-
PDF
- Split View
-
Views
-
Cite
Cite
Yasunori Cho, Shinichiro Shimura, Akira Aki, Hidekazu Furuya, Kimiaki Okada, Toshihiko Ueda, The SYNTAX score is correlated with long-term outcomes of coronary artery bypass grafting for complex coronary artery lesions, Interactive CardioVascular and Thoracic Surgery, Volume 23, Issue 1, July 2016, Pages 125–132, https://doi.org/10.1093/icvts/ivw057
Close - Share Icon Share
Abstract
We analysed retrospectively the long-term outcomes of conventional coronary artery bypass grafting (CABG) as employed routinely for complex coronary lesions by observing patients with low (0–22), intermediate (23–32) and high (≥33) SYNTAX scores. The purpose of this study was to evaluate the correlation between the SYNTAX score and long-term major adverse cardiac and cerebrovascular events (MACCEs) including all-cause death, stroke, myocardial infarction (MI) and repeat revascularization after CABG.
The study enrolled 396 consecutive patients with stable and untreated left main and/or three-vessel disease, who had been referred to our heart team from 2000 through 2009. They all routinely underwent conventional CABG. The three groups (low score; n = 159, intermediate score; n = 150, high score; n = 87) were compared, looking at the primary endpoint of MACCE and its components. We also analysed the effects of diverse variables on long-term MACCEs after the operation.
The cumulative 10-year MACCE rates in patients with low, intermediate and high SYNTAX score were 25.3, 35.8 and 48.1%, respectively. The Kaplan–Meier cumulative event curves showed a significantly higher MACCE rate after CABG in patients with a higher SYNTAX score than in those with a lower score (log-rank P = 0.0012). This was mainly because of a significantly increased rate of repeat revascularization in the higher SYNTAX score group (log-rank P = 0.0032). The cumulative rate of repeat revascularization at 10 years in patients having low, intermediate and high SYNTAX score were, respectively, 4.6, 15.7 and 16.8%. The cumulative rates of the combined outcomes of death/stroke/MI at 10 years did not show statistical differences between the three groups (22.3% with low, 25.0% with intermediate and 38.4% with high score, log-rank P = 0.063). In the multivariable analysis, the SYNTAX score [hazard ratio (HR) 1.03, P = 0.0043] and logistic EuroSCORE II (HR 1.34, P = 0.0012) were found to be significant predictors of long-term MACCEs.
The SYNTAX score is correlated with long-term outcomes, in terms of MACCEs, after conventional CABG for complex coronary lesions and is prognostic of long-term outcomes of CABG for patients with complex lesions.
INTRODUCTION
Coronary artery bypass grafting (CABG) was introduced in 1968, and is still the standard mode of treatment for patients with complex coronary artery lesions [1–8]. Since percutaneous coronary intervention (PCI) was introduced in 1977, interventional cardiologists have steadily widened the application of PCI to patients with complex multiple lesions [3, 4, 9, 10]. It is recognized that PCI offers immediate relief of angina in patients with stable coronary disease although it does not reduce the risk of myocardial infarction (MI) or death [11–13].
The SYNTAX trial is the first large trial to assess the most appropriate revascularization strategy. It assigns patients randomly to either CABG or PCI using drug-eluting stents for the treatment of de novo left main (LM) and/or three-vessel disease (3VD) [6–8]. According to Mohr et al. [8], in the final 5-year results of the SYNTAX trial the rate of major adverse cardiac and cerebrovascular events (MACCEs) was 26.9% in the CABG group and 37.3% in the PCI group (P < 0.0001). The MACCE rate after CABG for complex coronary artery lesions was found to be independent of the SYNTAX score. The conclusion was that CABG should remain the standard of care for patients with complex lesions, although PCI is an acceptable alternative for patients with less complex or LM disease.
Despite that conclusion, we have routinely employed CABG during the last decade for LM and/or 3VD, even in patients with cardiogenic shock or those who would have been recommended PCI at a Class I or II according to the current US and European guidelines [3, 4, 14]. These CABGs were performed by the conventional method with on-pump arrest, using internal mammary arteries (IMAs) to achieve long-term graft patency with the aim of good long-term outcome [15]. In the present study, we retrospectively analysed long-term outcomes with routine use of conventional CABG for previously untreated and stable LM and/or 3VD, looking at patients with low (0–22), intermediate (23–32) and high (≥33) SYNTAX scores. The aim of this study was to evaluate the correlation between the SYNTAX score and long-term MACCEs after conventional CABG for complex coronary lesions.
PATIENTS AND METHODS
Selection of patients
Following approval from our institution's ethics committee/institutional review board, a retrospective review was carried out on 396 consecutive patients with previously untreated and stable LM and/or 3VD who had been referred to our heart team from 2000 to 2009. All patients routinely underwent conventional CABG. Of these, 296 (74.7%) were men having a mean age of 66.9 ± 8.7 years. LM disease was defined as the presence of at least 50% stenosis, with or without stenosis in other vessels. We excluded patients who had previously undergone PCI or CABG, persisting acute MI, concomitant cardiac surgery or intra-aortic balloon pumping support for haemodynamic stability.
Study design
Relevant variables were reviewed retrospectively, including clinical demographics, physical examination findings, electrocardiography, echocardiography and procedural characteristics. All diagnostic angiographies were reviewed and scored by cardiologists, who were unaware of the study group. The SYNTAX score was calculated retrospectively according to the SYNTAX score algorithm [16]. For preoperative risk analysis, the Logistic EuroSCORE II was also calculated using the interactive calculator, launched at the 2011 EACTS meeting in Lisbon.
The present article focused on long-term MACCEs (i.e. all-cause death, stroke, MI or repeat revascularization) after conventional CABG, employed routinely for complex coronary artery lesions among patients having low SYNTAX score (0–22; n = 159), intermediate score (23–32; n = 150) and high score (≥33; n = 87). Univariable and multivariable predictors of long-term MACCEs were also analysed.
Surgical procedures
All patients were treated with the intention of achieving complete revascularization of all coronary vessels at least 1.5 mm in diameter having 50% stenosis or more. CABG was performed during cardiac arrest with cold crystalloid or blood cardioplegia and local cooling. The heart was bypassed using one or two IMAs as an in situ graft and vein grafts. The left IMA graft was anastomosed predominantly to the left anterior descending artery (LAD). Aspirin was prescribed for all patients prior to CABG and was continued after the operation. The extent of early revascularization was assessed post-procedure using an ultrasonic Doppler flowmeter, and complete revascularization for LAD and culprit lesions was confirmed by coronary graft angiography or computed tomography 2 weeks after the operation.
Follow-up and primary endpoint
Follow-up information was obtained during patients' visits. Coronary and graft angiography was mostly performed for asymptomatic patients 1 year after the operation unless problems with graft patency was suspected. Patent graft was defined as a graft without occlusion or significant stenosis (>75%) or string sign. Late graft failure was defined as any graft with occlusion, significant stenosis or string sign in the angiographic evaluation after 1 year, or a graft that required repeat revascularization even though the patient was asymptomatic.
The primary clinical endpoint was a composite of MACCEs, including all-cause death, stroke, MI and repeat revascularization, throughout the follow-up period after the operation [6–8]. A stroke, specifically cerebrovascular events or accidents, was defined as focal neurological deficits of central origin lasting for 72 h, with confirmed permanent brain damage or body impairment. MI was defined via new Q-waves or peak creatine kinase (CK)-MB/total CK >10% or a plasma level of CK-MB >100 U/l. Repeat revascularization was defined as involving a PCI or repeat CABG for graft failure, or acute coronary syndrome with a confirmed lesion within or adjacent to a previously treated graft.
