-
PDF
- Split View
-
Views
-
Cite
Cite
Richard J. Santen, Anju Joham, Lauren Fishbein, Kristen R. Vella, Peter R. Ebeling, Melanie Gibson-Helm, Helena Teede, Career Advancement: Meeting the Challenges Confronting the Next Generation of Endocrinologists and Endocrine Researchers, The Journal of Clinical Endocrinology & Metabolism, Volume 101, Issue 12, 1 December 2016, Pages 4512–4520, https://doi.org/10.1210/jc.2016-3016
Close - Share Icon Share
Challenges and opportunities face the next generation (Next-Gen) of endocrine researchers and clinicians, the lifeblood of the field of endocrinology for the future. A symposium jointly sponsored by The Endocrine Society and the Endocrine Society of Australia was convened to discuss approaches to addressing the present and future Next-Gen needs.
Data collection by literature review, assessment of previously completed questionnaires, commissioning of a new questionnaire, and summarization of symposium discussions were studied.
Next-Gen endocrine researchers face diminishing grant funding in inflation-adjusted terms. The average age of individuals being awarded their first independent investigator funding has increased to age 45 years. For clinicians, a workforce gap exists between endocrinologists needed and those currently trained. Clinicians in practice are increasingly becoming employees of integrated hospital systems, resulting in greater time spent on nonclinical issues. Workforce data and published reviews identify challenges specifically related to early career women in endocrinology.
Recommendations encompassed the areas of grant support for research, mentoring, education, templates for career development, specific programs for Next-Gen members by senior colleagues as outlined in the text, networking, team science, and life/work integration. Endocrine societies focusing on Next-Gen members provide a powerful mechanism to support these critical areas.
A concerted effort to empower, train, and support the next generation of clinical endocrinologists and endocrine researchers is necessary to ensure the viability and vibrancy of our discipline and to optimize our contributions to improving health outcomes. Collaborative engagement of endocrine societies globally will be necessary to support our next generation moving forward.
This manuscript summarizes the presentations and discussion at a joint symposium sponsored by The Endocrine Society (ES) and the Endocrine Society of Australia (ESA) held at the annual meeting of the ESA in Adelaide, Australia. on August 24, 2015. This collaborative effort between the two societies was designed to review pertinent literature and questionnaire data, specifically commission a new questionnaire, discuss the opportunities and challenges facing the next generation (Next-Gen) of clinical endocrinologists and endocrine researchers, and propose potential solutions. Because most issues confronting Next-Gens from developed countries are global in nature, the symposium focused on those generally applicable across countries, using specific examples primarily from the United States and Australia.
General observations
The next generation of clinical endocrinologists and endocrine researchers spanning the basic, translational, and clinical spectrum will serve as the lifeblood of our discipline over the following decades. The challenges and opportunities facing Next-Gens appear to apply internationally as advances in Internet-based communication methods have facilitated global interchange. Key issues confronting the Next-Gens include a rapidly evolving, innovative environment with the adoption of new technologies in both research and patient care that may transform biomedical research and medical practice. Recruitment, retention, career development, and empowerment of the Next-Gen cohort are all essential issues for the future of endocrinology. Strategies are needed for endocrine societies to support their Next-Gen members in conducting research and translating innovative, hormone-related findings from basic, translational, and clinical science to improve the health of individuals with hormone-related disorders.
Opportunities
Major technological advances are enhancing our ability to address new horizons, conquer new areas of research, and improve patient care, all exciting prospects for the Next-Gen cohort. Prismatic examples of emerging research technology include expanded use of stem cells based on a greater understanding of their function, application of genetic findings to enable precision patient care, and the revolutionary new ability to manipulate specific genes with Clustered Regularly Interspaced Short Palindromic Repeats/cysteine-aspartic-protease 9 (CRISPER/Caspase 9) methodology (1–9). Optimistic estimates suggest that newly applied technology and emerging data will allow the cure of type 1 diabetes and certain endocrine-dependent cancers in the next 2 decades. In the clinical translational space, enhanced use of big data, the influence and role of communication technology, the optimization and translation of guidelines to facilitate evidence-based practice, and improved patient self-management are critical for improving efficiency and effectiveness of care.
