-
PDF
- Split View
-
Views
-
Cite
Cite
Bertrand Barres, Antony Kelly, Fabrice Kwiatkowski, Marie Batisse-Lignier, Geneviève Fouilhoux, Bernadette Aubert, Frédéric Dutheil, Igor Tauveron, Florent Cachin, Salwan Maqdasy, Stimulated Thyroglobulin and Thyroglobulin Reduction Index Predict Excellent Response in Differentiated Thyroid Cancers, The Journal of Clinical Endocrinology & Metabolism, Volume 104, Issue 8, August 2019, Pages 3462–3472, https://doi.org/10.1210/jc.2018-02680
Close - Share Icon Share
Abstract
Despite its good prognosis, differentiated thyroid cancer (DTC) is characterized by high rates of disease persistence and recurrence. Estimation of long-term remission (excellent response) thanks to specific parameters could help to individualize the active surveillance schedule.
Evaluation of the ability of stimulated thyroglobulin (Tg) and Tg reduction index (TRI) to predict long-term remission in patients with DTC managed by thyroidectomy and radioactive iodine (RAI) remnant ablation.
Observational retrospective study of 1093 patients treated for DTC between 1995 and 2010. Preablation stimulated thyroglobulin (presTg) was measured under thyroid hormone withdrawal just before RAI. Recombinant human TSH–stimulated thyroglobulin (sTg) was measured at first evaluation of the initial management 6 to 12 months after RAI. TRI was calculated based on pre-Tg and sTg.
After univariate and multivariate analyses, lymph node invasion (N1, OR = 2.08; 95% CI, 1.19 to 3.64), presTg (OR = 4.04; 95% CI, 2.56 to 6.38), sTg (OR = 2.62; 95% CI, 2.05 to 3.34), and TRI (OR = 0.43; 95% CI, 0.21 to 0.88) were identified as independent prognostic factors influencing the rate of disease persistence or recurrence after the initial management. Receiver operating characteristic analysis identified presTg cutoff (<10 µg/L) to predict excellent response, with a negative predictive value of 94%, and validated for higher stages (T3/T4, N1). Furthermore, sTg <1 µg/L predicts excellent response. TRI >60% for the entire cohort and 62.5% for locally advanced disease (T3/T4, N1) was sensitive predictor for excellent response.
This study identifies presTg, sTg, and TRI as highly sensitive predictors of excellent response in patients with DTC and subsequently disease-free status. The cutoff of such parameters is also adapted for patients with higher tumor stages (T3/T4, N1).
Differentiated thyroid cancer (DTC) is the most common endocrine cancer and accounts for 90% of thyroid malignancies (1). The incidence of DTC has increased in the last 20 years (2, 3), mainly because of mass screening for thyroid pathologies by ultrasound (1). Indeed, 87% of “overdiagnosed” malignancies represent occult papillary cancers (<2 cm) (1). Fortunately, the prognosis is excellent, with a mean 10-year survival estimated at 90%. Management of DTC is based on total or near total thyroidectomy with or without remnant thyroid ablation by radioactive iodine (RAI) according to tumor staging and the risk of disease recurrence (4). Despite its good prognosis, DTC is characterized by a high risk of disease persistence and recurrence, suggesting the need for long-term active surveillance (3).
Recent recommendations include identifying patients with excellent response to the initial management to reduce follow-up and consequently decrease the psychological and economic burden on such patients (5, 6). Indeed, parameters in favor of excellent response or long-term remission are necessary to individualize the management of each patient. To date, American Thyroid Association (ATA) recommendations have been based mainly on TNM staging to determine the need for RAI remnant ablation, and on thyroglobulin (Tg) levels. Indeed, initial stimulated or preablation stimulated thyroglobulin (presTg) just before RAI reflects the residual disease after surgery and points out the presence of eventual occult distant metastases, even if morphological imaging is negative (7). Moreover, stimulated Tg measured after recombinant human TSH (rhTSH) stimulation 9 to 12 months after RAI (sTg) predicts the possible long-term remission and biochemical or structural incomplete response. A cutoff <1 µg/L suggests long-term remission and reflects a prolonged recurrence-free survival (8–10).
Indeed, presTg has been evaluated by many studies, and different cutoffs have been suggested to predict persistent or recurrent disease [meta-analyzed in (11)]. These studies confirmed the negative predictive value (NPV) associated with low presTg levels to predict disease recurrence. But the number of included patients was low, ranging from 63 to 450 patients. Furthermore, these studies suggested different cutoffs ranging from 3 to 30 µg/L. Besides, the evolution could be surprising in both negative and positive directions, even more, spontaneous Tg reduction was often reported (12, 13). Indeed, more parameters are needed for initial risk appraisal. Thyroglobulin reduction index (TRI) reflects the response to RAI and the degree of tissue destruction. To the best of our knowledge, no study evaluated the predictive value of presTg to predict an excellent response to the initial management, especially for locally advanced disease. Furthermore, TRI as a concept has never been suggested, and its impact on long-term survival has never been evaluated.
The objective of this study was to evaluate the ability of presTg and TRI to predict an excellent response or long-term remission in patients with DTC (including those with locally advanced disease) managed by thyroidectomy and RAI remnant ablation.
Patients and Methods
We have conducted an observational retrospective study to analyze the clinical, biological, and morphological data for patients treated for DTC (surgery and RAI) in our tertiary center between 1995 and 2010 and still followed up.
Database and inclusion
In 1995 we established a clinical database, “Registre Thyroïde Auvergne,” to continuously update patients’ clinical, histological, biological, and morphological data. Since then, 1500 patients who needed complementary RAI have been included in the register, with a follow-up of 5 to 15 years. Microcancers were excluded. Disease evolution including cancer persistence, recurrence, and localization, surgical procedures, and complementary treatments are regularly registered for each patient. The TNM staging system of the American Joint Committee on Cancer 2010 (7th edition) was used. Nevertheless, we took in consideration thyroid capsule invasion (the difference between T2 and T3) and tumor size in our cohort to be compatible with the new TNM system published just after the completion of the collection of our variables (2017).
