-
PDF
- Split View
-
Views
-
Cite
Cite
Alan G Nyitray, Ferenc Bagyinszky, Michael W Ross, Axel J Schmidt, Lack of HIV testing and dissatisfaction with HIV testing and counselling among men having sex with men in Hungary, European Journal of Public Health, Volume 28, Issue 4, August 2018, Pages 713–720, https://doi.org/10.1093/eurpub/ckx200
Close - Share Icon Share
Abstract
Using data from a large internet-based survey of European men having sex with men (MSM), we assessed factors associated with HIV testing and reasons for dissatisfaction with HIV testing and counselling among Hungarian MSM.
A total of 2052 Hungarian MSM provided evaluable data for the European MSM Internet Survey (EMIS) in 2010. χ2 tests and Poisson regression with a robust variance estimator were used to assess factors associated with HIV testing and dissatisfaction with HIV testing and counselling.
A total of 42.1% of MSM reported never being testing for HIV. Over one-half of men (54.1%) who reported condomless anal intercourse (CAI) in the prior 12 months with a person of unknown or sero-discordant HIV status reported no lifetime HIV testing. The factor most strongly associated with dissatisfaction with HIV testing and counselling was test site with increased dissatisfaction with inpatient hospital settings vs. community-based organizations. Both lack of HIV testing and dissatisfaction with testing were independently associated with MSM who reported that no one, or only a few people, knew they were attracted to men.
Lack of HIV testing was strongly associated with CAI. MSM reported that community-based organizations better supported confidentiality and were more respectful during HIV testing.
Introduction
Targeting populations at highest risk for HIV infection for early detection of HIV through testing and counselling activities remains a corner stone of the public health response to HIV.1,2 HIV testing is important for a number of reasons including that inadequate counselling and testing activities may lead to increased transmission;3 however, HIV testing rates remain suboptimal throughout Europe although rates are heterogeneous by country4 with particularly low rates in some eastern and central European countries.5,6 These suboptimal testing rates occur in the wake of increasing HIV and sexually transmitted infection (STI) incidence in a time of increased political, economic and social instability in the region.7
In Hungary, where unprotected sex between men is the main risk factor for HIV infection,8 42% of gay, bisexual and other men who have sex with men (MSM) report never having tested for HIV.4 This proportion is high compared to Western European countries but comparable to other Central-Eastern European countries.4 Reasons for lack of HIV and STI testing and treatment may include a lack of public resources,9 age, sexual identity4 and stigmatization.10–12 While a qualitative study explored provision of HIV services among 27 MSM in Budapest,13 factors associated with a lack of testing and reasons for dissatisfaction with HIV testing and counselling in Hungary have not been reported to our knowledge.
The European MSM Internet Survey14,15 collected evaluable data from 174 209 MSM in 2010, including data regarding demographics, sexual behaviour and HIV testing.4 Of these, 2067 men were living in Hungary and prior EMIS publications had not focused on these men. Our objective was to assess HIV testing behaviours and reasons for dissatisfaction with HIV testing among Hungarian MSM.
Methods
Recruitment
A detailed description of the EMIS methodology has been previously published.4,14 In brief, a total of 174 209 MSM recruited in 38 European countries met the inclusion criteria. Among inclusion criteria were men living in Europe who were at least the age of consent in their country of residence, and men with an attraction to men or a history of sex with men. The data were collected between June and August 2010.
Hungarian men were primarily recruited through gay social media (e.g. 65% PlanetRomeo). No incentive was provided for survey completion. All men completed an informed consent statement before the survey, and all EMIS procedures were approved by the Research Ethics Committee of the University of Portsmouth, UK.
Measures
The current analysis assessed survey data from Hungarian MSM dealing with demographics, sexual identity, sexual behaviour, HIV and STI testing behaviour, satisfaction with HIV test counselling, HIV/STI knowledge, and substance use behaviour. Age was categorized using 5-year increments through age 44. Ages 45–76 years were collapsed into one category due to sparse data. Country of birth and place of residence were dichotomized (i.e. Hungary or not, and Budapest or rest of Hungary, respectively). Relationship status asked men about a ‘steady relationship’ with a man or woman with reference to husband/wife or boyfriend/girlfriend to distinguish these relationships from casual or non-steady regular sex partners.
The place of the last HIV test was asked using the following options: ‘At an HIV testing service (i.e. not in a hospital or clinic),’ ‘In a bar/pub, club or sauna,’ or ‘Mobile medical unit’ (categorized as ‘community-based organization’); ‘General Practitioner/family doctor,’ or ‘A doctor in private practice’ (both categorized as ‘physician’s office’); ‘At a hospital or clinic as an out-patient’ (categorized as ‘outpatient clinic/hospital’); ‘At a hospital as an in-patient’ (categorized as ‘inpatient clinic/hospital’); or ‘At a blood bank, while donating blood,’ ‘I used a home testing kit,’ or ‘Elsewhere’ (all categorized as ‘other’). For creation of figure 1, the outpatient and inpatient clinic/hospital categories were combined as ‘Hospital or clinic.’
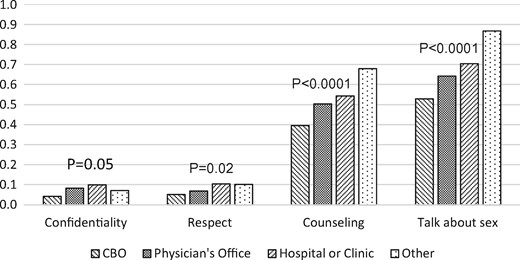
Percent dissatisfied with confidentiality, respect, counselling, and ability to talk about sex during HIV testing, by HIV test site. Note, “CBO” (community-based organization) includes HIV testing services that are not in a hospital or clinic, HIV testing in a bar/pub, club or sauna, or HIV testing in a mobile medical unit. “Hospital or Clinic” was created by combining inpatient and outpatient hospital/clinic test site categories. “Other” includes HIV testing at a blood bank, HIV testing using a home kit, or HIV testing “Elsewhere”
Men were asked to describe themselves as ‘gay or homosexual,’ ‘bisexual,’ ‘straight or heterosexual,’ ‘any other term,’ or ‘I don’t usually use a term.’ To assess factors associated with dissatisfaction with HIV counselling and testing, ‘straight or heterosexual,’ and ‘any other term,’ were combined due to sparse data. Men’s openness about their sexual identity was measured by asking men to report how many people knew about their identity, i.e. only a few or none, or more than a few.
Risk for HIV transmission was dichotomized by asking men if there had or had not been condomless anal intercourse with a person in the last 12 months whom they perceived as HIV discordant or HIV status unknown.
Knowledge of HIV, STIs and post-exposure prophylaxis was assessed by presenting men with true statements about these topics and then asking men to acknowledge if they already knew or did not know the information. Knowledge variables were categorized as ‘0–50% correct,’ ‘51–75% correct,’ and ‘76–100% correct.’ Substance use was assessed by dichotomous variables asking about use (no/yes) of a particular substance in a specified time period.
Analytical methods
Survey measures were stratified by HIV test result and lack of HIV testing with differences assessed by χ2 tests. Differences by test site regarding reasons for dissatisfaction with HIV testing and counselling were assessed with χ2 tests.
In order to determine factors associated with never getting an HIV test and factors associated with dissatisfaction with HIV testing and counselling, we undertook two rounds of modelling using Poisson regression with a robust variance estimator to estimate prevalence ratios.16 Factors chosen for multivariable analysis in each round were significant in univariable analysis (P < 0.20). In addition, known confounders (i.e. age,17 birth country, and residence) were retained in all multivariable analyses.18 For each multivariable analyses, variables were removed one-by-one until only statistically significant variables remained. A variable was considered statistically significant if the 95% CIs for any of its prevalence ratios excluded unity.
Directed acyclic graphs (DAGs)19 indicated that no variables significant in univariable analysis should be excluded from modelling factors associated with non-HIV testing.18 In addition to confounders, factors included in multivariable analysis for the outcome of non-HIV testers were relationship status, sexual identity, openness about sexual identity, sexual happiness, 12-month HIV transmission risk, access to free or affordable HIV testing, knowledge about HIV, STIs, and post-exposure prophylaxis, use of nitrate inhalants in the last four weeks, use of benzodiazepines in the last 12 months, use of cannabis in the last 12 months, and use of party-n-play drugs in the last 12 months.
The outcome of dissatisfaction with HIV testing and counselling was created from four variables: Dissatisfaction with or lack of counselling when testing for HIV, dissatisfaction with confidentiality when testing, dissatisfaction with respect when testing, and ability to talk about sexual behaviour when testing for HIV. In addition to confounders, factors included in multivariable analysis for the outcome of dissatisfaction with HIV testing and counselling were relationship status, sexual identity, openness about sexual identity, sexual happiness, test site, knowledge about HIV, STIs, and post-exposure prophylaxis, and use of nitrate inhalants in the last four weeks. DAGs19 indicated that access to free/affordable HIV testing and self-reported STI testing in the last 12 months, while significant in univariable analysis, may be intermediate variables to exclude from modelling;18 however, since multivariable modelling with these variables did not substantively change final model prevalence ratios, they were not excluded. Data were analysed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Of all MSM in Hungary providing evaluable surveys, 2052 provided data on HIV testing history (table 1). Their median age was 28 years (range, 15–76 years), 56.1% resided in Budapest, and 8.7% of men reported being born in another country.