Statistical analysis
Data relating to continuous variables are presented as mean ± standard deviation. Comparisons between the three groups undergoing CABG, involving patients with low-, immediate- and high SYNTAX scores, were performed using the one-way factorial analysis for variance for normally distributed data, as confirmed by the F-test. Category data were expressed as percentages. Proportions were analysed by the χ2 test. The Kaplan–Meier method was used to estimate cumulative event rates of MACCE and its composites for the three groups, and differences between these groups were assessed using the log-rank test. A Cox proportional-hazards model was used to analyse the effects of variables on long-term MACCEs. The stepwise regression was used for generating the multivariable model. Variables, including preoperative and procedural characteristics, that were significantly associated with the events, were then included in a multivariable analysis. A P-value smaller than 0.05 was taken as statistically significant. All statistical analyses were performed using SPSS 17.0.
RESULTS
Overall long-term outcomes
Overall, 396 consecutive patients with LM and/or 3VD were treated routinely by conventional CABG between January 2000 and December 2009. One hospital death (0.3%) occurred due to rupture of an abdominal aortic aneurysm. During follow-up (mean: 85.4 ± 38.6 months) there were 52 late deaths among the 395 survivors. These were due to neoplasms in 20 patients, heart failure in 10, renal failure in 8, pneumonia in 6, stroke in 4, arrhythmia in 3 and accident in 1. The overall rate of 10-year mortality was 20.0% and the overall 10-year MACCE rate was 34.3%.
Baseline characteristics and operative results
Patients in the three groups were well balanced with regard to most of the preoperative demographic and clinical characteristics (Table 1). No statistically significant difference was found in the logistic EuroSCORE II between the three groups (1.3 ± 0.9% with low, 1.4 ± 1.0% with intermediate and 1.5 ± 1.0% with high score, P = 0.37). The ejection fraction was significantly higher in patients with a lower SYNTAX score than in those with a higher score (60.4 ± 10.6% with low, 58.1 ± 11.3% with intermediate and 56.6 ± 11.3% with high score, P = 0.025). Patients with a lower SYNTAX score had significantly fewer multiple-vessel lesions (75.1% with low, 93.0% with intermediate and 98.8% with high score, P < 0.0001).
Preoperative clinical characteristics in patients who underwent routine CABG for complex coronary lesions grouped by baseline SYNTAX score tercile
| Variable . | Low score (n = 159) . | Intermediate score (n = 150) . | High score (n = 87) . | P-value . |
|---|---|---|---|---|
| Age (year) | 66.6 ± 10.2 | 67.0 ± 7.7 | 67.4 ± 7.4 | 0.79 |
| Age >80 years | 9 (5.6%) | 3 (2.0%) | 1 (1.2%) | 0.097 |
| Men | 116 (72.0%) | 112 (75.2%) | 68 (79.1%) | 0.48 |
| DM (HbA1c >6.2) | 76 (47.2%) | 73 (49.0%) | 44 (51.2%) | 0.84 |
| BMI | 24.0 ± 3.7 | 23.8 ± 3.0 | 23.0 ± 2.8 | 0.085 |
| Obesity | 39 (24.2%) | 24 (16.1%) | 12 (14.0%) | 0.078 |
| Current smoking | 29 (18.0%) | 28 (18.8%) | 18 (20.9%) | 0.86 |
| Hyperlipidaemia | 77 (47.8%) | 71 (47.7%) | 30 (34.9%) | 0.11 |
| EF | 60.4 ± 10.6 | 58.1 ± 11.3 | 56.6 ± 11.3 | 0.025 |
| Previous MI | 20 (12.4%) | 14 (9.4%) | 9 (10.5%) | 0.69 |
| Unstable angina | 38 (23.6%) | 21 (14.1%) | 21 (24.4%) | 0.062 |
| Coronary lesion (s) | <0.0001 | |||
| Isolated LM | 19 (11.8%) | 2 (1.3%) | 0 | |
| LM + 1 vessel | 21 (13.0%) | 7 (4.7%) | 1 (1.2%) | |
| LM + 2 vessels | 21 (13.0%) | 9 (6.0%) | 10 (11.6%) | |
| LM + 3 vessels | 18 (11.2%) | 20 (13.4%) | 50 (58.1%) | |
| 3 vessels | 82 (50.9%) | 111 (74.5%) | 25 (29.1%) | |
| SYNTAX score | 16.8 ± 4.0 | 26.9 ± 2.9 | 37.5 ± 6.5 | <0.0001 |
| Logistic EuroSCORE II | 1.3 ± 0.9% | 1.4 ± 1.0% | 1.5 ± 1.0% | 0.37 |
| Variable . | Low score (n = 159) . | Intermediate score (n = 150) . | High score (n = 87) . | P-value . |
|---|---|---|---|---|
| Age (year) | 66.6 ± 10.2 | 67.0 ± 7.7 | 67.4 ± 7.4 | 0.79 |
| Age >80 years | 9 (5.6%) | 3 (2.0%) | 1 (1.2%) | 0.097 |
| Men | 116 (72.0%) | 112 (75.2%) | 68 (79.1%) | 0.48 |
| DM (HbA1c >6.2) | 76 (47.2%) | 73 (49.0%) | 44 (51.2%) | 0.84 |
| BMI | 24.0 ± 3.7 | 23.8 ± 3.0 | 23.0 ± 2.8 | 0.085 |
| Obesity | 39 (24.2%) | 24 (16.1%) | 12 (14.0%) | 0.078 |
| Current smoking | 29 (18.0%) | 28 (18.8%) | 18 (20.9%) | 0.86 |
| Hyperlipidaemia | 77 (47.8%) | 71 (47.7%) | 30 (34.9%) | 0.11 |
| EF | 60.4 ± 10.6 | 58.1 ± 11.3 | 56.6 ± 11.3 | 0.025 |
| Previous MI | 20 (12.4%) | 14 (9.4%) | 9 (10.5%) | 0.69 |
| Unstable angina | 38 (23.6%) | 21 (14.1%) | 21 (24.4%) | 0.062 |
| Coronary lesion (s) | <0.0001 | |||
| Isolated LM | 19 (11.8%) | 2 (1.3%) | 0 | |
| LM + 1 vessel | 21 (13.0%) | 7 (4.7%) | 1 (1.2%) | |
| LM + 2 vessels | 21 (13.0%) | 9 (6.0%) | 10 (11.6%) | |
| LM + 3 vessels | 18 (11.2%) | 20 (13.4%) | 50 (58.1%) | |
| 3 vessels | 82 (50.9%) | 111 (74.5%) | 25 (29.1%) | |
| SYNTAX score | 16.8 ± 4.0 | 26.9 ± 2.9 | 37.5 ± 6.5 | <0.0001 |
| Logistic EuroSCORE II | 1.3 ± 0.9% | 1.4 ± 1.0% | 1.5 ± 1.0% | 0.37 |
BMI: body metabolic index; DM: diabetes mellitus; EF: ejection fraction; Hb: haemoglobin; LM: left main disease; MI: myocardial infarction; CABG: coronary artery bypass grafting.