Biochemical and structural incomplete response are also documented. For each patient, the decision between complementary RAI, reoperation, or active surveillance is made through a multidisciplinary regular meeting respecting the national recommendations.
We have limited the analysis to patients included between January 1995 and December 2010 to obtain ≥7-year follow-up after the initial management.
Thyroid cancer ablation protocol and follow-up
All patients underwent a total thyroidectomy, either at our institution or at a regional hospital, followed by complementary RAI ablation (100 mCi). A detailed histopathological description of the DTC with its particularities (cell types), extension, and staging was performed for all patients. RAI complementary ablation was systematically decided by a multidisciplinary meeting.
All RAI was administered under thyroid hormone withdrawal (THW). THW consisted of LT4 withdrawal during the 5 weeks leading up to RAI administration. LT4 was substituted with LT3 during the first 3 weeks, then stopped. presTg and anti-Tg antibodies were evaluated in the day of RAI therapy. A diagnostic RAI whole-body scintiscan (WBS) was performed on day 5 after RAI to document the RAI avidity of any structural disease or thyroid remnant. Six to 12 months after RAI administration, measurement of sTg, WBS, and cervical ultrasonography were performed to evaluate response to initial treatment and Tg status (sTg). Afterward, patients were followed up through clinical checkup, laboratory testing, and ultrasonography. In selected cases, additional CT imaging with varying intervals was chosen.
Thyroglobulin measurement
Thyroglobulin measurement method did not change throughout the study. The measurement was performed in the laboratory of radiopharmacology in Jean Perrin Center, with the minimal detectable value of 0.1 µg/L. Immunoradiometric assay with coated tubes (CisBio:TgIRMA) was used for Tg measurement, and an interference evaluation with antibodies was performed.
Exclusion
To harmonize management, patients with microcancer, patients treated with RAI after rhTSH stimulation instead of THW, patients with positive antithyroglobulin levels, and those missing Tg measurements were excluded from the analyzed cohort.
Definitions
Initial management reflects the initial thyroidectomy followed by remnant ablation by RAI. Long-term remission (excellent response) is defined as the absence of biochemical or morphological signs in favor of disease persistence or recurrence after the initial management, and the absence of any need for a second treatment (reoperation or adjuvant RAI).
presTg was measured after THW and just before RAI. RAI is usually administered within a couple of months after thyroidectomy. sTg was measured 72 hours after rhTSH during the evaluation of the initial management, usually performed 6 to 12 months after RAI. TRI was calculated based on presTg and sTg [TRI = 100 × (presTg − sTg)/presTg].
Persistent disease was defined based on the identification of structural or biochemical persistence of cancer after the initial management.
Recurrent disease was defined as evidence of disease reemergence (structural lesion identified by ultrasound, WBS, or biochemical increment of Tg) after an initial remission. Disease recurrence was detected via regular radiological and biochemical monitoring of these patients.
Evaluation of long-term remission and disease recurrence or persistence
Long-term remission or excellent response is identified through the biological (Tg) and morphological (ultrasound, CT scan, and radioisotope scan) results obtained after RAI remnant ablation. Biological and morphological evaluation was also performed 6 to 12 months after RAI after rhTSH stimulation. Undetectable sTg, normal cervical ultrasound, and normal radioisotope scan (0.18 GBq of 131I) suggest a long-term remission or excellent response.
Any anomaly persisting during the initial evaluation is considered disease persistence (incomplete biochemical or structural response). Disease recurrence is defined as the appearance of biochemical or structural anomalies in patients previously considered in remission.
Ethical issues
Study ethics approval was obtained on 30 June 2017 (CECIC Rhône-Alpes-Auvergne, Grenoble), IRB 5921.
Statistical analysis
The statistical analysis aimed first to describe the general characteristics of the population at inclusion. Quantitative parameters are expressed as means with SD (median and range if distribution is not Gaussian), and qualitative parameters are described in terms of population size and frequency. For the principal analysis, Student t test or Kruskal-Wallis H test (depending on normality and homoscedasticity of distributions) was used to identify the link between different quantitative parameters and disease remission from one side and persistence or recurrence on the other side. Statistical link between qualitative parameters was performed via χ2 test, and ANOVA or Kruskal-Wallis H tests were used for the association between qualitative and quantitative parameters. Pearson correlation or Spearman rank correlation was used to test the relation between two quantitative variables. The relative influence of several parameters was confirmed by a multivariate logistic regression analysis for dichotomous parameters and with the proportional hazard Cox model for survival variables. Because collinearity was logically found between presTg and sTg, we reanalyzed the Cox model with either parameter in the Cox model. When results were similar between the first model (both parameters) and the second (either parameter), the first model is presented.
For secondary analyses, receiver operating characteristic (ROC) curves (area under the curve and corresponding 95% CI) were used to obtain most sensitive and specific cutoffs for biological parameters. Area under the curve >0.7 suggested a valid estimation of the cutoff. The prognostic value of different factors affecting the persistence or recurrence-free survival was estimated by Kaplan-Meier method. Tumor recurrence was defined as described above, and survival delay was calculated from diagnosis to discover the first recurrence. Persistence or recurrence was compared with excellent response (no persistence, no recurrence, no second surgical or RAI treatment) to evaluate survival.
Statistical comparisons were achieved with log-rank and Mantel-Haenszel tests. All tests were two-sided, and a standard P-value <0.05 was used as the significance threshold. Structural equation modeling software was used for data management and statistical calculations (14).
Results
Population characteristics
A total of 1319 patients with DTC were treated between 1995 and 2010. After exclusion for one the reasons mentioned earlier, data from 1093 patients were analyzed. The median follow-up was 5.6 years (1 to 18 years), with a follow-up of >3 years in >80% of the included population. Long-term remission or excellent response was obtained in 79%, whereas 16% had disease persistence and 4.3% had disease recurrence (Fig. 1).