Selected characteristics of Hungarian MSM stratified by HIV diagnosis and testing historya
| Variable . | n (%) . | |||
|---|---|---|---|---|
| Last HIV test negative n = 1124 . | Last HIV test positive n = 65 . | Never tested n = 863 . | Total n = 2052 . | |
| Age, yearsb | ||||
| 15–19 | 37 (3.3) | 0 (0.0) | 153 (17.7) | 190 (9.3) |
| 20–24 | 234 (20.8) | 6 (9.2) | 238 (27.6) | 478 (23.3) |
| 25–29 | 296 (26.3) | 11 (16.9) | 189 (21.9) | 496 (24.2) |
| 30–34 | 272 (24.2) | 9 (13.9) | 137 (15.9) | 418 (20.4) |
| 35–39 | 132 (11.7) | 14 (21.5) | 60 (7.0) | 206 (10.0) |
| 40–44 | 76 (6.8) | 16 (24.6) | 38 (4.4) | 130 (6.3) |
| 45–76 | 77 (6.9) | 9 (13.9) | 48 (5.6) | 134 (6.5) |
| Median, range | 29, 16–68 | 37, 23–68 | 25, 15–76 | 28, 15–76 |
| Residenceb | ||||
| Budapest | 752 (66.9) | 49 (75.4) | 350 (40.6) | 1151 (56.1) |
| Rest of Hungary | 360 (32.0) | 14 (21.5) | 507 (58.8) | 881 (42.9) |
| Missing | 12 (1.1) | 2 (3.1) | 6 (0.7) | 20 (1.0) |
| Born in Hungaryb | ||||
| No | 124 (11.0) | 12 (18.5) | 43 (5.0) | 179 (8.7) |
| Yes | 974 (86.7) | 52 (80.0) | 807 (93.5) | 1833 (89.3) |
| Missing | 26 (2.3) | 1 (1.5) | 13 (1.5) | 40 (2.0) |
| Relationship statusb | ||||
| Single | 534 (47.5) | 29 (44.6) | 494 (57.2) | 1057 (51.5) |
| Steady relationship with men | 526 (46.8) | 35 (53.9) | 265 (30.7) | 826 (40.3) |
| Steady relationship with women only | 53 (4.7) | 1 (1.5) | 93 (10.8) | 147 (7.2) |
| Missing | 4 (0.4) | 0 (0.0) | 6 (0.7) | 10 (0.5) |
| How do you think of yourself? | ||||
| Gay or homosexual | 902 (80.3) | 61 (93.9) | 518 (60.0) | 1481 (72.2) |
| Bisexual | 107 (9.5) | 1 (1.5) | 185 (21.4) | 293 (14.3) |
| Straight or heterosexual | 7 (0.6) | 0 (0.0) | 22 (2.6) | 29 (1.4) |
| Any other term | 6 (0.5) | 0 (0.0) | 13 (1.5) | 19 (0.9) |
| I don’t usually use a term | 101 (9.0) | 3 (4.6) | 124 (14.4) | 228 (11.1) |
| Missing | 1 (0.1) | 0 (0.0) | 1 (0.1) | 2 (0.1) |
| Outness: Of all the people you know, what proportion know you are attracted to men?b | ||||
| More than a few | 759 (67.5) | 55 (84.6) | 300 (34.8) | 1114 (54.3) |
| A few or none | 360 (32.0) | 10 (15.4) | 556 (64.4) | 926 (45.1) |
| Missing | 5 (0.4) | 0 (0.0) | 7 (0.8) | 12 (0.6) |
| Experience with anti-gay violence or intimidation in the last 12 months | ||||
| No violence | 670 (59.6) | 36 (55.4) | 484 (56.1) | 1190 (58.0) |
| Experience with violence or intimidation | 449 (40.0) | 29 (44.6) | 374 (43.3) | 852 (41.5) |
| Missing | 5 (0.4) | 0 (0.0) | 5 (0.6) | 10 (0.5) |
| Sexual happinessb | ||||
| No | 469 (41.7) | 24 (36.9) | 485 (56.2) | 978 (47.7) |
| Yes | 596 (53.0) | 32 (49.2) | 333 (38.6) | 961 (46.8) |
| Missing | 59 (5.3) | 9 (13.9) | 45 (5.2) | 113 (5.5) |
| 12-month HIV transmission riskb | ||||
| No CAI with HIV-unknown/discordant man | 849 (75.5) | 28 (43.1) | 474 (54.9) | 1351 (65.8) |
| CAI with HIV-unknown/discordant man | 232 (20.6) | 36 (55.4) | 316 (36.6) | 584 (28.5) |
| Missing | 43 (3.8) | 1 (1.5) | 73 (8.5) | 117 (5.7) |
| Location of last HIV test/HIV diagnosisb | ||||
| Community-based organization | 498 (44.3) | 21 (32.3) | 0 (0.0) | 519 (25.3) |
| Physician’s office | 119 (10.6) | 5 (7.7) | 0 (0.0) | 124 (6.0) |
| Outpatient clinic/hospital | 363 (32.3) | 29 (44.6) | 0 (0.0) | 392 (19.1) |
| Inpatient clinic/hospital | 13 (1.2) | 5 (7.7) | 0 (0.0) | 18 (0.9) |
| Other | 128 (11.4) | 3 (4.6) | 0 (0.0) | 131 (6.4) |
| Missing/Never tested | 3 (0.3) | 2 (3.1) | 863 (100.0) | 868 (42.3) |
| Dissatisfaction with or lack of counselling when testing for HIV (HIV testers only) | ||||
| Satisfied | 518 (46.1) | 31 (47.7) | 0 (0.0) | 549 (26.8) |
| Dissatisfied or no counselling | 488 (43.4) | 28 (43.1) | 0 (0.0) | 516 (25.2) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 118 (10.5) | 6 (9.2) | 0 (0.0) | 124 (6.0) |
| Dissatisfaction with confidentiality when testing for HIV (HIV testers only)b | ||||
| Satisfied | 991 (88.2) | 44 (67.7) | 0 (0.0) | 1035 (50.4) |
| Dissatisfied | 61 (5.4) | 14 (21.5) | 0 (0.0) | 75 (3.7) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 72 (6.4) | 7 (10.8) | 0 (0.0) | 79 (3.9) |
| Dissatisfaction with respect when testing for HIV (HIV testers only)b | ||||
| Satisfied | 1019 (90.7) | 43 (66.2) | 0 (0.0) | 1062 (51.8) |
| Dissatisfied | 69 (6.1) | 17 (26.2) | 0 (0.0) | 86 (4.2) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 36 (3.2) | 5 (7.7) | 0 (0.0) | 41 (2.0) |
| Ability to talk about sexual behaviour when testing for HIV (HIV testers only)b | ||||
| No | 712 (63.4) | 25 (38.5) | 0 (0.0) | 737 (35.9) |
| Yes | 324 (28.8) | 23 (35.4) | 0 (0.0) | 347 (16.9) |
| I don’t remember | 86 (7.7) | 15 (23.1) | 0 (0.0) | 101 (4.9) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 2 (0.2) | 2 (3.1) | 0 (0.0) | 4 (0.2) |
| Access to free or affordable STI testingb | ||||
| No | 260 (23.1) | 6 (9.2) | 379 (43.9) | 645 (31.4) |
| Yes | 860 (76.5) | 58 (89.2) | 480 (55.6) | 1398 (68.1) |
| Missing | 4 (0.4) | 1 (1.5) | 4 (0.5) | 9 (0.4) |
| Access to free or affordable HIV testing (HIV negative or untested only)b | ||||
| No | 41 (3.7) | 0 (0.0) | 227 (26.3) | 268 (13.1) |
| Yes | 1077 (95.8) | 0 (0.0) | 636 (73.7) | 1713 (83.5) |
| Missing | 6 (0.5) | 65 (100.0) | 0 (0.0) | 71 (3.5) |
| Overall scores on basic knowledge about HIV, STIs, and post-exposure prophylaxisb | ||||
| 0–50% correct | 120 (10.7) | 3 (4.6) | 232 (26.9) | 355 (17.3) |
| 51–75% correct | 650 (57.8) | 17 (26.2) | 468 (54.2) | 1135 (55.5) |
| 76–100% correct | 354 (31.5) | 45 (69.2) | 163 (18.9) | 562 (27.4) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| STI testing in the prior 12 monthsb | ||||
| No STI test | 668 (59.4) | 21 (32.3) | 813 (94.2) | 1502 (73.2) |
| STI tested | 415 (36.9) | 43 (66.2) | 23 (2.7) | 481 (23.4) |
| Missing | 41 (3.7) | 1 (1.5) | 27 (3.1) | 69 (3.4) |
| Self-reported syphilis in last 12 months among those with a blood test | ||||
| Negative | 368 (32.7) | 28 (43.1) | 12 (1.4) | 408 (19.9) |
| Positive | 21 (1.9) | 12 (18.5) | 2 (0.2) | 35 (1.7) |
| No blood test in 12 months | 690 (61.4) | 24 (36.9) | 822 (95.3) | 1536 (74.9) |
| Missing | 45 (4.0) | 1 (1.5) | 27 (3.1) | 73 (3.6) |
| Self-reported anogenital warts in last 12 months among those with a penile/anal inspectionb | ||||
| No | 85 (7.6) | 11 (16.9) | 6 (0.7) | 102 (5.0) |
| Yes | 7 (0.6) | 4 (6.2) | 0 (0.0) | 11 (0.5) |
| No penile/anal inspection in 12 months | 991 (88.2) | 49 (75.4) | 830 (96.2) | 1870 (91.1) |
| Missing | 41 (3.7) | 1 (1.5) | 27 (3.1) | 69 (3.4) |
| Hepatitis B vaccine needsb | ||||
| Immune or already vaccinated | 373 (33.2) | 23 (35.4) | 253 (29.3) | 649 (31.6) |
| Not immune and not fully vaccinated | 583 (51.9) | 37 (56.9) | 389 (45.1) | 1009 (49.2) |
| I don’t know/Missing | 168 (15.0) | 5 (7.7) | 221 (25.6) | 394 (19.2) |
| Use of nitrate inhalants in the last 4 weeksb | ||||
| No | 930 (82.7) | 30 (46.2) | 798 (92.5) | 1758 (85.7) |
| Yes | 184 (16.4) | 35 (53.9) | 59 (6.8) | 278 (13.6) |
| Missing | 10 (0.9) | 0 (0.0) | 6 (0.7) | 16 (0.8) |
| Use of benzodiazepines in the last 12 monthsb | ||||
| No | 919 (81.8) | 48 (73.9) | 759 (88.0) | 1726 (84.1) |
| Yes | 196 (17.4) | 14 (21.5) | 98 (11.4) | 308 15.0 |
| Missing | 9 (0.8) | 3 (4.6) | 6 (0.7) | 18 (0.9) |
| Use of cannabis in the last 12 monthsb | ||||
| No | 882 (78.5) | 47 (72.3) | 739 (85.6) | 1668 (81.3) |
| Yes | 231 (20.6) | 18 (27.7) | 119 (13.8) | 368 (17.9) |
| Missing | 11 (1.0) | 0 (0.0) | 5 (0.6) | 16 (0.8) |
| Use of party-n-play drugs in the last 12 monthsb,c | ||||
| No | 977 (86.9) | 46 (70.8) | 796 (92.2) | 1819 (88.7) |
| Yes | 136 (12.1) | 19 (29.2) | 62 (7.2) | 217 (10.6) |
| Missing | 11 (1.0) | 0 (0.0) | 5 (0.6) | 16 (0.8) |
| Variable . | n (%) . | |||
|---|---|---|---|---|
| Last HIV test negative n = 1124 . | Last HIV test positive n = 65 . | Never tested n = 863 . | Total n = 2052 . | |
