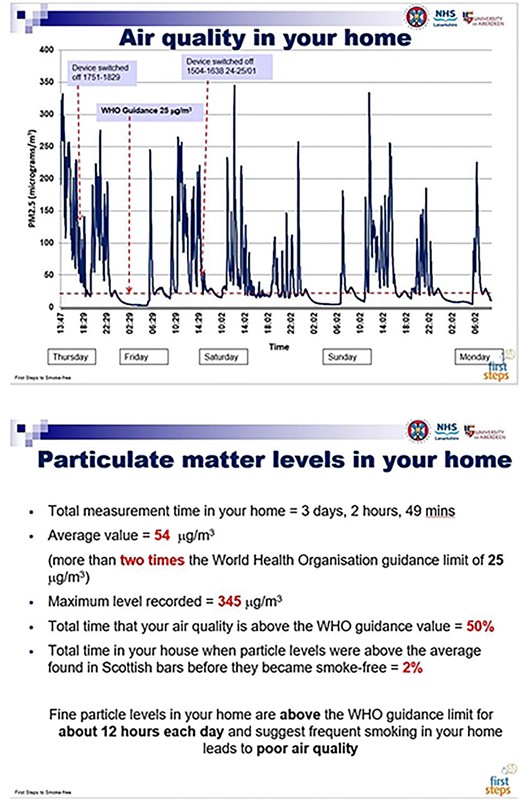
Example of the air-quality feedback graph and summary quantitative information on home air-quality measurements given to the participants.
Qualitative interviews
On completing the 6-month visit, 20 purposively selected Group B participants were invited by their FS worker to participate in an individual interview in their home, with one of the authors (RO). Participant selection aimed to optimize diversity in home smoking rules, change achieved, household circumstances, seasonality and FS workers involved. Two participants declined to take part in an interview and three participants agreed to take part but were uncontactable when the researcher attempted to schedule their interview. It was not possible to identify the characteristics of these five participants, due to confidentiality issues. Data collection and thematic analysis were conducted in parallel. Data saturation was reached, with no new themes emerging, by the 15th interview. The semi-structured interviews were audio-recorded with participant consent and lasted approximately 45 minutes. The interviews explored motivators and barriers to changing smoking behaviours, knowledge about SHS and health risks, perceived utility of air-quality measurements and intervention engagement. Participants received a £10 voucher at baseline and a £20 voucher at the 6-month visit. Interviewees received a further £10 voucher. Ethical approval was obtained from the NHS North of Scotland Research Ethics Committee.
Qualitative analysis
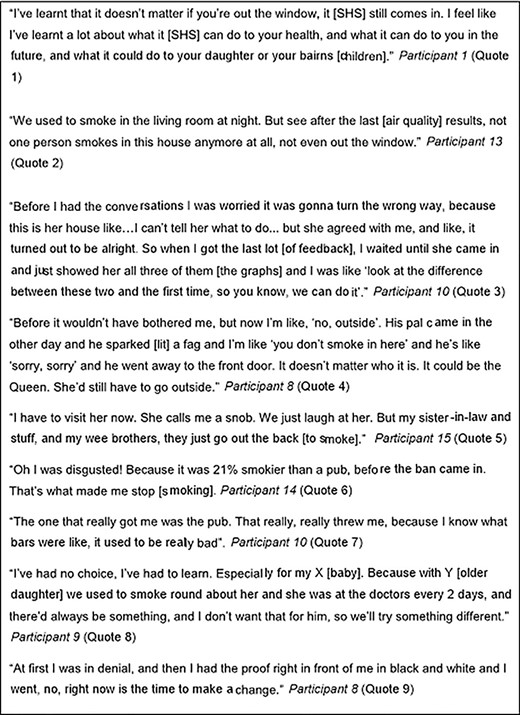
Interviews were verbatim transcribed. Initial coding was deductive, with codes derived from topic guide headings. Two authors (R.O., A.A.) independently read each transcript, noting topics and themes and potential connections between them. Deductive codes were then supplemented with more inductive codes derived from emergent themes in the data.21 Emerging themes provided a coherent fit with the COM-B model,22 which proposes that for individuals to engage in behaviour change, they must have the ‘capability’, ‘opportunity’ and ‘motivation’ (Fig. 2). The COM-B model was chosen as an appropriate analytical theoretical framework, because it considers both individual-level constructs (capability and motivation) and wider social contexts (opportunity). Relevant themes were organized by each of the three COM-B constructs. Discrepancies regarding theme or interpretation were discussed and resolved by two members of the study team (R.O., A.A.).