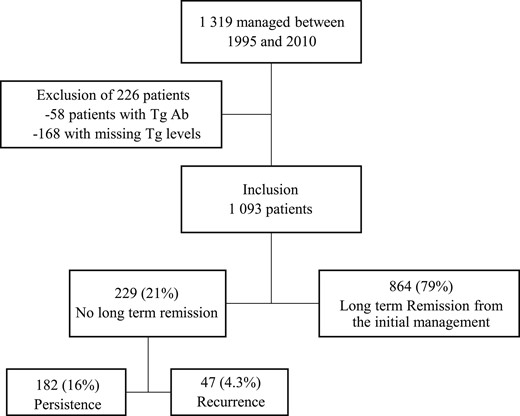
Flowchart summarizing patients’ inclusion at the study. Tg Ab, anti-thyroglobulin antibodies.
In this cohort, 78.4% of patients were women, the mean age was 48.9 years (SD 14.8; 95% CI, 48 to 50). Papillary thyroid cancer represents 88.5% of the histologies of the cohort. The mean lesion diameter was 1.9 cm (SD 1.48; 95% CI, 0.05 to 12.0). On staging, 55.8% of patients had T1, 19.4% had T2, 22.1% had T3, and 2.4% had T4 on histopathology. Multifocal lesions were present in 404 patients. Thyroid capsule invasion was documented for 263 patients. The number of patients presenting with lymph node (LN) invasion or N1 was 134, with a mean number of invaded LN of 4.3 (SD 4.3; 95% CI, 1 to 13). LN capsule rupture was present in 57 patients. Distant metastases (M1) were present in 29 patients. Mean presTg, sTg, and TRI were 110 µg/L, 74 µg/L, and 37.5% respectively. The general characteristics of the cohort are summarized in Table 1.
| . | Number or Value . | SD or % . |
|---|---|---|
| Sex, n | ||
| Female | 857 | 78.4% |
| Male | 236 | 21.6% |
| Age, y | 48.9 | 14.82 |
| Histological type, n | ||
| Papillary | 982 | 88.5% |
| Follicular | 127 | 11.5% |
| Main lesion diameter, cm | 1.9 | 1.47 |
| T, n | ||
| T1 | 606 | 55.8% |
| T2 | 211 | 19.4% |
| T3 | 240 | 22.1% |
| T4 | 26 | 2.4% |
| Multifocal, n | 404 | 37.2% |
| Thyroid capsule invasion, n | 263 | 24.4% |
| Number of invaded LNs | 4.3 | 4.29 |
| N, n | ||
| Nx | 788 | 72.4% |
| N0 | 143 | 13.1% |
| N1a | 87 | 8% |
| N1b | 47 | 4.3% |
| LN capsule rupture, n | 57 | 42.9% |
| M, n | ||
| Mx | 257 | 27.6% |
| M0 | 646 | 69.3% |
| M1 | 29 | 3.1% |
| PresTg, µg/L, mean | 110.9 | 1685 |
| PresTg <1 µg/L | 510 | 46.7% |
| PresTg 1–10 µg/L | 346 | 31.7% |
| PresTg >10 µg/L | 237 | 21.7% |
| sTg, µg/L, mean | 74.2 | 2221 |
| TRI, mean % | 37.5 | 304 |
| . | Number or Value . | SD or % . |
|---|---|---|
| Sex, n | ||
| Female | 857 | 78.4% |
| Male | 236 | 21.6% |
| Age, y | 48.9 | 14.82 |
| Histological type, n | ||
| Papillary | 982 | 88.5% |
| Follicular | 127 | 11.5% |
| Main lesion diameter, cm | 1.9 | 1.47 |
| T, n | ||
| T1 | 606 | 55.8% |
| T2 | 211 | 19.4% |
| T3 | 240 | 22.1% |
| T4 | 26 | 2.4% |
| Multifocal, n | 404 | 37.2% |
| Thyroid capsule invasion, n | 263 | 24.4% |
| Number of invaded LNs | 4.3 | 4.29 |
| N, n | ||
| Nx | 788 | 72.4% |
| N0 | 143 | 13.1% |
| N1a | 87 | 8% |
| N1b | 47 | 4.3% |
| LN capsule rupture, n | 57 | 42.9% |
| M, n | ||
| Mx | 257 | 27.6% |
| M0 | 646 | 69.3% |
| M1 | 29 | 3.1% |
| PresTg, µg/L, mean | 110.9 | 1685 |
| PresTg <1 µg/L | 510 | 46.7% |
| PresTg 1–10 µg/L | 346 | 31.7% |
| PresTg >10 µg/L | 237 | 21.7% |
| sTg, µg/L, mean | 74.2 | 2221 |
| TRI, mean % | 37.5 | 304 |
| . | Number or Value . | SD or % . |
|---|---|---|
| Sex, n | ||
| Female | 857 | 78.4% |
| Male | 236 | 21.6% |
| Age, y | 48.9 | 14.82 |
| Histological type, n | ||
| Papillary | 982 | 88.5% |
| Follicular | 127 | 11.5% |
| Main lesion diameter, cm | 1.9 | 1.47 |
| T, n | ||
| T1 | 606 | 55.8% |
| T2 | 211 | 19.4% |
| T3 | 240 | 22.1% |
| T4 | 26 | 2.4% |
| Multifocal, n | 404 | 37.2% |
| Thyroid capsule invasion, n | 263 | 24.4% |
| Number of invaded LNs | 4.3 | 4.29 |
| N, n | ||
| Nx | 788 | 72.4% |
| N0 | 143 | 13.1% |
| N1a | 87 | 8% |
| N1b | 47 | 4.3% |
| LN capsule rupture, n | 57 | 42.9% |
| M, n | ||
| Mx | 257 | 27.6% |
| M0 | 646 | 69.3% |
| M1 | 29 | 3.1% |
| PresTg, µg/L, mean | 110.9 | 1685 |
| PresTg <1 µg/L | 510 | 46.7% |
| PresTg 1–10 µg/L | 346 | 31.7% |
| PresTg >10 µg/L | 237 | 21.7% |
| sTg, µg/L, mean | 74.2 | 2221 |
| TRI, mean % | 37.5 | 304 |
