-
PDF
- Split View
-
Views
-
Cite
Cite
Randy M Stalter, Tracy Q Dong, Craig W Hendrix, Thesla Palanee-Phillips, Ariane van der Straten, Sharon L Hillier, Flavia M Kiweewa, Nyaradzo M Mgodi, Mark A Marzinke, Linda-Gail Bekker, Lydia Soto-Torres, Jared M Baeten, Elizabeth R Brown, for the MTN-020/ASPIRE Study Team , Assessing Per-Sex-Act HIV-1 Risk Reduction Among Women Using the Dapivirine Vaginal Ring, The Journal of Infectious Diseases, Volume 229, Issue 4, 15 April 2024, Pages 1158–1165, https://doi.org/10.1093/infdis/jiad550
Close - Share Icon Share
Abstract
Confounding introduced by individuals’ sexual risk behavior is potentially a significant source of bias in HIV-1 prevention intervention studies. To more completely account for sexual behaviors when assessing the efficacy of the monthly dapivirine ring, a new longer-acting HIV-1 prevention option for women, we estimated per-sex-act risk reduction associated with product use.
We conducted a secondary analysis of data from MTN-020/ASPIRE, a phase 3, randomized, placebo-controlled efficacy trial of the dapivirine ring that recruited HIV-uninfected, African women aged 18–45 years. With cumulative sex acts as the time scale, we used multivariable Cox regression with inverse probability of censoring weights to estimate HIV-1 risk reduction associated with a rate of dapivirine release indicative of consistent product use.
Women in the dapivirine ring group (n = 1187) had an estimated incidence rate of 2.3 (95% confidence interval [CI], 1.8–3.1) HIV-1 acquisition events per 10 000 sex acts versus 3.6 (95% CI, 2.9–4.4) per 10 000 acts in the placebo group (n = 1187). Dapivirine release indicative of consistent ring use was associated with a 63% (95% CI, 33%–80%) per-sex-act HIV-1 risk reduction.
These results support the efficacy of the dapivirine vaginal ring for HIV-1 prevention and help to inform decision-making for women, providers, and policymakers regarding product use.
NCT01617096.
In sub-Saharan Africa, women and girls account for more than half of new human immunodeficiency virus-1 (HIV-1) infections, underscoring the need for acceptable, novel, safe, and effective biomedical prevention interventions in this region [1]. Oral preexposure prophylaxis (PrEP) with tenofovir disoproxil fumarate and emtricitabine (TDF/FTC) is an important antiretroviral-based prevention strategy and is being scaled up rapidly in areas of sub-Saharan Africa with high HIV-1 burden [2]. However, challenges with daily PrEP adherence have been observed in past randomized trials and implementation studies [3–5], indicating that additional options are needed to fit women’s diverse needs and preferences. One such option is the vaginal ring containing the nonnucleoside reverse transcriptase inhibitor dapivirine, a product with a demonstrated favorable safety profile and HIV-1 risk reduction efficacy that women can wear continuously and discreetly for up to 1 month [6, 7]. In 2020, the ring received a positive opinion from the European Medicines Agency and prequalification and a recommendation from the World Health Organization [8–11]. The ring has since received regulatory approval in multiple countries in eastern and southern Africa [12–14].
As the dapivirine ring becomes an available PrEP option for women, it is important that its efficacy (ie, how well the product works when used under ideal conditions) be thoroughly assessed so that women can make well-informed decisions. The dapivirine ring was evaluated in 2 phase 3 efficacy trials in sub-Saharan Africa, MTN-020/ASPIRE and IPM 027/The Ring Study, and was found to be effective, reducing HIV-1 acquisition risk by 27% and 31% in intention-to-treat analyses, respectively [6, 7]. As observed in studies of oral PrEP agents [15, 16], efficacy was highly associated with greater adherence, and thus the intention-to-treat findings likely underestimate the product’s efficacy when there are varying levels of adherence in the intention-to-treat population. Further evaluation with objective measures of adherence, however, has helped to further elucidate product efficacy. Within the Partners PrEP Study, a case-cohort analysis demonstrated a 91% relative risk reduction (RRR) associated with plasma tenofovir concentrations consistent with daily use among TDF/FTC users [17], in contrast to 75% effectiveness of TDF/FTC estimated in the intention-to-treat analysis [15]. Similarly, a substudy of the iPrEx trial found that intracellular tenofovir metabolite concentrations indicative of 4 or more oral doses per week were predictive of 90% HIV-1 risk reduction relative to placebo versus 44% risk reduction in intention-to-treat analysis [18, 19]. For the dapivirine ring, disproportionately low adherence was seen among certain groups, particularly younger women. A secondary analysis of data from MTN-020/ASPIRE identified reductions in HIV-1 risk of 48% or more among women who demonstrated continuous ring use based on measured rates of dapivirine released from the ring [20].
However, a key factor to consider when further evaluating the efficacy of HIV prevention products in secondary analyses of clinical trial data where exposure groups are no longer randomized is the potential for confounding by sexual behavior. HIV-1 acquisition is dependent on exposure to the virus through unprotected sex, specifically with a partner with HIV-1. However, analytic approaches to evaluating HIV-1 prevention methods that use a standard time scale assume that individuals who are not having sex accumulate risk at the same rate as individuals who are having frequent sex, which can lead to biased efficacy estimates if sexual behaviors systematically differ between product use groups. By assessing risk on a sex act scale, periods of time with no sexual activity, and therefore without any chance of exposure, would not inform relative risk estimates. This work builds on the previous secondary analysis within MTN-020/ASPIRE by more thoroughly accounting for sexual behavior and estimating per-sex-act risk reduction associated with rates of dapivirine release from returned rings indicative of continuous use. We hypothesized that HIV risk reduction estimates will be higher after more thorough accounting of women’s sexual behaviors than previously estimated with dapivirine ring use.
METHODS
Study Population and Procedures
We conducted a secondary, longitudinal analysis of data collected from MTN-020/ASPIRE (NCT01617096), a phase 3 randomized placebo-controlled trial to assess the efficacy of the dapivirine vaginal ring for prevention of HIV-1 acquisition. Study procedures have been previously described in detail [6]. Briefly, healthy, HIV-uninfected cisgender women between ages 18 and 45 years, sexually active, and using an effective contraceptive method were recruited from 15 sites in Malawi, South Africa, Uganda, and Zimbabwe. Women were randomized 1:1 to use a silicone vaginal ring formulated with 25 mg of dapivirine or an inactive placebo ring and instructed to use the product continuously for 28 days. At monthly visits, women received a resupply of ring as well as serologic HIV-1 testing and product adherence counseling. Safety of ring use was evaluated at each follow-up visit and study product was held for one or more of the following criteria: pregnancy or breastfeeding, positive HIV-1 rapid test, experience of adverse event or allergic reaction related to the study product, or report of HIV-1 postexposure prophylaxis. Ethics review committees at each site approved the study protocol and all participants provided written informed consent prior to initiation of study procedures.
Survey and Laboratory Measures
Information on women’s sociodemographic characteristics, family planning use, menses/bleeding, and partner HIV-1 status and knowledge of ring use were collected by interviewer-administered surveys.
HIV-1 testing followed a standardized algorithm. At monthly study visits, women received 2 separate serological HIV-1 tests. If either test yielded a positive result, confirmatory western blot and HIV-1 RNA testing were performed on sera collected at the most recent quarterly visit. Archived sera from previous quarterly visits were also analyzed for HIV-1 RNA if needed to identify the earliest evidence of HIV-1 infection.
