-
PDF
- Split View
-
Views
-
Cite
Cite
Amir H. Sepehripour, Umar A. Chaudhry, Amna Suliman, Emaddin Kidher, Nusrat Sayani, Hutan Ashrafian, Leanne Harling, Thanos Athanasiou, How revascularization on the beating heart with cardiopulmonary bypass compares to off-pump? A meta-analysis of observational studies, Interactive CardioVascular and Thoracic Surgery, Volume 22, Issue 1, January 2016, Pages 63–71, https://doi.org/10.1093/icvts/ivv291
Close - Share Icon Share
Abstract
Off-pump coronary artery bypass surgery has been a controversial area of debate and the outcome profile of the technique has been thoroughly investigated. Scepticism regarding the reported outcomes and the conduct of the randomized trials comparing this technique with conventional on-pump coronary artery bypass surgery has been widely voiced, and the technique of off-pump surgery remains as an infrequently adopted approach to myocardial revascularization worldwide. Criticisms of the technique are related to lower rates of complete revascularization and its unknown long-term consequences, the significant detrimental effects on mortality and major adverse events when emergency conversion is required, and the significant lack of long-term survival and morbidity data. The hybrid technique of myocardial revascularization on the beating heart with the use of cardiopulmonary bypass may theoretically provide the beneficial effects of off-pump surgery in terms of myocardial protection and organ protection, while providing the safety and stability of on-pump surgery to allow complete revascularization. Large randomized comparison to support evidence-based choices is currently lacking. In this article, we have meta-analysed the outcomes of on-pump beating heart surgery in comparison with off-pump surgery focusing on major adverse cardiovascular and cerebrovascular adverse events (MACCE) including mortality, stroke and myocardial infarction and the degree of revascularization and number of bypass grafts performed. It was demonstrated that the beating heart on-pump technique allows a significantly higher number of bypass grafts to be performed, resulting in significantly higher degree of revascularization. We have also demonstrated a slightly higher rate of 30-day mortality and MACCE with the technique although not at a statistically significant level. These results should be considered alongside the population risk profile, where a significantly higher risk cohort had undergone the beating heart on-pump technique. Long-term survival and morbidity figures are required to assess the impact of these findings in the coronary surgery patient population.
INTRODUCTION
Off-pump coronary artery bypass (OPCAB) surgery has been thoroughly investigated and scrutinized with regard to its outcome profile [1–3]. Mortality, major adverse cardiovascular and cerebrovascular events (MACCE) as well as end-organ damage or protection, completeness of revascularization and, finally, the impact of conversion to on-pump (ONCAB) surgery have all been topics of much research and debate [4, 5]. Despite some scepticism regarding the conduct of particular randomized trials assessing the outcome of OPCAB surgery, it has been widely accepted that there are potential benefits in terms of mortality and end-organ protection when avoiding cardiopulmonary bypass [6–9]. There are, however, aspects of OPCAB surgery which have led to questions being raised regarding its widespread application, and which may well detract from its superior outcome profile. First is the completeness of revascularization, which has been well documented to be significantly less when employing the off-pump technique [6]. The long-term survival impact of this under-revascularization is yet to be determined. Second is the significant impact on mortality and MACCE when emergency conversion to ONCAB surgery is required [10]. Third, there is a significant lack of long-term survival and morbidity data with the OPCAB technique, which is reflected in the ambiguity of the impact of the above two factors (completeness of revascularization and emergency conversion) on the long-term outcome profile of the technique. Fourth, there is a profound learning curve associated with the OPCAB technique, which is technically more challenging in comparison with ONCAB technique.
The technique of myocardial revascularization on the beating heart (BH) with the use of cardiopulmonary bypass is one which will theoretically provide the benefits of OPCAB surgery in terms of myocardial and end-organ protection, while providing the safety and stability of ONCAB surgery to allow complete revascularization.
The aims of this study were to address the following questions: (i) Is the on-pump BH technique associated with a lower incidence of mortality and MACCE compared with OPCAB? (ii) Is there a difference in the incidence of myocardial infarction (MI), the degree of revascularization and the number of bypass grafts performed between the two groups? (iii) Is there heterogeneity in the data of the outcome profile of the two techniques (assessed by sensitivity analysis and meta-regression to assess the influence of moderator variables on effect size)?
MATERIALS AND METHODS
Search
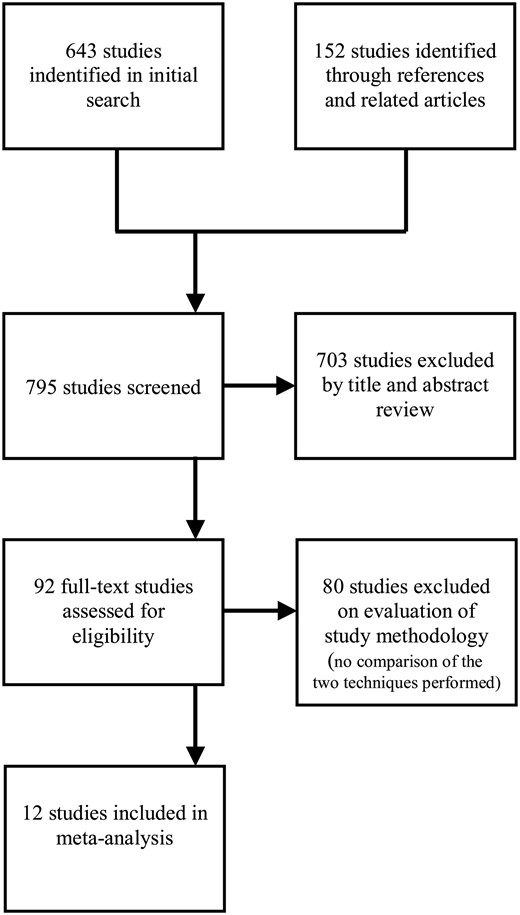
A literature search was performed using PubMed, EMBASE and Google Scholar up to December 2014 using the MESH headings ‘coronary surgery’, ‘off-pump’ and ‘beating heart’. Cochrane Central Register of Controlled Trials (CENTRAL/CCTR) and ClinicalTrials.gov were also searched. All types of studies were searched for including randomized trials and retrospective studies. Studies in English that compared outcomes in patients undergoing OPCAB versus BH were included (Table 1).