| . | Number or Value . | SD or % . |
|---|---|---|
| Sex, n | ||
| Female | 857 | 78.4% |
| Male | 236 | 21.6% |
| Age, y | 48.9 | 14.82 |
| Histological type, n | ||
| Papillary | 982 | 88.5% |
| Follicular | 127 | 11.5% |
| Main lesion diameter, cm | 1.9 | 1.47 |
| T, n | ||
| T1 | 606 | 55.8% |
| T2 | 211 | 19.4% |
| T3 | 240 | 22.1% |
| T4 | 26 | 2.4% |
| Multifocal, n | 404 | 37.2% |
| Thyroid capsule invasion, n | 263 | 24.4% |
| Number of invaded LNs | 4.3 | 4.29 |
| N, n | ||
| Nx | 788 | 72.4% |
| N0 | 143 | 13.1% |
| N1a | 87 | 8% |
| N1b | 47 | 4.3% |
| LN capsule rupture, n | 57 | 42.9% |
| M, n | ||
| Mx | 257 | 27.6% |
| M0 | 646 | 69.3% |
| M1 | 29 | 3.1% |
| PresTg, µg/L, mean | 110.9 | 1685 |
| PresTg <1 µg/L | 510 | 46.7% |
| PresTg 1–10 µg/L | 346 | 31.7% |
| PresTg >10 µg/L | 237 | 21.7% |
| sTg, µg/L, mean | 74.2 | 2221 |
| TRI, mean % | 37.5 | 304 |
Predictive factors of long-term remission after initial management
Univariate analysis
To determine the predictive factors for long-term remission after initial management, univariate analyses isolated sex, tumor stage T (including thyroid capsule invasion), LN involvement (N1), LN capsule rupture, presTg, sTg, and TRI as predictive factors. Patients with long-term remission had significantly lower presTg and sTg and higher TRI. Age and multifocal lesion were not predictive factors (Table 2).
Univariate Analysis Determining the Predictive Factors in Length of Remission
| Parameters . | Long-Term Remission . | Persistence or Recurrence . | P . |
|---|---|---|---|
| No. of patients (%) | 864 (79%) | 229 (21%) | |
| Sex, n | |||
| Female | 700 | 156 | <0.0001 |
| Male | 164 | 73 | |
| Mean age (SD), y | 37.3 (24.4) | 40.5 (23.5) | ns |
| Tumor diameter (SD), cm | 1.79 (1.35) | 2.31 (1.81) | < 0.0001 |
| T, n | <10−7 | ||
| T1 | 515 | 91 | |
| T2 | 170 | 41 | |
| T3 | 165 | 75 | |
| T4 | 8 | 18 | |
| Thyroid capsule invasion, n | 178 | 85 | <10−6 |
| N, n | <10−7 | ||
| Nx | 659 | 129 | |
| N0 | 121 | 22 | |
| N1 | 14 | 10 | |
| N1a | 43 | 44 | |
| N1b | 24 | 23 | |
| LN capsule rupture, n | 0.0073 | ||
| Yes | 25 | 32 | |
| No | 51 | 25 | |
| PresTg, no. of patients | 864 | 229 | <10−7 |
| Mean (SD) | 10.9 (162.9) | 488 (3643) | |
| Tg <1 µg/L | 329 | 17 | |
| Tg 1–10 µg/L | 429 | 81 | |
| Tg >10 µg/L | 106 | 131 | |
| sTg (mean ± SD), µg/L | 0.75 (5.72) | 432 (5360) | <10−7 |
| TRI (mean ± SD), % | |||
| When presTg > 10 µg/L | 92.2 (30) | 77.6 (77.9) | <0.001 |
| When presTg < 10 µg/L | 35.6 (323) | −156 (855) | <0.00001 |
| Parameters . | Long-Term Remission . | Persistence or Recurrence . | P . |
|---|---|---|---|
| No. of patients (%) | 864 (79%) | 229 (21%) | |
| Sex, n | |||
| Female | 700 | 156 | <0.0001 |
| Male | 164 | 73 | |
| Mean age (SD), y | 37.3 (24.4) | 40.5 (23.5) | ns |
| Tumor diameter (SD), cm | 1.79 (1.35) | 2.31 (1.81) | < 0.0001 |
| T, n | <10−7 | ||
| T1 | 515 | 91 | |
| T2 | 170 | 41 | |
| T3 | 165 | 75 | |
| T4 | 8 | 18 | |
| Thyroid capsule invasion, n | 178 | 85 | <10−6 |
| N, n | <10−7 | ||
| Nx | 659 | 129 | |
| N0 | 121 | 22 | |
| N1 | 14 | 10 | |
| N1a | 43 | 44 | |
| N1b | 24 | 23 | |
| LN capsule rupture, n | 0.0073 | ||
| Yes | 25 | 32 | |
| No | 51 | 25 | |
| PresTg, no. of patients | 864 | 229 | <10−7 |
| Mean (SD) | 10.9 (162.9) | 488 (3643) | |
| Tg <1 µg/L | 329 | 17 | |
| Tg 1–10 µg/L | 429 | 81 | |
| Tg >10 µg/L | 106 | 131 | |
| sTg (mean ± SD), µg/L | 0.75 (5.72) | 432 (5360) | <10−7 |
| TRI (mean ± SD), % | |||
| When presTg > 10 µg/L | 92.2 (30) | 77.6 (77.9) | <0.001 |
| When presTg < 10 µg/L | 35.6 (323) | −156 (855) | <0.00001 |
Abbreviation: ns, not significant.