Preoperative clinical characteristics in patients who underwent routine CABG for complex coronary lesions grouped by baseline SYNTAX score tercile
| Variable . | Low score (n = 159) . | Intermediate score (n = 150) . | High score (n = 87) . | P-value . |
|---|---|---|---|---|
| Age (year) | 66.6 ± 10.2 | 67.0 ± 7.7 | 67.4 ± 7.4 | 0.79 |
| Age >80 years | 9 (5.6%) | 3 (2.0%) | 1 (1.2%) | 0.097 |
| Men | 116 (72.0%) | 112 (75.2%) | 68 (79.1%) | 0.48 |
| DM (HbA1c >6.2) | 76 (47.2%) | 73 (49.0%) | 44 (51.2%) | 0.84 |
| BMI | 24.0 ± 3.7 | 23.8 ± 3.0 | 23.0 ± 2.8 | 0.085 |
| Obesity | 39 (24.2%) | 24 (16.1%) | 12 (14.0%) | 0.078 |
| Current smoking | 29 (18.0%) | 28 (18.8%) | 18 (20.9%) | 0.86 |
| Hyperlipidaemia | 77 (47.8%) | 71 (47.7%) | 30 (34.9%) | 0.11 |
| EF | 60.4 ± 10.6 | 58.1 ± 11.3 | 56.6 ± 11.3 | 0.025 |
| Previous MI | 20 (12.4%) | 14 (9.4%) | 9 (10.5%) | 0.69 |
| Unstable angina | 38 (23.6%) | 21 (14.1%) | 21 (24.4%) | 0.062 |
| Coronary lesion (s) | <0.0001 | |||
| Isolated LM | 19 (11.8%) | 2 (1.3%) | 0 | |
| LM + 1 vessel | 21 (13.0%) | 7 (4.7%) | 1 (1.2%) | |
| LM + 2 vessels | 21 (13.0%) | 9 (6.0%) | 10 (11.6%) | |
| LM + 3 vessels | 18 (11.2%) | 20 (13.4%) | 50 (58.1%) | |
| 3 vessels | 82 (50.9%) | 111 (74.5%) | 25 (29.1%) | |
| SYNTAX score | 16.8 ± 4.0 | 26.9 ± 2.9 | 37.5 ± 6.5 | <0.0001 |
| Logistic EuroSCORE II | 1.3 ± 0.9% | 1.4 ± 1.0% | 1.5 ± 1.0% | 0.37 |
| Variable . | Low score (n = 159) . | Intermediate score (n = 150) . | High score (n = 87) . | P-value . |
|---|---|---|---|---|
| Age (year) | 66.6 ± 10.2 | 67.0 ± 7.7 | 67.4 ± 7.4 | 0.79 |
| Age >80 years | 9 (5.6%) | 3 (2.0%) | 1 (1.2%) | 0.097 |
| Men | 116 (72.0%) | 112 (75.2%) | 68 (79.1%) | 0.48 |
| DM (HbA1c >6.2) | 76 (47.2%) | 73 (49.0%) | 44 (51.2%) | 0.84 |
| BMI | 24.0 ± 3.7 | 23.8 ± 3.0 | 23.0 ± 2.8 | 0.085 |
| Obesity | 39 (24.2%) | 24 (16.1%) | 12 (14.0%) | 0.078 |
| Current smoking | 29 (18.0%) | 28 (18.8%) | 18 (20.9%) | 0.86 |
| Hyperlipidaemia | 77 (47.8%) | 71 (47.7%) | 30 (34.9%) | 0.11 |
| EF | 60.4 ± 10.6 | 58.1 ± 11.3 | 56.6 ± 11.3 | 0.025 |
| Previous MI | 20 (12.4%) | 14 (9.4%) | 9 (10.5%) | 0.69 |
| Unstable angina | 38 (23.6%) | 21 (14.1%) | 21 (24.4%) | 0.062 |
| Coronary lesion (s) | <0.0001 | |||
| Isolated LM | 19 (11.8%) | 2 (1.3%) | 0 | |
| LM + 1 vessel | 21 (13.0%) | 7 (4.7%) | 1 (1.2%) | |
| LM + 2 vessels | 21 (13.0%) | 9 (6.0%) | 10 (11.6%) | |
| LM + 3 vessels | 18 (11.2%) | 20 (13.4%) | 50 (58.1%) | |
| 3 vessels | 82 (50.9%) | 111 (74.5%) | 25 (29.1%) | |
| SYNTAX score | 16.8 ± 4.0 | 26.9 ± 2.9 | 37.5 ± 6.5 | <0.0001 |
| Logistic EuroSCORE II | 1.3 ± 0.9% | 1.4 ± 1.0% | 1.5 ± 1.0% | 0.37 |
BMI: body metabolic index; DM: diabetes mellitus; EF: ejection fraction; Hb: haemoglobin; LM: left main disease; MI: myocardial infarction; CABG: coronary artery bypass grafting.
Upon looking at the procedural characteristics, the mean number of distal anastomoses was found to be significantly greater in patients with a higher SYNTAX score than in those with a lower score (3.0 ± 0.8% with low, 3.5 ± 0.7% with intermediate and 3.5 ± 0.8% with high score, P < 0.0001) (Table 2). The aortic clamp time (65.1 ± 19.5 min with low, 71.0 ± 17.1 min with intermediate and 75.0 ± 21.6 min with high score, P = 0.0003) and pump time (125.1 ± 32.2 min with low, 136.9 ± 29.5 min with intermediate and 144.0 ± 31.3 min with high score, P < 0.0001) were also significantly longer in a higher score group. More of the patients with a lower SYNTAX score achieved complete revascularization than those with a higher score and this observation has statistical significance (98.1% in low, 99.3% in intermediate and 93.0% in high score, P = 0.0096).
Procedural characteristics and early outcomes in patients who underwent routine CABG for complex coronary disease grouped by baseline SYNTAX score tercile
| Variable . | Low score (n = 159) . | Intermediate score (n = 150) . | High score (n = 87) . | P-value . |
|---|---|---|---|---|
| SIMA/BIMA use | 118 (73.3%)/34 (21.1%) | 118 (79.2%)/28 (18.8%) | 62 (72.1%)/22 (25.6%) | 0.77 |
| No. of distal anastomoses | 3.0 ± 0.8 | 3.5 ± 0.7 | 3.5 ± 0.8 | <0.0001 |
| Aortic clamp time (min) | 65.1 ± 19.5 | 71.0 ± 17.1 | 75.0 ± 21.6 | 0.0003 |
| Pump time (min) | 125.1 ± 32.2 | 136.9 ± 29.5 | 144.0 ± 31.3 | <0.0001 |
| Complete revascularization | 158 (98.1%) | 148 (99.3%) | 80 (93.0%) | 0.0096 |
| Operative death | 0 | 0 | 1 (1.2%) | 0.16 |
| Perioperative stroke | 0 | 2 (1.3%) | 0 | 0.19 |
| Perioperative MI | 3 (1.9%) | 1 (0.7%) | 0 | 0.33 |
| ICU stay (median) | 3 days | 3 days | 3 days | 0.83 |
| Hospital stay (median) | 17 days | 17 days | 18 days | 0.83 |
| Late graft failure | 45 (28.0%) | 40 (26.9%) | 25 (29.1%) | 0.67 |
| Variable . | Low score (n = 159) . | Intermediate score (n = 150) . | High score (n = 87) . | P-value . |
|---|---|---|---|---|
| SIMA/BIMA use | 118 (73.3%)/34 (21.1%) | 118 (79.2%)/28 (18.8%) | 62 (72.1%)/22 (25.6%) | 0.77 |
| No. of distal anastomoses | 3.0 ± 0.8 | 3.5 ± 0.7 | 3.5 ± 0.8 | <0.0001 |
| Aortic clamp time (min) | 65.1 ± 19.5 | 71.0 ± 17.1 | 75.0 ± 21.6 | 0.0003 |
| Pump time (min) | 125.1 ± 32.2 | 136.9 ± 29.5 | 144.0 ± 31.3 | <0.0001 |
| Complete revascularization | 158 (98.1%) | 148 (99.3%) | 80 (93.0%) | 0.0096 |
| Operative death | 0 | 0 | 1 (1.2%) | 0.16 |
| Perioperative stroke | 0 | 2 (1.3%) | 0 | 0.19 |
| Perioperative MI | 3 (1.9%) | 1 (0.7%) | 0 | 0.33 |
| ICU stay (median) | 3 days | 3 days | 3 days | 0.83 |
| Hospital stay (median) | 17 days | 17 days | 18 days | 0.83 |
| Late graft failure | 45 (28.0%) | 40 (26.9%) | 25 (29.1%) | 0.67 |
BIMAs: bilateral internal mammary arteries; ICU: intensive care unit; MI: myocardial infarction; SIMA: single internal mammary artery; CABG: coronary artery bypass grafting.