The COM-B System - a framework for understanding behaviour change.
Results
Capability - knowledge, awareness and communication
Interview findings indicated that participants found the intervention acceptable and understood the data they were shown, in some cases with assistance from their FS worker. Fourteen reported increased capability to change their smoking through increased knowledge and/or awareness about the health risks to children of SHS in the home, and how SHS remains suspended in the air (Fig. 3 quote 1). Some felt that having personalized results helped ‘prove’ facts about SHS that they had previously not believed. Participants also talked about their awareness of the ineffectiveness of previous strategies to reduce their children’s SHS exposure (i.e. opening a window and/or smoking in one room). During the intervention, they had adopted what they perceived to be the more effective strategies, from standing out on the veranda to smoke with the door shut to quitting smoking (Fig. 3 quote 2).
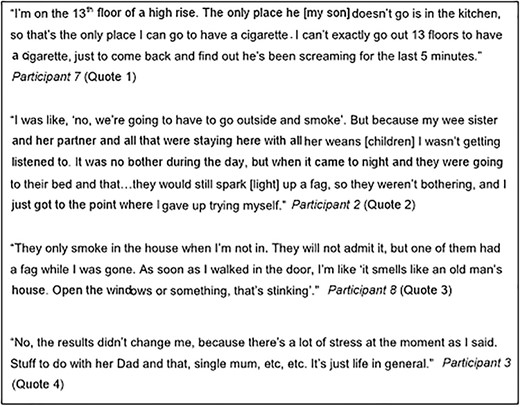
Most participants said they had talked with family and friends about the intervention, passing on their knowledge about SHS levels in their home. Several spoke with family members and/or regular visitors to gain their assistance in creating a smoke-free home. One woman, a non-smoker living with her baby and her mother (a smoker), had raised the issue with confidence using her personalized feedback (Fig. 3 quote 3). Subsequently, her mother decided to smoke outside the back door, with the door shut. Another participant spoke about changing her attitude toward visitors smoking in the home (Fig. 3 quote 4). However, a few participants described unsuccessful attempts to get others on board with new household smoking rules. Participant 15 described how her mother had been unhappy about having to smoke outside when she visited (Fig. 3 quote 5). These experiences highlighted the importance of psychological strength and stamina as a facet of capability related to persuading others in the household to support creating a smoke-free home.
Motivation - automatic (emotion-based) and reflective (belief/intention-based)
Thirteen participants reported increased motivation to change their smoking, with most expressing shock that their personalized feedback displayed higher PM2.5 readings than expected. Feelings of shock that were often discussed in relation to specific feedback on the percentage of time measurements were above the concentrations of SHS in Scottish bars prior to smoke-free legislation (Fig. 3 quote 6). This was surprising as smoke-free bars were implemented in 2006, but participants often had vivid images of their ‘smokiness’, which was more salient than the other quantitative feedbacks, such as average readings and time above WHO levels (Fig. 3 quote 7). This caused some to reflect on and change their smoking in the home. In most cases, their prime motivation was to better protect their children from SHS (Fig. 3 quote 8).
Participants also reflected that personalized data made the dangers of SHS more real to them than if they had simply heard or read about it. For some, having personalized data was the ‘proof’ they needed to reflect on and change their smoking behaviour (Fig. 3 quote 9). This motivated others to reflect on their smoking more generally, including three women who said that they had made a quit attempt and others who had reduced their smoking.
Opportunity
Whilst women often displayed increased capability and/or motivation to create a smoke-free home, their opportunities to do so were limited. Only seven reported having the opportunity to change their own or household members’ smoking behaviour. Five participants reported creating a smoke-free home, though only three had PM2.5 measurements that confirmed this, as two participants reported creating a smoke-free home after their last PM2.5 measurement was taken at the 6-month follow-up visit by their FS worker. Physical environmental factors and/or social relationships and contexts were described as constraining whether, and to what extent, changes were made and sustained. Sometimes this arose from being a single parent, unable to leave young, mobile children to go outside to smoke (Fig. 4 quote 1). This was illustrated by Participant 8 who moved between the second and third measurements, from a third floor flat with no easy access to outdoor space, to a flat with a veranda where she could now smoke as ‘even when it’s raining you have got a shelter!’.