Univariate Analysis Determining the Predictive Factors in Length of Remission
| Parameters . | Long-Term Remission . | Persistence or Recurrence . | P . |
|---|---|---|---|
| No. of patients (%) | 864 (79%) | 229 (21%) | |
| Sex, n | |||
| Female | 700 | 156 | <0.0001 |
| Male | 164 | 73 | |
| Mean age (SD), y | 37.3 (24.4) | 40.5 (23.5) | ns |
| Tumor diameter (SD), cm | 1.79 (1.35) | 2.31 (1.81) | < 0.0001 |
| T, n | <10−7 | ||
| T1 | 515 | 91 | |
| T2 | 170 | 41 | |
| T3 | 165 | 75 | |
| T4 | 8 | 18 | |
| Thyroid capsule invasion, n | 178 | 85 | <10−6 |
| N, n | <10−7 | ||
| Nx | 659 | 129 | |
| N0 | 121 | 22 | |
| N1 | 14 | 10 | |
| N1a | 43 | 44 | |
| N1b | 24 | 23 | |
| LN capsule rupture, n | 0.0073 | ||
| Yes | 25 | 32 | |
| No | 51 | 25 | |
| PresTg, no. of patients | 864 | 229 | <10−7 |
| Mean (SD) | 10.9 (162.9) | 488 (3643) | |
| Tg <1 µg/L | 329 | 17 | |
| Tg 1–10 µg/L | 429 | 81 | |
| Tg >10 µg/L | 106 | 131 | |
| sTg (mean ± SD), µg/L | 0.75 (5.72) | 432 (5360) | <10−7 |
| TRI (mean ± SD), % | |||
| When presTg > 10 µg/L | 92.2 (30) | 77.6 (77.9) | <0.001 |
| When presTg < 10 µg/L | 35.6 (323) | −156 (855) | <0.00001 |
| Parameters . | Long-Term Remission . | Persistence or Recurrence . | P . |
|---|---|---|---|
| No. of patients (%) | 864 (79%) | 229 (21%) | |
| Sex, n | |||
| Female | 700 | 156 | <0.0001 |
| Male | 164 | 73 | |
| Mean age (SD), y | 37.3 (24.4) | 40.5 (23.5) | ns |
| Tumor diameter (SD), cm | 1.79 (1.35) | 2.31 (1.81) | < 0.0001 |
| T, n | <10−7 | ||
| T1 | 515 | 91 | |
| T2 | 170 | 41 | |
| T3 | 165 | 75 | |
| T4 | 8 | 18 | |
| Thyroid capsule invasion, n | 178 | 85 | <10−6 |
| N, n | <10−7 | ||
| Nx | 659 | 129 | |
| N0 | 121 | 22 | |
| N1 | 14 | 10 | |
| N1a | 43 | 44 | |
| N1b | 24 | 23 | |
| LN capsule rupture, n | 0.0073 | ||
| Yes | 25 | 32 | |
| No | 51 | 25 | |
| PresTg, no. of patients | 864 | 229 | <10−7 |
| Mean (SD) | 10.9 (162.9) | 488 (3643) | |
| Tg <1 µg/L | 329 | 17 | |
| Tg 1–10 µg/L | 429 | 81 | |
| Tg >10 µg/L | 106 | 131 | |
| sTg (mean ± SD), µg/L | 0.75 (5.72) | 432 (5360) | <10−7 |
| TRI (mean ± SD), % | |||
| When presTg > 10 µg/L | 92.2 (30) | 77.6 (77.9) | <0.001 |
| When presTg < 10 µg/L | 35.6 (323) | −156 (855) | <0.00001 |
Abbreviation: ns, not significant.
Multivariate analyses
N1 (OR 2.08), presTg (OR 4.04), sTg (OR 2.62), and TRI (OR 0.43) were independent predictive factors for persistent or recurrent disease vs long-term remission in multivariate analysis (Fig. 2). Indeed, the predictive value of these parameters was confirmed, whether they were included as continuous (Fig. 2A) or categorical variables (PresTg >1 µg/L and sTg <1 µg/L) (Fig. 2B). However, the T value differs between these types of analyses. T staging (T2, T3, T4) significantly influenced prognosis in our cohort only when Tg values (both presTg and sTg) were included as categorical in the multivariate analysis.
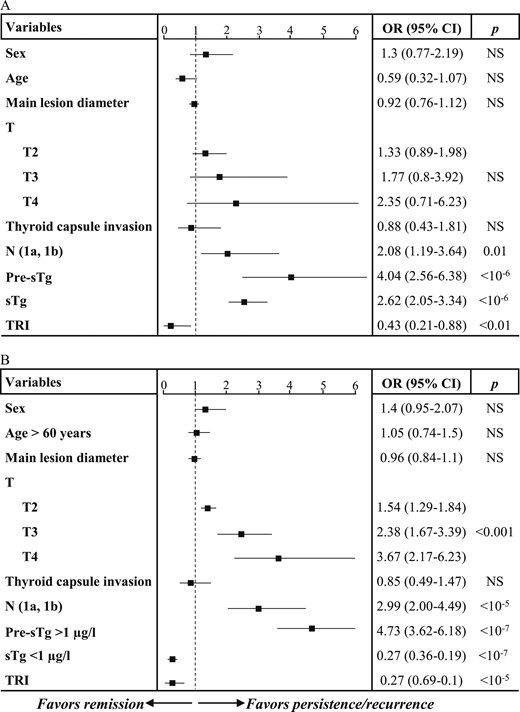
Multivariate analysis of predictive factors in favor of long-term remission (excellent response) vs nonremission (disease persistence or recurrence). (A) Cox model taking into consideration Tg levels as continuous variables. (B) Cox model taking in consideration categorical classification of Tg levels. NS, not significant.