Procedural characteristics and early outcomes in patients who underwent routine CABG for complex coronary disease grouped by baseline SYNTAX score tercile
| Variable . | Low score (n = 159) . | Intermediate score (n = 150) . | High score (n = 87) . | P-value . |
|---|---|---|---|---|
| SIMA/BIMA use | 118 (73.3%)/34 (21.1%) | 118 (79.2%)/28 (18.8%) | 62 (72.1%)/22 (25.6%) | 0.77 |
| No. of distal anastomoses | 3.0 ± 0.8 | 3.5 ± 0.7 | 3.5 ± 0.8 | <0.0001 |
| Aortic clamp time (min) | 65.1 ± 19.5 | 71.0 ± 17.1 | 75.0 ± 21.6 | 0.0003 |
| Pump time (min) | 125.1 ± 32.2 | 136.9 ± 29.5 | 144.0 ± 31.3 | <0.0001 |
| Complete revascularization | 158 (98.1%) | 148 (99.3%) | 80 (93.0%) | 0.0096 |
| Operative death | 0 | 0 | 1 (1.2%) | 0.16 |
| Perioperative stroke | 0 | 2 (1.3%) | 0 | 0.19 |
| Perioperative MI | 3 (1.9%) | 1 (0.7%) | 0 | 0.33 |
| ICU stay (median) | 3 days | 3 days | 3 days | 0.83 |
| Hospital stay (median) | 17 days | 17 days | 18 days | 0.83 |
| Late graft failure | 45 (28.0%) | 40 (26.9%) | 25 (29.1%) | 0.67 |
| Variable . | Low score (n = 159) . | Intermediate score (n = 150) . | High score (n = 87) . | P-value . |
|---|---|---|---|---|
| SIMA/BIMA use | 118 (73.3%)/34 (21.1%) | 118 (79.2%)/28 (18.8%) | 62 (72.1%)/22 (25.6%) | 0.77 |
| No. of distal anastomoses | 3.0 ± 0.8 | 3.5 ± 0.7 | 3.5 ± 0.8 | <0.0001 |
| Aortic clamp time (min) | 65.1 ± 19.5 | 71.0 ± 17.1 | 75.0 ± 21.6 | 0.0003 |
| Pump time (min) | 125.1 ± 32.2 | 136.9 ± 29.5 | 144.0 ± 31.3 | <0.0001 |
| Complete revascularization | 158 (98.1%) | 148 (99.3%) | 80 (93.0%) | 0.0096 |
| Operative death | 0 | 0 | 1 (1.2%) | 0.16 |
| Perioperative stroke | 0 | 2 (1.3%) | 0 | 0.19 |
| Perioperative MI | 3 (1.9%) | 1 (0.7%) | 0 | 0.33 |
| ICU stay (median) | 3 days | 3 days | 3 days | 0.83 |
| Hospital stay (median) | 17 days | 17 days | 18 days | 0.83 |
| Late graft failure | 45 (28.0%) | 40 (26.9%) | 25 (29.1%) | 0.67 |
BIMAs: bilateral internal mammary arteries; ICU: intensive care unit; MI: myocardial infarction; SIMA: single internal mammary artery; CABG: coronary artery bypass grafting.
In the early outcomes, no significant differences between the three groups were observed in mortality (0% with low, 0% with intermediate and 1.2% with high score, P = 0.16), or morbidity such as perioperative stroke (0% with low, 1.3% with intermediate and 0% with high score, P = 0.19) and MI (1.9% with low, 0.7% with intermediate and 0% with high score, P = 0.33).
Long-term outcomes by baseline SYNTAX score tercile
In the Kaplan–Meier cumulative event curves, the rate of all-cause mortality at 10 years in the patients with low SYNTAX score, intermediate score and high score were, respectively, 12.8, 18.8 and 28.7% (Fig. 1A). It was significantly better in the lower SYNTAX score group than in the higher score group (log-rank P = 0.049). There was no significant difference between the three groups for stroke at 10 years (10.7% with low, 6.9% with intermediate and 7.7% with high score, log-rank P = 0.89; Fig. 1B) or MI (2.7% with low, 3.7% with intermediate and 13.7% with high score, log-rank P = 0.17; Fig. 1C). The Kaplan–Meier cumulative event curves for combined outcome at 10 years did not differ significantly among the three groups according to the SYNTAX score (22.3% with low, 25.0% with intermediate and 38.4% with high score, log-rank P = 0.063; Fig. 2).
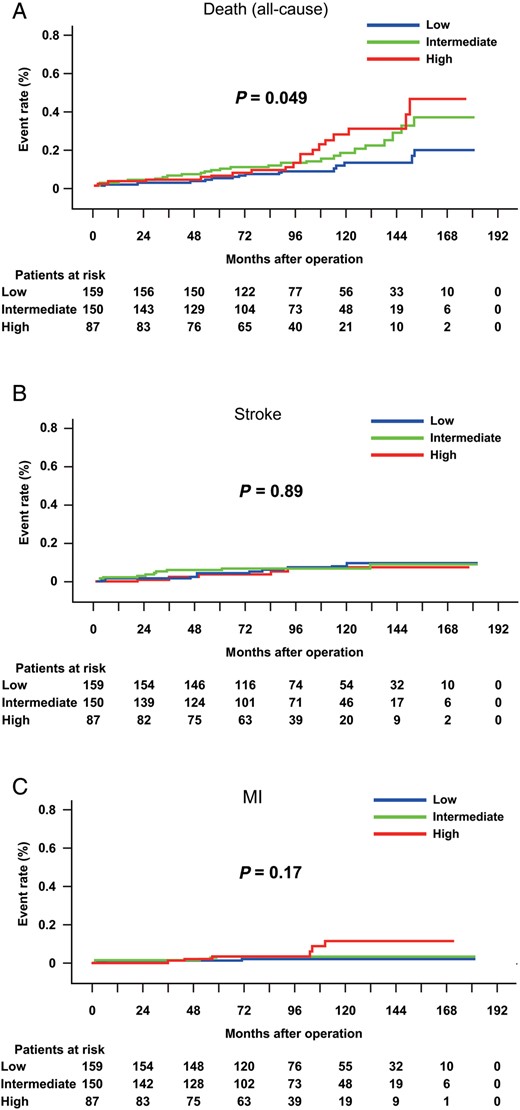
Kaplan–Meier cumulative event curves for all-cause death, stroke and MI in patients with low SYNTAX score (0–22) (n = 159), patients with intermediate score (23–32) (n = 150) and those with high score (≥33) (n = 87). The rate of all-cause death at 10 years was better in the lower SYNTAX score group (12.8% with low, 18.8% with intermediate and 28.7% with high score, log-rank P = 0.049) (A). The three groups had similar rates of stroke (10.7% with low, 6.9% with intermediate and 7.7% with high score at 10 years, log-rank P = 0.89) (B) and MI (2.7% with low, 3.7% with intermediate and 13.7% with high score at 10 years, log-rank P = 0.17) (C). MI: myocardial infarction.
