-
PDF
- Split View
-
Views
-
Cite
Cite
Megumi Sato, Michio Otsuki, Tomomi Mori, Juro Yanagida, Toshiyuki Yamamoto, Tomoko Nakagami, Remission of Insulin-Dependent Diabetes Mellitus in Multiple Endocrine Neoplasia Type 2A After Adrenalectomy, JCEM Case Reports, Volume 3, Issue 1, January 2025, luae240, https://doi.org/10.1210/jcemcr/luae240
Close - Share Icon Share
Abstract
A 37-year-old man presented with symptoms of polyuria and weight loss over the past year. Initial laboratory examination showed elevated blood glucose level (468 mg/dL [25.9 mmol/L]; normal reference range [RR], 75-109 mg/dL [4.1-6.0 mmol/L]), high glycated hemoglobin A1c (13.2% [120 mmol/mol]; RR, 4.6-6.2% [26-44 mmol/mol]), low urinary C-peptide excretion (17.4 μg/day [5.76 nmol/day]; RR, 18.3-124.4 μg/day [6.0-41.1 nmol/day]), and ketosis, leading to a diagnosis of insulin-dependent diabetes mellitus. Subsequent investigations identified medullary thyroid carcinoma and bilateral pheochromocytomas. Given the detected RET gene variant and the patient's family history of multiple endocrine neoplasia type 2A (MEN2A), the diagnosis of MEN2A was confirmed. Upon hospital admission, intensive insulin therapy was commenced, which resolved the symptoms and normalized blood glucose levels. Subsequently, laparoscopic bilateral adrenalectomy was performed, after which the patient's glucose tolerance normalized, eliminating the need for diabetes treatment and avoiding hypoglycemia. This case highlights the potential for catecholamine-induced suppression of insulin secretion via α2 action on pancreatic β-cells to be remission and rapidly improved by adrenalectomy in individuals with MEN2A experiencing insulin-dependent diabetes mellitus.
Introduction
Pheochromocytoma, a tumor of the adrenal gland, is known to potentially induce secondary diabetes mellitus [1]. Approximately 50% of individuals with pheochromocytoma exhibit glucose intolerance, and 20% to 30% develop diabetes mellitus [2, 3]. Some may experience diabetic ketoacidosis or hyperglycemic hyperosmolar syndrome [4-6].
Multiple endocrine neoplasia type 2A (MEN2A) is characterized by medullary thyroid carcinoma, pheochromocytoma, and primary hyperparathyroidism. However, the prevalence of glucose intolerance and diabetes in individuals with MEN2A remains unclear. We report a unique case of insulin-dependent diabetes mellitus and ketosis due to pheochromocytoma in a patient with MEN2A, who achieved complete remission following adrenalectomy. This is the first report to evaluate glucose tolerance before and after adrenalectomy in a patient with MEN2A characterized by insulin-dependent diabetes mellitus and ketosis.
Case Presentation
A 37-year-old man was referred to our hospital for evaluation of polyuria and significant weight loss of approximately 5 kg over the past 6 months. He had been healthy all his life, and he had no family history of diabetes, including his mother. Upon admission, he weighted 45.7 kg and measured 171.5 cm in height, resulting in a body mass index of 15.6 kg/m2. His blood pressure was 108/64 mmHg, and his pulse rate was 108 beats per minute. He was awake and alert, and other vital signs were unremarkable. Hard nodular lesions were identified in both thyroid lobes. Routine laboratory examinations indicated a severely elevated plasma glucose level (468 mg/dL [25.9 mmol/L]; normal reference range [RR], 75-109 mg/dL [4.1-6.0 mmol/L]), a high glycated hemoglobin A1c level (13.2% [120 mmol/mol]; RR, 4.6-6.2% [26-44 mmol/mol]), and the presence of ketone bodies in his urine. He was subsequently admitted for the management of diabetes mellitus and further evaluation of the enlarged thyroid glands.
Diagnostic Assessment
Ultrasound examination of the thyroid glands revealed hypoechoic masses in both thyroid lobes, characterized by irregular margins and microcalcifications. Technetium-99 m sestamibi scintigraphy demonstrated localized accumulation in the same areas, with no uptake on other sites, including the parathyroid glands. Serum carcinoembryonic antigen and calcitonin levels were elevated (123 ng/mL [123 μg/L]; RR, < 5.0 ng/mL [5.0 μg/L]) and (4410 pg/mL [1290 pmol/L]; R < 9.52 pg/mL [< 2.78 pmol/L]), respectively. Serum calcium and phosphorus and intact PTH were within the normal range. These findings led to a diagnosis of medullary thyroid carcinoma. A subsequent review of the family history disclosed that his mother had been diagnosed with MEN2A. After providing genetic counseling, informed consent was obtained. Then, genetic analysis was performed and NM_020975.6(RET):c.1900T > C (p.Cys634Arg) was detected. This variant is included in the dbSNP database (https://www.ncbi.nlm.nih.gov/snp/) with rs75076352 and classified as “Pathogenic/Likely pathogenic” in the ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/). Therefore, a diagnosis of MEN2A was genetically confirmed.