Prognostic value of presTg in terms of long-term remission
In multivariate analysis presTg was the most significant independent predictive factor for long-term remission. The risk of disease persistence or recurrence was 5 times and 22 times higher when presTg was >5 µg/L and >10 µg/L, respectively (Fig. 3A). With the cutoff set at 10 µg/L, 755 patients out of 835 (90%) obtained long-term remission from the initial management (Fig. 3B). ROC analysis identified presTg <10 µg/L as a sensitive predictor for long-term remission. The sensitivity and specificity of this value were 75% and 72%, respectively. The positive predictive value was low (41%) but with a high NPV (94%) (Fig. 3C). Kaplan-Meier analysis confirmed the predictive value of presTg on long-term remission. Indeed, the rate of excellent response was significantly reduced when presTg > 10 µg/L (Fig. 3D).
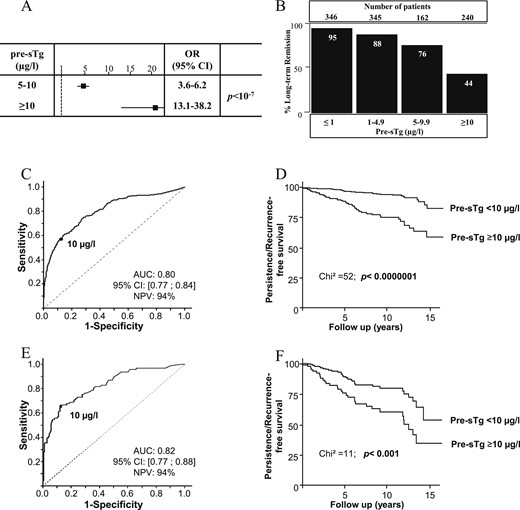
Prognostic impact of presTg on disease remission and persistence or recurrence of DTC. (A) Multivariate analysis demonstrated the impact of presTg on the risk of disease persistence or recurrence (nonremission). (B) Repartition of patients who are in long-term remission according to their presTg levels. (C) ROC analysis determining the cutoff of presTg to determine long-term remission in patients with DTC. The threshold was determined by identifying the presTg that maximized sensitivity and specificity. (D) Kaplan-Meier analysis of persistence and recurrence-free survival according to the identified presTg cutoff. (E) ROC analysis determining the cutoff of presTg to determine long-term remission of locally advanced DTC (T3–T4/Nx–N1). (F) Kaplan-Meier analysis of persistence and recurrence-free survival according to the identified presTg cutoff in locally advanced DTC (T3–T4/Nx–N1). Persistance/recurrence-free survival represents “event-free survival” during patients' follow up. AUC, area under the curve.
PresTg cutoff for locally advanced disease
In multivariate analysis, T and N were further predictive factors for remission (Fig. 2). PresTg was studied in the subpopulation T3 to T4/Nx and T3 to T4/N1. In this population, with ROC analyses, presTg cutoff 10 µg/L had an NPV of 84% in favor of long-term remission (Fig. 3E). The Kaplan-Meier analysis confirmed the importance of this cutoff in the estimation of long-term remission (Fig. 3F).
Prognostic value of sTg
Considering the new recommendations, sTg is very sensitive for predicting an excellent response to the initial management.
To confirm such sensitivity in our cohort, we performed an ROC analysis that identified the same cutoff (<1 µg/L) to define an excellent response or long-term remission (Fig. 4A). Persistence or recurrence-free survival was greatly reduced when sTg was ≥1 µg/L (Fig. 4B). The same cutoff was valid for the locally advanced disease (Fig. 4C). Also, sTg was highly correlated with disease persistence, locoregional recurrence, and distant metastases. Furthermore, sTg was significantly correlated with presTg (P < 0.0000001). To explore this correlation, we studied TRI value in relation to disease prognosis.
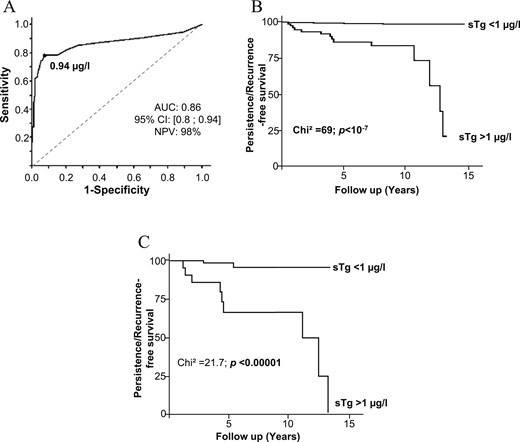
Prognostic impact of sTg on disease remission and persistence or recurrence of DTC. (A) ROC analysis determining the threshold of sTg to determine long-term remission of patients with DTC. (B) Kaplan-Meier analysis of persistence or recurrence-free survival according to the identified sTg cutoff for patients with DTC. (C) Kaplan-Meier analysis of persistence or recurrence-free survival according to the identified sTg cutoff in locally advanced DTC (T3–T4/Nx–N1). Persistance/recurrence-free survival represents “event-free survival” during patients' follow up. AUC, area under the curve.
Prognostic value of TRI
TRI was calculated as described in the Methods section. ROC analysis identified a TRI cutoff of 60% that predicted long-term remission and improved the persistence and recurrence-free survival (Fig. 5A). In multivariate analysis, TRI >60% was an independent predictive factor of persistence or recurrence-free survival (Fig. 5B). Subgroup analysis limited to patients with T3 to T4/N1 identified the importance of TRI in such a locally advanced stage. Indeed, a TRI >62.5% predicted an excellent persistence or recurrence-free survival, independent of tumor status for the entire group or those with T1/T2 tumors (NPV 96%, P < 0.0000001) (Fig. 5C, 5D).