| Age, yearsb | ||||
| 15–19 | 37 (3.3) | 0 (0.0) | 153 (17.7) | 190 (9.3) |
| 20–24 | 234 (20.8) | 6 (9.2) | 238 (27.6) | 478 (23.3) |
| 25–29 | 296 (26.3) | 11 (16.9) | 189 (21.9) | 496 (24.2) |
| 30–34 | 272 (24.2) | 9 (13.9) | 137 (15.9) | 418 (20.4) |
| 35–39 | 132 (11.7) | 14 (21.5) | 60 (7.0) | 206 (10.0) |
| 40–44 | 76 (6.8) | 16 (24.6) | 38 (4.4) | 130 (6.3) |
| 45–76 | 77 (6.9) | 9 (13.9) | 48 (5.6) | 134 (6.5) |
| Median, range | 29, 16–68 | 37, 23–68 | 25, 15–76 | 28, 15–76 |
| Residenceb | ||||
| Budapest | 752 (66.9) | 49 (75.4) | 350 (40.6) | 1151 (56.1) |
| Rest of Hungary | 360 (32.0) | 14 (21.5) | 507 (58.8) | 881 (42.9) |
| Missing | 12 (1.1) | 2 (3.1) | 6 (0.7) | 20 (1.0) |
| Born in Hungaryb | ||||
| No | 124 (11.0) | 12 (18.5) | 43 (5.0) | 179 (8.7) |
| Yes | 974 (86.7) | 52 (80.0) | 807 (93.5) | 1833 (89.3) |
| Missing | 26 (2.3) | 1 (1.5) | 13 (1.5) | 40 (2.0) |
| Relationship statusb | ||||
| Single | 534 (47.5) | 29 (44.6) | 494 (57.2) | 1057 (51.5) |
| Steady relationship with men | 526 (46.8) | 35 (53.9) | 265 (30.7) | 826 (40.3) |
| Steady relationship with women only | 53 (4.7) | 1 (1.5) | 93 (10.8) | 147 (7.2) |
| Missing | 4 (0.4) | 0 (0.0) | 6 (0.7) | 10 (0.5) |
| How do you think of yourself? | ||||
| Gay or homosexual | 902 (80.3) | 61 (93.9) | 518 (60.0) | 1481 (72.2) |
| Bisexual | 107 (9.5) | 1 (1.5) | 185 (21.4) | 293 (14.3) |
| Straight or heterosexual | 7 (0.6) | 0 (0.0) | 22 (2.6) | 29 (1.4) |
| Any other term | 6 (0.5) | 0 (0.0) | 13 (1.5) | 19 (0.9) |
| I don’t usually use a term | 101 (9.0) | 3 (4.6) | 124 (14.4) | 228 (11.1) |
| Missing | 1 (0.1) | 0 (0.0) | 1 (0.1) | 2 (0.1) |
| Outness: Of all the people you know, what proportion know you are attracted to men?b | ||||
| More than a few | 759 (67.5) | 55 (84.6) | 300 (34.8) | 1114 (54.3) |
| A few or none | 360 (32.0) | 10 (15.4) | 556 (64.4) | 926 (45.1) |
| Missing | 5 (0.4) | 0 (0.0) | 7 (0.8) | 12 (0.6) |
| Experience with anti-gay violence or intimidation in the last 12 months | ||||
| No violence | 670 (59.6) | 36 (55.4) | 484 (56.1) | 1190 (58.0) |
| Experience with violence or intimidation | 449 (40.0) | 29 (44.6) | 374 (43.3) | 852 (41.5) |
| Missing | 5 (0.4) | 0 (0.0) | 5 (0.6) | 10 (0.5) |
| Sexual happinessb | ||||
| No | 469 (41.7) | 24 (36.9) | 485 (56.2) | 978 (47.7) |
| Yes | 596 (53.0) | 32 (49.2) | 333 (38.6) | 961 (46.8) |
| Missing | 59 (5.3) | 9 (13.9) | 45 (5.2) | 113 (5.5) |
| 12-month HIV transmission riskb | ||||
| No CAI with HIV-unknown/discordant man | 849 (75.5) | 28 (43.1) | 474 (54.9) | 1351 (65.8) |
| CAI with HIV-unknown/discordant man | 232 (20.6) | 36 (55.4) | 316 (36.6) | 584 (28.5) |
| Missing | 43 (3.8) | 1 (1.5) | 73 (8.5) | 117 (5.7) |
| Location of last HIV test/HIV diagnosisb | ||||
| Community-based organization | 498 (44.3) | 21 (32.3) | 0 (0.0) | 519 (25.3) |
| Physician’s office | 119 (10.6) | 5 (7.7) | 0 (0.0) | 124 (6.0) |
| Outpatient clinic/hospital | 363 (32.3) | 29 (44.6) | 0 (0.0) | 392 (19.1) |
| Inpatient clinic/hospital | 13 (1.2) | 5 (7.7) | 0 (0.0) | 18 (0.9) |
| Other | 128 (11.4) | 3 (4.6) | 0 (0.0) | 131 (6.4) |
| Missing/Never tested | 3 (0.3) | 2 (3.1) | 863 (100.0) | 868 (42.3) |
| Dissatisfaction with or lack of counselling when testing for HIV (HIV testers only) | ||||
| Satisfied | 518 (46.1) | 31 (47.7) | 0 (0.0) | 549 (26.8) |
| Dissatisfied or no counselling | 488 (43.4) | 28 (43.1) | 0 (0.0) | 516 (25.2) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 118 (10.5) | 6 (9.2) | 0 (0.0) | 124 (6.0) |
| Dissatisfaction with confidentiality when testing for HIV (HIV testers only)b | ||||
| Satisfied | 991 (88.2) | 44 (67.7) | 0 (0.0) | 1035 (50.4) |
| Dissatisfied | 61 (5.4) | 14 (21.5) | 0 (0.0) | 75 (3.7) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 72 (6.4) | 7 (10.8) | 0 (0.0) | 79 (3.9) |
| Dissatisfaction with respect when testing for HIV (HIV testers only)b | ||||
| Satisfied | 1019 (90.7) | 43 (66.2) | 0 (0.0) | 1062 (51.8) |
| Dissatisfied | 69 (6.1) | 17 (26.2) | 0 (0.0) | 86 (4.2) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 36 (3.2) | 5 (7.7) | 0 (0.0) | 41 (2.0) |
| Ability to talk about sexual behaviour when testing for HIV (HIV testers only)b | ||||
| No | 712 (63.4) | 25 (38.5) | 0 (0.0) | 737 (35.9) |
| Yes | 324 (28.8) | 23 (35.4) | 0 (0.0) | 347 (16.9) |
| I don’t remember | 86 (7.7) | 15 (23.1) | 0 (0.0) | 101 (4.9) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 2 (0.2) | 2 (3.1) | 0 (0.0) | 4 (0.2) |
| Access to free or affordable STI testingb | ||||
| No | 260 (23.1) | 6 (9.2) | 379 (43.9) | 645 (31.4) |
| Yes | 860 (76.5) | 58 (89.2) | 480 (55.6) | 1398 (68.1) |
| Missing | 4 (0.4) | 1 (1.5) | 4 (0.5) | 9 (0.4) |
| Access to free or affordable HIV testing (HIV negative or untested only)b | ||||
| No | 41 (3.7) | 0 (0.0) | 227 (26.3) | 268 (13.1) |
| Yes | 1077 (95.8) | 0 (0.0) | 636 (73.7) | 1713 (83.5) |
| Missing | 6 (0.5) | 65 (100.0) | 0 (0.0) | 71 (3.5) |
| Overall scores on basic knowledge about HIV, STIs, and post-exposure prophylaxisb | ||||
| 0–50% correct | 120 (10.7) | 3 (4.6) | 232 (26.9) | 355 (17.3) |
| 51–75% correct | 650 (57.8) | 17 (26.2) | 468 (54.2) | 1135 (55.5) |
| 76–100% correct | 354 (31.5) | 45 (69.2) | 163 (18.9) | 562 (27.4) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| STI testing in the prior 12 monthsb | ||||
| No STI test | 668 (59.4) | 21 (32.3) | 813 (94.2) | 1502 (73.2) |
| STI tested | 415 (36.9) | 43 (66.2) | 23 (2.7) | 481 (23.4) |
| Missing | 41 (3.7) | 1 (1.5) | 27 (3.1) | 69 (3.4) |
| Self-reported syphilis in last 12 months among those with a blood test | ||||
| Negative | 368 (32.7) | 28 (43.1) | 12 (1.4) | 408 (19.9) |
| Positive | 21 (1.9) | 12 (18.5) | 2 (0.2) | 35 (1.7) |
| No blood test in 12 months | 690 (61.4) | 24 (36.9) | 822 (95.3) | 1536 (74.9) |
| Missing | 45 (4.0) | 1 (1.5) | 27 (3.1) | 73 (3.6) |
| Self-reported anogenital warts in last 12 months among those with a penile/anal inspectionb | ||||
| No | 85 (7.6) | 11 (16.9) | 6 (0.7) | 102 (5.0) |
| Yes | 7 (0.6) | 4 (6.2) | 0 (0.0) | 11 (0.5) |
| No penile/anal inspection in 12 months | 991 (88.2) | 49 (75.4) | 830 (96.2) | 1870 (91.1) |
| Missing | 41 (3.7) | 1 (1.5) | 27 (3.1) | 69 (3.4) |
| Hepatitis B vaccine needsb | ||||
| Immune or already vaccinated | 373 (33.2) | 23 (35.4) | 253 (29.3) | 649 (31.6) |
| Not immune and not fully vaccinated | 583 (51.9) | 37 (56.9) | 389 (45.1) | 1009 (49.2) |
| I don’t know/Missing | 168 (15.0) | 5 (7.7) | 221 (25.6) | 394 (19.2) |
| Use of nitrate inhalants in the last 4 weeksb | ||||
| No | 930 (82.7) | 30 (46.2) | 798 (92.5) | 1758 (85.7) |
| Yes | 184 (16.4) | 35 (53.9) | 59 (6.8) | 278 (13.6) |
| Missing | 10 (0.9) | 0 (0.0) | 6 (0.7) | 16 (0.8) |
| Use of benzodiazepines in the last 12 monthsb | ||||
| No | 919 (81.8) | 48 (73.9) | 759 (88.0) | 1726 (84.1) |
| Yes | 196 (17.4) | 14 (21.5) | 98 (11.4) | 308 15.0 |
| Missing | 9 (0.8) | 3 (4.6) | 6 (0.7) | 18 (0.9) |
| Use of cannabis in the last 12 monthsb | ||||
| No | 882 (78.5) | 47 (72.3) | 739 (85.6) | 1668 (81.3) |
| Yes | 231 (20.6) | 18 (27.7) | 119 (13.8) | 368 (17.9) |
| Missing | 11 (1.0) | 0 (0.0) | 5 (0.6) | 16 (0.8) |
| Use of party-n-play drugs in the last 12 monthsb,c | ||||
| No | 977 (86.9) | 46 (70.8) | 796 (92.2) | 1819 (88.7) |
| Yes | 136 (12.1) | 19 (29.2) | 62 (7.2) | 217 (10.6) |
| Missing | 11 (1.0) | 0 (0.0) | 5 (0.6) | 16 (0.8) |
Note: MSM: men having sex with men; CAI: condomless anal intercourse; STI: sexually transmitted infection.
The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey.
χ2P values <0.001; Hypothesis test does not include missing observations.
That is, Ecstasy/MDMA, amphetamines, crystal methamphetamine, mephedrone, GHB/GBL, ketamine, or cocaine.