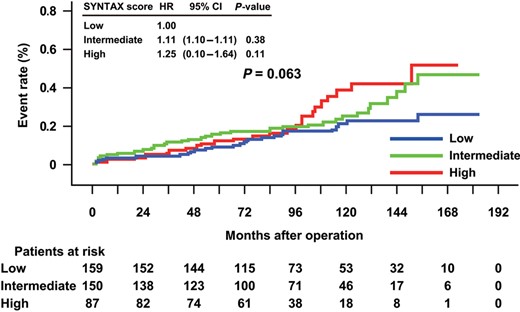
Kaplan–Meier cumulative event curves for combined outcomes of death/stroke/MI in patients with low SYNTAX score (0–22) (n = 159), with intermediate score (23–32) (n = 150) and with high score (≥33) (n = 87). The rate of combined outcome at 10 years did not differ significantly between the three groups according to the baseline SYNTAX score (22.3% with low, 25.0% with intermediate and 38.4% with high score, log-rank P = 0.063). MI: myocardial infarction; HR: hazard ratio; CI: confidence interval.
A total of 339 (85.6%) patients underwent angiographic evaluation mostly performed beyond 1 year after CABG. The occlusion rate as confirmed by angiography in the LAD grafts using the IMA was 2.4%, and 15.0% in other grafts. The rate of late graft failure did not show statistical difference between the three groups (28.0% with low, 26.9% with intermediate and 29.1% with high score, P = 0.67) (Table 2).
Six patients with an occluded IMA–LAD graft, who were found to have ischaemia in the territory of the graft, underwent repeat revascularization with PCI, without mortality or morbidity. All patients who required repeat revascularization for residual ischaemia underwent PCI; the majority received PCI not more than 2 years after the CABG. The Kaplan–Meier cumulative event curves showed significantly increased rate of repeat revascularization in a higher SYNTAX score group than in a lower score group (log-rank P = 0.0032) (Fig. 3). The rate of repeat revascularization at 10 years in patients with a low SYNTAX score, intermediate score and high sore were, respectively, 4.6, 15.7 and 16.8%. Patients with a high SYNTAX score had significantly increased chance of repeat revascularization than patients with a low SYNTAX score [hazard ratio (HR) 3.70, P = 0.0052].
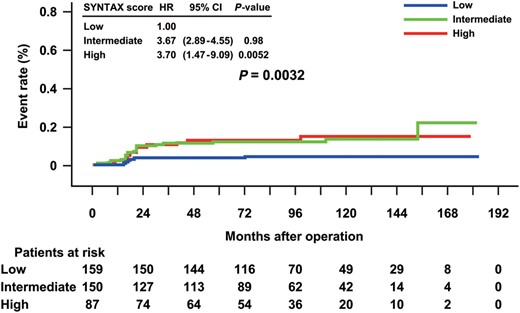
Kaplan–Meier cumulative event curves for repeat revascularization after CABG for the 3 patient groups: low SYNTAX score (0–22) (n = 159), intermediate score (23–32) (n = 150) and high score (≥33) (n = 87). The repeat revascularization rate at 10 years was increased in patients with a higher SYNTAX score than in those with a lower SYNTAX score (4.6% with low, 15.7% with intermediate and 16.8% with high score, log-rank P = 0.0032). Patients with a high SYNTAX score had significantly increased chance of repeat revascularization than patients with a low SYNTAX score (HR 3.70, P = 0.0052). CI: confidence interval; HR: hazard ratio; CABG: coronary artery bypass grafting.
In the present study, the Kaplan–Meier cumulative event curves for MACCEs showed a significantly higher MACCE rate after conventional CABG in patients with a higher SYNTAX score than in those with a lower score (log-rank P = 0.0012) (Fig. 4). The cumulative 10-year MACCE rates in patients with a low SYNTAX score, intermediate score and high score were, respectively, 25.3, 35.8 and 48.1%. Patients with a high SYNTAX score experienced significantly more MACCEs than patients with a low SYNTAX score (HR 2.17, P = 0.0016).
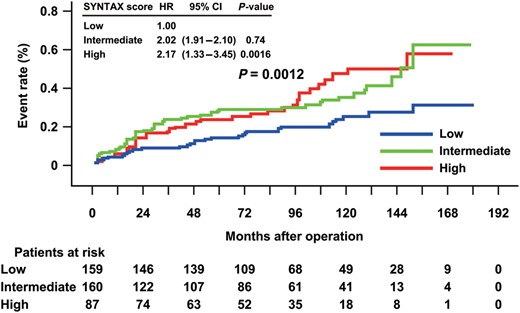
Kaplan–Meier cumulative event curves for MACCEs after CABG for the 3 patient groups: low SYNTAX score (0–22) (n = 159), intermediate score (23–32) (n = 150) and high score (≥33) (n = 87). The 10-year MACCE rates were higher in patients with a higher SYNTAX score than in those with lower SYNTAX score (25.3% with low, 35.8% with intermediate and 48.1% with high score, log-rank P = 0.0012). Patients with high SYNTAX score experienced significantly more MACCEs than patients with lower SYNTAX score (HR 2.17, P = 0.0016). CI: confidence interval; HR: hazard ratio; MACCEs: major adverse cardiac and cardiovascular events; CABG: coronary artery bypass grafting.
Table 3 shows the number of clinical events and the cumulative rate at 5, 10 years and overall. During the follow-up, MACCEs occurred in 31 (33.5%) patients with a low SYNTAX score, in 49 (63.1%) patients with an intermediate score and in 32 (52.0%) patients with a high score. Overall, patients with a lower SYNTAX score had a significantly lower MACCE rate after CABG (log-rank P = 0.0012) than patients with a higher SYNTAX score. This was due mainly to significantly less repeat revascularization being needed (log-rank P = 0.0032).