Testing for STIs and bacterial vaginosis (BV) occurred at the screening visit and then semiannually and when clinically indicated. Urine samples were tested for Neisseria gonorrhoeae and Chlamydia trachomatis using a nucleic acid amplification test. Rapid tests for Trichomonas vaginalis were conducted on vaginal swabs. Vaginal fluid samples were assessed for BV by Gram stain using the Nugent score.
Adherence Measures
Ring adherence was evaluated using multiple objective measures. First, stored plasma specimens from quarterly study visits were analyzed for dapivirine concentrations via a previously described ultraperformance liquid chromatography-tandem mass spectrometry assay [21]. Second, approximately 1 year after study enrollment began, used rings were collected at monthly visits and analyzed for quantities of residual dapivirine to assess cumulative use. Residual dapivirine in rings was collected using acetone extraction and then quantified using high-pressure liquid chromatography. The amount of drug released during intravaginal use was estimated by subtracting the amount of residual dapivirine measured in the ring from the batch-specific dapivirine loading mass. Given that women may not have returned to the clinic exactly 4 weeks after their previous visit, we standardized the amount of dapivirine released to 28 days of use. In previous phase 1 studies, approximately 4–5 mg of drug was released from the ring among women who reported continuous product use over a 28-day period [22, 23]. Because this analysis uses a continuous dapivirine release rate exposure variable, we used the point estimate at the midpoint of these values (4.5 mg/month) to assess risk reduction associated with consistent ring use. Use of the 4.5 mg/month midpoint allows for adequate comparison to previous evaluations of ring efficacy that use categorical exposure variables. These studies define consistent ring use as >4.0 mg/month, which includes all dapivirine release rates between 4 and 5 mg/month. Given that measurement of residual dapivirine in returned rings began a year into the study, we imputed monthly dapivirine release rates using a joint hidden Markov model (Supplementary Methods).
Estimating Per-Sex-Act Risk Reduction
Modeling the Sex Act Time Scale
At quarterly visits, women were asked to provide information about their sexual behaviors, including the number of sexual partners they had in the past 3 months, whether they had a consistent primary partner over the past 3 months, the number of vaginal sex acts with their primary partner in the past week, and number of times a condom was used. Women were also asked about numbers of anal sex acts; however, only vaginal sex acts were considered in this analysis given that anal sex may have occurred at the same encounter and receptive anal intercourse was not found to be an independent risk factor for HIV-1 acquisition in prior analyses of ASPIRE participants [24]. To carry out our analysis on the per-sex-act scale, we required complete monthly sexual behavior data for participants across follow-up. To predict numbers of monthly sex acts, we modeled participant-reported sex acts in the past week using a mixed effects Poisson model. The model included participant-specific intercepts and slopes for the study visit month variable to allow for individual variation in sex acts at baseline and change in sex acts over time. We included as fixed effects baseline and time-varying covariates thought to be correlated with sexual behaviors based on our own hypotheses and the published literature, including study site, age, marital status, number of live births, BV status, N. gonorrhoeae, C. trachomatis, and T. vaginalis infection, alcohol use, smoking status, having a primary or new sexual partner, number of sexual partners, number of sex acts at baseline, family planning use, and having any vaginal cleaning practices. A single fitted model was used to predict numbers of sex acts since the last monthly visit.
Regression Models
Models of per-sex-act risk reduction included women who were confirmed to be without HIV-1 at enrollment and had imputed sex acts and dapivirine release data across follow-up. Additionally, we excluded women from 2 study sites with lower product adherence and study retention that were discontinued early, as was done in a post hoc analysis for the ASPIRE trial. To model per-sex-act HIV-1 risk reduction associated with ring release rates of 4.5 mg/month (ie, consistent ring use), we fit Cox regression models using the cumulative number of predicted sex acts between enrollment and first HIV-1 detection as the outcome. Given that tests for HIV-1 RNA were only conducted quarterly, the month when HIV-1 acquisition occurred was imputed using the same joint hidden Markov model used to impute monthly dapivirine release rates (Supplementary Methods). Primary exposure variables for study group (dapivirine or placebo ring) and continuous ring release rate were included in the Cox models; the exponentiated linear combination of the coefficients of these 2 terms was used to obtain a parameter estimate analogous to a hazard ratio (HR), comparing the probability of HIV-1 infection at a particular number of cumulative sex acts between women in the dapivirine ring group with 4.5 mg/month drug release and women in the placebo ring group (for whom dapivirine release rate was 0 mg/month), assuming no HIV-1 infection up to that point. Percent RRR was calculated using the following formula: %RRR = (1 − HR) × 100. Women were censored at first pregnancy, first product hold >3 days, and loss to follow-up given likely changes in HIV-1 risk after these events. All models were stratified by study site. Multivariable models were adjusted for time-varying participant-reported condomless sex in the past 7 days and the following baseline variables: age, education, marital status, BV status, N. gonorrhoeae, C. trachomati,s and T. vaginalis diagnosis, any new sexual partners, multiple sexual partners, number of sex acts in last 3 months, any reported condomless sex in last 7 days, alcohol use, partner HIV-1 status and knowledge of ring use, family planning method, and age-specific local male HIV-1 prevalence (assuming that women had partners who were in their age group). Model parameter estimates were calculated separately for each of the 20 imputed datasets and averaged; standard errors were pooled using Rubin’s rules to obtain 95% confidence intervals (CIs) and 2-sided P values. Given that women in our analysis were censored for reasons that may be related to the study outcome of HIV-1 acquisition, we further adjusted our models using inverse probability of censoring weights (IPCWs) to account for potential selection bias due to informative censoring (Supplementary Methods). Subgroup analyses were carried out based on baseline age (<25 and ≥25 years), N. gonorrhoeae/C. trachomatis/T. vaginalis diagnoses, BV status, and whether women reported bleeding in the prior month given that women may have less HIV-1 exposure while experiencing bleeding. All statistical analyses were carried out in R version 3.6.1 (R Core Team).
RESULTS
In ASPIRE, 2629 women were randomized to use of either the dapivirine (n = 1313) or placebo ring (n = 1316). Of those women, 3 were retrospectively discovered to have had acute HIV-1 infection at baseline and were excluded. An additional 12 women had no follow-up after the enrollment visit. For this analysis, 9 women who had a product hold before their first follow-up visit, 17 with missing data for variables used in prediction and Markov chain Monte Carlo (MCMC) models, and an additional 214 women from 2 sites with lower product adherence and study retention were also excluded. Therefore, we included a total of 2374 women (1187 each in the dapivirine and placebo groups) in our analysis.