Selected characteristics of Hungarian MSM stratified by HIV diagnosis and testing historya
| Variable . | n (%) . | |||
|---|---|---|---|---|
| Last HIV test negative n = 1124 . | Last HIV test positive n = 65 . | Never tested n = 863 . | Total n = 2052 . | |
| Age, yearsb | ||||
| 15–19 | 37 (3.3) | 0 (0.0) | 153 (17.7) | 190 (9.3) |
| 20–24 | 234 (20.8) | 6 (9.2) | 238 (27.6) | 478 (23.3) |
| 25–29 | 296 (26.3) | 11 (16.9) | 189 (21.9) | 496 (24.2) |
| 30–34 | 272 (24.2) | 9 (13.9) | 137 (15.9) | 418 (20.4) |
| 35–39 | 132 (11.7) | 14 (21.5) | 60 (7.0) | 206 (10.0) |
| 40–44 | 76 (6.8) | 16 (24.6) | 38 (4.4) | 130 (6.3) |
| 45–76 | 77 (6.9) | 9 (13.9) | 48 (5.6) | 134 (6.5) |
| Median, range | 29, 16–68 | 37, 23–68 | 25, 15–76 | 28, 15–76 |
| Residenceb | ||||
| Budapest | 752 (66.9) | 49 (75.4) | 350 (40.6) | 1151 (56.1) |
| Rest of Hungary | 360 (32.0) | 14 (21.5) | 507 (58.8) | 881 (42.9) |
| Missing | 12 (1.1) | 2 (3.1) | 6 (0.7) | 20 (1.0) |
| Born in Hungaryb | ||||
| No | 124 (11.0) | 12 (18.5) | 43 (5.0) | 179 (8.7) |
| Yes | 974 (86.7) | 52 (80.0) | 807 (93.5) | 1833 (89.3) |
| Missing | 26 (2.3) | 1 (1.5) | 13 (1.5) | 40 (2.0) |
| Relationship statusb | ||||
| Single | 534 (47.5) | 29 (44.6) | 494 (57.2) | 1057 (51.5) |
| Steady relationship with men | 526 (46.8) | 35 (53.9) | 265 (30.7) | 826 (40.3) |
| Steady relationship with women only | 53 (4.7) | 1 (1.5) | 93 (10.8) | 147 (7.2) |
| Missing | 4 (0.4) | 0 (0.0) | 6 (0.7) | 10 (0.5) |
| How do you think of yourself? | ||||
| Gay or homosexual | 902 (80.3) | 61 (93.9) | 518 (60.0) | 1481 (72.2) |
| Bisexual | 107 (9.5) | 1 (1.5) | 185 (21.4) | 293 (14.3) |
| Straight or heterosexual | 7 (0.6) | 0 (0.0) | 22 (2.6) | 29 (1.4) |
| Any other term | 6 (0.5) | 0 (0.0) | 13 (1.5) | 19 (0.9) |
| I don’t usually use a term | 101 (9.0) | 3 (4.6) | 124 (14.4) | 228 (11.1) |
| Missing | 1 (0.1) | 0 (0.0) | 1 (0.1) | 2 (0.1) |
| Outness: Of all the people you know, what proportion know you are attracted to men?b | ||||
| More than a few | 759 (67.5) | 55 (84.6) | 300 (34.8) | 1114 (54.3) |
| A few or none | 360 (32.0) | 10 (15.4) | 556 (64.4) | 926 (45.1) |
| Missing | 5 (0.4) | 0 (0.0) | 7 (0.8) | 12 (0.6) |
| Experience with anti-gay violence or intimidation in the last 12 months | ||||
| No violence | 670 (59.6) | 36 (55.4) | 484 (56.1) | 1190 (58.0) |
| Experience with violence or intimidation | 449 (40.0) | 29 (44.6) | 374 (43.3) | 852 (41.5) |
| Missing | 5 (0.4) | 0 (0.0) | 5 (0.6) | 10 (0.5) |
| Sexual happinessb | ||||
| No | 469 (41.7) | 24 (36.9) | 485 (56.2) | 978 (47.7) |
| Yes | 596 (53.0) | 32 (49.2) | 333 (38.6) | 961 (46.8) |
| Missing | 59 (5.3) | 9 (13.9) | 45 (5.2) | 113 (5.5) |
| 12-month HIV transmission riskb | ||||
| No CAI with HIV-unknown/discordant man | 849 (75.5) | 28 (43.1) | 474 (54.9) | 1351 (65.8) |
| CAI with HIV-unknown/discordant man | 232 (20.6) | 36 (55.4) | 316 (36.6) | 584 (28.5) |
| Missing | 43 (3.8) | 1 (1.5) | 73 (8.5) | 117 (5.7) |
| Location of last HIV test/HIV diagnosisb | ||||
| Community-based organization | 498 (44.3) | 21 (32.3) | 0 (0.0) | 519 (25.3) |
| Physician’s office | 119 (10.6) | 5 (7.7) | 0 (0.0) | 124 (6.0) |
| Outpatient clinic/hospital | 363 (32.3) | 29 (44.6) | 0 (0.0) | 392 (19.1) |
| Inpatient clinic/hospital | 13 (1.2) | 5 (7.7) | 0 (0.0) | 18 (0.9) |
| Other | 128 (11.4) | 3 (4.6) | 0 (0.0) | 131 (6.4) |
| Missing/Never tested | 3 (0.3) | 2 (3.1) | 863 (100.0) | 868 (42.3) |
| Dissatisfaction with or lack of counselling when testing for HIV (HIV testers only) | ||||
| Satisfied | 518 (46.1) | 31 (47.7) | 0 (0.0) | 549 (26.8) |
| Dissatisfied or no counselling | 488 (43.4) | 28 (43.1) | 0 (0.0) | 516 (25.2) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 118 (10.5) | 6 (9.2) | 0 (0.0) | 124 (6.0) |
| Dissatisfaction with confidentiality when testing for HIV (HIV testers only)b | ||||
| Satisfied | 991 (88.2) | 44 (67.7) | 0 (0.0) | 1035 (50.4) |
| Dissatisfied | 61 (5.4) | 14 (21.5) | 0 (0.0) | 75 (3.7) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 72 (6.4) | 7 (10.8) | 0 (0.0) | 79 (3.9) |
| Dissatisfaction with respect when testing for HIV (HIV testers only)b | ||||
| Satisfied | 1019 (90.7) | 43 (66.2) | 0 (0.0) | 1062 (51.8) |
| Dissatisfied | 69 (6.1) | 17 (26.2) | 0 (0.0) | 86 (4.2) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 36 (3.2) | 5 (7.7) | 0 (0.0) | 41 (2.0) |
| Ability to talk about sexual behaviour when testing for HIV (HIV testers only)b | ||||
| No | 712 (63.4) | 25 (38.5) | 0 (0.0) | 737 (35.9) |
| Yes | 324 (28.8) | 23 (35.4) | 0 (0.0) | 347 (16.9) |
| I don’t remember | 86 (7.7) | 15 (23.1) | 0 (0.0) | 101 (4.9) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 2 (0.2) | 2 (3.1) | 0 (0.0) | 4 (0.2) |
| Access to free or affordable STI testingb | ||||
| No | 260 (23.1) | 6 (9.2) | 379 (43.9) | 645 (31.4) |
| Yes | 860 (76.5) | 58 (89.2) | 480 (55.6) | 1398 (68.1) |
| Missing | 4 (0.4) | 1 (1.5) | 4 (0.5) | 9 (0.4) |
| Access to free or affordable HIV testing (HIV negative or untested only)b | ||||
| No | 41 (3.7) | 0 (0.0) | 227 (26.3) | 268 (13.1) |
| Yes | 1077 (95.8) | 0 (0.0) | 636 (73.7) | 1713 (83.5) |
| Missing | 6 (0.5) | 65 (100.0) | 0 (0.0) | 71 (3.5) |
| Overall scores on basic knowledge about HIV, STIs, and post-exposure prophylaxisb | ||||
| 0–50% correct | 120 (10.7) | 3 (4.6) | 232 (26.9) | 355 (17.3) |
| 51–75% correct | 650 (57.8) | 17 (26.2) | 468 (54.2) | 1135 (55.5) |
| 76–100% correct | 354 (31.5) | 45 (69.2) | 163 (18.9) | 562 (27.4) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| STI testing in the prior 12 monthsb | ||||
| No STI test | 668 (59.4) | 21 (32.3) | 813 (94.2) | 1502 (73.2) |
| STI tested | 415 (36.9) | 43 (66.2) | 23 (2.7) | 481 (23.4) |
| Missing | 41 (3.7) | 1 (1.5) | 27 (3.1) | 69 (3.4) |
| Self-reported syphilis in last 12 months among those with a blood test | ||||
| Negative | 368 (32.7) | 28 (43.1) | 12 (1.4) | 408 (19.9) |
| Positive | 21 (1.9) | 12 (18.5) | 2 (0.2) | 35 (1.7) |
| No blood test in 12 months | 690 (61.4) | 24 (36.9) | 822 (95.3) | 1536 (74.9) |
| Missing | 45 (4.0) | 1 (1.5) | 27 (3.1) | 73 (3.6) |
| Self-reported anogenital warts in last 12 months among those with a penile/anal inspectionb | ||||
| No | 85 (7.6) | 11 (16.9) | 6 (0.7) | 102 (5.0) |
| Yes | 7 (0.6) | 4 (6.2) | 0 (0.0) | 11 (0.5) |
| No penile/anal inspection in 12 months | 991 (88.2) | 49 (75.4) | 830 (96.2) | 1870 (91.1) |
| Missing | 41 (3.7) | 1 (1.5) | 27 (3.1) | 69 (3.4) |
| Hepatitis B vaccine needsb | ||||
| Immune or already vaccinated | 373 (33.2) | 23 (35.4) | 253 (29.3) | 649 (31.6) |
| Not immune and not fully vaccinated | 583 (51.9) | 37 (56.9) | 389 (45.1) | 1009 (49.2) |
| I don’t know/Missing | 168 (15.0) | 5 (7.7) | 221 (25.6) | 394 (19.2) |
| Use of nitrate inhalants in the last 4 weeksb | ||||
| No | 930 (82.7) | 30 (46.2) | 798 (92.5) | 1758 (85.7) |
| Yes | 184 (16.4) | 35 (53.9) | 59 (6.8) | 278 (13.6) |
| Missing | 10 (0.9) | 0 (0.0) | 6 (0.7) | 16 (0.8) |
| Use of benzodiazepines in the last 12 monthsb | ||||
| No | 919 (81.8) | 48 (73.9) | 759 (88.0) | 1726 (84.1) |
| Yes | 196 (17.4) | 14 (21.5) | 98 (11.4) | 308 15.0 |
| Missing | 9 (0.8) | 3 (4.6) | 6 (0.7) | 18 (0.9) |
| Use of cannabis in the last 12 monthsb | ||||
| No | 882 (78.5) | 47 (72.3) | 739 (85.6) | 1668 (81.3) |
| Yes | 231 (20.6) | 18 (27.7) | 119 (13.8) | 368 (17.9) |
| Missing | 11 (1.0) | 0 (0.0) | 5 (0.6) | 16 (0.8) |
| Use of party-n-play drugs in the last 12 monthsb,c | ||||
| No | 977 (86.9) | 46 (70.8) | 796 (92.2) | 1819 (88.7) |
| Yes | 136 (12.1) | 19 (29.2) | 62 (7.2) | 217 (10.6) |
| Missing | 11 (1.0) | 0 (0.0) | 5 (0.6) | 16 (0.8) |
| Variable . | n (%) . | |||