Challenges
Severe limitations in research funding (10) and increasing difficulty in gaining recognition for professional achievements represent obstacles to career advancement for those involved in research. For physicians in practice, effective transition to nearly exclusive hospital-based practice in the United States, greater demand for clinical efficiency, competing administrative responsibilities, and reduced time available for continuing education provide challenges (11). As endocrinology transitions to a predominantly female specialty (72% of endocrinology fellows in the United States are now female), gender-related challenges at specific stages in career advancement become increasingly important as recently outlined in several manuscripts (12, 13).
Methodology
A variety of specific data sources were used for the preparation of the ES/ESA Next-Gen symposium and were prioritized and distilled for this manuscript by the organizers of the symposium (H.T., P.R.E., R.J.S.) as well as Next-Gen representatives of the two organizations (M.G.-H., A.J., K.V., L.F.). These included the following: 1) a focused literature review; 2) a Next-Gen task force report commissioned by the ES; 3) three questionnaires specifically targeting Next-Gen members (an ES survey sent to all members in 2012 on competing workplace responsibilities; an Early Career ES Survey in 2013 sent to 7200 members aged ≤ 45 y; and a new questionnaire specifically commissioned by the ESA in 2015 for the symposium and sent to members < 45 y of age; 4) an ES workforce analysis (12); 5) Workforce Australia national data; 6) a National Institutes of Health (NIH) model of Next-Gen investigators entering the pool (14); and 7) objective data and interactive discussion from the ES/ESA symposium on August 24, 2015.
Review of existing data: issues facing researchers
Grant-funding age and availability
Government research support available to early career investigators is diminishing in both the United States and Australia, likely reflecting global trends (10, 15–21). Inflation-adjusted funding for research by the NIH in the United States decreased by 23% (Figure 1A) from 2003 until 2013. The percentage of independent-investigator NIH grants funded has gradually decreased from 57.9% in 1963 to 23.3% in 2008 and 14% in 2013 (22). The average age of the first-time independent investigator has increased from age 37 years in 1980 to 44–45 years currently (Figure 1B). In 1981, 25% of NIH RO-1 grants were awarded to those aged 36 years and younger vs 2% in 2014 (Figure 1C). Examination of numerator and denominator data further emphasize the reduction in absolute numbers of grants to those 36 years old or younger, falling from 1854 of 8785 grants awarded in 1980 to 289 of 19 417 in 2014. Similarly in Australia, research funding by the National Health and Medical Research Council (NHMRC) for project grants also has decreased over the last 5 years (Figure 1D), with an overall fall in inflation-adjusted terms and with a rising age of first-time independent investigators. A greater share of funding in both countries is currently being awarded to older established investigators, consequently diminishing the funds available for Next-Gen investigators (Figure 1C).
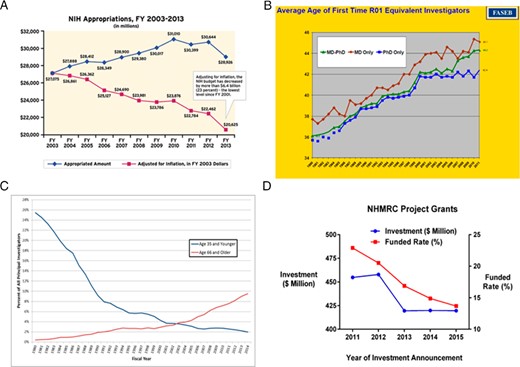
A, Inflation-adjusted NIH appropriations for biomedical research (http://www.clfoundation.org/sites/default/files/content/OVACFY2014CancerResearchFactsheet.pdf). B, Average age of first-time RO-1 equivalent investigators (19). C, Percentage of NIH RO-1 grants obtained by those 36 years old and younger and 66 years old and older (https://nexus.od.nih.gov/all/2012/02/13/age-distribution-of-nih-principal-investigators-and-medical-school-faculty/). Numerator and denominator data from 1980 and 2014 provide further insight into these statistics. Of the 8785 grants awarded in 1980, 1854 were to those age 36 years old and younger and only 52 to those 66 years old and older. Of the 19 417 grants awarded in 2014, 289 were to those 36 years old and younger and 289 1833 to those 66 years old and older. As the figure suggests, the numerators and denominators for the intermediate years between 1980 and 2014 gradually change. Full data are available from the power point data at the web site above. Figure credit: NIH Office of Extramural Research. D, Australian data on research funding for project grants (23).