Women in the placebo and dapivirine ring groups (regardless of estimated release rates) had comparable sociodemographic characteristics (Table 1). Women who were estimated to have demonstrated consistent ring use at least once during the trial (≥4.5 mg/month) reported a median of 15.0 sex acts in the last 3 months (interquartile range [IQR], 6.0–36.0) and 33.4% reported recent condomless sex. Depot medroxyprogesterone acetate was the most used contraceptive method (used by 40.1% of women) at enrollment among all participants, and most women experienced regular bleeding at screening (53.2%).
| Characteristic . | Placebo Group (n = 1187) . | Dapivirine Group: No Months With Estimated Release Rate ≥4.5 mg/mo (n = 813) . | Dapivirine Group: at Least 1 Month With Estimated Release Rate ≥4.5 mg/mo (n = 374) . |
|---|---|---|---|
| Age, y, median (IQR) | 26.0 (23.0–31.0) | 27.0 (23.0–32.0) | 26.0 (22.0–31.0) |
| Country | |||
| Malawi | 136 (11.5) | 103 (12.7) | 29 (7.8) |
| South Africa | 592 (49.9) | 373 (45.9) | 220 (58.8) |
| Uganda | 126 (10.6) | 100 (12.3) | 27 (7.2) |
| Zimbabwe | 333 (28.1) | 237 (29.2) | 98 (26.2) |
| Highest level of education | |||
| None | 11 (0.9) | 10 (1.2) | 1 (0.3) |
| Primary, not complete | 111 (9.4) | 98 (12.1) | 26 (7.0) |
| Primary, complete | 65 (5.5) | 50 (6.2) | 18 (4.8) |
| Secondary, not complete | 466 (39.3) | 313 (38.5) | 136 (36.4) |
| Secondary, complete | 462 (38.9) | 311 (38.3) | 155 (41.4) |
| College or university | 72 (6.1) | 31 (3.8) | 38 (10.2) |
| Married | 537 (45.2) | 383 (47.1) | 135 (36.1) |
| No. of live births, median (IQR) | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 2.0 (1.0, 2.0) |
| Has primary partner | 1181 (99.5) | 811 (99.8) | 373 (99.7) |
| Partner knows about ring use | 779 (66.0) | 530 (65.4) | 238 (63.8) |
| Partner is circumcised | 508 (43.0) | 331 (40.8) | 161 (43.2) |
| Partner HIV-1 status | |||
| Positive | 12 (1.0) | 15 (1.8) | 7 (1.9) |
| Negative | 650 (55.0) | 429 (52.9) | 198 (53.1) |
| Don’t know | 519 (43.9) | 367 (45.3) | 168 (45.0) |
| Multiple sexual partners in the past 3 mo | 211 (17.8) | 135 (16.6) | 57 (15.2) |
| Any new partner in past 3 mo | 34 (2.9) | 28 (3.4) | 16 (4.3) |
| No. of sex acts in last 3 mo, median (IQR) | 21.0 (8.0–36.0) | 24.0 (10.0–40.0) | 15.0 (6.0–36.0) |
| No. of sex acts in last 7 d, median (IQR) | 2.0 (1.0–3.0) | 2.0 (1.0–4.0) | 1.0 (0.0–3.0) |
| Any condomless sex with partner in last 7 d | 524 (44.1) | 359 (44.2) | 125 (33.4) |
| Intrauterine device | 159 (13.4) | 128 (15.7) | 32 (8.6) |
| Oral pills | 118 (9.9) | 88 (10.8) | 32 (8.6) |
| Hormonal implant | 238 (20.1) | 194 (23.9) | 62 (16.6) |
| Depot medroxyprogesterone acetate | 500 (42.1) | 279 (34.3) | 173 (46.3) |
| Norethisterone enanthate | 149 (12.6) | 96 (11.8) | 75 (20.1) |
| Any menstrual bleeding in past 3 mo | 926 (78.0) | 656 (80.8) | 276 (74.0) |
| Any vaginal practices | 771 (65.0) | 533 (65.6) | 219 (58.6) |
| Usual bleeding pattern at screening | |||
| Amenorrheic | 254 (21.4) | 147 (18.1) | 99 (26.5) |
| Irregular | 301 (25.4) | 194 (23.9) | 95 (25.4) |
| Regular | 632 (53.2) | 472 (58.1) | 180 (48.1) |
| Neisseria gonorrhoeae | 48 (4.0) | 39 (4.8) | 14 (3.7) |
| Chlamydia trachomatis | 126 (10.6) | 96 (11.8) | 51 (13.6) |
| Trichomonas vaginalis | 82 (6.9) | 60 (7.4) | 21 (5.6) |
| Bacterial vaginosis | 472 (39.8) | 379 (6.6) | 1 (31.8) |
| Characteristic . | Placebo Group (n = 1187) . | Dapivirine Group: No Months With Estimated Release Rate ≥4.5 mg/mo (n = 813) . | Dapivirine Group: at Least 1 Month With Estimated Release Rate ≥4.5 mg/mo (n = 374) . |
|---|---|---|---|
| Age, y, median (IQR) | 26.0 (23.0–31.0) | 27.0 (23.0–32.0) | 26.0 (22.0–31.0) |
| Country | |||
| Malawi | 136 (11.5) | 103 (12.7) | 29 (7.8) |
| South Africa | 592 (49.9) | 373 (45.9) | 220 (58.8) |
| Uganda | 126 (10.6) | 100 (12.3) | 27 (7.2) |
| Zimbabwe | 333 (28.1) | 237 (29.2) | 98 (26.2) |
| Highest level of education | |||
| None | 11 (0.9) | 10 (1.2) | 1 (0.3) |
| Primary, not complete | 111 (9.4) | 98 (12.1) | 26 (7.0) |
| Primary, complete | 65 (5.5) | 50 (6.2) | 18 (4.8) |
| Secondary, not complete | 466 (39.3) | 313 (38.5) | 136 (36.4) |
| Secondary, complete | 462 (38.9) | 311 (38.3) | 155 (41.4) |
| College or university | 72 (6.1) | 31 (3.8) | 38 (10.2) |
| Married | 537 (45.2) | 383 (47.1) | 135 (36.1) |
| No. of live births, median (IQR) | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 2.0 (1.0, 2.0) |
| Has primary partner | 1181 (99.5) | 811 (99.8) | 373 (99.7) |
| Partner knows about ring use | 779 (66.0) | 530 (65.4) | 238 (63.8) |
| Partner is circumcised | 508 (43.0) | 331 (40.8) | 161 (43.2) |
| Partner HIV-1 status | |||
| Positive | 12 (1.0) | 15 (1.8) | 7 (1.9) |
| Negative | 650 (55.0) | 429 (52.9) | 198 (53.1) |
| Don’t know | 519 (43.9) | 367 (45.3) | 168 (45.0) |
| Multiple sexual partners in the past 3 mo | 211 (17.8) | 135 (16.6) | 57 (15.2) |
| Any new partner in past 3 mo | 34 (2.9) | 28 (3.4) | 16 (4.3) |
| No. of sex acts in last 3 mo, median (IQR) | 21.0 (8.0–36.0) | 24.0 (10.0–40.0) | 15.0 (6.0–36.0) |
| No. of sex acts in last 7 d, median (IQR) | 2.0 (1.0–3.0) | 2.0 (1.0–4.0) | 1.0 (0.0–3.0) |
| Any condomless sex with partner in last 7 d | 524 (44.1) | 359 (44.2) | 125 (33.4) |
| Intrauterine device | 159 (13.4) | 128 (15.7) | 32 (8.6) |
| Oral pills | 118 (9.9) | 88 (10.8) | 32 (8.6) |
| Hormonal implant | 238 (20.1) | 194 (23.9) | 62 (16.6) |
| Depot medroxyprogesterone acetate | 500 (42.1) | 279 (34.3) | 173 (46.3) |
| Norethisterone enanthate | 149 (12.6) | 96 (11.8) | 75 (20.1) |
| Any menstrual bleeding in past 3 mo | 926 (78.0) | 656 (80.8) | 276 (74.0) |
| Any vaginal practices | 771 (65.0) | 533 (65.6) | 219 (58.6) |
| Usual bleeding pattern at screening | |||
| Amenorrheic | 254 (21.4) | 147 (18.1) | 99 (26.5) |
| Irregular | 301 (25.4) | 194 (23.9) | 95 (25.4) |
| Regular | 632 (53.2) | 472 (58.1) | 180 (48.1) |
| Neisseria gonorrhoeae | 48 (4.0) | 39 (4.8) | 14 (3.7) |
| Chlamydia trachomatis | 126 (10.6) | 96 (11.8) | 51 (13.6) |
| Trichomonas vaginalis | 82 (6.9) | 60 (7.4) | 21 (5.6) |
| Bacterial vaginosis | 472 (39.8) | 379 (6.6) | 1 (31.8) |
Data are No. (%) except where indicated. Abbreviation: IQR, interquartile range.