Number of clinical events and cumulative rate for each endpoint and overall in patients grouped by baseline SYNTAX score tercile
| Variable . | Low score . | Intermediate score . | High score . | Log-rank . |
|---|---|---|---|---|
| 5 years/10 years overall . | 5 years/10 years overall . | 5 years/10 years overall . | P-value . | |
| Death | 5 (3.3%)/12 (12.8%) 13 (17.3%) | 14 (10.1%)/20 (18.8%) 23 (37.5%) | 5 (6.2%)/15 (28.7%) 17 (49.3%) | 0.049 |
| Stroke | 6 (4.1%)/8 (10.7%) 9 (13.8%) | 8 (5.5%)/8 (6.9%) 9 (11.1%) | 4 (5.0%)/5 (7.7%) 6 (10.2%) | 0.89 |
| Myocardial infarction | 5 (1.8%)/6 (2.7%) 6 (2.7%) | 4 (3.1%)/4 (3.7%) 4 (3.7%) | 2 (4.6%)/5 (13.7%) 5 (13.7%) | 0.17 |
| Combined outcomes | 14 (9.1%)/23 (22.3%) 24 (25.7%) | 23 (16.1%)/29 (25.0%) 33 (42.3%) | 9 (10.9%)/20 (38.4%) 21 (46.7%) | 0.063 |
| Repeat revascularization | 5 (4.6%)/5 (4.6%) 5 (4.6%) | 19 (13.5%)/20 (15.7%) 21 (21.7%) | 12 (14.6%)/13 (16.8%) 13 (16.8%) | 0.0032 |
| MACCEs | 20 (13.0%)/29 (25.3%) 31 (33.5%) | 41 (28.3%)/45 (35.8%) 49 (63.1%) | 20 (23.9%)/31 (48.1%) 32 (52.0%) | 0.0012 |
| Variable . | Low score . | Intermediate score . | High score . | Log-rank . |
|---|---|---|---|---|
| 5 years/10 years overall . | 5 years/10 years overall . | 5 years/10 years overall . | P-value . | |
| Death | 5 (3.3%)/12 (12.8%) 13 (17.3%) | 14 (10.1%)/20 (18.8%) 23 (37.5%) | 5 (6.2%)/15 (28.7%) 17 (49.3%) | 0.049 |
| Stroke | 6 (4.1%)/8 (10.7%) 9 (13.8%) | 8 (5.5%)/8 (6.9%) 9 (11.1%) | 4 (5.0%)/5 (7.7%) 6 (10.2%) | 0.89 |
| Myocardial infarction | 5 (1.8%)/6 (2.7%) 6 (2.7%) | 4 (3.1%)/4 (3.7%) 4 (3.7%) | 2 (4.6%)/5 (13.7%) 5 (13.7%) | 0.17 |
| Combined outcomes | 14 (9.1%)/23 (22.3%) 24 (25.7%) | 23 (16.1%)/29 (25.0%) 33 (42.3%) | 9 (10.9%)/20 (38.4%) 21 (46.7%) | 0.063 |
| Repeat revascularization | 5 (4.6%)/5 (4.6%) 5 (4.6%) | 19 (13.5%)/20 (15.7%) 21 (21.7%) | 12 (14.6%)/13 (16.8%) 13 (16.8%) | 0.0032 |
| MACCEs | 20 (13.0%)/29 (25.3%) 31 (33.5%) | 41 (28.3%)/45 (35.8%) 49 (63.1%) | 20 (23.9%)/31 (48.1%) 32 (52.0%) | 0.0012 |
MACCEs: major adverse cardiac and cerebrovascular events.
Number of clinical events and cumulative rate for each endpoint and overall in patients grouped by baseline SYNTAX score tercile
| Variable . | Low score . | Intermediate score . | High score . | Log-rank . |
|---|---|---|---|---|
| 5 years/10 years overall . | 5 years/10 years overall . | 5 years/10 years overall . | P-value . | |
| Death | 5 (3.3%)/12 (12.8%) 13 (17.3%) | 14 (10.1%)/20 (18.8%) 23 (37.5%) | 5 (6.2%)/15 (28.7%) 17 (49.3%) | 0.049 |
| Stroke | 6 (4.1%)/8 (10.7%) 9 (13.8%) | 8 (5.5%)/8 (6.9%) 9 (11.1%) | 4 (5.0%)/5 (7.7%) 6 (10.2%) | 0.89 |
| Myocardial infarction | 5 (1.8%)/6 (2.7%) 6 (2.7%) | 4 (3.1%)/4 (3.7%) 4 (3.7%) | 2 (4.6%)/5 (13.7%) 5 (13.7%) | 0.17 |
| Combined outcomes | 14 (9.1%)/23 (22.3%) 24 (25.7%) | 23 (16.1%)/29 (25.0%) 33 (42.3%) | 9 (10.9%)/20 (38.4%) 21 (46.7%) | 0.063 |
| Repeat revascularization | 5 (4.6%)/5 (4.6%) 5 (4.6%) | 19 (13.5%)/20 (15.7%) 21 (21.7%) | 12 (14.6%)/13 (16.8%) 13 (16.8%) | 0.0032 |
| MACCEs | 20 (13.0%)/29 (25.3%) 31 (33.5%) | 41 (28.3%)/45 (35.8%) 49 (63.1%) | 20 (23.9%)/31 (48.1%) 32 (52.0%) | 0.0012 |
| Variable . | Low score . | Intermediate score . | High score . | Log-rank . |
|---|---|---|---|---|
| 5 years/10 years overall . | 5 years/10 years overall . | 5 years/10 years overall . | P-value . | |
| Death | 5 (3.3%)/12 (12.8%) 13 (17.3%) | 14 (10.1%)/20 (18.8%) 23 (37.5%) | 5 (6.2%)/15 (28.7%) 17 (49.3%) | 0.049 |
| Stroke | 6 (4.1%)/8 (10.7%) 9 (13.8%) | 8 (5.5%)/8 (6.9%) 9 (11.1%) | 4 (5.0%)/5 (7.7%) 6 (10.2%) | 0.89 |
| Myocardial infarction | 5 (1.8%)/6 (2.7%) 6 (2.7%) | 4 (3.1%)/4 (3.7%) 4 (3.7%) | 2 (4.6%)/5 (13.7%) 5 (13.7%) | 0.17 |
| Combined outcomes | 14 (9.1%)/23 (22.3%) 24 (25.7%) | 23 (16.1%)/29 (25.0%) 33 (42.3%) | 9 (10.9%)/20 (38.4%) 21 (46.7%) | 0.063 |
| Repeat revascularization | 5 (4.6%)/5 (4.6%) 5 (4.6%) | 19 (13.5%)/20 (15.7%) 21 (21.7%) | 12 (14.6%)/13 (16.8%) 13 (16.8%) | 0.0032 |
| MACCEs | 20 (13.0%)/29 (25.3%) 31 (33.5%) | 41 (28.3%)/45 (35.8%) 49 (63.1%) | 20 (23.9%)/31 (48.1%) 32 (52.0%) | 0.0012 |
MACCEs: major adverse cardiac and cerebrovascular events.
Predictors of long-term major adverse cardiac and cerebrovascular event
Table 4 shows univariable and multivariable predictors of MACCE during follow-up after the operation, deployed in a Cox proportional-hazards model. In the multivariable analysis, SYNTAX score (HR 1.03, P = 0.0043) and logistic EuroSCORE II (HR 1.34, P = 0.0012) were significant predictors of long-term MACCEs.