Increases in the following adrenal medulla lesion-related markers were also observed: plasma epinephrine (13,944 pg/mL [76 120 pmol/L]; RR, < 100 pg/mL [<545.9 pmol/L]), plasma norepinephrine (10 858 pg/mL [64 181 nmol/L]; RR, 100-450 pg/mL [0.5911-2660 nmol/L]), urinary metanephrine (28.05 mg/g creatinine [1423 μmol/g creatinine]; RR, 0.03-0.3 mg/g creatinine [1.52-15.2 μmol/g creatinine]), and urinary normetanephrine (8.6 mg/g creatinine [469.4 μmol/g creatinine]; RR, 0.08-0.45 mg/g creatinine [4.36-24.56 μmol/g creatinine], respectively). Computed tomography imaging revealed bilateral adrenal masses (Fig. 1A). Consistent with these findings, iodine-123-metaiodobenzylguanidine scintigraphy showed marked accumulation in these lesions, confirming the diagnosis of bilateral pheochromocytoma (Fig. 1B).
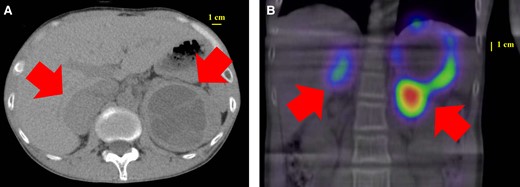
Images of CT and 123I-MIBG scintigraphy. The abdominal CT scan showed bilateral adrenal masses with a low-density area inside (A). 123I-MIBG scintigraphy showed accumulation consistent with the CT image (B). The arrows indicate the adrenal masses.
Abbreviations: CT, computed tomography; 123I-MIBG, iodine-123-metaiodobenzylguanidine.
In terms of diabetes mellitus, a meal tolerance test was performed to evaluate insulin secretory capacity. Before the test, plasma glucose and C-peptide levels were 293 mg/dL [16.3 mmol/L] and 0.61 ng/mL [0.20 nmol/L]; RR, 1.1-3.3 ng/mL [0.36-1.09 nmol/L], respectively. At 120 minutes posttest, these levels decreased to 180 mg/dL [10.0 mmol/L] and 0.52 ng/mL [0.17 nmol/L], respectively. Plasma pancreatic islet-related autoantibodies were not detected. A significant decrease in C-peptide index (0.21) and urinary C-peptide excretion (17.4 μg/day [5.76 nmol/day]; RR, 18.3-124.4 μg/day [6.0-41.1 nmol/day]) was also found. These observations led to the diagnosis of nonautoimmune-mediated insulin-dependent diabetes mellitus attributed to pheochromocytoma. He had insulin-dependent diabetes, but his blood pressure was in the normal range, and he did not experience either sustained or paroxysmal hypertension.
Treatment
His plasma glucose levels were managed with intensive insulin therapy, and the total daily dose insulin (TDD) was 39 units. After the discharge, fasting glucose level rose to around 200 mg/dL, and the TDD was increased to 46 units per day. Two months later, after readmission for the surgery for pheochromocytoma, the TDD was decreased to 19 units to prevent postoperative hypoglycemia. The patient underwent laparoscopic bilateral adrenalectomy for bilateral pheochromocytoma. Postoperatively, he needed hydrocortisone replacement therapy, but without using fludrocortisone, blood pressure and serum sodium levels remained within normal range. Both fasting and postprandial blood glucose levels were kept within the normal range without the need for insulin therapy. On the fifth postoperative day, a 75 g oral glucose tolerance test was performed, yielding normal results for glucose tolerance and insulin secretory capacity (fasting plasma glucose was 87 mg/dL [4.83 mmol/L], plasma glucose after 2 hours of 75 g oral glucose loading was 134 mg/dL [7.44 mmol/L], fasting insulin was 3.4 μIU/mL [23.6 pmol/L]; RR, 1.4-13.0 μIU/mL [9.7-90.2 pmol/L], homeostatic model assessment of β cell function was 51%, homeostatic model assessment for insulin resistance was 0.73, and insulinogenic index was 0.364). On the 19th day following the surgery, his serum C-peptide was 3.31 ng/mL [1.09 nmol/L], while fasting blood glucose levels were observed at 108 mg/dL [5.99 mmol/L], which means that his insulin secretion was recovered. Urinary metanephrine and urinary normetanephrine decreased to within the normal range on the fifth day following surgery.
Outcome and Follow-up
Two months later, he underwent total thyroidectomy for medullary thyroid carcinoma. During the procedure, no enlargement of the parathyroid glands was observed. Pathological examination confirmed partially resected parathyroid glands admixed with lymph nodes, with no evidence of parathyroid adenoma. He is now in good health and has not had a relapse of diabetes.
Discussion
In this report, we describe a rare case of diabetes mellitus characterized by marked hyperglycemia and ketosis in a patient with MEN2A. Although pheochromocytoma is well known to be associated with secondary diabetes mellitus, the frequency of abnormal glucose tolerance in MEN2A patients remains unclear. There is only 1 report, where the patient with MEN2A exhibited relatively preserved insulin secretion and borderline glucose intolerance [7]. To the best of our knowledge, there are no previous reports documenting diabetes mellitus with ketosis in the context of MEN2A, making our case the first to describe severe hyperglycemia with ketosis in this population.