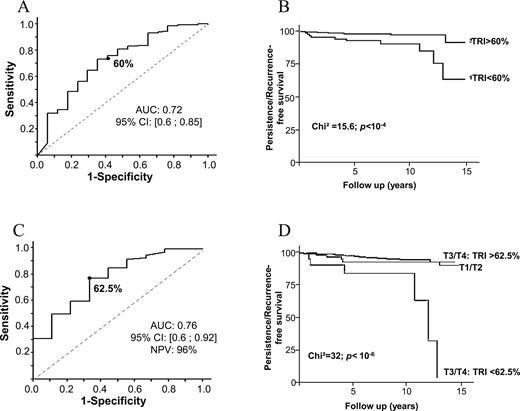
Prognostic impact of TRI on disease remission and recurrence of DTC. (A) ROC analysis determining the optimal threshold of TRI to determine tumor recurrence in patients with DTC. The threshold was determined by identifying the TRI percentage that maximized sensitivity and specificity with a point that is farthest from chance. (B) Kaplan-Meier analysis of persistence and recurrence-free survival according to the identified TRI cutoff for patients with DTC. (C) ROC analysis determining the optimal threshold of TRI to determine tumor persistence or recurrence in patients with locally advanced DTC (T3–T4/Nx–N1). (D) Kaplan-Meier analysis of persistence and recurrence-free survival according to the identified TRI cutoff for patients with locally advanced DTC (T3–T4/Nx–N1). Persistance/recurrence-free survival represents “event-free survival” during patients' follow up. AUC, area under the curve.
Specific populations
In patients with no structurally identifiable disease at initial management (normal ultrasound and absence of fixation on scintiscan) who will have structural disease persistence or recurrence, we analyzed presTg, sTg, and TRI predictive values. In this population of 22 patients, the median presTg was 22.9 µg/L (1.1 to 268 µg/L), sTg was 6.35 µg/L (0.1 to 46.8 µg/L), and median TRI was 33% (−20% to 95%). The sensitivity of presTg, sTg, and TRI to determine disease persistence or recurrence was 73%, 93%, and 41%, respectively. Low sensitivity of TRI was related to high presTg levels. Indeed, all patients with TRI >60% had presTg >10 µg/L. Combining presTg and TRI raises the sensitivity to 100% to predict long-term remission.
In patients with atypical histological findings with known aggressive character (tall, cylindrical, and trabecular cells, sclerosing and insular types), we analyzed presTg, sTg, and TRI value in terms of prediction of excellent response. We identified 21 patients in our cohort. The rate of remission was significantly lower compared with the whole cohort (62% vs 80%, P < 0.05). For patients with remission compared with persistent or recurrent disease, the median presTg was 2.8 µg/L (2.3 to 6.2 µg/L) vs 12.3 µg/L (6.1 to 24.5 µg/L) (P < 0.05), sTg was 0.2 µg/L (0.2 to 0.25 µg/L) vs 6 µg/L (3.11 to 6.8 µg/L) (P < 0.0001), and the median TRI was 95.6% (92.3% to 96.7%) vs 52% (28% to 65%) (P < 0.01). The sensitivities of these parameters (presTg, sTg and TRI) were 76.1%, 100%, and 90.4%, respectively. These parameters remain valuable in these patients.
Discussion
We have studied 1093 patients treated with thyroidectomy and remnant thyroid ablation in our center. Over a mean follow-up of 5.6 years, 79% (864 patients) had a long-term remission from their cancer thanks to the initial management, whereas 17% (182 patients) and 4% (47 patients) had disease persistence and recurrence, respectively.
This study demonstrates the prognostic value of the initial presTg, sTg, and TRI in predicting long-term remission in different tumor stages, including locally advanced disease (T3 to T4/N1). Indeed, presTg <10 µg/L, sTg <1 µg/L, and TRI >60% are excellent predictors for long-term remission and persistence or recurrence-free survival. In locally advanced tumors, a cutoff of presTg of 10 µg/L, sTg <1 µg/L, and TRI >62.5% are precious predictors for excellent response to the initial management.
Disease persistence or recurrence reduces the chances of long-term remission. Disease recurrence varies between 10% and 15% (5, 15, 16). These variations are related mainly to the risk stratification and the follow-up period. The highest level is identified after 30 years of follow-up. Disease persistence is detected in 5% to 20% of cases (3). As evidenced, locally advanced disease (local infiltration or T3 to T4/N1) and high presTg are the main predictors of persistence and recurrence. Such factors were identified in the other studies and are highly weighted in the ATA risk stratification (4, 16–20).
Indeed, many studies and even recent recommendations of the ATA in the management of DTC opted to identify high-risk groups for disease recurrence and separate them from those with excellent response to the initial management to individualize the follow-up period and reduce its psychological and economic consequences. It is thus necessary to identify independent biological parameters to predict disease evolution. Tuttle et al. (12) demonstrated that in low-risk patients the chance of remission was 86%, whereas this decreased to 57% and 14% in moderate and high risk, respectively. With stimulated Tg integrated in the stratification, sTg <1 µg/L was a good prognostic factor, with long-term remission chances to increasing to 97%, 92%, and 84% in low-, moderate-, and high-risk patients, respectively. Since then, sTg has been considered one of the cornerstones to for evaluating the response to initial management (4).
In our cohort, we confirmed the importance of sTg in predicting persistence and recurrence-free survival. Indeed, sTg is significantly correlated to presTg in our cohort. The latter is revealed as an excellent parameter to predict long-term remission. Furthermore, it is adapted to more advanced tumor stages.