| Characteristic . | Placebo Group (n = 1187) . | Dapivirine Group: No Months With Estimated Release Rate ≥4.5 mg/mo (n = 813) . | Dapivirine Group: at Least 1 Month With Estimated Release Rate ≥4.5 mg/mo (n = 374) . |
|---|---|---|---|
| Age, y, median (IQR) | 26.0 (23.0–31.0) | 27.0 (23.0–32.0) | 26.0 (22.0–31.0) |
| Country | |||
| Malawi | 136 (11.5) | 103 (12.7) | 29 (7.8) |
| South Africa | 592 (49.9) | 373 (45.9) | 220 (58.8) |
| Uganda | 126 (10.6) | 100 (12.3) | 27 (7.2) |
| Zimbabwe | 333 (28.1) | 237 (29.2) | 98 (26.2) |
| Highest level of education | |||
| None | 11 (0.9) | 10 (1.2) | 1 (0.3) |
| Primary, not complete | 111 (9.4) | 98 (12.1) | 26 (7.0) |
| Primary, complete | 65 (5.5) | 50 (6.2) | 18 (4.8) |
| Secondary, not complete | 466 (39.3) | 313 (38.5) | 136 (36.4) |
| Secondary, complete | 462 (38.9) | 311 (38.3) | 155 (41.4) |
| College or university | 72 (6.1) | 31 (3.8) | 38 (10.2) |
| Married | 537 (45.2) | 383 (47.1) | 135 (36.1) |
| No. of live births, median (IQR) | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 2.0 (1.0, 2.0) |
| Has primary partner | 1181 (99.5) | 811 (99.8) | 373 (99.7) |
| Partner knows about ring use | 779 (66.0) | 530 (65.4) | 238 (63.8) |
| Partner is circumcised | 508 (43.0) | 331 (40.8) | 161 (43.2) |
| Partner HIV-1 status | |||
| Positive | 12 (1.0) | 15 (1.8) | 7 (1.9) |
| Negative | 650 (55.0) | 429 (52.9) | 198 (53.1) |
| Don’t know | 519 (43.9) | 367 (45.3) | 168 (45.0) |
| Multiple sexual partners in the past 3 mo | 211 (17.8) | 135 (16.6) | 57 (15.2) |
| Any new partner in past 3 mo | 34 (2.9) | 28 (3.4) | 16 (4.3) |
| No. of sex acts in last 3 mo, median (IQR) | 21.0 (8.0–36.0) | 24.0 (10.0–40.0) | 15.0 (6.0–36.0) |
| No. of sex acts in last 7 d, median (IQR) | 2.0 (1.0–3.0) | 2.0 (1.0–4.0) | 1.0 (0.0–3.0) |
| Any condomless sex with partner in last 7 d | 524 (44.1) | 359 (44.2) | 125 (33.4) |
| Intrauterine device | 159 (13.4) | 128 (15.7) | 32 (8.6) |
| Oral pills | 118 (9.9) | 88 (10.8) | 32 (8.6) |
| Hormonal implant | 238 (20.1) | 194 (23.9) | 62 (16.6) |
| Depot medroxyprogesterone acetate | 500 (42.1) | 279 (34.3) | 173 (46.3) |
| Norethisterone enanthate | 149 (12.6) | 96 (11.8) | 75 (20.1) |
| Any menstrual bleeding in past 3 mo | 926 (78.0) | 656 (80.8) | 276 (74.0) |
| Any vaginal practices | 771 (65.0) | 533 (65.6) | 219 (58.6) |
| Usual bleeding pattern at screening | |||
| Amenorrheic | 254 (21.4) | 147 (18.1) | 99 (26.5) |
| Irregular | 301 (25.4) | 194 (23.9) | 95 (25.4) |
| Regular | 632 (53.2) | 472 (58.1) | 180 (48.1) |
| Neisseria gonorrhoeae | 48 (4.0) | 39 (4.8) | 14 (3.7) |
| Chlamydia trachomatis | 126 (10.6) | 96 (11.8) | 51 (13.6) |
| Trichomonas vaginalis | 82 (6.9) | 60 (7.4) | 21 (5.6) |
| Bacterial vaginosis | 472 (39.8) | 379 (6.6) | 1 (31.8) |
| Characteristic . | Placebo Group (n = 1187) . | Dapivirine Group: No Months With Estimated Release Rate ≥4.5 mg/mo (n = 813) . | Dapivirine Group: at Least 1 Month With Estimated Release Rate ≥4.5 mg/mo (n = 374) . |
|---|---|---|---|
| Age, y, median (IQR) | 26.0 (23.0–31.0) | 27.0 (23.0–32.0) | 26.0 (22.0–31.0) |
| Country | |||
| Malawi | 136 (11.5) | 103 (12.7) | 29 (7.8) |
| South Africa | 592 (49.9) | 373 (45.9) | 220 (58.8) |
| Uganda | 126 (10.6) | 100 (12.3) | 27 (7.2) |
| Zimbabwe | 333 (28.1) | 237 (29.2) | 98 (26.2) |
| Highest level of education | |||
| None | 11 (0.9) | 10 (1.2) | 1 (0.3) |
| Primary, not complete | 111 (9.4) | 98 (12.1) | 26 (7.0) |
| Primary, complete | 65 (5.5) | 50 (6.2) | 18 (4.8) |
| Secondary, not complete | 466 (39.3) | 313 (38.5) | 136 (36.4) |
| Secondary, complete | 462 (38.9) | 311 (38.3) | 155 (41.4) |
| College or university | 72 (6.1) | 31 (3.8) | 38 (10.2) |
| Married | 537 (45.2) | 383 (47.1) | 135 (36.1) |
| No. of live births, median (IQR) | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 2.0 (1.0, 2.0) |
| Has primary partner | 1181 (99.5) | 811 (99.8) | 373 (99.7) |
| Partner knows about ring use | 779 (66.0) | 530 (65.4) | 238 (63.8) |
| Partner is circumcised | 508 (43.0) | 331 (40.8) | 161 (43.2) |
| Partner HIV-1 status | |||
| Positive | 12 (1.0) | 15 (1.8) | 7 (1.9) |
| Negative | 650 (55.0) | 429 (52.9) | 198 (53.1) |
| Don’t know | 519 (43.9) | 367 (45.3) | 168 (45.0) |
| Multiple sexual partners in the past 3 mo | 211 (17.8) | 135 (16.6) | 57 (15.2) |
| Any new partner in past 3 mo | 34 (2.9) | 28 (3.4) | 16 (4.3) |
| No. of sex acts in last 3 mo, median (IQR) | 21.0 (8.0–36.0) | 24.0 (10.0–40.0) | 15.0 (6.0–36.0) |
| No. of sex acts in last 7 d, median (IQR) | 2.0 (1.0–3.0) | 2.0 (1.0–4.0) | 1.0 (0.0–3.0) |
| Any condomless sex with partner in last 7 d | 524 (44.1) | 359 (44.2) | 125 (33.4) |
| Intrauterine device | 159 (13.4) | 128 (15.7) | 32 (8.6) |
| Oral pills | 118 (9.9) | 88 (10.8) | 32 (8.6) |
| Hormonal implant | 238 (20.1) | 194 (23.9) | 62 (16.6) |
| Depot medroxyprogesterone acetate | 500 (42.1) | 279 (34.3) | 173 (46.3) |
| Norethisterone enanthate | 149 (12.6) | 96 (11.8) | 75 (20.1) |
| Any menstrual bleeding in past 3 mo | 926 (78.0) | 656 (80.8) | 276 (74.0) |
| Any vaginal practices | 771 (65.0) | 533 (65.6) | 219 (58.6) |
| Usual bleeding pattern at screening | |||
| Amenorrheic | 254 (21.4) | 147 (18.1) | 99 (26.5) |
| Irregular | 301 (25.4) | 194 (23.9) | 95 (25.4) |
| Regular | 632 (53.2) | 472 (58.1) | 180 (48.1) |
| Neisseria gonorrhoeae | 48 (4.0) | 39 (4.8) | 14 (3.7) |
| Chlamydia trachomatis | 126 (10.6) | 96 (11.8) | 51 (13.6) |
| Trichomonas vaginalis | 82 (6.9) | 60 (7.4) | 21 (5.6) |
| Bacterial vaginosis | 472 (39.8) | 379 (6.6) | 1 (31.8) |
Data are No. (%) except where indicated. Abbreviation: IQR, interquartile range.