Workforce
Research funding issues have led to a diminishing pool of young, independently funded investigators, a subject of several scholarly analyses in the United States (10, 16–21). The NIH has developed models to estimate the rate of replenishment necessary to stabilize the age of the pool of first NIH research grantees in the United States and to reduce the average age of individuals awarded their first independent investigator grant (14). The model suggested that increasing the number of early-stage investigator grants in the United States by a third, from 2138 per year to 3100, would be required to substantially lower the average age, and this increase would have to occur gradually over a decade (14). Likewise, the Australian NHMRC has enhanced the focus on early-investigator funding with dedicated processes leading to some increase in success rates of early investigator-led project grants in recent years, but the rising age at first grant funded persists.
Competing responsibilities
Results from both the ES and ESA surveys highlight the plethora of competing responsibilities confronting researchers (Table 1), which include administration, education, clinical practice, and other activities (23, 24). The ESA survey also highlighted that research extends to unpaid time (63%) both after hours (64%) and during leave (43%).
| Activity . | Basic Scientist, % . | Clinical Scientist, % . | Clinical Practice, % . |
|---|---|---|---|
| Administration | 17.7 | 12.4 | 9.4 |
| Clinical practice | 7.6 | 27.7 | 54.4 |
| Education | 17.8 | 14.7 | 15.2 |
| Research | 59.1 | 43.5 | 16.8 |
| Other | 5.1 | 2.8 | 0.5 |
| Activity . | Basic Scientist, % . | Clinical Scientist, % . | Clinical Practice, % . |
|---|---|---|---|
| Administration | 17.7 | 12.4 | 9.4 |
| Clinical practice | 7.6 | 27.7 | 54.4 |
| Education | 17.8 | 14.7 | 15.2 |
| Research | 59.1 | 43.5 | 16.8 |
| Other | 5.1 | 2.8 | 0.5 |
| Activity . | Basic Scientist, % . | Clinical Scientist, % . | Clinical Practice, % . |
|---|---|---|---|
| Administration | 17.7 | 12.4 | 9.4 |
| Clinical practice | 7.6 | 27.7 | 54.4 |
| Education | 17.8 | 14.7 | 15.2 |
| Research | 59.1 | 43.5 | 16.8 |
| Other | 5.1 | 2.8 | 0.5 |
| Activity . | Basic Scientist, % . | Clinical Scientist, % . | Clinical Practice, % . |
|---|---|---|---|
| Administration | 17.7 | 12.4 | 9.4 |
| Clinical practice | 7.6 | 27.7 | 54.4 |
| Education | 17.8 | 14.7 | 15.2 |
| Research | 59.1 | 43.5 | 16.8 |
| Other | 5.1 | 2.8 | 0.5 |
Review of existing data: issues facing clinicians in practice
Workforce issues
An increased clinical practice demand for endocrinologists has resulted from a widening gap between the number of trained endocrinologists and those needed for patient care, both in the United States and Australia (12, 25, 26). A recent US workforce study reported a current gap of 1500 adult endocrinologists, which represents 28% of the current number of board certified endocrinologists, and this study projected the gap to increase to 2700 physicians by 2025 (12). This has resulted in growing demands for clinical care time.