Several women reported challenges involving household members continuing to smoke indoors while they were out of the house or asleep, which undermined their own behavioural change (Fig. 4 quotes 2 & 3). Participants dealt with often unstable living circumstances, resulting from relationship breakdowns, drug addiction, homelessness, partners in and out of prison, children in social care, re-housing and estranged families. Fluid household membership was common, with households’ smoking status often varying during the study. This posed extra challenges and reduced opportunities to create smoke-free environments, making behaviour change difficult to even contemplate (Fig. 4 quote 4).
Discussion
Main findings of this study
The FS2SF intervention appeared to increase women’s capability to change their smoking behaviour in the home. For some, the shock associated with learning their PM2.5 readings were higher than anticipated, and the personalized nature of the feedback increased their motivation to act. In most cases, the underlying motivation was to protect their children’s health. Our findings also indicate that when social and physical opportunities are restricted, often from limited control over their home environment, changing smoking behaviour in the home becomes less feasible using this intervention approach. This fits with the quantitative findings, which showed no change in household SHS concentrations after the intervention.20 This highlights the key limitation of the intervention–it’s inability to fully address the constraints on ‘choice’ associated with challenging and changing life circumstances, women’s often limited power to influence the behaviour of significant others, and the increasing mobility of children in their early years, which are important obstacles to taking smoking outside. Encouraging women who experience intersecting dimensions of disadvantage to be responsible for making ‘choices’ about their lives, and those of their families/children, and attempting to empower them to do so, has limited impact if the socio-economic conditions they live in are insufficient to facilitate change.
What is already known on this topic
There has been increasing awareness of the need for health-promotion approaches that recognize the gendered nature of health issues and develop gender accommodating and transformative approaches that empower women rather than exploit gender roles and norms.23,24,25 While adopting an asset-based approach, the FS2SF intervention placed the onus on women to convince partners/other family members to assist in creating a smoke-free home. This approach reflects smoke-free homes literature, which is dominated by interventions focusing on mothers.6 However, research on the barriers and facilitators to changing smoking behaviour in these settings has revealed gender power imbalances and women’s limited agency in changing the smoking behaviour of other adults in their household.6
What this study adds
Smoke-free homes interventions need to acknowledge and accommodate the precarious and complex nature of vulnerable, disadvantaged women’s lives, which makes creating smoke-free homes difficult. In the FS2SF study, the shock that most participants experienced when their personalized feedback displayed higher PM2.5 readings than expected caused some to reflect on and change their smoking behaviour, taking their smoking outside so as to better protect their children from SHS exposure in the home. However, some participants were unable to fully protect their children from SHS exposure in the home, as a result of housing and/or childcare constraints, and household relations. Future research and policy initiatives must ensure that disadvantaged women’s sense of hope, self-efficacy and well-being are not unduly compromised as a result of interventions designed to encourage efforts to create a smoke-free home.26 Using NRT for temporary abstinence or reducing smoking in the home could address some of these complexities, eliminating parents’ need to go outside whilst caring for young children.15,16 More fundamentally though, the FS2SF findings support the Kuala Lumpur Smoke-Free Homes Charter’s27 call for smoke-free home interventions to be delivered at a household level rather than only targeting mothers. Developing smoke-free home interventions that work with men and other family members, framing household smoking as a collective responsibility rather than tasking women as mothers and wives to persuade others to take their smoking outside, would address gender-specific issues. However, the feasibility of health professional delivery in ‘real world’ settings remains unclear.20
Limitations of this study
This qualitative study used a purposive sample and therefore the findings may not be generalizable to all study participants. Women who perceived that they had made positive changes may have been more likely to be interviewed and give more positive accounts than other FS2SF participants. Participants’ accounts may have been influenced by social desirability, especially given the shock that some mothers described in response to unexpectedly high SHS levels, and given that FS workers were generally present when the interviews took place.
Acknowledgements
We would like to thank all the mothers who participated, the Lanarkshire First Steps Programme workers and Ms C Briffa-Watt.
Conflict of interest
None.
Funding
This work was supported by the Scottish Government Chief Scientist Office (CZH_4_983).
R. O’Donnell, Dr.
A. Amos, Professor
S.W. Turner, Professor
L. Adams, Ms.
T. Henderson, Ms.
S. Lyttle, Ms.
S. Mitchell, Ms.
S. Semple, Dr.