| Study (n) . | n . | Mean age . | Redo . | Mean EF . | Previous MI . | CCF/NYHA III/IV . | Previous
CVA/TIA . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | |
| Darwazah et al. [11] (137) | 98 (72%) | 39 (28%) | 57.0 ± 10 | 58.0 ± 8 | 3 (3%)* | 5 (13%)* | 26.0 ± 5 | 28.0 ± 6 | 65 (66%) | 26 (67%) | 52 (53%) | 12 (31%) | 6 (6%) | 5 (13%) |
| Edgerton et al. [12] (2272) | 1908 (84%) | 364 (16%) | 64.0 ± 11.3 | 63.4 ± 10.3 | 158 (8%)* | 43 (12%)* | 51.0 ± 13.1* | 45.6 ± 12.5* | 797 (42%)* | 196 (54%)* | 242 (13%)* | 59 (17%)* | 126 (7%)* | 33 (9%)* |
| Jalal et al. [13] (30) | 15 (50%) | 15 (50%) | 54.6 ± 11.1 | 63.1 ± 10.2 | NS | NS | 45.0 ± 8 | 40.0 ± 8.6 | NS | NS | NS | NS | NS | NS |
| Letsou et al. [14] (481) | 397 (83%) | 84 (17%) | NS | NS | NS | NS | 53.5 ± 14.5 | 46.3 ± 18.1 | 261 (66%)* | 65 (78%)* | 113 (29%)* | 37 (46%)* | 45 (11%) | 10 (12%) |
| Lin et al. [15] (25) | 12 (48%) | 13 (52%) | 62.6 ± 6.5 | 63.4 ± 5 | NS | NS | 54.7 ± 5.8 | 50.5 ± 8 | 3 (25%) | 3 (25%) | 1 (8%) | 0 (0%) | NS | NS |
| Munos et al. [16] (108) | 57 (53%) | 51 (47%) | 73.7 ± 9.9 | 72.9 ± 7.8 | 2 (3%) | 2 (4%) | 33.6 ± 10.1 | 35.0 ± 11.6 | 29 (51%) | 27 (53%) | NS | NS | NS | NS |
| Rastan et al. [17] (40) | 19 (48%) | 21 (52%) | 63.0 ± 6 | 65.3 ± 3.9 | NS | NS | 66.1 ± 6.7 | 63.0 ± 14.2 | 9 (45%) | 8 (40%) | NS | NS | NS | NS |
| Reber et al. [18] (302) | 185 (61%) | 117 (39%) | 69.3 ± 1* | 72.1 ± 8* | 4 (2%) | 9 (8%) | NS | NS | 81 (43%) | 32 (27%) | NS | NS | NS | NS |
| Sabban et al. [19] (54) | 21 (39%) | 33 (61%) | 55.9 ± 12.7 | 63.8 ± 10.3 | NS | NS | 45.8 ± 10.9* | 40.1 ± 11.2* | NS | NS | 1 (5%) | 5 (15%) | 0 (0%) | 0 (0%) |
| Tsai et al. [20] (104) | 56 (54%) | 48 (46%) | 62.7 ± 11.9* | 68.3 ± 12* | NS | NS | 55.2 ± 12.6* | 40.9 ± 9.9* | 8 (14%) | 10 (21%) | 36 (64%)* | 40 (83%)* | 13 (23%) | 12 (25%) |
| Uva et al. [21] (155) | 108 (70%) | 47 (30%) | 65.0 ± 9.3 | 66.2 ± 9.7 | NS | NS | NS | NS | NS | NS | 72 (67%) | 27 (54%) | NS | NS |
| Wan et al. [22] (37) | 18 (49%) | 19 (51%) | 63.6 ± 10.5 | 65.4 ± 9.1 | NS | NS | 52.9 ± 13.4 | 50.4 ± 12 | 4 (22%) | 3 (16%) | 8 (44%) | 6 (32%) | NS | NS |
| Hypertension | Diabetes | Renal dysfunction | COPD | Urgent/emergent | EuroSCORE | |||||||||
| OP | BH | OP | BH | OP | BH | OP | BH | OP | BH | OP | BH | |||
| Darwazah et al. [11] (137) | 49 (50%) | 17 (44%) | 45 (46%) | 18 (46%) | 11 (11%) | 6 (15%) | 15 (15%) | 6 (15%) | 28 (29%) | 8 (21%) | 12.2 ± 12.5 | 14.1 ± 11.0 | ||
| Edgerton et al. [12] (2272) | 1360 (71%) | 254 (70%) | 620 (33%) | 115 (32%) | 99 (5%)* | 16 (4%)* | 270 (14%)* | 42 (12%)* | 981 (52%)* | 225 (62%)* | NS | NS | ||
| Jalal et al. [13] (30) | 2 (13%) | 8 (53%) | 6 (40%) | 7 (47%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Letsou et al. [14] (481) | 336 (85%) | 72 (88%) | 158 (40%) | 36 (44%) | NS | NS | 124 (31%)* | 37 (45%)* | 294 (75%) | 45 (75%) | NS | NS | ||
| Lin et al. [15] (25) | 8 (67%) | 10 (77%) | 5 (42%) | 7 (54%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Munos et al. [16] (108) | 51 (89%) | 45 (88%) | 35 (61%) | 32 (62%) | 34 (59%) | 25 (49%) | 25 (44%) | 22 (43%) | 25 (44%) | 23 (45%) | 12.8 ± 3.5 | 13.3 ± 3.3 | ||
| Rastan et al. [17] (40) | 20 (100%) | 18 (90%) | 13 (65%) | 12 (60%) | NS | NS | NS | NS | NS | NS | 3.4 ± 2.3 | 3.3 ± 2.1 | ||
| Reber et al. [18] (302) | NS | NS | NS | NS | 35 (19%)* | 16 (14%)* | 43 (23.2%) | 27 (23%) | NS | NS | 5.4* | 6.5* | ||
| Sabban et al. [19] (54) | 9 (43%) | 24 (73%) | 11 (52%) | 25 (76%) | NS | NS | 1 (5%) | 2 (9%) | 6 (29%) | 3 (13%) | NS | NS | ||
| Tsai et al. [20] (104) | 21 (38%) | 19 (40%) | 38 (68%) | 34 (71%) | 56 (100%) | 48 (100%) | 12 (21%) | 11 (23%) | 14 (25%) | 13 (27%) | 8.4 ± 3.6* | 11.4 ± 5.0* | ||
| Uva et al. [21] (155) | 85 (79%) | 29 (62%) | 31 (29%) | 21 (45%) | NS | NS | NS | NS | NS | NS | 2.8 | 3.1 | ||
| Wan et al. [22] (37) | 13 (72%) | 15 (79%) | 7 (39%) | 6 (32%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Study (n) . | n . | Mean age . | Redo . | Mean EF . | Previous MI . | CCF/NYHA III/IV . | Previous
CVA/TIA . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | |
| Darwazah et al. [11] (137) | 98 (72%) | 39 (28%) | 57.0 ± 10 | 58.0 ± 8 | 3 (3%)* | 5 (13%)* | 26.0 ± 5 | 28.0 ± 6 | 65 (66%) | 26 (67%) | 52 (53%) | 12 (31%) | 6 (6%) | 5 (13%) |
| Edgerton et al. [12] (2272) | 1908 (84%) | 364 (16%) | 64.0 ± 11.3 | 63.4 ± 10.3 | 158 (8%)* | 43 (12%)* | 51.0 ± 13.1* | 45.6 ± 12.5* | 797 (42%)* | 196 (54%)* | 242 (13%)* | 59 (17%)* | 126 (7%)* | 33 (9%)* |
| Jalal et al. [13] (30) | 15 (50%) | 15 (50%) | 54.6 ± 11.1 | 63.1 ± 10.2 | NS | NS | 45.0 ± 8 | 40.0 ± 8.6 | NS | NS | NS | NS | NS | NS |
| Letsou et al. [14] (481) | 397 (83%) | 84 (17%) | NS | NS | NS | NS | 53.5 ± 14.5 | 46.3 ± 18.1 | 261 (66%)* | 65 (78%)* | 113 (29%)* | 37 (46%)* | 45 (11%) | 10 (12%) |
| Lin et al. [15] (25) | 12 (48%) | 13 (52%) | 62.6 ± 6.5 | 63.4 ± 5 | NS | NS | 54.7 ± 5.8 | 50.5 ± 8 | 3 (25%) | 3 (25%) | 1 (8%) | 0 (0%) | NS | NS |
| Munos et al. [16] (108) | 57 (53%) | 51 (47%) | 73.7 ± 9.9 | 72.9 ± 7.8 | 2 (3%) | 2 (4%) | 33.6 ± 10.1 | 35.0 ± 11.6 | 29 (51%) | 27 (53%) | NS | NS | NS | NS |
| Rastan et al. [17] (40) | 19 (48%) | 21 (52%) | 63.0 ± 6 | 65.3 ± 3.9 | NS | NS | 66.1 ± 6.7 | 63.0 ± 14.2 | 9 (45%) | 8 (40%) | NS | NS | NS | NS |
| Reber et al. [18] (302) | 185 (61%) | 117 (39%) | 69.3 ± 1* | 72.1 ± 8* | 4 (2%) | 9 (8%) | NS | NS | 81 (43%) | 32 (27%) | NS | NS | NS | NS |
| Sabban et al. [19] (54) | 21 (39%) | 33 (61%) | 55.9 ± 12.7 | 63.8 ± 10.3 | NS | NS | 45.8 ± 10.9* | 40.1 ± 11.2* | NS | NS | 1 (5%) | 5 (15%) | 0 (0%) | 0 (0%) |
| Tsai et al. [20] (104) | 56 (54%) | 48 (46%) | 62.7 ± 11.9* | 68.3 ± 12* | NS | NS | 55.2 ± 12.6* | 40.9 ± 9.9* | 8 (14%) | 10 (21%) | 36 (64%)* | 40 (83%)* | 13 (23%) | 12 (25%) |
| Uva et al. [21] (155) | 108 (70%) | 47 (30%) | 65.0 ± 9.3 | 66.2 ± 9.7 | NS | NS | NS | NS | NS | NS | 72 (67%) | 27 (54%) | NS | NS |
| Wan et al. [22] (37) | 18 (49%) | 19 (51%) | 63.6 ± 10.5 | 65.4 ± 9.1 | NS | NS | 52.9 ± 13.4 | 50.4 ± 12 | 4 (22%) | 3 (16%) | 8 (44%) | 6 (32%) | NS | NS |
| Hypertension | Diabetes | Renal dysfunction | COPD | Urgent/emergent | EuroSCORE | |||||||||
| OP | BH | OP | BH | OP | BH | OP | BH | OP | BH | OP | BH | |||
| Darwazah et al. [11] (137) | 49 (50%) | 17 (44%) | 45 (46%) | 18 (46%) | 11 (11%) | 6 (15%) | 15 (15%) | 6 (15%) | 28 (29%) | 8 (21%) | 12.2 ± 12.5 | 14.1 ± 11.0 | ||
| Edgerton et al. [12] (2272) | 1360 (71%) | 254 (70%) | 620 (33%) | 115 (32%) | 99 (5%)* | 16 (4%)* | 270 (14%)* | 42 (12%)* | 981 (52%)* | 225 (62%)* | NS | NS | ||
| Jalal et al. [13] (30) | 2 (13%) | 8 (53%) | 6 (40%) | 7 (47%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Letsou et al. [14] (481) | 336 (85%) | 72 (88%) | 158 (40%) | 36 (44%) | NS | NS | 124 (31%)* | 37 (45%)* | 294 (75%) | 45 (75%) | NS | NS | ||
| Lin et al. [15] (25) | 8 (67%) | 10 (77%) | 5 (42%) | 7 (54%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Munos et al. [16] (108) | 51 (89%) | 45 (88%) | 35 (61%) | 32 (62%) | 34 (59%) | 25 (49%) | 25 (44%) | 22 (43%) | 25 (44%) | 23 (45%) | 12.8 ± 3.5 | 13.3 ± 3.3 | ||
| Rastan et al. [17] (40) | 20 (100%) | 18 (90%) | 13 (65%) | 12 (60%) | NS | NS | NS | NS | NS | NS | 3.4 ± 2.3 | 3.3 ± 2.1 | ||
| Reber et al. [18] (302) | NS | NS | NS | NS | 35 (19%)* | 16 (14%)* | 43 (23.2%) | 27 (23%) | NS | NS | 5.4* | 6.5* | ||
| Sabban et al. [19] (54) | 9 (43%) | 24 (73%) | 11 (52%) | 25 (76%) | NS | NS | 1 (5%) | 2 (9%) | 6 (29%) | 3 (13%) | NS | NS | ||
| Tsai et al. [20] (104) | 21 (38%) | 19 (40%) | 38 (68%) | 34 (71%) | 56 (100%) | 48 (100%) | 12 (21%) | 11 (23%) | 14 (25%) | 13 (27%) | 8.4 ± 3.6* | 11.4 ± 5.0* | ||
| Uva et al. [21] (155) | 85 (79%) | 29 (62%) | 31 (29%) | 21 (45%) | NS | NS | NS | NS | NS | NS | 2.8 | 3.1 | ||
| Wan et al. [22] (37) | 13 (72%) | 15 (79%) | 7 (39%) | 6 (32%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
EF: ejection fraction; MI: myocardial infarction; CCF: congestive cardiac failure; NYHA: New York Heart Association; CVA: cerebrovascular accident; TIA: transient ischaemic attack; COPD: chronic obstructive pulmonary disease; NS: not stated; BH: beating heart; OP: off-pump; OPCAB: off-pump coronary artery bypass.