Time management issues
The Endocrine Society survey data (24) show significant competing responsibilities for clinicians that can diminish the time available for training, education, and career advancement opportunities (Table 1). At a systems level, physicians in practice are increasingly becoming employees of integrated hospitals (11). More time is spent on hospital committees in learning and adhering to system-wide regulations and in implementing and monitoring quality control measures, in dealing with insurance and preapproval issues, and in engaging in electronic medical record systems (24). Physicians also are required to see more patients with a trend toward limiting patient contact time in hospital-based practices. Time-limited consultation funding is now standard practice in Australian settings. ESA questionnaire data indicate that endocrinologists worked more hours in their clinical work than they are paid for, with 48% reporting that they often/always provided clinical care after work hours (23). Whereas clinical service is a priority, in aggregate these factors limit career advancement opportunities and reduce time for continuing medical education and research. In addition, a reduction in opportunities for career advancement for Next-Gen clinicians results from the greater cadre of senior physicians due to increasing retirement age (23).
Gender issues
Currently 38% of adult endocrinologists in the United States and 50% in Australia are women (12), and the trainee pool is increasingly composed of women (72% in the United States and 75% in Australia). These data have encouraged a recent examination of gender as an important component in workforce issues (27–31). Australian workforce data indicate a decrease in working hours in women compared with men from the ages of 35 to 45 years, a time period often corresponding to early parenting (23). This is a transient phenomenon because work hours prior to this are comparable and also increase after this life stage in women (31). In the Australian Next-Gen survey, 73% of endocrinologists aged younger than 45 years reported having preschool-aged children, with 76% of women with children working clinically part time (<32 h/wk) compared with 56% of men (23). Of those with children, only 36% of women and 52% of men reported satisfaction with balancing family and career. A recent US workforce analysis (12) indicated that male adult endocrinologists work an average of 42 hours per week and provide 3434 visits per year, whereas their female counterparts work 39 hours per week and provide 2484 visits per year. Notably, peak productivity for men occurs at 41–45 years of age, whereas for women it is reached between ages 46 and 50 years (12). Interestingly, opposite trends are seen among pediatric endocrinologists in which the peak productivity occurs at the same age in men and women. Among pediatric endocrinologists, women are most of the workforce (51%), work more hours in clinical service (31 vs 21 h/wk), and see more patients (2158 vs 1840 visits per year) (12).
Recent analyses report that women physicians in general and women endocrinologists, in particular (13, 31), have been less likely to advance in their careers in both research and clinical practice. Observations suggest that this is due in part to lack of adequate mentorship as well as gender discrimination and bias in career advancement (31). Objective statistics provide a stark reminder of inequality in career advancement for early-career young women, with lower numbers promoted to tenure-track positions out of fellowships, promoted to full professors, or appointed to leadership positions across the board including division chiefs, department chairs, deans, or clinical leadership positions. It is notable that both the ES and ESA have female leadership at the highest levels of the societies, yet these do not always translate to the workplace, presenting not only an opportunity but also an imperative for action.
Needs assessment of the Next-Gen in research and clinical practice
Next-Gen insights
High on the list of perceived needs of Next-Gen endocrinologists (clinical and basic) in the United States (Figure 2) were topic-specific education meetings with focused, in-depth sessions attuned to Next-Gen requirements, assistance with grant and manuscript writing (for those engaged in research), availability of expert advice on the management of difficult cases (for clinicians), effective mentorship, networking opportunities, and support to manage costs of attending national/international meetings. Other priority areas included online learning modules, with topics from highest to lowest priority being biostatistics, evaluation of hormone assays, manuscript writing, grant writing, clinical trial design, and setting up one’s first laboratory. The ESA data were consistent and also noted mentoring and provision of fellowships/scholarships as priority areas. No specific data were collected on gender-specific career advancement strategies, and this gap is now the subject of future ongoing collaborative work.
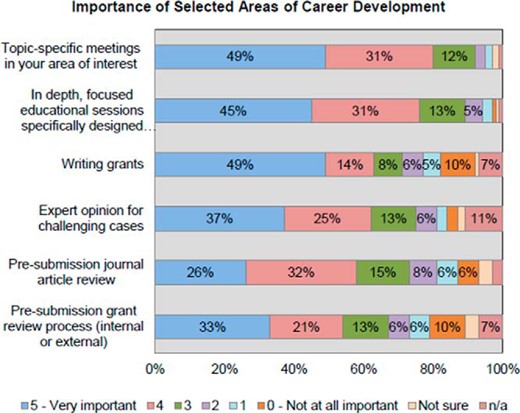
Questionnaire data representing responses of Next-Gen Endocrine Society members (35). n/a, not available.