|---|---|---|---|---|
| Last HIV test negative n = 1124 . | Last HIV test positive n = 65 . | Never tested n = 863 . | Total n = 2052 . | |
| Age, yearsb | ||||
| 15–19 | 37 (3.3) | 0 (0.0) | 153 (17.7) | 190 (9.3) |
| 20–24 | 234 (20.8) | 6 (9.2) | 238 (27.6) | 478 (23.3) |
| 25–29 | 296 (26.3) | 11 (16.9) | 189 (21.9) | 496 (24.2) |
| 30–34 | 272 (24.2) | 9 (13.9) | 137 (15.9) | 418 (20.4) |
| 35–39 | 132 (11.7) | 14 (21.5) | 60 (7.0) | 206 (10.0) |
| 40–44 | 76 (6.8) | 16 (24.6) | 38 (4.4) | 130 (6.3) |
| 45–76 | 77 (6.9) | 9 (13.9) | 48 (5.6) | 134 (6.5) |
| Median, range | 29, 16–68 | 37, 23–68 | 25, 15–76 | 28, 15–76 |
| Residenceb | ||||
| Budapest | 752 (66.9) | 49 (75.4) | 350 (40.6) | 1151 (56.1) |
| Rest of Hungary | 360 (32.0) | 14 (21.5) | 507 (58.8) | 881 (42.9) |
| Missing | 12 (1.1) | 2 (3.1) | 6 (0.7) | 20 (1.0) |
| Born in Hungaryb | ||||
| No | 124 (11.0) | 12 (18.5) | 43 (5.0) | 179 (8.7) |
| Yes | 974 (86.7) | 52 (80.0) | 807 (93.5) | 1833 (89.3) |
| Missing | 26 (2.3) | 1 (1.5) | 13 (1.5) | 40 (2.0) |
| Relationship statusb | ||||
| Single | 534 (47.5) | 29 (44.6) | 494 (57.2) | 1057 (51.5) |
| Steady relationship with men | 526 (46.8) | 35 (53.9) | 265 (30.7) | 826 (40.3) |
| Steady relationship with women only | 53 (4.7) | 1 (1.5) | 93 (10.8) | 147 (7.2) |
| Missing | 4 (0.4) | 0 (0.0) | 6 (0.7) | 10 (0.5) |
| How do you think of yourself? | ||||
| Gay or homosexual | 902 (80.3) | 61 (93.9) | 518 (60.0) | 1481 (72.2) |
| Bisexual | 107 (9.5) | 1 (1.5) | 185 (21.4) | 293 (14.3) |
| Straight or heterosexual | 7 (0.6) | 0 (0.0) | 22 (2.6) | 29 (1.4) |
| Any other term | 6 (0.5) | 0 (0.0) | 13 (1.5) | 19 (0.9) |
| I don’t usually use a term | 101 (9.0) | 3 (4.6) | 124 (14.4) | 228 (11.1) |
| Missing | 1 (0.1) | 0 (0.0) | 1 (0.1) | 2 (0.1) |
| Outness: Of all the people you know, what proportion know you are attracted to men?b | ||||
| More than a few | 759 (67.5) | 55 (84.6) | 300 (34.8) | 1114 (54.3) |
| A few or none | 360 (32.0) | 10 (15.4) | 556 (64.4) | 926 (45.1) |
| Missing | 5 (0.4) | 0 (0.0) | 7 (0.8) | 12 (0.6) |
| Experience with anti-gay violence or intimidation in the last 12 months | ||||
| No violence | 670 (59.6) | 36 (55.4) | 484 (56.1) | 1190 (58.0) |
| Experience with violence or intimidation | 449 (40.0) | 29 (44.6) | 374 (43.3) | 852 (41.5) |
| Missing | 5 (0.4) | 0 (0.0) | 5 (0.6) | 10 (0.5) |
| Sexual happinessb | ||||
| No | 469 (41.7) | 24 (36.9) | 485 (56.2) | 978 (47.7) |
| Yes | 596 (53.0) | 32 (49.2) | 333 (38.6) | 961 (46.8) |
| Missing | 59 (5.3) | 9 (13.9) | 45 (5.2) | 113 (5.5) |
| 12-month HIV transmission riskb | ||||
| No CAI with HIV-unknown/discordant man | 849 (75.5) | 28 (43.1) | 474 (54.9) | 1351 (65.8) |
| CAI with HIV-unknown/discordant man | 232 (20.6) | 36 (55.4) | 316 (36.6) | 584 (28.5) |
| Missing | 43 (3.8) | 1 (1.5) | 73 (8.5) | 117 (5.7) |
| Location of last HIV test/HIV diagnosisb | ||||
| Community-based organization | 498 (44.3) | 21 (32.3) | 0 (0.0) | 519 (25.3) |
| Physician’s office | 119 (10.6) | 5 (7.7) | 0 (0.0) | 124 (6.0) |
| Outpatient clinic/hospital | 363 (32.3) | 29 (44.6) | 0 (0.0) | 392 (19.1) |
| Inpatient clinic/hospital | 13 (1.2) | 5 (7.7) | 0 (0.0) | 18 (0.9) |
| Other | 128 (11.4) | 3 (4.6) | 0 (0.0) | 131 (6.4) |
| Missing/Never tested | 3 (0.3) | 2 (3.1) | 863 (100.0) | 868 (42.3) |
| Dissatisfaction with or lack of counselling when testing for HIV (HIV testers only) | ||||
| Satisfied | 518 (46.1) | 31 (47.7) | 0 (0.0) | 549 (26.8) |
| Dissatisfied or no counselling | 488 (43.4) | 28 (43.1) | 0 (0.0) | 516 (25.2) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 118 (10.5) | 6 (9.2) | 0 (0.0) | 124 (6.0) |
| Dissatisfaction with confidentiality when testing for HIV (HIV testers only)b | ||||
| Satisfied | 991 (88.2) | 44 (67.7) | 0 (0.0) | 1035 (50.4) |
| Dissatisfied | 61 (5.4) | 14 (21.5) | 0 (0.0) | 75 (3.7) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 72 (6.4) | 7 (10.8) | 0 (0.0) | 79 (3.9) |
| Dissatisfaction with respect when testing for HIV (HIV testers only)b | ||||
| Satisfied | 1019 (90.7) | 43 (66.2) | 0 (0.0) | 1062 (51.8) |
| Dissatisfied | 69 (6.1) | 17 (26.2) | 0 (0.0) | 86 (4.2) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 36 (3.2) | 5 (7.7) | 0 (0.0) | 41 (2.0) |
| Ability to talk about sexual behaviour when testing for HIV (HIV testers only)b | ||||
| No | 712 (63.4) | 25 (38.5) | 0 (0.0) | 737 (35.9) |
| Yes | 324 (28.8) | 23 (35.4) | 0 (0.0) | 347 (16.9) |
| I don’t remember | 86 (7.7) | 15 (23.1) | 0 (0.0) | 101 (4.9) |
| Never tested | 0 (0.0) | 0 (0.0) | 863 (100.0) | 863 (42.1) |
| Missing | 2 (0.2) | 2 (3.1) | 0 (0.0) | 4 (0.2) |
| Access to free or affordable STI testingb | ||||
| No | 260 (23.1) | 6 (9.2) | 379 (43.9) | 645 (31.4) |
| Yes | 860 (76.5) | 58 (89.2) | 480 (55.6) | 1398 (68.1) |
| Missing | 4 (0.4) | 1 (1.5) | 4 (0.5) | 9 (0.4) |
| Access to free or affordable HIV testing (HIV negative or untested only)b | ||||
| No | 41 (3.7) | 0 (0.0) | 227 (26.3) | 268 (13.1) |
| Yes | 1077 (95.8) | 0 (0.0) | 636 (73.7) | 1713 (83.5) |
| Missing | 6 (0.5) | 65 (100.0) | 0 (0.0) | 71 (3.5) |
| Overall scores on basic knowledge about HIV, STIs, and post-exposure prophylaxisb | ||||
| 0–50% correct | 120 (10.7) | 3 (4.6) | 232 (26.9) | 355 (17.3) |
| 51–75% correct | 650 (57.8) | 17 (26.2) | 468 (54.2) | 1135 (55.5) |
| 76–100% correct | 354 (31.5) | 45 (69.2) | 163 (18.9) | 562 (27.4) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| STI testing in the prior 12 monthsb | ||||
| No STI test | 668 (59.4) | 21 (32.3) | 813 (94.2) | 1502 (73.2) |
| STI tested | 415 (36.9) | 43 (66.2) | 23 (2.7) | 481 (23.4) |
| Missing | 41 (3.7) | 1 (1.5) | 27 (3.1) | 69 (3.4) |
| Self-reported syphilis in last 12 months among those with a blood test | ||||
| Negative | 368 (32.7) | 28 (43.1) | 12 (1.4) | 408 (19.9) |
| Positive | 21 (1.9) | 12 (18.5) | 2 (0.2) | 35 (1.7) |
| No blood test in 12 months | 690 (61.4) | 24 (36.9) | 822 (95.3) | 1536 (74.9) |
| Missing | 45 (4.0) | 1 (1.5) | 27 (3.1) | 73 (3.6) |
| Self-reported anogenital warts in last 12 months among those with a penile/anal inspectionb | ||||
| No | 85 (7.6) | 11 (16.9) | 6 (0.7) | 102 (5.0) |
| Yes | 7 (0.6) | 4 (6.2) | 0 (0.0) | 11 (0.5) |
| No penile/anal inspection in 12 months | 991 (88.2) | 49 (75.4) | 830 (96.2) | 1870 (91.1) |
| Missing | 41 (3.7) | 1 (1.5) | 27 (3.1) | 69 (3.4) |
| Hepatitis B vaccine needsb | ||||
| Immune or already vaccinated | 373 (33.2) | 23 (35.4) | 253 (29.3) | 649 (31.6) |
| Not immune and not fully vaccinated | 583 (51.9) | 37 (56.9) | 389 (45.1) | 1009 (49.2) |
| I don’t know/Missing | 168 (15.0) | 5 (7.7) | 221 (25.6) | 394 (19.2) |
| Use of nitrate inhalants in the last 4 weeksb | ||||
| No | 930 (82.7) | 30 (46.2) | 798 (92.5) | 1758 (85.7) |
| Yes | 184 (16.4) | 35 (53.9) | 59 (6.8) | 278 (13.6) |
| Missing | 10 (0.9) | 0 (0.0) | 6 (0.7) | 16 (0.8) |
| Use of benzodiazepines in the last 12 monthsb | ||||
| No | 919 (81.8) | 48 (73.9) | 759 (88.0) | 1726 (84.1) |
| Yes | 196 (17.4) | 14 (21.5) | 98 (11.4) | 308 15.0 |
| Missing | 9 (0.8) | 3 (4.6) | 6 (0.7) | 18 (0.9) |
| Use of cannabis in the last 12 monthsb | ||||
| No | 882 (78.5) | 47 (72.3) | 739 (85.6) | 1668 (81.3) |
| Yes | 231 (20.6) | 18 (27.7) | 119 (13.8) | 368 (17.9) |
| Missing | 11 (1.0) | 0 (0.0) | 5 (0.6) | 16 (0.8) |
| Use of party-n-play drugs in the last 12 monthsb,c | ||||
| No | 977 (86.9) | 46 (70.8) | 796 (92.2) | 1819 (88.7) |
| Yes | 136 (12.1) | 19 (29.2) | 62 (7.2) | 217 (10.6) |
| Missing | 11 (1.0) | 0 (0.0) | 5 (0.6) | 16 (0.8) |
Note: MSM: men having sex with men; CAI: condomless anal intercourse; STI: sexually transmitted infection.