*Statistical significance.
| Study (n) . | n . | Mean age . | Redo . | Mean EF . | Previous MI . | CCF/NYHA III/IV . | Previous
CVA/TIA . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | |
| Darwazah et al. [11] (137) | 98 (72%) | 39 (28%) | 57.0 ± 10 | 58.0 ± 8 | 3 (3%)* | 5 (13%)* | 26.0 ± 5 | 28.0 ± 6 | 65 (66%) | 26 (67%) | 52 (53%) | 12 (31%) | 6 (6%) | 5 (13%) |
| Edgerton et al. [12] (2272) | 1908 (84%) | 364 (16%) | 64.0 ± 11.3 | 63.4 ± 10.3 | 158 (8%)* | 43 (12%)* | 51.0 ± 13.1* | 45.6 ± 12.5* | 797 (42%)* | 196 (54%)* | 242 (13%)* | 59 (17%)* | 126 (7%)* | 33 (9%)* |
| Jalal et al. [13] (30) | 15 (50%) | 15 (50%) | 54.6 ± 11.1 | 63.1 ± 10.2 | NS | NS | 45.0 ± 8 | 40.0 ± 8.6 | NS | NS | NS | NS | NS | NS |
| Letsou et al. [14] (481) | 397 (83%) | 84 (17%) | NS | NS | NS | NS | 53.5 ± 14.5 | 46.3 ± 18.1 | 261 (66%)* | 65 (78%)* | 113 (29%)* | 37 (46%)* | 45 (11%) | 10 (12%) |
| Lin et al. [15] (25) | 12 (48%) | 13 (52%) | 62.6 ± 6.5 | 63.4 ± 5 | NS | NS | 54.7 ± 5.8 | 50.5 ± 8 | 3 (25%) | 3 (25%) | 1 (8%) | 0 (0%) | NS | NS |
| Munos et al. [16] (108) | 57 (53%) | 51 (47%) | 73.7 ± 9.9 | 72.9 ± 7.8 | 2 (3%) | 2 (4%) | 33.6 ± 10.1 | 35.0 ± 11.6 | 29 (51%) | 27 (53%) | NS | NS | NS | NS |
| Rastan et al. [17] (40) | 19 (48%) | 21 (52%) | 63.0 ± 6 | 65.3 ± 3.9 | NS | NS | 66.1 ± 6.7 | 63.0 ± 14.2 | 9 (45%) | 8 (40%) | NS | NS | NS | NS |
| Reber et al. [18] (302) | 185 (61%) | 117 (39%) | 69.3 ± 1* | 72.1 ± 8* | 4 (2%) | 9 (8%) | NS | NS | 81 (43%) | 32 (27%) | NS | NS | NS | NS |
| Sabban et al. [19] (54) | 21 (39%) | 33 (61%) | 55.9 ± 12.7 | 63.8 ± 10.3 | NS | NS | 45.8 ± 10.9* | 40.1 ± 11.2* | NS | NS | 1 (5%) | 5 (15%) | 0 (0%) | 0 (0%) |
| Tsai et al. [20] (104) | 56 (54%) | 48 (46%) | 62.7 ± 11.9* | 68.3 ± 12* | NS | NS | 55.2 ± 12.6* | 40.9 ± 9.9* | 8 (14%) | 10 (21%) | 36 (64%)* | 40 (83%)* | 13 (23%) | 12 (25%) |
| Uva et al. [21] (155) | 108 (70%) | 47 (30%) | 65.0 ± 9.3 | 66.2 ± 9.7 | NS | NS | NS | NS | NS | NS | 72 (67%) | 27 (54%) | NS | NS |
| Wan et al. [22] (37) | 18 (49%) | 19 (51%) | 63.6 ± 10.5 | 65.4 ± 9.1 | NS | NS | 52.9 ± 13.4 | 50.4 ± 12 | 4 (22%) | 3 (16%) | 8 (44%) | 6 (32%) | NS | NS |
| Hypertension | Diabetes | Renal dysfunction | COPD | Urgent/emergent | EuroSCORE | |||||||||
| OP | BH | OP | BH | OP | BH | OP | BH | OP | BH | OP | BH | |||
| Darwazah et al. [11] (137) | 49 (50%) | 17 (44%) | 45 (46%) | 18 (46%) | 11 (11%) | 6 (15%) | 15 (15%) | 6 (15%) | 28 (29%) | 8 (21%) | 12.2 ± 12.5 | 14.1 ± 11.0 | ||
| Edgerton et al. [12] (2272) | 1360 (71%) | 254 (70%) | 620 (33%) | 115 (32%) | 99 (5%)* | 16 (4%)* | 270 (14%)* | 42 (12%)* | 981 (52%)* | 225 (62%)* | NS | NS | ||
| Jalal et al. [13] (30) | 2 (13%) | 8 (53%) | 6 (40%) | 7 (47%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Letsou et al. [14] (481) | 336 (85%) | 72 (88%) | 158 (40%) | 36 (44%) | NS | NS | 124 (31%)* | 37 (45%)* | 294 (75%) | 45 (75%) | NS | NS | ||
| Lin et al. [15] (25) | 8 (67%) | 10 (77%) | 5 (42%) | 7 (54%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Munos et al. [16] (108) | 51 (89%) | 45 (88%) | 35 (61%) | 32 (62%) | 34 (59%) | 25 (49%) | 25 (44%) | 22 (43%) | 25 (44%) | 23 (45%) | 12.8 ± 3.5 | 13.3 ± 3.3 | ||
| Rastan et al. [17] (40) | 20 (100%) | 18 (90%) | 13 (65%) | 12 (60%) | NS | NS | NS | NS | NS | NS | 3.4 ± 2.3 | 3.3 ± 2.1 | ||
| Reber et al. [18] (302) | NS | NS | NS | NS | 35 (19%)* | 16 (14%)* | 43 (23.2%) | 27 (23%) | NS | NS | 5.4* | 6.5* | ||
| Sabban et al. [19] (54) | 9 (43%) | 24 (73%) | 11 (52%) | 25 (76%) | NS | NS | 1 (5%) | 2 (9%) | 6 (29%) | 3 (13%) | NS | NS | ||
| Tsai et al. [20] (104) | 21 (38%) | 19 (40%) | 38 (68%) | 34 (71%) | 56 (100%) | 48 (100%) | 12 (21%) | 11 (23%) | 14 (25%) | 13 (27%) | 8.4 ± 3.6* | 11.4 ± 5.0* | ||
| Uva et al. [21] (155) | 85 (79%) | 29 (62%) | 31 (29%) | 21 (45%) | NS | NS | NS | NS | NS | NS | 2.8 | 3.1 | ||
| Wan et al. [22] (37) | 13 (72%) | 15 (79%) | 7 (39%) | 6 (32%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Study (n) . | n . | Mean age . | Redo . | Mean EF . | Previous MI . | CCF/NYHA III/IV . | Previous
CVA/TIA . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | OP . | BH . | |
| Darwazah et al. [11] (137) | 98 (72%) | 39 (28%) | 57.0 ± 10 | 58.0 ± 8 | 3 (3%)* | 5 (13%)* | 26.0 ± 5 | 28.0 ± 6 | 65 (66%) | 26 (67%) | 52 (53%) | 12 (31%) | 6 (6%) | 5 (13%) |
| Edgerton et al. [12] (2272) | 1908 (84%) | 364 (16%) | 64.0 ± 11.3 | 63.4 ± 10.3 | 158 (8%)* | 43 (12%)* | 51.0 ± 13.1* | 45.6 ± 12.5* | 797 (42%)* | 196 (54%)* | 242 (13%)* | 59 (17%)* | 126 (7%)* | 33 (9%)* |