Key points raised in symposium discussion: role of endocrine societies in addressing issues
Grants and earlier-career funding success
Solutions to the issue of grant funding are most challenging. Most endocrine societies do not have sufficient financial resources to provide comprehensive, ongoing research funding. A generally recognized principle is that young investigators are more likely to be creative, innovative, and energetic than their older peers; less daunted by new ideas and technologies; and often discover dimension-enhancing breakthroughs. This principle informs the imperative need for alternative, more creative, early-career start-up funds. Partnering with external organizations including industry and philanthropy to facilitate competitive seed funding or small project grants and bequests targeted to career advancing research provides one avenue to assist the Next-Gen. The ESA already offers competitive start-up funds through partnerships and bequest funding and seeks to expand this initiative further.
A critical role of endocrine societies is to advocate for a transformation in the approaches to funding early career researchers. The NIH in the United States has been addressing this grant-funding challenge as has the Australian NHMRC, with multiple stakeholders currently involved in consultation (25, 26, 32). Many strategies may emerge and could include a rebalancing process with potential redirection of funds from more senior investigators to highly talented Next-Gen researchers selected on the basis of talent, track record, and significance of innovative ideas and approaches. The specific mechanisms discussed to achieve this rebalancing created controversy among the authors of this treatise and led to deferral to the comprehensive review by the distinguished panel of B. Alberts, M. W. Kirschner, S. Tilghman, and H. Varmus (20). These thought leaders recently addressed this issue and identified the goal of producing a better alignment between the number of PhD entrants and their future opportunities and to alter the ratio of trainees to staff scientists in research groups. Several cogent suggestions included limiting the damaging effects of hypercompetition, addressing the crippling effects of increasing demands on one’s time, planning for the stable funding of science, and increasing the roles of staff scientists. At the ES/ESA symposium, it was noted that at the present time, approximately seven individuals are trained for every trainee who successfully competes for an independent-investigator award. The rebalancing of this ratio might better align funds (33, 34) and ultimately provide more funding for independent early-career investigators.
The Next-Gens have asked for more educational opportunities beyond core clinical and research content. This could be offered by endocrine societies and encompass a broad range of areas. One very useful area would be leadership training to help Next-Gens succeed in career-advancement positions and education regarding the team science environment of today. Notably, leadership and team-building skills are key components of success. Self-advocacy, prioritization, and time management training also may assist the Next-Gens to manage competing demands. Generic grant and manuscript writing workshops are a simple practical step, and recent novel initiatives by the ES training committee to offer education sessions for nondomestic trainees on coming to work in the United States have also proved popular. At present, greater than half of endocrinology fellows are international medical graduates, and the specific issues confronting these trainees require careful consideration and thoughtful solutions. In the future, senior endocrinologists and researchers with expertise in grant writing could provide greater training and support with formal programs and assist in prereviewing submissions. Potential solutions could include engaging study section alumni into a voluntary grant facilitation committee or for societies to facilitate exchange of services during which department leaders could exchange an independent review of Next-Gen grant submissions.
The issue of competing demands for basic and clinical researchers needs to be thoughtfully addressed. Increasing compliance and administrative responsibilities present challenges, which multiply when conducting collaborative multiinstitutional research. National initiatives to streamline governance and compliance are needed, as has occurred in the United Kingdom. Our surveys provide unique insight into the pressures that Next-Gen endocrine researchers experience, with the majority undertaking research out of usual work hours (23). Expectations and time needed to accomplish innovative research outstrip time currently available (or contracted for). This issue has implications for retaining highly skilled Next-Gen researchers and compromises the quality of endocrine research. Needed solutions are greater protected research time, reduced duplication of administrative work, and streamlined compliance requirements.