If the excellent response and remission are largely correlated to TNM staging of the tumor, presTg remains uncertain. Indeed, in the literature many retrospective studies have focused on the prognostic value of postoperative Tg (11, 21–24). PresTg is often found to be an independent predictor of persistent or recurrent disease (17, 23, 25, 26). These studies confirmed the NPV associated with low presTg levels. However, the suggested cutoffs varied from 0.27 to 30 µg/L. Based on ROC analyses, presTg values between 20 and 30 µg/L were suggested to achieve the best balance for predicting recurrent or persistent disease (24, 27, 28). Such variable cutoffs could be related to the low sensitivity of Tg measurement technique and on the presence or absence of premeasurement stimulation. Furthermore, the number of included patients was low, ranging from 63 to 450 patients. Webb etal. (11) meta-analyzed 15 studies (3900 patients) and calculated a cutoff of 10 µg/L with a good NPV. Another study suggested a cutoff of 13 µg/L as a predictive of disease recurrence (27). Baudin etal. (29) suggested a positive predictive value of 42% for a cutoff of 5 µg/L and 50% for 10 µg/L. Elsewhere, presTg values >5 µg/L have been associated with higher rates of failed ablation (30). Our results were concordant with the latter studies. Likewise, they identified that recurrence was correlated to advanced tumor stages.
It is noteworthy that no study identified a sensitive cutoff for presTg in locally advanced disease. Moreover, TRI was never evoked. Increased delta between the measurements was associated with a higher risk of recurrence (29). Sciuto etal. (31) identified the response to the remnant ablation with RAI as a highly sensitive predictor of morbidity and mortality in patients with DTC. Although Tg was not detailed in this study, response to RAI is reflected by maximal Tg reduction to obtain undetectable values. In line with this observation, ATA recommendations call for risk restratification according to the response to initial management. Such a parameter could indirectly reflect tumor differentiation and its capacity to incorporate RAI. TRI could be a supplemental tool to predict the response to RAI. Indeed, TRI index is useful in tumor stages T3 to T4/N1, where a significant reduction suggests an excellent response. Tumors at stage T1 or T2 have an excellent recurrence-free survival (>90%), whereas T3 to T4/N1 tumors have a higher risk of recurrence (20% to 40%) (17–20, 32). We determined that persistence or recurrence-free survival was restratified as excellent when TRI was >62.5% in such patients. TRI is thus a good indicator of tumor response to remnant ablation with RAI. Furthermore, it is important to highlight the impact of Tg levels on the T staging and its predictive value in terms of remission. As we demonstrated in Fig. 2, T staging loses its significance in the multivariate model when Tg values are continuous but not categorical. This finding indicates that T staging should be taken in consideration according to Tg levels. In cases of presTg >1 µg/L, advanced T staging (T3 to T4) decreases long-term remission. However, beyond 10 µg/L, T staging loses its importance (Fig. 3E).
This study was performed with one of the largest cohorts, with a continuous update of patients’ follow-up, and with a sufficient mean follow-up time to appreciate long-term remission and persistence or recurrence. Furthermore, it used TRI to characterize the response to initial management. Moreover, these parameters seem valuable in patients without a structurally identifiable disease after initial management and in patients with a specific aggressive histological type.
Nevertheless, the study has its limitations, such as the retrospective nature of the inclusion and the nonrandomization. However, our data are regularly and prospectively registered in our database (Registre Thyroïde Auvergne), and the management of our patients was consistent with national and international recommendations. Furthermore, presTg was measured after THW, whereas sTg was measured after rhTSH injections. Stimulation with the latter is less powerful than THW. Nevertheless, TRI was calculated in the same manner for all patients. Furthermore, patients treated with RAI after rhTSH stimulation were excluded (30 patients during the study period). Elimination of these patients was important because of the difference in the methods of stimulation and their intensity (THW vs rhTSH), timing of presTg measurement (day 5 after 131I administration in case of THW vs day 3 in rhTSH). Furthermore, the populations are usually different; indeed, rhTSH was usually used for older adults with a low risk of disease recurrence, and usually such patients received 30 mCi instead of 100 mCi. Thus, presTg analysis in such a population will be a source of bias. However, it is interesting to study patients with rhTSH stimulation independently, to validate such parameters or identify other cutoffs. Indeed, Melo etal. (22) identified a Tg cutoff of 7.2 µg/L after rhTSH to predict disease-free status with an NPV of 90% in 150 patients. Finally, the TNM classification of 2010 was adopted; however, we took in consideration thyroid capsule invasion and tumor size in our cohort to be compatible with the new TNM system published just after completion of our data collection (2017). Indeed, these parameters did not influence the response to initial treatment.
Conclusion
Despite its good prognosis, DTC recurrence and persistence rates remain high. This study identified presTg, sTg, and TRI as sensitive parameters to predict an excellent response to initial management of DTC in a large cohort and estimate long-term remission and disease-free status, including in specific populations such as those with an aggressive cellular type or those without structurally identifiable disease after initial management. Sensitive cutoffs of such parameters were identified for all patients and for those with locally advanced disease (T3 to T4/N1). Identifying prognostic parameters to predict an excellent response or long-term remission after initial management is essential to individualize the risk of disease persistence or recurrence and follow-up for such patients. Additional studies are needed to confirm TRI as a sensitive index for restratifying cancer-related risk.
Abbreviations:
- ATA
American Thyroid Association
- DTC
differentiated thyroid cancer
- LN
lymph node
- NPV
negative predictive value
- presTg
preablation stimulated thyroglobulin
- RAI
radioactive iodine
- rhTSH
recombinant human TSH
- ROC
receiver operating characteristic
- sTg
recombinant human TSH–stimulated thyroglobulin
- Tg
thyroglobulin
- THW
thyroid hormone withdrawal
- TRI
thyroglobulin reduction index
- WBS
whole body scintiscan
Acknowledgments
We thank Professor Philippe Thieblot and Doctor Catherine Dejax for their efforts to establish this study and their participation in patient management.
Author Contributions: B.B. and A.K. collected data; F.K. did the statistical analyses; G.F., A.K., S.M., M.B.L., and I.T. participated in patient management; F.C., I.T., F.D., M.B.-L., and S.M. designed the study and carefully reviewed the results and the manuscript; and S.M. wrote the manuscript.
Disclosure Summary: The authors have nothing to disclose.