In our mixed model to predict monthly sex acts, the standard deviation of the study month random effect term was 0.35. The median number of predicted sex acts per 28 days across follow-up was similar between women in the placebo and dapivirine ring groups (median, 8; IQR, 5–13 in both groups) and sexual behaviors gradually declined in frequency over time (Supplementary Figure 1A). Among women in the dapivirine ring group, the median estimated dapivirine release rate across the 20 posterior samples was 3.3 mg/28 days (IQR, 2.7–3.7) (distribution of dapivirine release rates by study visit shown in Supplementary Figure 1B). The median estimated dapivirine release rate was similar across categories of sex acts (Supplementary Figure 1C).
Overall, women in the placebo group experienced an estimated 83 HIV-1 acquisition events over 231 637 predicted sex acts, for an incidence rate of 3.6 events per 10 000 acts (95% CI, 2.9–4.4) (Table 2). Women in the dapivirine group experienced an estimated 54 HIV-1 acquisition events over 230 517 predicted sex acts, for an incidence rate of 2.3 events per 10 000 acts (95% CI, 1.8–3.1).
Per-Sex-Act HIV-1 Relative Risk Reduction Associated With Consistent Dapivirine Ring Use (Estimated Release of 4.5 mg/mo)
| . | Dapivirine Group: HIV-1 Events Per 10 000 Sex Acts (95% CI)a . | Placebo Group: HIV-1 Events Per 10 000 Sex Acts (95% CI) . | Unadjusted Model . | Adjusted Modelb . | Adjusted and Weighted Modelb,c . | ||||
|---|---|---|---|---|---|---|---|---|---|
| . | Per-Sex-Act RRR, % (95% CI) . | P . | Per-Sex-Act RRR, % (95% CI) . | P . | Per-Sex-Act RRR, % (95% CI) . | P . | Interaction P . | ||
| Overall | 2.3 (1.8–3.1) | 3.6 (2.9–4.4) | 57 (24–75) | .004 | 62 (32–79) | .001 | 63 (33–80) | .001 | … |
| Baseline age | |||||||||
| <25 y (n = 886) | 5.0 (3.5–6.9) | 5.3 (3.9–7.3) | 53 (0–77) | .049 | 61 (16–82) | .016 | 62 (17–82) | .014 | .844 |
| ≥25 y (n = 1488) | 1.1 (.7–1.8) | 2.8 (2.0–3.7) | 47 (−25 to 77) | .148 | 54 (−20 to 82) | .114 | 55 (−16 to 83) | .096 | |
| Baseline STIs/BV | |||||||||
| N. gonorrhoeae not detected (n = 2273) | 2.1 (1.6–2.8) | 3.3 (2.6–4.2) | 56 (19–76) | .009 | 61 (27–79) | .003 | 62 (29–80) | .003 | .683 |
| N. gonorrhoeae detected (n = 101) | 7.2 (2.9–14.9) | 11.0 (5.0–20.8) | 59 (−104 to 92) | .277 | 72 (−67 to 95) | .162 | 72 (−64 to 95) | .159 | |
| C. trachomatis not detected (n = 2101) | 1.9 (1.3–2.6) | 3.2 (2.5–4.1) | 49 (3–73) | .039 | 53 (9–76) | .026 | 54 (10–77) | .023 | .181 |
| C. trachomatis detected (n = 273) | 6.2 (3.5–10.2) | 7.3 (4.2–11.9) | 75 (2–92) | .020 | 81 (37–95) | .007 | 83 (42–95) | .005 | |
| T. vaginalis detected (n = 2211) | 2.1 (1.6–2.9) | 3.5 (2.7–4.3) | 62 (30–80) | .002 | 66 (35–83) | .001 | 68 (38–83) | .001 | .250 |
| T. vaginalis detected (n = 163) | 4.9 (2.1–9.7) | 5.2 (2.2–10.2) | −26 (−621 to 78) | .798 | 16 (−348 to 84) | .839 | 10 (−363 to 83) | .899 | |
| BV not detected (n = 1404) | 2.0 (1.4–2.9) | 2.7 (1.9–3.7) | 51 (−6 to 77) | .071 | 53 (−1 to 78) | .052 | 54 (1 to 78) | .048 | .441 |
| BV detected (n = 970) | 2.8 (1.8–4.1) | 5.0 (3.6–6.7) | 63 (10–84) | .028 | 71 (26–89) | .010 | 72 (28–89) | .008 | |
| Menses/bleeding in past mo | |||||||||
| No | 2.9 (2.0–3.9) | 4.0 (3.0–5.2) | 47 (0–72) | .049 | 55 (12–77) | .020 | 56 (14–78) | .017 | .282 |
| Yes | 1.6 (.9–2.7) | 2.9 (1.9–4.2) | 77 (26–93) | .014 | 78 (28–94) | .013 | 79 (30–94) | .011 | |
| . | Dapivirine Group: HIV-1 Events Per 10 000 Sex Acts (95% CI)a . | Placebo Group: HIV-1 Events Per 10 000 Sex Acts (95% CI) . | Unadjusted Model . | Adjusted Modelb . | Adjusted and Weighted Modelb,c . | ||||
|---|---|---|---|---|---|---|---|---|---|
| . | Per-Sex-Act RRR, % (95% CI) . | P . | Per-Sex-Act RRR, % (95% CI) . | P . | Per-Sex-Act RRR, % (95% CI) . | P . | Interaction P . | ||
| Overall | 2.3 (1.8–3.1) | 3.6 (2.9–4.4) | 57 (24–75) | .004 | 62 (32–79) | .001 | 63 (33–80) | .001 | … |
| Baseline age | |||||||||
| <25 y (n = 886) | 5.0 (3.5–6.9) | 5.3 (3.9–7.3) | 53 (0–77) | .049 | 61 (16–82) | .016 | 62 (17–82) | .014 | .844 |
| ≥25 y (n = 1488) | 1.1 (.7–1.8) | 2.8 (2.0–3.7) | 47 (−25 to 77) | .148 | 54 (−20 to 82) | .114 | 55 (−16 to 83) | .096 | |
| Baseline STIs/BV | |||||||||
| N. gonorrhoeae not detected (n = 2273) | 2.1 (1.6–2.8) | 3.3 (2.6–4.2) | 56 (19–76) | .009 | 61 (27–79) | .003 | 62 (29–80) | .003 | .683 |
| N. gonorrhoeae detected (n = 101) | 7.2 (2.9–14.9) | 11.0 (5.0–20.8) | 59 (−104 to 92) | .277 | 72 (−67 to 95) | .162 | 72 (−64 to 95) | .159 | |
| C. trachomatis not detected (n = 2101) | 1.9 (1.3–2.6) | 3.2 (2.5–4.1) | 49 (3–73) | .039 | 53 (9–76) | .026 | 54 (10–77) | .023 | .181 |
| C. trachomatis detected (n = 273) | 6.2 (3.5–10.2) | 7.3 (4.2–11.9) | 75 (2–92) | .020 | 81 (37–95) | .007 | 83 (42–95) | .005 | |
| T. vaginalis detected (n = 2211) | 2.1 (1.6–2.9) | 3.5 (2.7–4.3) | 62 (30–80) | .002 | 66 (35–83) | .001 | 68 (38–83) | .001 | .250 |
| T. vaginalis detected (n = 163) | 4.9 (2.1–9.7) | 5.2 (2.2–10.2) | −26 (−621 to 78) | .798 | 16 (−348 to 84) | .839 | 10 (−363 to 83) | .899 | |
| BV not detected (n = 1404) | 2.0 (1.4–2.9) | 2.7 (1.9–3.7) | 51 (−6 to 77) | .071 | 53 (−1 to 78) | .052 | 54 (1 to 78) | .048 | .441 |
| BV detected (n = 970) | 2.8 (1.8–4.1) | 5.0 (3.6–6.7) | 63 (10–84) | .028 | 71 (26–89) | .010 | 72 (28–89) | .008 | |
| Menses/bleeding in past mo | |||||||||
| No | 2.9 (2.0–3.9) | 4.0 (3.0–5.2) | 47 (0–72) | .049 | 55 (12–77) | .020 | 56 (14–78) | .017 | .282 |
| Yes | 1.6 (.9–2.7) | 2.9 (1.9–4.2) | 77 (26–93) | .014 | 78 (28–94) | .013 | 79 (30–94) | .011 | |
All models were stratified by study site. RRR calculated as ( − hazard ratio) × 100.