| Jalal et al. [13] (30) | 15 (50%) | 15 (50%) | 54.6 ± 11.1 | 63.1 ± 10.2 | NS | NS | 45.0 ± 8 | 40.0 ± 8.6 | NS | NS | NS | NS | NS | NS |
| Letsou et al. [14] (481) | 397 (83%) | 84 (17%) | NS | NS | NS | NS | 53.5 ± 14.5 | 46.3 ± 18.1 | 261 (66%)* | 65 (78%)* | 113 (29%)* | 37 (46%)* | 45 (11%) | 10 (12%) |
| Lin et al. [15] (25) | 12 (48%) | 13 (52%) | 62.6 ± 6.5 | 63.4 ± 5 | NS | NS | 54.7 ± 5.8 | 50.5 ± 8 | 3 (25%) | 3 (25%) | 1 (8%) | 0 (0%) | NS | NS |
| Munos et al. [16] (108) | 57 (53%) | 51 (47%) | 73.7 ± 9.9 | 72.9 ± 7.8 | 2 (3%) | 2 (4%) | 33.6 ± 10.1 | 35.0 ± 11.6 | 29 (51%) | 27 (53%) | NS | NS | NS | NS |
| Rastan et al. [17] (40) | 19 (48%) | 21 (52%) | 63.0 ± 6 | 65.3 ± 3.9 | NS | NS | 66.1 ± 6.7 | 63.0 ± 14.2 | 9 (45%) | 8 (40%) | NS | NS | NS | NS |
| Reber et al. [18] (302) | 185 (61%) | 117 (39%) | 69.3 ± 1* | 72.1 ± 8* | 4 (2%) | 9 (8%) | NS | NS | 81 (43%) | 32 (27%) | NS | NS | NS | NS |
| Sabban et al. [19] (54) | 21 (39%) | 33 (61%) | 55.9 ± 12.7 | 63.8 ± 10.3 | NS | NS | 45.8 ± 10.9* | 40.1 ± 11.2* | NS | NS | 1 (5%) | 5 (15%) | 0 (0%) | 0 (0%) |
| Tsai et al. [20] (104) | 56 (54%) | 48 (46%) | 62.7 ± 11.9* | 68.3 ± 12* | NS | NS | 55.2 ± 12.6* | 40.9 ± 9.9* | 8 (14%) | 10 (21%) | 36 (64%)* | 40 (83%)* | 13 (23%) | 12 (25%) |
| Uva et al. [21] (155) | 108 (70%) | 47 (30%) | 65.0 ± 9.3 | 66.2 ± 9.7 | NS | NS | NS | NS | NS | NS | 72 (67%) | 27 (54%) | NS | NS |
| Wan et al. [22] (37) | 18 (49%) | 19 (51%) | 63.6 ± 10.5 | 65.4 ± 9.1 | NS | NS | 52.9 ± 13.4 | 50.4 ± 12 | 4 (22%) | 3 (16%) | 8 (44%) | 6 (32%) | NS | NS |
| Hypertension | Diabetes | Renal dysfunction | COPD | Urgent/emergent | EuroSCORE | |||||||||
| OP | BH | OP | BH | OP | BH | OP | BH | OP | BH | OP | BH | |||
| Darwazah et al. [11] (137) | 49 (50%) | 17 (44%) | 45 (46%) | 18 (46%) | 11 (11%) | 6 (15%) | 15 (15%) | 6 (15%) | 28 (29%) | 8 (21%) | 12.2 ± 12.5 | 14.1 ± 11.0 | ||
| Edgerton et al. [12] (2272) | 1360 (71%) | 254 (70%) | 620 (33%) | 115 (32%) | 99 (5%)* | 16 (4%)* | 270 (14%)* | 42 (12%)* | 981 (52%)* | 225 (62%)* | NS | NS | ||
| Jalal et al. [13] (30) | 2 (13%) | 8 (53%) | 6 (40%) | 7 (47%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Letsou et al. [14] (481) | 336 (85%) | 72 (88%) | 158 (40%) | 36 (44%) | NS | NS | 124 (31%)* | 37 (45%)* | 294 (75%) | 45 (75%) | NS | NS | ||
| Lin et al. [15] (25) | 8 (67%) | 10 (77%) | 5 (42%) | 7 (54%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
| Munos et al. [16] (108) | 51 (89%) | 45 (88%) | 35 (61%) | 32 (62%) | 34 (59%) | 25 (49%) | 25 (44%) | 22 (43%) | 25 (44%) | 23 (45%) | 12.8 ± 3.5 | 13.3 ± 3.3 | ||
| Rastan et al. [17] (40) | 20 (100%) | 18 (90%) | 13 (65%) | 12 (60%) | NS | NS | NS | NS | NS | NS | 3.4 ± 2.3 | 3.3 ± 2.1 | ||
| Reber et al. [18] (302) | NS | NS | NS | NS | 35 (19%)* | 16 (14%)* | 43 (23.2%) | 27 (23%) | NS | NS | 5.4* | 6.5* | ||
| Sabban et al. [19] (54) | 9 (43%) | 24 (73%) | 11 (52%) | 25 (76%) | NS | NS | 1 (5%) | 2 (9%) | 6 (29%) | 3 (13%) | NS | NS | ||
| Tsai et al. [20] (104) | 21 (38%) | 19 (40%) | 38 (68%) | 34 (71%) | 56 (100%) | 48 (100%) | 12 (21%) | 11 (23%) | 14 (25%) | 13 (27%) | 8.4 ± 3.6* | 11.4 ± 5.0* | ||
| Uva et al. [21] (155) | 85 (79%) | 29 (62%) | 31 (29%) | 21 (45%) | NS | NS | NS | NS | NS | NS | 2.8 | 3.1 | ||
| Wan et al. [22] (37) | 13 (72%) | 15 (79%) | 7 (39%) | 6 (32%) | NS | NS | NS | NS | NS | NS | NS | NS | ||
EF: ejection fraction; MI: myocardial infarction; CCF: congestive cardiac failure; NYHA: New York Heart Association; CVA: cerebrovascular accident; TIA: transient ischaemic attack; COPD: chronic obstructive pulmonary disease; NS: not stated; BH: beating heart; OP: off-pump; OPCAB: off-pump coronary artery bypass.
*Statistical significance.
Outcomes of interest
Comparisons of interest in the OPCAB and BH groups were 30-day mortality, MI, composite outcome of MACCE (composite of 30-day mortality, stroke and MI), the completeness of revascularization and the mean number of bypass grafts constructed.
Analysis
Meta-analysis was performed in line with recommendations from PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and MOOSE (Meta-Analysis Of Observational Studies in Epidemiology) [23, 24]. Review Manager (RevMan) Version 5.3, STATA Data Analysis and Statistical Software Version 14 and WinPepi Version 11:32 were used for the analyses. A random-effects model was used to aggregate the data; the odds ratio (OR) was used as the summary statistic for binary data. Studies reporting zero events for both OPCAB and BH groups were excluded from meta-analysis.