Wallerstein et al reported a case of MEN2A combined with autoimmune diabetes [8]. In our case, plasma pancreatic islet-related autoantibodies were not detected, and insulin secretion improved after surgery. Therefore, diabetes in our case might be induced by excessive catecholamine secretion but not by autoimmunity.
Catecholamines cause reduced insulin secretion and insulin resistance via adrenergic receptors [9]. The cause of hyperglycemia differs depending on the type of catecholamine produced. Epinephrine affects glucose intolerance mainly by a decrease in insulin secretion via α2 receptor, while norepinephrine affects mainly by insulin resistance via α1, β1, β2, β3 receptors [10]. There is a relationship between the catecholamine levels and the severity of hyperglycemia. Pheochromocytoma patients with hyperglycemia had significantly higher 24-hour urine metanephrine and normetanephrine levels than those with normal glucose tolerance [2]. In our case, both blood and urinary C-peptide levels were markedly decreased, indicating severely decreased insulin secretion. Although the immediate insulin therapy for marked hyperglycemia and ketosis precluded the confirmation of insulin resistance indices, the presence of ketosis and diminished insulin secretion suggest that decreased insulin secretion, rather than insulin resistance.
Shimoda et al reported that the TDD in Japanese type 2 diabetes patients is <0.6 units/kg/day [11]. The TDD in this case was approximately 0.87 units/kg/day, which is higher than the average insulin requirement for Japanese type 2 diabetes patients and suggests the presence of insulin resistance before the surgery in our case. At the time of admission, the skeletal muscle mass index was 5.85 kg/m², which was significantly lower than that of adult Japanese males. Increased lipolysis and decreased glucose uptake in skeletal muscle might contribute to insulin resistance. Postoperatively, our case became low insulin resistance (homeostatic model assessment for insulin resistance 0.73).
Adrenalectomy for pheochromocytoma has been demonstrated to improve glycemic control in more than 90% of patients, with 79% returning to normal glucose tolerance [3]. There is also a report that diabetes can remit after surgery in patients with bilateral pheochromocytoma associated with MEN2A [12]. Our case is the first report that insulin-dependent diabetes remitted after bilateral adrenalectomy in a patient with MEN2A-associated pheochromocytoma. Khatiwada et al reported that having diabetes for less than 3 years is a predicter of remission of diabetes after surgery [13]. The duration between the onset of pheochromocytoma and diabetes might be short in our case.
Postoperative hypoglycemia, which can arise from the remission of suppressed insulin secretion and improved insulin resistance, requires careful monitoring. This complication is observed not only in insulin-using patients but also in those with glucose intolerance who did not use insulin and even in patients with normal glucose tolerance [14]. A study indicated that high preoperative urinary metanephrine levels may be associated with postoperative hypoglycemia [9]. Given the high urinary metanephrine levels and insulin-dependent status in our case, there was a pronounced risk for postoperative hypoglycemia, necessitating intensive monitoring due to the dual risks of preoperative insulin use and elevated catecholamine levels. We preemptively discontinued insulin therapy on the day of surgery, which successfully prevented hypoglycemia. Insulin secretion improved immediately after adrenalectomy without any hypoglycemic episodes. This outcome suggests that the risk of postoperative hypoglycemia can be reduced by discontinuing insulin therapy and closely monitoring blood glucose levels after surgery, even in patients with preoperative insulin dependence.
Catecholamine production pattern in MEN2A-associated pheochromocytoma differ from other hereditary pheochromocytomas [15, 16]. Excessive epinephrine secretion in MEN2A-associated pheochromocytomas leads to a decrease in insulin secretion compared to other types of pheochromocytomas [10]. Thus, severe diabetes in our case was developed due to the highly suppressed insulin secretion by excessive epinephrine secretion.
Learning Points
Bilateral pheochromocytoma in patients with MEN2A may suppress insulin secretion via α2 action on pancreatic β cells, potentially resulting in an insulin-dependent state.
Even in patients with bilateral pheochromocytoma in MEN2A who are in an insulin-dependent state, insulin secretion may rapidly recover to the normal range following bilateral adrenalectomy.
Postoperative discontinuation of insulin and careful monitoring of blood glucose levels can effectively reduce the risk of postoperative hypoglycemia.
Acknowledgments
Tetsuya Babazono contributed by advising our practice.
Contributors
All authors made individual contributions to authorship. M.S., M.O., T.Y., T.M., and T.N. were involved in the diagnosis and management of this patient and manuscript submission. J.Y. was responsible for the patient's surgeries. All authors reviewed and approved the final draft.
Funding
No public or commercial funding.
Disclosures
M.O. is a JCEM Case Reports Editorial Board member and played no role in the journal's evaluation of the manuscript. No other disclosures are declared.
Informed Patient Consent for Publication
Signed informed consent was obtained directly from the patient.
Data Availability Statement
Original data generated and analyzed during this study are included in this published article.