Abbreviations: BV, bacterial vaginosis; CI, confidence interval; HIV-1, human immunodeficiency virus-1; RRR, relative risk reduction; STI, sexually transmitted infection.
aCrude incidence rates of HIV-1 events per 10 000 sex acts include all participants in the dapivirine ring group. However, the per-sex-act RRR estimates in the table compare the probability of HIV-1 infection between women in the dapivirine ring group with 4.5 mg/month drug release and women in the placebo ring group (for whom dapivirine release rate was 0 mg/month). Hence, comparison of the crude incidence rates will not equate to the unadjusted RRR estimate.
bMultivariable Cox regression models were adjusted for report of any condomless sex and the following baseline variables: age, education, marital status, BV status, Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis diagnosis, any new sexual partners, multiple sexual partners, number of sex acts in last 3 months, any condomless sex in last 7 days, alcohol use, partner HIV-1 status and knowledge of ring use, family planning method, and local HIV-1 prevalence for men within the same age group.
cAdjusted using inverse probability of censoring weights to account for selection bias due to participant censoring at first pregnancy, first product hold >3 days, and loss-to-follow-up given likely changes in HIV-1 risk after these events.
Per-Sex-Act HIV-1 Relative Risk Reduction Associated With Consistent Dapivirine Ring Use (Estimated Release of 4.5 mg/mo)
| . | Dapivirine Group: HIV-1 Events Per 10 000 Sex Acts (95% CI)a . | Placebo Group: HIV-1 Events Per 10 000 Sex Acts (95% CI) . | Unadjusted Model . | Adjusted Modelb . | Adjusted and Weighted Modelb,c . | ||||
|---|---|---|---|---|---|---|---|---|---|
| . | Per-Sex-Act RRR, % (95% CI) . | P . | Per-Sex-Act RRR, % (95% CI) . | P . | Per-Sex-Act RRR, % (95% CI) . | P . | Interaction P . | ||
| Overall | 2.3 (1.8–3.1) | 3.6 (2.9–4.4) | 57 (24–75) | .004 | 62 (32–79) | .001 | 63 (33–80) | .001 | … |
| Baseline age | |||||||||
| <25 y (n = 886) | 5.0 (3.5–6.9) | 5.3 (3.9–7.3) | 53 (0–77) | .049 | 61 (16–82) | .016 | 62 (17–82) | .014 | .844 |
| ≥25 y (n = 1488) | 1.1 (.7–1.8) | 2.8 (2.0–3.7) | 47 (−25 to 77) | .148 | 54 (−20 to 82) | .114 | 55 (−16 to 83) | .096 | |
| Baseline STIs/BV | |||||||||
| N. gonorrhoeae not detected (n = 2273) | 2.1 (1.6–2.8) | 3.3 (2.6–4.2) | 56 (19–76) | .009 | 61 (27–79) | .003 | 62 (29–80) | .003 | .683 |
| N. gonorrhoeae detected (n = 101) | 7.2 (2.9–14.9) | 11.0 (5.0–20.8) | 59 (−104 to 92) | .277 | 72 (−67 to 95) | .162 | 72 (−64 to 95) | .159 | |
| C. trachomatis not detected (n = 2101) | 1.9 (1.3–2.6) | 3.2 (2.5–4.1) | 49 (3–73) | .039 | 53 (9–76) | .026 | 54 (10–77) | .023 | .181 |
| C. trachomatis detected (n = 273) | 6.2 (3.5–10.2) | 7.3 (4.2–11.9) | 75 (2–92) | .020 | 81 (37–95) | .007 | 83 (42–95) | .005 | |
| T. vaginalis detected (n = 2211) | 2.1 (1.6–2.9) | 3.5 (2.7–4.3) | 62 (30–80) | .002 | 66 (35–83) | .001 | 68 (38–83) | .001 | .250 |
| T. vaginalis detected (n = 163) | 4.9 (2.1–9.7) | 5.2 (2.2–10.2) | −26 (−621 to 78) | .798 | 16 (−348 to 84) | .839 | 10 (−363 to 83) | .899 | |
| BV not detected (n = 1404) | 2.0 (1.4–2.9) | 2.7 (1.9–3.7) | 51 (−6 to 77) | .071 | 53 (−1 to 78) | .052 | 54 (1 to 78) | .048 | .441 |
| BV detected (n = 970) | 2.8 (1.8–4.1) | 5.0 (3.6–6.7) | 63 (10–84) | .028 | 71 (26–89) | .010 | 72 (28–89) | .008 | |
| Menses/bleeding in past mo | |||||||||
| No | 2.9 (2.0–3.9) | 4.0 (3.0–5.2) | 47 (0–72) | .049 | 55 (12–77) | .020 | 56 (14–78) | .017 | .282 |
| Yes | 1.6 (.9–2.7) | 2.9 (1.9–4.2) | 77 (26–93) | .014 | 78 (28–94) | .013 | 79 (30–94) | .011 | |
| . | Dapivirine Group: HIV-1 Events Per 10 000 Sex Acts (95% CI)a . | Placebo Group: HIV-1 Events Per 10 000 Sex Acts (95% CI) . | Unadjusted Model . | Adjusted Modelb . | Adjusted and Weighted Modelb,c . | ||||
|---|---|---|---|---|---|---|---|---|---|
| . | Per-Sex-Act RRR, % (95% CI) . | P . | Per-Sex-Act RRR, % (95% CI) . | P . | Per-Sex-Act RRR, % (95% CI) . | P . | Interaction P . | ||
| Overall | 2.3 (1.8–3.1) | 3.6 (2.9–4.4) | 57 (24–75) | .004 | 62 (32–79) | .001 | 63 (33–80) | .001 | … |
| Baseline age | |||||||||
| <25 y (n = 886) | 5.0 (3.5–6.9) | 5.3 (3.9–7.3) | 53 (0–77) | .049 | 61 (16–82) | .016 | 62 (17–82) | .014 | .844 |
| ≥25 y (n = 1488) | 1.1 (.7–1.8) | 2.8 (2.0–3.7) | 47 (−25 to 77) | .148 | 54 (−20 to 82) | .114 | 55 (−16 to 83) | .096 | |
| Baseline STIs/BV | |||||||||
| N. gonorrhoeae not detected (n = 2273) | 2.1 (1.6–2.8) | 3.3 (2.6–4.2) | 56 (19–76) | .009 | 61 (27–79) | .003 | 62 (29–80) | .003 | .683 |
| N. gonorrhoeae detected (n = 101) | 7.2 (2.9–14.9) | 11.0 (5.0–20.8) | 59 (−104 to 92) | .277 | 72 (−67 to 95) | .162 | 72 (−64 to 95) | .159 | |
| C. trachomatis not detected (n = 2101) | 1.9 (1.3–2.6) | 3.2 (2.5–4.1) | 49 (3–73) | .039 | 53 (9–76) | .026 | 54 (10–77) | .023 | .181 |
| C. trachomatis detected (n = 273) | 6.2 (3.5–10.2) | 7.3 (4.2–11.9) | 75 (2–92) | .020 | 81 (37–95) | .007 | 83 (42–95) | .005 | |
| T. vaginalis detected (n = 2211) | 2.1 (1.6–2.9) | 3.5 (2.7–4.3) | 62 (30–80) | .002 | 66 (35–83) | .001 | 68 (38–83) | .001 | .250 |
| T. vaginalis detected (n = 163) | 4.9 (2.1–9.7) | 5.2 (2.2–10.2) | −26 (−621 to 78) | .798 | 16 (−348 to 84) | .839 | 10 (−363 to 83) | .899 | |