Clinicians in practice recognize that quality improvement projects, health services research, and clinical leadership are drivers for delivering high standards of health care. However, nonpatient care-related time is increasingly limited, and as yet, an analysis of time constraints has attracted minimal attention. Hospital systems including computer-based compliance programs, service on hospital committees, quality improvement, administrative work, and required certification updates need increasing time. These are important but are rarely compensated by reduction in clinical commitments. Potential solutions here require design of work templates that provide a more flexible structure for total hours that sets feasible limits on competing responsibilities. The concept is not new because residency programs in the United States and faculty programs in Europe have established time-frame limits and in Australia, nonclinical or training time is incorporated into the educational system. However, even in these instances, this time increasingly is eroded with structured commitments. The ES, ESA, and other endocrine societies can advocate for joint initiatives with professional societies and associations to ensure that medical protected time is encompassed in all work agreements, much as they are for other health workforce groups.
Another strategy that the endocrine societies can contribute to, as a means of addressing time constraints, is to devise methods to increase efficiency. This is particularly pertinent with respect to continuing education. Presentations by a working group at the ES emphasized that many young professionals learn best by short, focused presentations in which the material can be accessed at any time on multiple devices and with various audio or audiovisual materials (G.T. McMahon, unpublished presentation). Any 10- to 15-minute downtime can then be used for education. With appropriate safeguards, these techniques could be integrated into the maintenance of certification programs and expanded to support clinical training. The ES Endocrine Cases program is under development and aims to provide expert clinical consultations to young endocrinologists on a global basis. When confronted with a complex case, endocrinologists can submit a brief case report with questions to be answered to The Endocrine Society. Within a week, two highly vetted experts will respond with their opinions and suggestions. In this way, younger members can use the advice of highly experienced, senior members in a time-efficient way.
For clinicians, strategies to increase leadership opportunities are also needed. Although head-of-unit positions are scarce, recognition of the need for innovative strategies to engage, retain, and provide experience in leadership is important. Societies can play a larger part in developing more leadership and mentoring roles for Next-Gen members as well as provide more experiences in education, quality, and research such as trainee editor positions on society journals. The Mayo leadership model with rotating leadership roles has also been highly successful.
Several other Next-Gen career advancement strategies are relevant to both researchers and clinicians including recognition and networking. Early-career endocrinologists and endocrine researchers might be more motivated to academic engagement if there were avenues for timely recognition by their peers. All aspects of career advancement depend on professional recognition including promotion and tenure in academic settings, establishing referral clinical practice, and enhanced employment opportunities.
Several successful strategies used by other organizations could be employed for Next-Gen members to help with early recognition. Widely divergent professional groups have established independent, quasiindependent, or internal organizational structures of Next-Gen members to enhance peer to peer recognition. Examples include Young Active in Research Endocrinology, a European group; the American Federation for Medical Research and the Society of Young Clinical Laboratorians. These focus on Next-Gen needs and empowerment through independent meetings, online blogs and short educational presentations, and networking opportunities, with strategies for wider recognition by senior colleagues. The ES has focused on this by establishing internal committees, such as the Trainee and Career Development Core Committee. Other potential strategies include establishment of regional meetings in which only Next-Gen endocrinologists present, but senior members are present. One example is the ESA annual clinical meeting, which precedes the Annual Scientific Meeting and allows only Next-Gen members to present to highly experienced, nationally and internationally recognized endocrinologists. American Federation for Medical Research meetings in the United States, which generally limit presentations to Next-Gen physicians, also provide a model of success for this type of meeting. Endocrine societies can also develop formal policies to appoint Next-Gen members to committees and to designate that meeting cochairs consist of a pair of senior and Next-Gen members. Formal society programs to identify and nurture future leaders would serve as a means to support career development of Next-Gen members. An example is The Endocrine Society’s Future Leaders Advancing Research in Endocrinology program funded by the NIH in the United States, which provides a number of activities for trainees from underrepresented communities.