The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey.
χ2P values <0.001; Hypothesis test does not include missing observations.
That is, Ecstasy/MDMA, amphetamines, crystal methamphetamine, mephedrone, GHB/GBL, ketamine, or cocaine.
While 45.1% said that no one, or only a few people, knew they were attracted to men, a majority identified as gay (72.2%) and 14.3% identified as bisexual. Four out of ten men (41.5%) reported anti-gay violence or intimidation in the prior year. Less than one-half of men (40.3%) reported being in a relationship with another man while more than a quarter of men (28.5%) reported condomless anal intercourse (CAI) in the prior year with another man of unknown or discordant HIV status.
A total of 42.1% of all men reported never being tested for HIV. About 55% of men reported their last HIV test was negative and 3.2% reported the last HIV test was positive. A plurality of men testing negative (44.3%) had the test at a community-based organization while another 33.5% were tested in a hospital. Approximately 43% of both HIV-positive and HIV-negative men reported either no counselling or dissatisfaction with HIV counselling. Most men who had never tested for HIV also reported no STI testing in the prior 12 months (table 1). A majority of foreign-born men never reporting an HIV test were from Romania, Serbia, and Germany (data not shown).
In multivariable analysis to assess factors associated with non-HIV testers, a number of demographic, sexual behaviour, health care, knowledge, and substance use variables were associated with HIV testing (table 2). For example, men never testing were more likely to live outside of Budapest (aPR 1.50, 95% CI 1.34–1.67), to say that few people or no one knew they were attracted to men (aPR 1.52, 95% CI 1.36–1.71, compared with men who said that more than a few persons knew), to have had CAI with a man of unknown or discordant HIV status in the last year (aPR 1.75, 95% CI 1.58–1.93, compared to men with no CAI risk), and to report no access to free or affordable HIV testing (aPR 1.54, 95% CI 1.41–1.70, compared to HIV-negative men who reported access to free or affordable HIV testing).
| . | Univariable . | Multivariable . | ||
|---|---|---|---|---|
| Variable . | n . | %NTc . | PR (95% CI) . | aPR (95% CI) . |
| Age, years | ||||
| 15–19 | 190 | 0.81 | 2.25 (1.77–2.85) | - |
| 20–24 | 478 | 0.50 | 1.39 (1.09–1.77) | - |
| 25–29 | 496 | 0.38 | 1.06 (0.83–1.37) | - |
| 30–34 | 418 | 0.33 | 0.92 (0.70–1.19) | - |
| 35–39 | 206 | 0.29 | 0.81 (0.60–1.11) | - |
| 40–44 | 130 | 0.29 | 0.82 (0.57–1.16) | - |
| 45–76 | 134 | 0.36 | 1.0 | - |
| Birthplace | ||||
| In Hungary | 1816 | 0.44 | 1.83 (1.41–2.39) | 1.34 (1.05–1.73) |
| Outside of Hungary | 177 | 0.24 | 1.0 | 1.0 |
| Residence | ||||
| Budapest | 1151 | 0.30 | 1.0 | 1.0 |
| Rest of Hungary | 881 | 0.58 | 1.89 (1.71–2.10) | 1.50 (1.34–1.67) |
| Relationship status | ||||
| Single | 1057 | 0.47 | 1.0 | 1.0 |
| Steady relationship with men | 838 | 0.32 | 0.69 (0.61–0.78) | 0.85 (0.75–0.95) |
| Steady relationship with women only | 147 | 0.63 | 1.35 (1.18–1.56) | 1.17 (0.95–1.44) |
| How do you think of yourself? | ||||
| Gay or homosexual | 1481 | 0.35 | 1.0 | 1.0 |
| Bisexual | 293 | 0.63 | 1.81 (1.61–2.02) | 1.33 (1.17–1.52) |
| Straight or heterosexual | 29 | 0.76 | 2.17 (1.75–2.69) | 1.10 (0.67 –1.79) |
| Any other term | 19 | 0.68 | 1.96 (1.43–2.68) | 1.40 (0.85–2.30) |
| I don’t usually use a term | 228 | 0.54 | 1.55 (1.35–1.78) | 1.14 (0.99–1.31) |
| Of all the people you know, what proportion know you are attracted to men? | ||||
| More than a few | 1114 | 0.27 | 1.0 | 1.0 |
| A few or none | 926 | 0.60 | 2.23 (2.00–2.49) | 1.52 (1.36–1.71) |
| Sexual happiness | ||||
| No | 978 | 0.50 | 1.0 | 1.0 |
| Yes | 961 | 0.35 | 0.70 (0.63–0.78) | 0.82 (0.73–0.92) |
| 12-month HIV transmission risk | ||||
| No CAI with HIV-unknown/discordant man | 1351 | 0.35 | 1.0 | 1.0 |
| CAI with HIV-unknown/discordant man | 584 | 0.54 | 1.54 (1.39–1.71) | 1.75 (1.58–1.93) |
| Access to free or affordable HIV testing (HIV negative or untested only) | ||||
| No | 268 | 0.84 | 2.28 (2.11–2.47) | 1.54 (1.41–1.70) |
| Yes | 1713 | 0.37 | 1.0 | 1.0 |
| Overall scores on basic knowledge about HIV, STIs, and post-exposure prophylaxis | ||||
| 0–50% correct | 355 | 0.65 | 2.25 (1.94–2.62) | 1.35 (1.16–1.57) |
| 51–75% correct | 1135 | 0.41 | 1.42 (1.23–1.65) | 1.17 (1.02–1.35) |
| 76–100% correct | 562 | 0.29 | 1.0 | 1.0 |
| Use of nitrate inhalants in the last 4 weeks | ||||
| No | 1758 | 0.45 | 1.0 | 1.0 |
| Yes | 278 | 0.79 | 0.47 (0.37–0.59) | 0.72 (0.57–0.90) |
| Use of benzodiazepines in the last 12 months | ||||
| No | 1726 | 0.56 | 1.0 | 1.0 |
| Yes | 308 | 0.68 | 0.72 (0.61–0.86) | 0.81 (0.68–0.94) |
| Use of cannabis in the last 12 months | ||||
| No | 1668 | 0.56 | 1.0 | 1.0 |
| Yes | 368 | 0.68 | 0.73 (0.62–0.85) | 0.80 (0.68–0.94) |
| . | Univariable . | Multivariable . | ||
|---|---|---|---|---|
| Variable . | n . | %NTc . | PR (95% CI) . | aPR (95% CI) . |
| Age, years | ||||
| 15–19 | 190 | 0.81 | 2.25 (1.77–2.85) | - |
| 20–24 | 478 | 0.50 | 1.39 (1.09–1.77) | - |
| 25–29 | 496 | 0.38 | 1.06 (0.83–1.37) | - |
| 30–34 | 418 | 0.33 | 0.92 (0.70–1.19) | - |
| 35–39 | 206 | 0.29 | 0.81 (0.60–1.11) | - |
| 40–44 | 130 | 0.29 | 0.82 (0.57–1.16) | - |
| 45–76 | 134 | 0.36 | 1.0 | - |
| Birthplace | ||||
| In Hungary | 1816 | 0.44 | 1.83 (1.41–2.39) | 1.34 (1.05–1.73) |
| Outside of Hungary | 177 | 0.24 | 1.0 | 1.0 |
| Residence | ||||
| Budapest | 1151 | 0.30 | 1.0 | 1.0 |
| Rest of Hungary | 881 | 0.58 | 1.89 (1.71–2.10) | 1.50 (1.34–1.67) |
| Relationship status | ||||
| Single | 1057 | 0.47 | 1.0 | 1.0 |
| Steady relationship with men | 838 | 0.32 | 0.69 (0.61–0.78) | 0.85 (0.75–0.95) |
| Steady relationship with women only | 147 | 0.63 | 1.35 (1.18–1.56) | 1.17 (0.95–1.44) |
| How do you think of yourself? | ||||
| Gay or homosexual | 1481 | 0.35 | 1.0 | 1.0 |
| Bisexual | 293 | 0.63 | 1.81 (1.61–2.02) | 1.33 (1.17–1.52) |
| Straight or heterosexual | 29 | 0.76 | 2.17 (1.75–2.69) | 1.10 (0.67 –1.79) |
| Any other term | 19 | 0.68 | 1.96 (1.43–2.68) | 1.40 (0.85–2.30) |
| I don’t usually use a term | 228 | 0.54 | 1.55 (1.35–1.78) | 1.14 (0.99–1.31) |
| Of all the people you know, what proportion know you are attracted to men? | ||||
| More than a few | 1114 | 0.27 | 1.0 | 1.0 |
| A few or none | 926 | 0.60 | 2.23 (2.00–2.49) | 1.52 (1.36–1.71) |
| Sexual happiness | ||||
| No | 978 | 0.50 | 1.0 | 1.0 |
| Yes | 961 | 0.35 | 0.70 (0.63–0.78) | 0.82 (0.73–0.92) |
| 12-month HIV transmission risk | ||||
| No CAI with HIV-unknown/discordant man | 1351 | 0.35 | 1.0 | 1.0 |
| CAI with HIV-unknown/discordant man | 584 | 0.54 | 1.54 (1.39–1.71) | 1.75 (1.58–1.93) |
| Access to free or affordable HIV testing (HIV negative or untested only) | ||||
| No | 268 | 0.84 | 2.28 (2.11–2.47) | 1.54 (1.41–1.70) |
| Yes | 1713 | 0.37 | 1.0 | 1.0 |
| Overall scores on basic knowledge about HIV, STIs, and post-exposure prophylaxis | ||||
| 0–50% correct | 355 | 0.65 | 2.25 (1.94–2.62) | 1.35 (1.16–1.57) |
| 51–75% correct | 1135 | 0.41 | 1.42 (1.23–1.65) | 1.17 (1.02–1.35) |
| 76–100% correct | 562 | 0.29 | 1.0 | 1.0 |
| Use of nitrate inhalants in the last 4 weeks | ||||
| No | 1758 | 0.45 | 1.0 | 1.0 |
| Yes | 278 | 0.79 | 0.47 (0.37–0.59) | 0.72 (0.57–0.90) |
| Use of benzodiazepines in the last 12 months | ||||
| No | 1726 | 0.56 | 1.0 | 1.0 |
| Yes | 308 | 0.68 | 0.72 (0.61–0.86) | 0.81 (0.68–0.94) |
| Use of cannabis in the last 12 months | ||||
| No | 1668 | 0.56 | 1.0 | 1.0 |
| Yes | 368 | 0.68 | 0.73 (0.62–0.85) | 0.80 (0.68–0.94) |
Note: Point estimates and confidence intervals in bold indicate the confidence interval does not include unity. MSM: men having sex with men; PR: prevalence ratio; Apr: adjusted prevalence ratio; CAI: condomless anal intercourse; STI: sexually transmitted infection.