| Variables . | Univariable . | Multivariable . | ||
|---|---|---|---|---|
| HR (95% CI) . | P-value . | HR (95% CI) . | P-value . | |
| Age | 1.05 (1.02–1.07) | 0.0001 | 1.03 (1.00–1.05) | 0.097 |
| Male gender | 0.67 (0.45–0.98) | 0.037 | 0.97 (0.62–1.52) | 0.90 |
| Coronary lesion (s) | 0.32 | |||
| Isolated LM | 0.44 (0.16–1.25) | 0.12 | ||
| LM + 1 vessel | 0.60 (0.27–1.36) | 0.22 | ||
| LM + 2 vessels | 0.58 (0.29–1.18) | 0.13 | ||
| LM + 3 vessels | 1.00 | – | ||
| 3 vessels | 0.78 (0.52–1.18) | 0.24 | ||
| SYNTAX score | 1.03 (1.01–1.05) | 0.0005 | 1.03 (1.01–1.05) | 0.0043 |
| DM | 1.09 (0.77–1.56) | 0.63 | ||
| EF | 0.98 (0.97–1.00) | 0.016 | 0.99 (0.98–1.01) | 0.50 |
| Logistic EuroSCORE II | 1.48 (1.29–1.71) | 0.0001 | 1.34 (1.12–1.59) | 0.0012 |
| SIMA/BIMA use | 0.014 | 0.64 | ||
| SIMA | 0.57 (0.26–1.22) | 0.15 | 0.73 (0.31–1.74) | 0.48 |
| BIMA | 0.31 (0.13–0.74) | 0.0084 | 0.61 (0.22–1.71) | 0.35 |
| Variables . | Univariable . | Multivariable . | ||
|---|---|---|---|---|
| HR (95% CI) . | P-value . | HR (95% CI) . | P-value . | |
| Age | 1.05 (1.02–1.07) | 0.0001 | 1.03 (1.00–1.05) | 0.097 |
| Male gender | 0.67 (0.45–0.98) | 0.037 | 0.97 (0.62–1.52) | 0.90 |
| Coronary lesion (s) | 0.32 | |||
| Isolated LM | 0.44 (0.16–1.25) | 0.12 | ||
| LM + 1 vessel | 0.60 (0.27–1.36) | 0.22 | ||
| LM + 2 vessels | 0.58 (0.29–1.18) | 0.13 | ||
| LM + 3 vessels | 1.00 | – | ||
| 3 vessels | 0.78 (0.52–1.18) | 0.24 | ||
| SYNTAX score | 1.03 (1.01–1.05) | 0.0005 | 1.03 (1.01–1.05) | 0.0043 |
| DM | 1.09 (0.77–1.56) | 0.63 | ||
| EF | 0.98 (0.97–1.00) | 0.016 | 0.99 (0.98–1.01) | 0.50 |
| Logistic EuroSCORE II | 1.48 (1.29–1.71) | 0.0001 | 1.34 (1.12–1.59) | 0.0012 |
| SIMA/BIMA use | 0.014 | 0.64 | ||
| SIMA | 0.57 (0.26–1.22) | 0.15 | 0.73 (0.31–1.74) | 0.48 |
| BIMA | 0.31 (0.13–0.74) | 0.0084 | 0.61 (0.22–1.71) | 0.35 |
BIMAs: bilateral internal mammary arteries; CI: confidence interval; DM: diabetes mellitus; HR: hazard ratio; LM: left main; MACCEs: major adverse cardiac and cerebrovascular events; MI: myocardial infarction; SIMA: single internal mammary artery; EF: ejection fraction.
| Variables . | Univariable . | Multivariable . | ||
|---|---|---|---|---|
| HR (95% CI) . | P-value . | HR (95% CI) . | P-value . | |
| Age | 1.05 (1.02–1.07) | 0.0001 | 1.03 (1.00–1.05) | 0.097 |
| Male gender | 0.67 (0.45–0.98) | 0.037 | 0.97 (0.62–1.52) | 0.90 |
| Coronary lesion (s) | 0.32 | |||
| Isolated LM | 0.44 (0.16–1.25) | 0.12 | ||
| LM + 1 vessel | 0.60 (0.27–1.36) | 0.22 | ||
| LM + 2 vessels | 0.58 (0.29–1.18) | 0.13 | ||
| LM + 3 vessels | 1.00 | – | ||
| 3 vessels | 0.78 (0.52–1.18) | 0.24 | ||
| SYNTAX score | 1.03 (1.01–1.05) | 0.0005 | 1.03 (1.01–1.05) | 0.0043 |
| DM | 1.09 (0.77–1.56) | 0.63 | ||
| EF | 0.98 (0.97–1.00) | 0.016 | 0.99 (0.98–1.01) | 0.50 |
| Logistic EuroSCORE II | 1.48 (1.29–1.71) | 0.0001 | 1.34 (1.12–1.59) | 0.0012 |
| SIMA/BIMA use | 0.014 | 0.64 | ||
| SIMA | 0.57 (0.26–1.22) | 0.15 | 0.73 (0.31–1.74) | 0.48 |
| BIMA | 0.31 (0.13–0.74) | 0.0084 | 0.61 (0.22–1.71) | 0.35 |
| Variables . | Univariable . | Multivariable . | ||
|---|---|---|---|---|
| HR (95% CI) . | P-value . | HR (95% CI) . | P-value . | |
| Age | 1.05 (1.02–1.07) | 0.0001 | 1.03 (1.00–1.05) | 0.097 |
| Male gender | 0.67 (0.45–0.98) | 0.037 | 0.97 (0.62–1.52) | 0.90 |
| Coronary lesion (s) | 0.32 | |||
| Isolated LM | 0.44 (0.16–1.25) | 0.12 | ||
| LM + 1 vessel | 0.60 (0.27–1.36) | 0.22 | ||
| LM + 2 vessels | 0.58 (0.29–1.18) | 0.13 | ||
| LM + 3 vessels | 1.00 | – | ||
| 3 vessels | 0.78 (0.52–1.18) | 0.24 | ||
| SYNTAX score | 1.03 (1.01–1.05) | 0.0005 | 1.03 (1.01–1.05) | 0.0043 |
| DM | 1.09 (0.77–1.56) | 0.63 | ||
| EF | 0.98 (0.97–1.00) | 0.016 | 0.99 (0.98–1.01) | 0.50 |
| Logistic EuroSCORE II | 1.48 (1.29–1.71) | 0.0001 | 1.34 (1.12–1.59) | 0.0012 |
| SIMA/BIMA use | 0.014 | 0.64 | ||
| SIMA | 0.57 (0.26–1.22) | 0.15 | 0.73 (0.31–1.74) | 0.48 |
| BIMA | 0.31 (0.13–0.74) | 0.0084 | 0.61 (0.22–1.71) | 0.35 |
BIMAs: bilateral internal mammary arteries; CI: confidence interval; DM: diabetes mellitus; HR: hazard ratio; LM: left main; MACCEs: major adverse cardiac and cerebrovascular events; MI: myocardial infarction; SIMA: single internal mammary artery; EF: ejection fraction.
DISCUSSION
CABG has been found to achieve a reduction of MI and mortality superior to PCI in high-risk patients with complex coronary artery lesions and left ventricular dysfunction; this finding is consistent in numerous randomized control trials, registry data and associated meta-analyses [5–8, 17–19]. We have routinely employed CABG for complex coronary artery lesions as a result [14]. During long-term follow-up, exceeding 15 years, the rates of MACCEs and repeat revascularization, but not combined outcomes of death-stroke/MI, were significantly better in patients with a lower SYNTAX score, who are potential candidates for PCI, than in patients with a higher SYNTAX score. Our main finding that long-term MACCE rates after conventional CABG for complex coronary lesions showed significant differences between the three groups according to the SYNTAX score tercile (log-rank P = 0.0012) (Fig. 4) was interesting because, in the SYNTAX trial, 5-year MACCE rates in the CABG cohort was reported to be independent of the SYNTAX score (28.6% in patients with a low-, 25.8% in patients with intermediate- and 26.8% in patients with high score) [8].
Complex coronary pathology as measured by the SYNTAX score reportedly implies worse long-term outcomes after PCI, but it is not clear whether the SYNTAX score is correlated with long-term outcomes after CABG [6–8]. In the multivariable analysis, however, the SYNTAX score (HR 1.03, P = 0.0043) proved to be a significant predictor of long-term MACCEs (Table 4). In the present study, the rate of complete revascularization was found to be significantly lower in the patients with a higher SYNTAX score than in those with a lower SYNTAX score (Table 2). Thus, the rate of repeat revascularization was significantly increased in the higher SYNTAX score group (Fig. 3), although the rate of combined outcomes of death/stroke/MI did not show statistical difference between the three groups (Fig. 2). We speculate, therefore, that long-term MACCEs after CABG in patients with complex coronary artery lesions is driven mainly by the incidence of repeat revascularization, estimated by the SYNTAX score. These results suggest that the SYNTAX score, which was introduced to measure the complexity and severity of atherosclerotic coronary disease, is prognostic of long-term outcomes after CABG for complex coronary artery lesions. Our data support the result of the SYNTAX trial that CABG should remain the standard of care for patients with complex coronary lesions. They also suggest that patients with lower SYNTAX score who were believed to be candidates for PCI might achieve better long-term MACCEs over 10 years, with conventional CABG.