Key points raised in symposium discussion: women trainees
A major area of discussion in the symposium, and a focus of a recent manuscript, was the increasing number of women trainees entering the field of endocrinology (12, 13). Career advancement for women in research and clinical practice is an important area for endocrine societies to foster. The incoming ES president noted in his 2016 Women in Endocrinology speech that women are less likely to self-nominate for awards, higher positions, and other opportunities than men. This is an area in which professional societies and groups such as Women in Endocrinology can assist with a focus on the Next-Gen. Literature on academic advancement for women generally highlights the importance of mentoring and role modeling, increasing exposure to research, and addressing conscious and unconscious gender biases in career advancement (27–29, 31). However, more research is needed to inform effective strategies to promote career advancement for women. Development of supportive/adaptive and flexible career paths designed to recruit and retain highly skilled Next-Gen members is generally needed. Increasingly, women in senior positions have successfully fostered cultures for support and are overcoming disadvantages in career advancement. Positive female role models are important, and both men and women in leadership positions need to engage to ensure identified challenges are considered within institutions, societies, and granting bodies so that equal career opportunities are provided.
Gender differences impact workforce planning (12) and also influence career satisfaction issues as seen in the ESA survey. The need to appropriately balance lifestyle, work, and career advancement at vital career stages suggests that proactive strategies to support the Next-Gen regarding these issues are important. USA maternity leave and part-time work flexibility differ from that in Australia, which has generous maternity leave provisions and established acknowledgment of career disruptions. Equivalent data for female and male fellows in the United States are not currently available, highlighting a gap for future research.
Next-Gen task force recommendations
The Endocrine Society commissioned a Next-Gen task force (NGTF) to discuss pertinent issues and to come up with potential solutions (35). The NGTF recommendations align well with the above suggestions and include working with program directors and mentors to identify and develop effective online education programs. Indeed, they noted that educational experiences for undergraduate and graduate students need to be broadened to bring more people into the field. Because professional satisfaction of established endocrinologists is a key requirement for recruitment of new members, the NGTF suggested developing a strategy to communicate the high degree of satisfaction from appropriately selected established members. In recognition of the complexities of work/life integration with clinical and research requirements, the NGTF recommended initiating a comprehensive career development program, with outreach differing with respect to clinical trainees, laboratory science trainees, and translational/clinical research trainees. Programs should stress the synergies in collaboration among laboratory scientists, translational researchers, clinical scientists, and clinical practitioners. The ES could provide mock study sections and grant-writing workshops, develop a comprehensive database on all existing funding sources, and devise methods to make new and existing programs more accessible. Leadership development was also recognized as essential. Finally, comprehensive planning is needed to recruit talented young men and women into endocrinology at the undergraduate, graduate, and training levels. Most often this takes place with person-to-person interactions with successful endocrinologists who are willing to reach out to others. Endocrine societies can also take the lead in facilitating these opportunities.
Conclusions
An analysis of the issues confronting Next-Gen endocrinologists and endocrine researchers has identified many challenges and opportunities. Most agree that a concerted effort to empower, train, and support the next generation of endocrinologists and endocrine researchers is necessary to ensure the viability and vibrancy of our discipline and to optimize our contribution to improving health outcomes. Here we propose a range of strategies that the ES, ESA, and other societies can develop in collaboration including the following: opportunities for increased grant funding, support in grant preparation, approaches to managing competing demands, efficient online education and case support, and the promotion of vital high-quality mentorship and support.
Glossary
The following are glossary terms: 1) clinical endocrinologist, an MD endocrinologist who devotes most time to taking care of patients; 2) endocrine researcher, a PhD or MD who conducts research in the area of endocrinology, basic, translational, or clinical; and 3) translational research, a form of research that resides in the interface between pure basic and clinical research and is focused on ultimate clinical applications.
Acknowledgments
Disclosure Summary: The authors have nothing to disclose.
Abbreviations
- ES
The Endocrine Society
- ESA
Endocrine Society of Australia
- Next-Gen
next generation
- NGTF
Next-Gen task force
- NHMRC
National Health and Medical Research Council.