The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey.
All variables adjusted for each other and by age.
Proportion reporting never testing for HIV.
| . | Univariable . | Multivariable . | ||
|---|---|---|---|---|
| Variable . | n . | %NTc . | PR (95% CI) . | aPR (95% CI) . |
| Age, years | ||||
| 15–19 | 190 | 0.81 | 2.25 (1.77–2.85) | - |
| 20–24 | 478 | 0.50 | 1.39 (1.09–1.77) | - |
| 25–29 | 496 | 0.38 | 1.06 (0.83–1.37) | - |
| 30–34 | 418 | 0.33 | 0.92 (0.70–1.19) | - |
| 35–39 | 206 | 0.29 | 0.81 (0.60–1.11) | - |
| 40–44 | 130 | 0.29 | 0.82 (0.57–1.16) | - |
| 45–76 | 134 | 0.36 | 1.0 | - |
| Birthplace | ||||
| In Hungary | 1816 | 0.44 | 1.83 (1.41–2.39) | 1.34 (1.05–1.73) |
| Outside of Hungary | 177 | 0.24 | 1.0 | 1.0 |
| Residence | ||||
| Budapest | 1151 | 0.30 | 1.0 | 1.0 |
| Rest of Hungary | 881 | 0.58 | 1.89 (1.71–2.10) | 1.50 (1.34–1.67) |
| Relationship status | ||||
| Single | 1057 | 0.47 | 1.0 | 1.0 |
| Steady relationship with men | 838 | 0.32 | 0.69 (0.61–0.78) | 0.85 (0.75–0.95) |
| Steady relationship with women only | 147 | 0.63 | 1.35 (1.18–1.56) | 1.17 (0.95–1.44) |
| How do you think of yourself? | ||||
| Gay or homosexual | 1481 | 0.35 | 1.0 | 1.0 |
| Bisexual | 293 | 0.63 | 1.81 (1.61–2.02) | 1.33 (1.17–1.52) |
| Straight or heterosexual | 29 | 0.76 | 2.17 (1.75–2.69) | 1.10 (0.67 –1.79) |
| Any other term | 19 | 0.68 | 1.96 (1.43–2.68) | 1.40 (0.85–2.30) |
| I don’t usually use a term | 228 | 0.54 | 1.55 (1.35–1.78) | 1.14 (0.99–1.31) |
| Of all the people you know, what proportion know you are attracted to men? | ||||
| More than a few | 1114 | 0.27 | 1.0 | 1.0 |
| A few or none | 926 | 0.60 | 2.23 (2.00–2.49) | 1.52 (1.36–1.71) |
| Sexual happiness | ||||
| No | 978 | 0.50 | 1.0 | 1.0 |
| Yes | 961 | 0.35 | 0.70 (0.63–0.78) | 0.82 (0.73–0.92) |
| 12-month HIV transmission risk | ||||
| No CAI with HIV-unknown/discordant man | 1351 | 0.35 | 1.0 | 1.0 |
| CAI with HIV-unknown/discordant man | 584 | 0.54 | 1.54 (1.39–1.71) | 1.75 (1.58–1.93) |
| Access to free or affordable HIV testing (HIV negative or untested only) | ||||
| No | 268 | 0.84 | 2.28 (2.11–2.47) | 1.54 (1.41–1.70) |
| Yes | 1713 | 0.37 | 1.0 | 1.0 |
| Overall scores on basic knowledge about HIV, STIs, and post-exposure prophylaxis | ||||
| 0–50% correct | 355 | 0.65 | 2.25 (1.94–2.62) | 1.35 (1.16–1.57) |
| 51–75% correct | 1135 | 0.41 | 1.42 (1.23–1.65) | 1.17 (1.02–1.35) |
| 76–100% correct | 562 | 0.29 | 1.0 | 1.0 |
| Use of nitrate inhalants in the last 4 weeks | ||||
| No | 1758 | 0.45 | 1.0 | 1.0 |
| Yes | 278 | 0.79 | 0.47 (0.37–0.59) | 0.72 (0.57–0.90) |
| Use of benzodiazepines in the last 12 months | ||||
| No | 1726 | 0.56 | 1.0 | 1.0 |
| Yes | 308 | 0.68 | 0.72 (0.61–0.86) | 0.81 (0.68–0.94) |
| Use of cannabis in the last 12 months | ||||
| No | 1668 | 0.56 | 1.0 | 1.0 |
| Yes | 368 | 0.68 | 0.73 (0.62–0.85) | 0.80 (0.68–0.94) |
| . | Univariable . | Multivariable . | ||
|---|---|---|---|---|
| Variable . | n . | %NTc . | PR (95% CI) . | aPR (95% CI) . |
| Age, years | ||||
| 15–19 | 190 | 0.81 | 2.25 (1.77–2.85) | - |
| 20–24 | 478 | 0.50 | 1.39 (1.09–1.77) | - |
| 25–29 | 496 | 0.38 | 1.06 (0.83–1.37) | - |
| 30–34 | 418 | 0.33 | 0.92 (0.70–1.19) | - |
| 35–39 | 206 | 0.29 | 0.81 (0.60–1.11) | - |
| 40–44 | 130 | 0.29 | 0.82 (0.57–1.16) | - |
| 45–76 | 134 | 0.36 | 1.0 | - |
| Birthplace | ||||
| In Hungary | 1816 | 0.44 | 1.83 (1.41–2.39) | 1.34 (1.05–1.73) |
| Outside of Hungary | 177 | 0.24 | 1.0 | 1.0 |
| Residence | ||||
| Budapest | 1151 | 0.30 | 1.0 | 1.0 |
| Rest of Hungary | 881 | 0.58 | 1.89 (1.71–2.10) | 1.50 (1.34–1.67) |
| Relationship status | ||||
| Single | 1057 | 0.47 | 1.0 | 1.0 |
| Steady relationship with men | 838 | 0.32 | 0.69 (0.61–0.78) | 0.85 (0.75–0.95) |
| Steady relationship with women only | 147 | 0.63 | 1.35 (1.18–1.56) | 1.17 (0.95–1.44) |
| How do you think of yourself? | ||||
| Gay or homosexual | 1481 | 0.35 | 1.0 | 1.0 |
| Bisexual | 293 | 0.63 | 1.81 (1.61–2.02) | 1.33 (1.17–1.52) |
| Straight or heterosexual | 29 | 0.76 | 2.17 (1.75–2.69) | 1.10 (0.67 –1.79) |
| Any other term | 19 | 0.68 | 1.96 (1.43–2.68) | 1.40 (0.85–2.30) |
| I don’t usually use a term | 228 | 0.54 | 1.55 (1.35–1.78) | 1.14 (0.99–1.31) |
| Of all the people you know, what proportion know you are attracted to men? | ||||
| More than a few | 1114 | 0.27 | 1.0 | 1.0 |
| A few or none | 926 | 0.60 | 2.23 (2.00–2.49) | 1.52 (1.36–1.71) |
| Sexual happiness | ||||
| No | 978 | 0.50 | 1.0 | 1.0 |
| Yes | 961 | 0.35 | 0.70 (0.63–0.78) | 0.82 (0.73–0.92) |
| 12-month HIV transmission risk | ||||
| No CAI with HIV-unknown/discordant man | 1351 | 0.35 | 1.0 | 1.0 |
| CAI with HIV-unknown/discordant man | 584 | 0.54 | 1.54 (1.39–1.71) | 1.75 (1.58–1.93) |
| Access to free or affordable HIV testing (HIV negative or untested only) | ||||
| No | 268 | 0.84 | 2.28 (2.11–2.47) | 1.54 (1.41–1.70) |
| Yes | 1713 | 0.37 | 1.0 | 1.0 |
| Overall scores on basic knowledge about HIV, STIs, and post-exposure prophylaxis | ||||
| 0–50% correct | 355 | 0.65 | 2.25 (1.94–2.62) | 1.35 (1.16–1.57) |
| 51–75% correct | 1135 | 0.41 | 1.42 (1.23–1.65) | 1.17 (1.02–1.35) |
| 76–100% correct | 562 | 0.29 | 1.0 | 1.0 |
| Use of nitrate inhalants in the last 4 weeks | ||||
| No | 1758 | 0.45 | 1.0 | 1.0 |
| Yes | 278 | 0.79 | 0.47 (0.37–0.59) | 0.72 (0.57–0.90) |
| Use of benzodiazepines in the last 12 months | ||||
| No | 1726 | 0.56 | 1.0 | 1.0 |
| Yes | 308 | 0.68 | 0.72 (0.61–0.86) | 0.81 (0.68–0.94) |
| Use of cannabis in the last 12 months | ||||
| No | 1668 | 0.56 | 1.0 | 1.0 |
| Yes | 368 | 0.68 | 0.73 (0.62–0.85) | 0.80 (0.68–0.94) |
Note: Point estimates and confidence intervals in bold indicate the confidence interval does not include unity. MSM: men having sex with men; PR: prevalence ratio; Apr: adjusted prevalence ratio; CAI: condomless anal intercourse; STI: sexually transmitted infection.
The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey.
All variables adjusted for each other and by age.
Proportion reporting never testing for HIV.
Among men who had ever had an HIV test and after adjustment for age, birthplace, and residence, men were more likely to be dissatisfied with HIV-test counselling (or to have never received counselling during HIV testing) if they reported that few people or no one knew they were attracted to men (aPR 1.09, 95% CI 1.02–1.15, compared with men who said that more than a few persons knew). In addition, men who reported they were sexually happy had less dissatisfaction with HIV testing and counselling while men who had no STI testing in the prior 12 months had increased dissatisfaction (table 3).