To quantitatively assess data validity and heterogeneity, subgroup analysis was performed for (i) studies with a large sample size (≥100) in each cohort, (ii) studies with a high degree of matching between OPCAB and BH groups (matching score ≥12) and (iii) studies with a quality score ≥9.
Quality assessment
Each study was assessed in two ways using (i) a matching criteria score, and (ii) a quality assessment score based on a modified Newcastle–Ottawa scale [25]. The matching score was defined for each study by attributing one point for each preoperative characteristic for which there was no statistically significant difference between the OPCAB and ONCAB groups (Supplementary material, Table S1). The maximum matching score was 36 and the median score was 12. Studies achieving a score equal to or greater than 12 points were considered as highly matched studies and were analysed as subgroup. The modified Newcastle–Ottawa quality score was defined for each study using the subgroup criteria of ‘selection’, ‘comparability’ and ‘outcome assessment’, and attributing stars to each study for these criteria (Supplementary material, Table S2). The maximum quality assessment score was 15 and the median score was 9. Studies achieving a score equal to or greater than 9 points were considered as high quality and were analysed as a subgroup.
Meta-regression
To investigate whether a degree of clinical heterogeneity exists as a result of differing preoperative risk profiles between OPCAB and BH patients, meta-regression was performed to determine the impact of age, redo surgery, urgency of surgical intervention and EuroSCORE on postoperative mortality and MI outcomes. Results were considered statistically significant where P < 0.05.
RESULTS
Twelve observational studies were identified by systematic search to fulfil the inclusion criteria (Fig. 1) [11–22]. Studies were excluded on evaluation of methodology where there was no comparison of the two techniques. These studies included 3745 patients, 2894 of whom underwent OPCAB and 851 underwent BH. The search and the data extraction were performed by two reviewers (Amir H. Sepehripour and Amna Suliman). The data extracted for both study groups included preoperative characteristics, inclusion and exclusion criteria, matching criteria, quality assessment criteria, 30-day mortality, incidence of MI, the degree of completeness of revascularization and the mean number of bypass grafts performed. The two reviewers followed a predefined protocol and ultimately reached complete agreement for the search and data extraction.
Primary outcomes
Mortality (30 days)
Thirty-day mortality was 2.7% in the OPCAB group and 4.2% in the BH group. This difference was not statistically significant using a random-effects model [OR 1.5; 95% confidence interval (CI): 0.94–2.38; Z = 1.71, P = 0.09] (Fig. 2A). This analysis was based on eight studies [11, 12, 16–21]; two studies [13, 14] had not reported 30-day mortality and two studies [15, 22] had reported zero events for both OPCAB and BH groups and were thus excluded. No significant statistical heterogeneity was found between the studies.
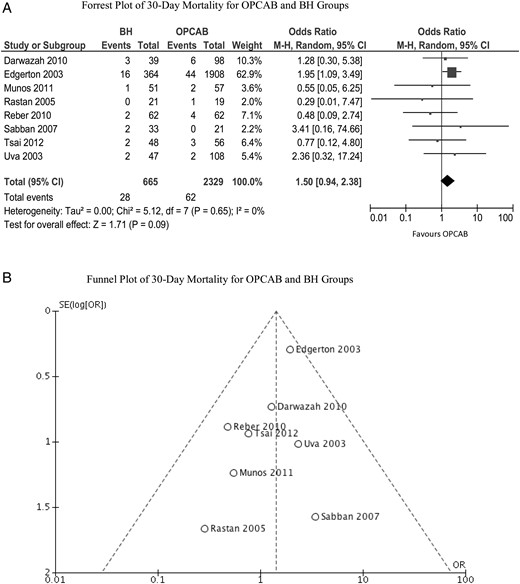
(A) Forrest plot of 30-day mortality for OPCAB and BH groups. (B) Funnel plot of 30-day mortality for OPCAB and BH groups. BH: beating heart; OPCAB: off-pump coronary artery bypass; CI: confidence interval; OR: odds ratio; SD: standard deviation; M-H: Mantel-Haenszel.
Myocardial infarction
The incidence of MI was 1.3% in the OPCAB group and 2.1% in the BH group. This difference was not significant using a random-effects model (OR 1.08; 95% CI: 0.52–2.22; Z = 0.2, P = 0.84) (Fig. 3A). The incidence was reported by seven studies [11, 12, 15–17, 21, 22]; however, one study [22] had reported zero events for both OPCAB and BH groups and was excluded. No significant statistical heterogeneity was found between the studies.
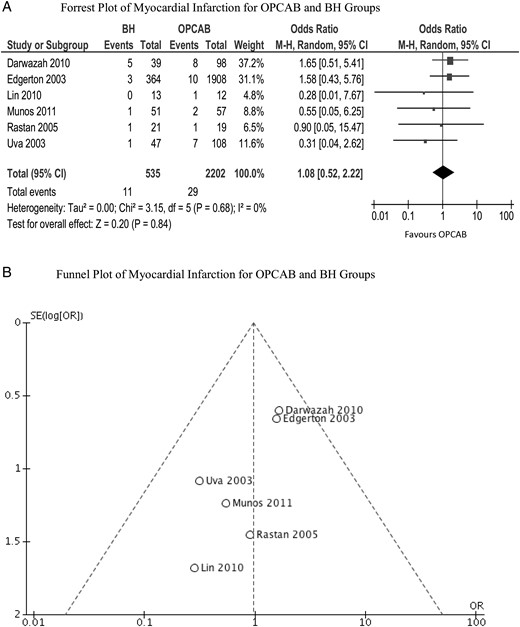
(A) Forrest plot of myocardial infarction for OPCAB and BH groups. (B) Funnel plot of myocardial infarction for OPCAB and BH groups. BH: beating heart; OPCAB: off-pump coronary artery bypass; CI: confidence interval; OR: odds ratio; SD: standard deviation; M-H: Mantel-Haenszel.
Composite major adverse cardiovascular and cerebrovascular adverse events
Composite outcome of MACCE was 4.6% in the OPCAB group and 7.9% in the BH group. This difference was not statistically significant using a random-effects model (OR 1.52; 95% CI: 0.97–2.38; Z = 1.85, P = 0.06) (Fig. 4A). This analysis was based on four studies [11, 12, 16, 21] which had reported outcomes for 30-day morality and stroke and MI. No significant statistical heterogeneity was found between the studies.