| BV not detected (n = 1404) | 2.0 (1.4–2.9) | 2.7 (1.9–3.7) | 51 (−6 to 77) | .071 | 53 (−1 to 78) | .052 | 54 (1 to 78) | .048 | .441 |
| BV detected (n = 970) | 2.8 (1.8–4.1) | 5.0 (3.6–6.7) | 63 (10–84) | .028 | 71 (26–89) | .010 | 72 (28–89) | .008 | |
| Menses/bleeding in past mo | |||||||||
| No | 2.9 (2.0–3.9) | 4.0 (3.0–5.2) | 47 (0–72) | .049 | 55 (12–77) | .020 | 56 (14–78) | .017 | .282 |
| Yes | 1.6 (.9–2.7) | 2.9 (1.9–4.2) | 77 (26–93) | .014 | 78 (28–94) | .013 | 79 (30–94) | .011 | |
All models were stratified by study site. RRR calculated as ( − hazard ratio) × 100.
Abbreviations: BV, bacterial vaginosis; CI, confidence interval; HIV-1, human immunodeficiency virus-1; RRR, relative risk reduction; STI, sexually transmitted infection.
aCrude incidence rates of HIV-1 events per 10 000 sex acts include all participants in the dapivirine ring group. However, the per-sex-act RRR estimates in the table compare the probability of HIV-1 infection between women in the dapivirine ring group with 4.5 mg/month drug release and women in the placebo ring group (for whom dapivirine release rate was 0 mg/month). Hence, comparison of the crude incidence rates will not equate to the unadjusted RRR estimate.
bMultivariable Cox regression models were adjusted for report of any condomless sex and the following baseline variables: age, education, marital status, BV status, Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis diagnosis, any new sexual partners, multiple sexual partners, number of sex acts in last 3 months, any condomless sex in last 7 days, alcohol use, partner HIV-1 status and knowledge of ring use, family planning method, and local HIV-1 prevalence for men within the same age group.
cAdjusted using inverse probability of censoring weights to account for selection bias due to participant censoring at first pregnancy, first product hold >3 days, and loss-to-follow-up given likely changes in HIV-1 risk after these events.
Women in the dapivirine ring group demonstrating consistent ring use (estimated dapivirine release of 4.5 mg/28 days) had a 57% reduction in HIV-1 risk (95% CI, 20%–74%) relative to placebo in unadjusted models. In multivariable models adjusting for time-varying report of any condomless sex and baseline variables for age, education, marital status, BV status, N. gonorrhoeae/C. trachomatis/T. vaginalis diagnoses, sexual behaviors, alcohol use, partner HIV-1 status and knowledge of ring use, family planning method, and local HIV-1 prevalence for men within the same age group, release rates associated with consistent ring use were associated with a 62% HIV-1 RRR (95% CI, 32%–79%) compared to placebo.
Mean stabilized IPCW values were close to 1 (South Africa sites IPCW mean, 0.997 [range: 0.319–3.514]; non-South Africa sites IPCW mean, 0.995 [range: 0.505–10.550]). However, standardized mean differences of covariates between censored and uncensored women were similar after weighting, indicating possible inadequate model specification (Supplementary Figure 3). In the adjusted model incorporating IPCWs, dapivirine release indicative of consistent ring use was associated with a 63% RRR (95% CI, 33%–80%). There was significant risk reduction with dapivirine release rates as low as 1.3 mg/month, but risk reduction estimates were higher with greater dapivirine release (Figure 1).
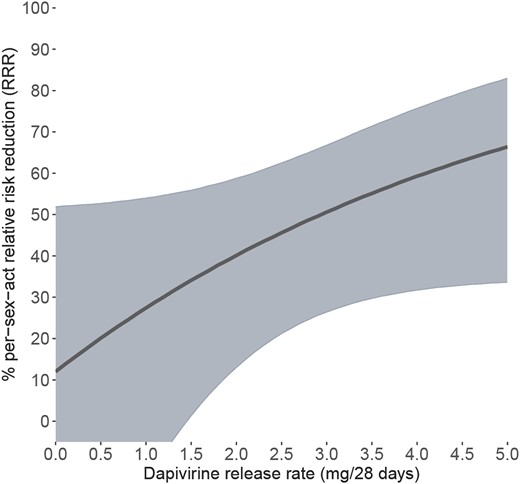
Per-sex-act HIV-1 risk reduction with incremental dapivirine release rates. Solid line indicates percent relative risk reduction estimate. Shaded area indicates 95% confidence interval.
In subgroup analyses, estimated per-sex-act HIV-1 incidence was highest among women with detected N. gonorrhoeae (11.0 events per 10 000 acts in placebo group and 7.2 events per 10 000 acts in dapivirine group) and C. trachomatis (7.3 events per 10 000 acts in placebo group vs 6.2 events per 10 000 acts in dapivirine group) at enrollment. However, RRR estimates did not differ between women with or without N. gonorrhoeae and C. trachomatis infection at enrollment according to interaction models (P = .683 and P = .181, respectively). Additionally, no significant difference in RRR was identified between age, BV status, and T. vaginalis detection subgroups. In our interaction model based on time-varying experience of bleeding in the past month, risk reduction estimates were higher for months when bleeding was reported versus when not reported (Supplementary Figure 2), but this difference was not statistically significant (P = .282).
DISCUSSION
In this secondary analysis of data from the ASPIRE trial, we conducted a rigorous evaluation of HIV-1 risk reduction associated with use of the dapivirine vaginal ring with a more complete accounting for women’s sexual behaviors. Unlike other analyses that evaluate HIV-1 risk reduction on a time scale, assessing risk reduction on the sex act scale may better control for the heterogeneity in women’s sexual behaviors and ensure that accumulation of HIV-1 risk is directly tied to potential exposure. We demonstrated a positive relationship between rate of drug release from the dapivirine vaginal ring and HIV-1 risk reduction. Further, dapivirine release rates indicative of consistent ring use were associated with an estimated 63% reduction in per-sex-act HIV-1 risk after adjusting for other potential confounders and accounting for informative censoring using IPCWs.