The logistic EuroSCORE II was also a significant predictor of long-term MACCEs in the multivariable analysis. In our series, there were no significant differences in logistic EuroSCORE II between the three groups (1.3 ± 0.9% with low, 1.4 ± 1.0% with intermediate and 1.5 ± 1.0% with high score, P = 0.37) (Table 1). The operative mortality, as well as comorbidities such as perioperative stroke, perioperative MI, length of intensive care unit stay and length of hospital stay did not differ significantly between the three groups (Table 2). Furthermore, long-term combined outcomes of all-cause death, stroke and MI did not show statistical differences between the three groups (Fig. 2). These findings emphasize that the logistic EuroSCORE II, which was launched to assess risk factors for cardiac surgical mortality including CABG, is a better predictor of long-term outcomes after CABG for complex coronary artery lesions than the SYNTAX score [20].
The SYNTAX Score II was designed to overcome limitations of the anatomical SYNTAX score [21]. It augmented the SYNTAX score with clinical variables, namely age, creatinine and left ventricular ejection fraction, to be at least comparable with the 17-variable EuroSCORE in predicting in-hospital mortality after CABG. Furthermore, prospective validation studies are underway in the EXCEL Trial (LM) and planned SYNTAX II Trial (de novo three-vessel disease). In this respect, the SYNTAX score coupled with the additive logistic EuroSCORE II or several clinical variables including measures of frailty could accurately point to long-term outcomes and clinical risk in patients with complex coronary artery lesions.
We routinely employ conventional CABG with cardiopulmonary bypass with cardioplegic arrest, and use single or bilateral IMA as an in situ graft for better long-term graft patency [15]. We also confirm early revascularization of the LAD territory and culprit lesions, mainly by coronary graft angiography during hospitalization. We speculate that these surgical and perioperative managements, associated with less atherosclerotic anastomoses sites in CABG for patients with lower SYNTAX score, are at least partly responsible for the lower incidence of repeat revascularization, which in turn influences the MACCE rate.
From the mid-1990s, interest grew in performing CABG without the use of cardiopulmonary bypass (off pump), in order to reduce complications associated with the heart–lung machine [22]. However, a randomized trial and meta-analysis found a reduction in postoperative patency of bypass grafts performed during off-pump CABG [23, 24]. We believe that long-term graft patency after conventional CABG using an in situ IMA gives excellent long-term outcomes, with a 20.0% overall mortality and a 34.3% overall MACCE rate at 10 years. Our patients could have long-term benefits from conventional CABG as to be compared with age- and gender- matched Japanese population, who did not have cardiovascular disease, of 24.4% in the 10-year mortality rate [25].
Despite better long-term outcomes of CABG with the use of bilateral IMA [15], we did not find that our use of bilateral IMA is a significantly better predictor of long-term MACCEs, at least by the multivariable analysis. In the univariable analyses, however, our use of bilateral IMA was identified as a significant predictor of better combined outcomes (HR 0.17, P = 0.0005) (data not shown) and MACCEs (HR 0.31, P = 0.0084) (Table 4). We use single or bilateral IMA routinely as an in situ graft. Thus, in the present study, the number of the patients whose hearts were bypassed with bilateral IMA was small [n = 84 (21.2%)] relative to those bypassed with a single IMA [n = 298 (75.2%)].
The main limitation in this study comes from the small numbers in the SYNTAX score sub-groups. We analysed only 87 patients with a high SYNTAX score and failed complete follow-up in all patients. This study also has its retrospective and single institutional nature. There was also no joint assessment by the heart team aiming to classify whether patients were equally suitable for revascularization with CABG and PCI in this retrospective setting. Although this was a relatively large cohort of patients routinely undergoing CABG for complex coronary artery lesions, patients suitable only for PCI might nevertheless be entered in the study group. In addition, our long-term graft patency failed to give any improvement in long-term outcomes. Despite this, we believe that our excellent long-term outcomes after CABG in patients with complex coronary artery lesions can assist physicians in determining the optimal revascularization method involving Class I or II recommendation for PCI. Although we have excellent results upon employing conventional CABG, this study was not designed to show that conventional CABG is superior to off-pump CABG.
In our routine strategy of conventional CABG for complex coronary artery lesions, the SYNTAX score, which evaluates coronary pathology as a determinant of treatment, is indeed prognostic of long-term outcomes after CABG. These results support the result of the SYNTAX trial that CABG should remain the standard of care for patients with complex lesions. Our findings also provide a benchmark against which long-term outcomes of PCI for complex coronary artery lesions can be compared.
Conflict of interest: none declared.
REFERENCES
APPENDIX. CONFERENCE DISCUSSION
Dr R. Yadav(London, UK): If I'm right, I think you have looked at patients who have had coronary artery bypass graft over a period of time, 10 years, and in equally-matched groups you have shown that patients with worse coronary anatomy or more aggressive disease do worse in the longer term. I just wonder whether that tells us something which we knew already intuitively and whether we should focus our efforts on aggressive secondary prevention with patients who have got really bad coronary disease, bad SYNTAX scores. In that context, my question to you is, and it's not in your paper, whether it is possible for you to compare the patients who have undergone coronary artery bypass graft with an age-atched normal population and see whether performing coronary artery bypass graft on these patients adds value and whether or not the curve normalizes to a normal curve after coronary artery bypass graft. That would be quite interesting to see.
My second observation is, you have arrived pretty much at the SYNTAX II score, so you have looked at Euro SCORE and SYNTAX score together and shown that it predicts long-term mortality for patients, and I think SYNTAX has done it the other way around and they have started off with the SYNTAX score and then they got parameters from the Euro SCORE and seen that that is also predictive of long-term outcome. Your comments, please?
Dr Cho: Unfortunately, I have no information on the 10-year MACCE rate in the control group of age-matched non-cardiovascular disease. However, in the present study, the overall 10-year mortality was 20%. It is less than the 10-year rate of age-matched non-cardiovascular Japanese population of 29%. The 10-year rate of stroke in the present cohort and age-matched non-cardiovascular population was respectively 8% and 10%. The 10-year rate of myocardial infarction in the present cohort was 6.7%. It is much higher than that of the age-matched non-cardiovascular population of 0.1%. These findings show patients with complex coronary lesions have long-term benefits undergoing coronary artery bypass graft in terms of survival and stroke. We speculate that postoperative management is related to better long-term outcomes in the present cohort. Actually, we administer an antiplatelet agent and a statin before the operation. We also control hypertension, hyperlipidaemia, and diabetes. So your second question?
Dr Yadav: It was really a comment rather than a question. It was an observation.
Dr D. Pagano(Birmingham, UK): I would like to ask you a methodological question. You looked at the SYNTAX score in the early population. How did you calculate their score? The second methodological question is, how do you actually know about death and stroke in this population.
Dr Cho: We have data from the Japanese population on risk of stroke and myocardial infarction and survival, so we compared this data from my personal data.
Dr Pagano: So from a registry?
Dr Cho: The Japanese registry.
Dr Pagano: And how did you calculate the SYNTAX score in the earlier?
Dr Cho: They are non-cardiovascular patients. This is in my cohort.
Dr Pagano: So in your cohort the SYNTAX score was prospectively calculated at the time of surgery?
Dr Cho: Yes.
Author notes
Presented at the 29th Annual Meeting of the European Association for Cardio-Thoracic Surgery, Amsterdam, Netherlands, 3–7 October 2015.




