-
PDF
- Split View
-
Views
-
Cite
Cite
María-Teresa González-López, Adrian Crucean, Anna Seale, Simon McGuirk, Truncus arteriosus, tricuspid atresia and partial anomalous pulmonary venous drainage: a unique form of univentricular heart, Interactive CardioVascular and Thoracic Surgery, Volume 21, Issue 2, August 2015, Pages 252–253, https://doi.org/10.1093/icvts/ivv118
Close - Share Icon Share
Abstract
We present the first reported case of truncus arteriosus, tricuspid atresia and partial anomalous pulmonary venous drainage into a retro-aortic innominate vein in a neonate in whom successful palliation was performed using a two-staged procedure. An early repair after presentation along with a re-routing of anomalous pulmonary venous drainage at the time of the second stage should be undertaken to optimize the patient's haemodynamic status prior to a Fontan completion.
BACKGROUND
The first successful surgical palliation of tricuspid atresia and common arterial trunk (CAT) was described by Sreeram in 1991 [1]. To date, only a few cases have been reported [2, 3]. The association with anomalies of the pulmonary venous return has not been described before. We present the first reported case of these three concomitant cardiac defects in a neonate who underwent successful palliation.
CASE REPORT
A neonate with antenatal diagnosis of tricuspid atresia, hypoplastic right ventricle (RV), ventricular septal defect and type I CAT was born at term and the echocardiogram confirmed the previous diagnosis. There was normal atrial arrangement, tricuspid atresia and a CAT arising from the hypoplastic RV (Fig. 1). The main pulmonary trunk branched off posteriorly from the CAT and divided into good-sized branch pulmonary arteries (PAs). The truncal valve was trileaflet with no stenosis/regurgitation. The left upper pulmonary vein (LUPV) (unobstructed) appeared to drain into a retro-aortic innominate vein.
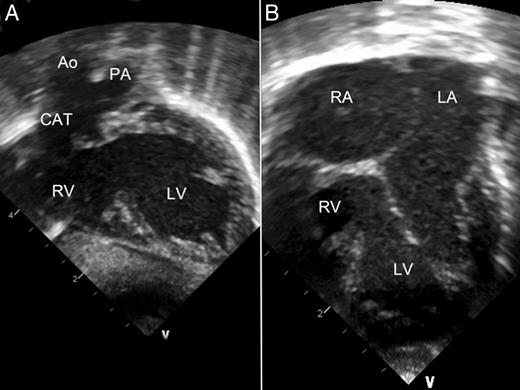
Preoperative 2D echocardiography. (A) Long-axis view. Hypoplastic RV and PA arising from the posterior aspect of the CAT. (B) Four-chamber view. Normal atrial arrangement is noted. Ao: aorta; CAT: common arterial trunk; LA: left atrium; LV: left ventricle; PA: pulmonary artery; RA: right atrium; RV: right ventricle.
Following birth, he continued to over-circulate and was taken to the operation theatre the next day. He underwent a right modified 3.5-mm Blalock–Taussig (BT) shunt, atrial septectomy and disconnection of the PAs from the trunk (bypass time 48 min). He had an uneventful recovery and was discharged on postoperative day 11.
At the 5-month follow-up, a computed tomography angiogram confirmed the LUPV draining into the retro-aortic innominate vein (Fig. 2). A mean PA pressure of 12 mmHg was confirmed by the haemodynamic study. He underwent the second stage of the palliation. The anomalous LUPV was ligated at its connection with the retro-aortic innominate vein and then pulled through a window in the pericardium below the phrenic nerve. The back wall of the LUPV was connected to the left atrial appendage and its anterior surface was incised longitudinally and the resulting defect was hooded over with a patch of homograft sewn in. After cooling the patient to 18°C, a right bidirectional cavopulmonary shunt and central pulmonary arterioplasty were performed (bypass time 83 min). The patency of the pulmonary veins draining into the left atrium was confirmed by echocardiography and he was discharged on postoperative day 10. At the 16-month follow-up, he remains asymptomatic, awaiting the third stage of palliation.
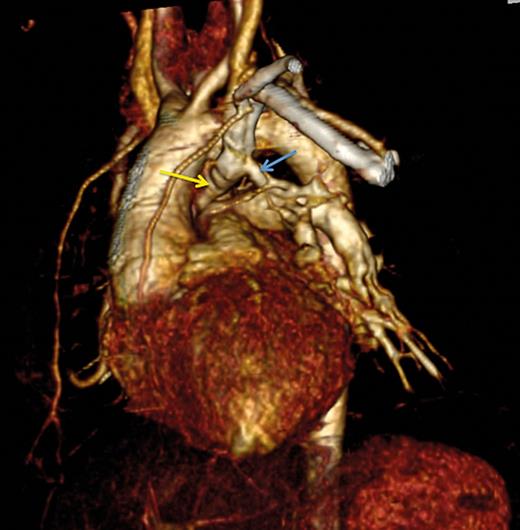
Three-dimensional computed tomography scan. The 3-mm left upper pulmonary vein (blue arrow) draining into the retro-aortic innominate vein (yellow arrow).
COMMENT
An accurate diagnosis of this unique form of congenital heart defect is mandatory for an early treatment. Initially, in our case the anatomy was delineated on echocardiography; however, if any features are unclear, further imaging with computed tomography or cardiac magnetic resonance is required.
We recommend an early repair after presentation to reduce the pulmonary vascular morbidity, along with a source of pulmonary blood flow. A primary separation of the PAs from the aorta and placement of a BT shunt would be an optimal first-stage palliation in this scenario, although a RV-PA shunt (Sano type) as an approach for the management of coexistent tricuspid atresia and CAT has also been described with varying success [4]. Despite a lack of consensus due to the extremely uncommon combination, we demonstrate that successful treatment of this condition can be undertaken using a BT shunt as primary palliation.
We also suggest that repair of the anomalous pulmonary venous drainage should be undertaken at the time of the second stage to avoid excessive blood flow into the lungs and to optimally manage cardiac output. In addition, this management would optimize the haemodynamics profile prior to Fontan completion and it may be essential to improve outcomes.
Conflict of interest: none declared.
REFERENCES