Dapivirine release rates were imputed in our analysis using MCMC methods to account for missingness and measurement error in observed ring release measures. In our previous analysis using all available measured ring release data, which excluded 46 women with HIV-1 end points that occurred prior to collection of used rings for dapivirine quantification, we demonstrated a 43% risk reduction associated with dapivirine release rates consistent with continuous use [20]. In this previous analysis, the same levels of dapivirine release were associated with a 71% HIV-1 risk reduction when starting follow-up at 12 months to create a common start time; however, as this was a secondary analysis that excluded an additional 54 HIV-1 end points and 1436 woman-years of follow-up, it is possible this estimate was biased due to missing data from early study visits. Here, our ability to use the full range of study follow-up data due to our imputation methods allows us to correct for selection bias due to previous exclusion of these end points.
We observed little change in HIV-1 risk reduction estimates when models were weighted using IPCWs. This was also observed in previous work utilizing IPCWs to evaluate the efficacy of oral PrEP, which censored participants at first missed visit and detection of poor adherence [19]. Estimating unbiased IPCWs is dependent correct model specification [25, 26] and inclusion of all variables associated with time to censoring and time to failure. Therefore, this small change could be due to poor weight model specification and might suggest our models exclude other unmeasured predictors of censoring. This is supported by our IPCW diagnostics that showed similar covariate balance between censored and uncensored before and after weighting.
Other potential limitations of our analysis should be considered. First, predicted numbers of monthly sex acts were based on women’s self-reported sex acts in the prior week. Such data are subject to recall bias (particularly among women who have frequent sex) and social desirability bias. Additionally, given that estimated values (ie, predicted sex acts and IPCWs) are treated as fixed quantities in the Cox regression models, the pooled standard errors used to estimate per-sex-act HIV risk reduction may not fully reflect the variability in these data. Second, per-sex-act risk depends largely on the HIV-1 status of their partner. However, <2% of women reported that their primary partner was living with HIV-1 at baseline while nearly half of women did not know their partner’s status. We also adjusted for age-specific local HIV-1 prevalence among men to further account for partner HIV-1 status and variation in women’s HIV-1 exposure, but this is an imperfect proxy for confirmation of women’s partner status. As a result, per-act incidence calculated in our analysis is likely an underestimate of the per-act incidence of women who are HIV-exposed.
Our analysis supports the use of the dapivirine ring as an efficacious HIV-1 prevention product for women. While the efficacy of the ring for preventing male-to-female HIV-1 transmission via vaginal sex is not as high as the efficacy of daily PrEP or consistent condom use, both of which reduce the risk of HIV transmission via multiple routes and are associated with >90% risk reduction [17, 27], the ring has important characteristics that may suit some women’s needs (eg, longer duration, less user-dependent, allows for discreet use, potentially fewer side effects, and high acceptability [28]). Therefore, communication of risk associated with the ring relative to other PrEP options should be part of a person-centered approach, acknowledging that women are in the best position to decide which option is best for their individual situation [29]. As additional HIV-1 prevention products emerge from the development pipeline, including multipurpose prevention technologies, we encourage similar analyses to evaluate risk reduction associated with product exposure as a complement to intention-to-treat analysis as an approach to best understand product efficacy.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online (http://jid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Study team leadership. Jared Baeten, University of Washington (Protocol Chair); Thesla Palanee-Phillips, Wits Reproductive Health and HIV Institute (Protocol Cochair); Elizabeth Brown, Fred Hutchinson Cancer Research Center (Protocol Statistician); Lydia Soto-Torres, US National Institute of Allergy and Infectious Diseases (Medical Officer); and Katie Schwartz, FHI 360 (Clinical Research Manager).
Study sites and site investigators of record. Malawi, Blantyre site (Johns Hopkins University, Queen Elizabeth Hospital), Bonus Makanani; Malawi, Lilongwe site (University of North Carolina, Chapel Hill), Francis Martinson; South Africa, Cape Town site (University of Cape Town), Linda-Gail Bekker; South Africa, Durban-Botha’s Hill, Chatsworth, Isipingo, Tongaat, Umkomaas, Verulam sites (South African Medical Research Council), Vaneshree Govender, Samantha Siva, Zakir Gaffoor, Logashvari Naidoo, Arendevi Pather, and Nitesha Jeenarain; South Africa, Durban, eThekwini site (Center for the AIDS Programme for Research in South Africa), Gonasagrie Nair; South Africa, Johannesburg site (Wits RHI), Thesla Palanee-Phillips; Uganda, Kampala site (John Hopkins University, Makerere University), Flavia Matovu Kiweewa; Zimbabwe, Chitungwiza, Seke South and Zengeza sites (University of Zimbabwe Clinical Trials Research Centre), Nyaradzo Mgodi; Zimbabwe, Harare, Spilhaus site (University of Zimbabwe Clinical Trials Research Centre), Felix Mhlanga.
Author contributions. R. M. S., J. M. B., and E. R. B. conceptualized the primary research question and overall study design. R. M. S. led the data analyses. T. Q. D. and E. R. B. contributed to the data analyses and provided statistical guidance. C. W. H., T. P. P., A. v. d. S., S. L. H., F. M. K., N. M. M., M. A. M., L. G. B., L. S. T., J. M. B., and E. R. B. led parts of or directly contributed to implementation and data collection for the parent study (MTN-020/ASPIRE). R. M. S. drafted the initial manuscript, and all authors contributed to results interpretation and manuscript revisions. All authors have read and approved the manuscript.
Acknowledgments. We thank all the women who participated in MTN-020/ASPIRE. Data management was provided by The Statistical Center for HIV/AIDS Research and Prevention (Fred Hutchinson Cancer Research Center, Seattle, WA) and site laboratory oversight was provided by the Microbicide Trials Network Laboratory Center (Pittsburgh, PA). The vaginal rings used in this study were developed and supplied by the International Partnership for Microbicides. The study was designed and implemented by the Microbicide Trials Network.
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH) (grant numbers UM1AI068633, UM1AI068615, and UM1AI106707); with cofunding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH and the National Institute of Mental Health, NIH. R. M. S. was supported by an NIH institutional training grant (grant number T32AI007140).
References
Author notes
Potential conflicts of interest. C. W. H. has received grant support from Merck and Gilead Sciences; is a co-inventer of two issued U.S. patents related to microbicides; and is founder of Prionde BioPharma, LLC, a microbicide company. T. P. P. has received grant support from Gilead Sciences, MSD, and the South African Medical Research Council; and participates on advisory boards for the Dual Protection Pill (DPP) Consortium and the Maximizing Options to Advance Informed Choice for HIV Prevention (MOSAIC) project. A. D. S. has received consulting fees from the Magee Women’s Research Institute. S. L. H. has received consulting fees from Merck. M. M. has received grant support from ViiV Healthcare, GSK, and Gilead Sciences; royalties from Elsevier; and consulting fees and honoraria from Bio-Rad. L. G. B. has received honoraria from ViiV Healthcare, Gilead Sciences and Merck Pty Ltd. J. M. B. is an employee of Gilead Sciences, outside the present work. E. R. B. has received payment for participation on Data Safety Monitoring Boards for Merck and the Adolescent Trials Network and is a paid statistical editor for JID. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.