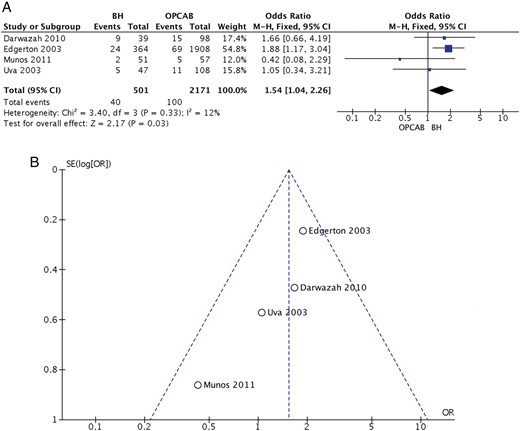
(A) Forrest plot of composite MACCE for OPCAB and BH groups. (B) Funnel plot of composite MACCE for OPCAB and BH groups. BH: beating heart; OPCAB: off-pump coronary artery bypass; CI: confidence interval; OR: odds ratio; SD: standard deviation; M-H: Mantel-Haenszel.
Complete revascularization
Complete revascularization was performed in 74% of the OPCAB group and 92% of the BH group. This increase in complete revascularization with BH was statistically significant using a random-effects model (OR 3.14; 95% CI: 1.78–5.57; Z = 3.93, P < 0.0001) (Fig. 5). The completeness of revascularization was reported by six studies [11, 15–18, 20]; however, one study [15] had reported 100% revascularization for both groups and was excluded from the analysis. No significant statistical heterogeneity was found between the studies.

Complete revascularization for OPCAB and BH groups. BH: beating heart; OPCAB: off-pump coronary artery bypass; CI: confidence interval; OR: odds ratio; M-H: Mantel-Haenszel.
Mean number of grafts
The mean number of grafts performed was 2.4 in the OPCAB group and 3.0 in the BH group. This increase in the number of grafts in the BH group was statistically significant using a random-effects model (weighted mean difference 0.52; 95% CI: 0.30–0.74; Z = 4.64, P < 0.0001) (Fig. 6A). The mean number of grafts was reported by 11 studies [11–13, 15–22]. Significant heterogeneity was observed between the studies (I2 = 82%).
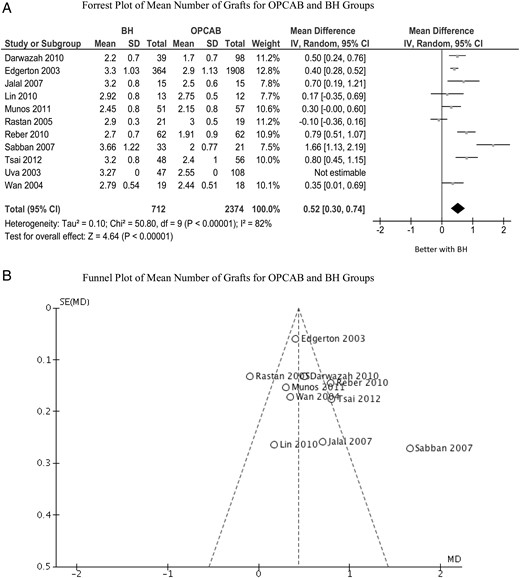
(A) Forrest plot of mean number of grafts for OPCAB and BH groups. (B) Funnel plot of mean number of grafts for OPCAB and BH groups. SD: standard deviation; CI: confidence interval; OR: odds ratio; BH: beating heart; OPCAB: off-pump coronary artery bypass. IV: inverse variance.
Subgroup analysis
Sample size
Seven studies had a large sample size (≥100) in each cohort and were included in this subgroup analysis [11, 12, 14, 16, 18, 20, 21].
Thirty-day mortality was 2.7% in the OPCAB group and 4.3% in the BH group. This reduction in mortality with OPCAB was not statistically significant (OR 1.52; 95% CI: 0.95–2.44; Z = 1.73, P = 0.08).
The incidence of MI was 1.2% in the OPCAB group and 2.0% in the BH group. This difference was not statistically significant (OR 1.17; 95% CI: 0.54–2.53; Z = 0.41, P = 0.68).
The incidence of composite MACCE was 4.6% in the OPCAB group and 7.9% in the BH group. This difference was not statistically significant using a random-effects model (OR 1.52; 95% CI: 0.97–2.38; Z = 1.85, P = 0.06).
Complete revascularization was performed in 71% in the OPCAB group and in 91% in the BH group. This increase was statistically significant (OR 3.13; 95% CI: 1.75–5.60; Z = 3.86, P < 0.0001).
The mean number of grafts performed was 2.3 in the OPCAB group and 2.9 in the BH group. This increase was statistically significant (OR 0.53; 95% CI: 0.35–0.72; Z = 5.75, P < 0.0001).
Matching score
Eight studies were attributed a matching score of 12 or greater and were included in this subgroup analysis [11, 12, 14, 16, 18–21].
Thirty-day mortality was 2.6% in the OPCAB group and 4.3% in the BH group. This reduction in mortality with OPCAB was not statistically significant (OR 1.55; 95% CI: 0.97–2.47; Z = 1.83, P = 0.07).
The incidence of MI was 1.2% in the OPCAB group and 2.0% in the BH group. This difference was not statistically significant (OR 1.17; 95% CI: 0.54–2.53; Z = 0.41, P = 0.68).
The incidence of composite MACCE was 4.6% in the OPCAB group and 7.9% in the BH group. This difference was not statistically significant using a random-effects model (OR 1.52; 95% CI: 0.97–2.38; Z = 1.85, P = 0.06).
Complete revascularization was performed in 71% in the OPCAB group and in 91% in the BH group. This increase was statistically significant (OR 3.13; 95% CI: 1.75–5.60; Z = 3.86, P < 0.0001).
The mean number of grafts performed was 2.2 in the OPCAB group and 3.0 in the BH group. This increase was statistically significant (OR 0.68; 95% CI: 0.41–0.94; Z = 4.99, P < 0.0001).
Quality score
Eleven studies were attributed a matching score of 9 or greater and were included in this subgroup analysis [11–17, 19–22].
Thirty-day mortality was 2.6% in the OPCAB group and 4.3% in the BH group. This reduction in mortality with OPCAB was not statistically significant (OR 1.63; 95% CI: 1.01–2.64; Z = 2.0, P = 0.05).
The incidence of MI was 1.3% in the OPCAB group and 2.1% in the BH group. This difference was not statistically significant (OR 1.08; 95% CI: 0.52–2.22; Z = 0.2, P = 0.84).
The incidence of composite MACCE was 4.6% in the OPCAB group and 7.9% in the BH group. This difference was not statistically significant using a random-effects model (OR 1.52; 95% CI: 0.97–2.38; Z = 1.85, P = 0.06).
Complete revascularization was performed in 74% in the OPCAB group and in 91% in the BH group. This increase was statistically significant (OR 2.78; 95% CI: 1.45–5.36; Z = 3.06, P < 0.01).
The mean number of grafts performed was 2.4 in the OPCAB group and 3.0 in the BH group. This increase was statistically significant (OR 0.49; 95% CI: 0.26–0.72; Z = 4.1, P < 0.0001).
Meta-regression
Meta-regression revealed that preoperative age (mortality P = 0.414; MI P = 0.635), redo surgery (mortality P = 0.342; MI P = 0.599), urgent/emergent procedure status (mortality P = 0.377; MI P = 0.599) and EuroSCORE (mortality P = 0.937; MI P = 0.536) did not significantly affect the incidence of 30-day mortality or postoperative MI.
Power calculation
A power calculation was performed using the composite MACCE primary outcome group, in which the total number of included patients in both groups was 2672. At 90% power, to detect a 0.05% level of significance, 2378 subjects are required. This demonstrates that this meta-analysis is appropriately powered to detect changes between the two groups.
DISCUSSION
The results of this meta-analysis demonstrate that myocardial revascularization using the on-pump beating heart (BH) technique is associated with a slightly higher, although a non-significant rate of 30-day mortality, MI and composite MACCE outcome. There is, however, a significantly higher rate of complete revascularization and mean number of bypass grafts performed with the BH technique. These observed effects remained consistent in the subgroup analysis of large sample size, high matching score and high quality score studies. No significant statistical heterogeneity was observed in the analysis of 30-day mortality, MI, composite MACCE and completeness of revascularization; however, there was statistical heterogeneity in the analysis of the mean number of grafts (this is not surprising in meta-analytical surgical studies for continuous outcomes of interest). Clinical heterogeneity was observed in the preoperative demographic data with regard to (i) mean age, (ii) redo surgery, (iii) urgent/emergent surgery, (iv) EuroSCORE. The influence of these preoperative demographics on postoperative outcomes was analysed using meta-regression; however, these outcomes were not found to significantly impact on either 30-day mortality or postoperative MI although this can be due to the low number of studies available for meta-regression affecting its statistical power. A large variation in study size was observed, with the Edgerton study [12] notably larger than the rest. Risk of publication bias was assessed by visual inspection of funnel plots in addition to statistical estimation with Egger's test for small study effects, both performed for the analyses in which this study was included (30-day mortality, incidence of MI, composite MACCE and the mean number of grafts) (Figs 2B, 3B, 4B and 6B). These plots demonstrated the Edgerton study not to be an outlier in the above analyses. The Egger's test gave an overall non-significant value (P = 0.101) for 30-day mortality, a non-significant value (P = 0.344) for the mean number of grafts and a significant value (P = 0.039) for the incidence of MI; however, there was no heterogeneity in the MI outcome.
Arrested heart on-pump surgery still remains the conventional technique for coronary artery bypass surgery. It is widely considered as the safest and technically easiest technique of myocardial revascularization being very amenable to training. There are, however, major disadvantages with the technique and these include the profound systemic inflammatory response to cardiopulmonary bypass, aortic cross-clamping, end-organ malperfusion and damage, myocardial protection issues and possible consequences of hypothermia. These compromises of a technique, which is supposed to provide the safest and easiest technique of coronary artery surgery, have led some to revert to off-pump surgery on the beating heart. Numerous randomized trials, systematic reviews and meta-analyses have compared the effects and outcomes of the two techniques, and these studies themselves have received much criticism regarding their conduct [1–3, 5, 26–30]. Off-pump surgery has been demonstrated to be associated with lower mortality (at least in the short-term) and lower major adverse events and morbidity, especially in the higher risk patient population, where the deleterious risk of ONCAB may be more pronounced [4, 9, 30]. These benefits are quite expected, given the avoidance of the systemic inflammatory response of cardiopulmonary bypass and the associated coagulopathy, the relative absence of end-organ malperfusion and damage, the avoidance of aortic cross-clamping, thereby minimizing embolization and myocardial ischaemia, further reduction of myocardial ischaemia with the use of intracoronary shunts and maintenance of normothermia throughout the procedure. The significant criticism aimed at the OPCAB technique has been generally two-fold: firstly, regarding the effects of emergency conversion to the ONCAB technique and its significant impact on mortality and morbidity [10]; secondly, regarding the relatively lower completeness of revascularization that is achieved [1–3, 6, 26, 27]. It is thus far unclear what impact the latter has on the mid- and long-term survival following OPCAB surgery.
The combination of the factors discussed above heralds the potential for the development of a hybrid technique of the two, whereby safe and complete revascularization can be performed while minimizing the detrimental effects of the conventional technique of non-beating heart on-pump surgery. The on-pump beating heart technique provides easier and safer access to distal posterior and lateral coronary territories in comparison with the OPCAB technique, allowing more complete myocardial revascularization. Additionally, while the deleterious effects of CPB are present, the potentially more damaging effects of aortic cross-clamping and myocardial ischaemia are minimized.
The results of this study constitute the higher level of evidence supporting consistently what has already been observed with the two techniques. The lower short-term mortality rate of OPCAB has been well documented in retrospective analyses, especially in the high-risk patient population, and it is not surprising that we have demonstrated a marginally lower rate of mortality using this technique. It is very important however, to consider that, as previously mentioned, the long-term survival following OPCAB has yet to be demonstrated, especially given the higher observed rates of incomplete revascularization. It is also important to note that while it is the higher risk patient population that is at most benefit from OPCAB, the mean EuroSCORE was in fact significantly higher in the BH group (8.6 vs 7.5%, P < 0.01) (independent t-test). In keeping with our expectations of the two techniques, we demonstrated a significantly higher number of grafts performed per patient in the BH group and, therefore, a significantly higher rate of complete revascularization with this technique is observed. The stability and safety provided by CPB allows far better access to distal coronary territories, thereby facilitating complete revascularization.
CONCLUSIONS
On-pump beating heart coronary artery bypass surgery allows a significantly higher number of grafts to be performed, thereby providing significantly higher rates of complete revascularization in comparison with off-pump coronary artery bypass surgery which is an important consideration for the quality control process of multivessel revascularization. The on-pump beating heart technique does however result in a slightly higher rate of 30-day mortality, MI and the composite outcome of MACCE (including 30-day mortality, stroke and MI). It is extremely important to highlight that these results are based on short-term results for MACCE and that they do need to be taken into consideration alongside the risk profile of patients undergoing the on-pump beating heart technique as well as longer term survival figures, in which the effects of greater complete revascularization may be reflected. It is most certain that these longer term survival and morbidity figures are lacking for both techniques. The theory behind the beneficial effects of the beating heart technique is physiologically sound, and it would not at all be surprising, that, with the benefit of longer term data, the outcome profile of the beating heart technique will prove to be far more favourable than we have been able to demonstrate here. It does, however, remain to be said that more studies are certainly required to reliably compare the cost burden of the two techniques. A randomized, controlled trial comparing the two techniques is complex, raising ethical concerns and is prone to bias due to the crossover effect in case of conversion and learning curve considerations from the off-pump to on-pump technique. Conversion and its established relationship to mortality may violate the assumption of clinical equipoise between the two trial arms. As previously mentioned, this study is limited by the lack of equal groups for the two techniques as well as the lack of longer term outcome measures to truly assess the impact of each technique on MACCE.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Conflict of interest: none declared.
REFERENCES