Factors associated with dissatisfaction with HIV testing and counselling among 1154 MSM testing for HIV in Hungarya
| . | Univariable . | Multivariableb . | ||
|---|---|---|---|---|
| Variable . | n . | %Disc . | PR (95% CI) . | aPR (95% CI) . |
| Age, years | ||||
| 15–19 | 36 | 0.89 | 1.17 (0.99–1.38) | - |
| 20–24 | 235 | 0.79 | 1.04 (0.90–1.19) | - |
| 25–29 | 294 | 0.80 | 1.06 (0.93–1.21) | - |
| 30–34 | 272 | 0.81 | 1.07 (0.93–1.22) | - |
| 35–39 | 144 | 0.79 | 1.03 (0.89–1.20) | - |
| 40–44 | 90 | 0.83 | 1.10 (0.94–1.28) | - |
| 45–76 | 83 | 0.76 | 1.0 | - |
| Birthplace | ||||
| In Hungary | 999 | 0.80 | 1.05 (0.95–1.16) | - |
| Outside of Hungary | 128 | 0.77 | 1.0 | - |
| Residence | ||||
| Budapest | 777 | 0.78 | 1.0 | - |
| Rest of Hungary | 365 | 0.84 | 1.08 (1.02–1.14) | - |
| Relationship status | ||||
| Single | 548 | 0.82 | 1.0 | - |
| Steady relationship with men | 550 | 0.77 | 0.94 (0.89–1.00) | - |
| Steady relationship with women only | 52 | 0.92 | 1.13 (1.03–1.23) | - |
| How do you think of yourself? | ||||
| Gay or homosexual | 935 | 0.79 | 1.0 | - |
| Bisexual | 104 | 0.87 | 1.09 (1.01–1.19) | - |
| Any other term | 13 | 0.84 | 1.07 (0.85–1.35) | - |
| I don’t usually use a term | 101 | 0.82 | 1.04 (0.94–1.15) | - |
| Of all the people you know, what proportion know you are attracted to men? | ||||
| More than a few | 789 | 0.77 | 1.0 | 1.0 |
| A few or none | 360 | 0.86 | 1.11 (1.05–1.17) | 1.09 (1.02–1.15) |
| Sexual happiness | ||||
| No | 478 | 0.83 | 1.0 | 1.0 |
| Yes | 611 | 0.78 | 0.94 (0.88–0.99) | 0.94 (0.88–0.99) |
| Location of last HIV test/HIV diagnosis | ||||
| Community-based organization | 505 | 0.72 | 1.0 | 1.0 |
| Physician’s office | 120 | 0.78 | 1.07 (0.96–1.20) | 1.10 (0.98–1.23) |
| Outpatient clinic/hospital | 380 | 0.85 | 1.18 (1.10–1.26) | 1.16 (1.08–1.25) |
| Inpatient clinic/hospital | 18 | 0.94 | 1.31 (1.16–1.48) | 1.32 (1.16–1.50) |
| Other | 130 | 0.97 | 1.34 (1.26–1.43) | 1.30 (1.22–1.39) |
| Self-reported STI testing in the prior 12 months | ||||
| No STI test | 669 | 0.85 | 1.15 (1.08–1.23) | 1.15 (1.07–1.23) |
| STI tested | 445 | 0.74 | 1.0 | 1.0 |
| Self-reported syphilis result in last 12 months among those with a blood test | ||||
| Negative | 384 | 0.75 | 1.0 | - |
| Positive | 33 | 0.67 | 0.89 (0.69–1.14) | - |
| No blood test in 12 months | 693 | 0.84 | 1.12 (1.04–1.19) | |
| . | Univariable . | Multivariableb . | ||
|---|---|---|---|---|
| Variable . | n . | %Disc . | PR (95% CI) . | aPR (95% CI) . |
| Age, years | ||||
| 15–19 | 36 | 0.89 | 1.17 (0.99–1.38) | - |
| 20–24 | 235 | 0.79 | 1.04 (0.90–1.19) | - |
| 25–29 | 294 | 0.80 | 1.06 (0.93–1.21) | - |
| 30–34 | 272 | 0.81 | 1.07 (0.93–1.22) | - |
| 35–39 | 144 | 0.79 | 1.03 (0.89–1.20) | - |
| 40–44 | 90 | 0.83 | 1.10 (0.94–1.28) | - |
| 45–76 | 83 | 0.76 | 1.0 | - |
| Birthplace | ||||
| In Hungary | 999 | 0.80 | 1.05 (0.95–1.16) | - |
| Outside of Hungary | 128 | 0.77 | 1.0 | - |
| Residence | ||||
| Budapest | 777 | 0.78 | 1.0 | - |
| Rest of Hungary | 365 | 0.84 | 1.08 (1.02–1.14) | - |
| Relationship status | ||||
| Single | 548 | 0.82 | 1.0 | - |
| Steady relationship with men | 550 | 0.77 | 0.94 (0.89–1.00) | - |
| Steady relationship with women only | 52 | 0.92 | 1.13 (1.03–1.23) | - |
| How do you think of yourself? | ||||
| Gay or homosexual | 935 | 0.79 | 1.0 | - |
| Bisexual | 104 | 0.87 | 1.09 (1.01–1.19) | - |
| Any other term | 13 | 0.84 | 1.07 (0.85–1.35) | - |
| I don’t usually use a term | 101 | 0.82 | 1.04 (0.94–1.15) | - |
| Of all the people you know, what proportion know you are attracted to men? | ||||
| More than a few | 789 | 0.77 | 1.0 | 1.0 |
| A few or none | 360 | 0.86 | 1.11 (1.05–1.17) | 1.09 (1.02–1.15) |
| Sexual happiness | ||||
| No | 478 | 0.83 | 1.0 | 1.0 |
| Yes | 611 | 0.78 | 0.94 (0.88–0.99) | 0.94 (0.88–0.99) |
| Location of last HIV test/HIV diagnosis | ||||
| Community-based organization | 505 | 0.72 | 1.0 | 1.0 |
| Physician’s office | 120 | 0.78 | 1.07 (0.96–1.20) | 1.10 (0.98–1.23) |
| Outpatient clinic/hospital | 380 | 0.85 | 1.18 (1.10–1.26) | 1.16 (1.08–1.25) |
| Inpatient clinic/hospital | 18 | 0.94 | 1.31 (1.16–1.48) | 1.32 (1.16–1.50) |
| Other | 130 | 0.97 | 1.34 (1.26–1.43) | 1.30 (1.22–1.39) |
| Self-reported STI testing in the prior 12 months | ||||
| No STI test | 669 | 0.85 | 1.15 (1.08–1.23) | 1.15 (1.07–1.23) |
| STI tested | 445 | 0.74 | 1.0 | 1.0 |
| Self-reported syphilis result in last 12 months among those with a blood test | ||||
| Negative | 384 | 0.75 | 1.0 | - |
| Positive | 33 | 0.67 | 0.89 (0.69–1.14) | - |
| No blood test in 12 months | 693 | 0.84 | 1.12 (1.04–1.19) | |
Note: MSM: men having sex with men; PR: prevalence ratio; aPR: adjusted prevalence ratio; STI: sexually transmitted infection.
The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey. Variable ‘Dissatisfaction with HIV testing’ created from four variables in table 1: dissatisfaction with confidentiality when testing, dissatisfaction with respect when testing, lack of counselling or dissatisfaction with counselling when testing, and able to talk about sexual behaviour when testing for HIV.
All variables adjusted for each other and by age, birthplace, and residence.
Proportion dissatisfied with HIV testing and counselling.
Factors associated with dissatisfaction with HIV testing and counselling among 1154 MSM testing for HIV in Hungarya
| . | Univariable . | Multivariableb . | ||
|---|---|---|---|---|
| Variable . | n . | %Disc . | PR (95% CI) . | aPR (95% CI) . |
| Age, years | ||||
| 15–19 | 36 | 0.89 | 1.17 (0.99–1.38) | - |
| 20–24 | 235 | 0.79 | 1.04 (0.90–1.19) | - |
| 25–29 | 294 | 0.80 | 1.06 (0.93–1.21) | - |
| 30–34 | 272 | 0.81 | 1.07 (0.93–1.22) | - |
| 35–39 | 144 | 0.79 | 1.03 (0.89–1.20) | - |
| 40–44 | 90 | 0.83 | 1.10 (0.94–1.28) | - |
| 45–76 | 83 | 0.76 | 1.0 | - |
| Birthplace | ||||
| In Hungary | 999 | 0.80 | 1.05 (0.95–1.16) | - |
| Outside of Hungary | 128 | 0.77 | 1.0 | - |
| Residence | ||||
| Budapest | 777 | 0.78 | 1.0 | - |
| Rest of Hungary | 365 | 0.84 | 1.08 (1.02–1.14) | - |
| Relationship status | ||||
| Single | 548 | 0.82 | 1.0 | - |
| Steady relationship with men | 550 | 0.77 | 0.94 (0.89–1.00) | - |
| Steady relationship with women only | 52 | 0.92 | 1.13 (1.03–1.23) | - |
| How do you think of yourself? | ||||
| Gay or homosexual | 935 | 0.79 | 1.0 | - |
| Bisexual | 104 | 0.87 | 1.09 (1.01–1.19) | - |
| Any other term | 13 | 0.84 | 1.07 (0.85–1.35) | - |
| I don’t usually use a term | 101 | 0.82 | 1.04 (0.94–1.15) | - |
| Of all the people you know, what proportion know you are attracted to men? | ||||
| More than a few | 789 | 0.77 | 1.0 | 1.0 |
| A few or none | 360 | 0.86 | 1.11 (1.05–1.17) | 1.09 (1.02–1.15) |
| Sexual happiness | ||||
| No | 478 | 0.83 | 1.0 | 1.0 |
| Yes | 611 | 0.78 | 0.94 (0.88–0.99) | 0.94 (0.88–0.99) |
| Location of last HIV test/HIV diagnosis | ||||
| Community-based organization | 505 | 0.72 | 1.0 | 1.0 |
| Physician’s office | 120 | 0.78 | 1.07 (0.96–1.20) | 1.10 (0.98–1.23) |
| Outpatient clinic/hospital | 380 | 0.85 | 1.18 (1.10–1.26) | 1.16 (1.08–1.25) |
| Inpatient clinic/hospital | 18 | 0.94 | 1.31 (1.16–1.48) | 1.32 (1.16–1.50) |
| Other | 130 | 0.97 | 1.34 (1.26–1.43) | 1.30 (1.22–1.39) |
| Self-reported STI testing in the prior 12 months | ||||
| No STI test | 669 | 0.85 | 1.15 (1.08–1.23) | 1.15 (1.07–1.23) |
| STI tested | 445 | 0.74 | 1.0 | 1.0 |
| Self-reported syphilis result in last 12 months among those with a blood test | ||||
| Negative | 384 | 0.75 | 1.0 | - |
| Positive | 33 | 0.67 | 0.89 (0.69–1.14) | - |
| No blood test in 12 months | 693 | 0.84 | 1.12 (1.04–1.19) | |
| . | Univariable . | Multivariableb . | ||
|---|---|---|---|---|
| Variable . | n . | %Disc . | PR (95% CI) . | aPR (95% CI) . |
| Age, years | ||||
| 15–19 | 36 | 0.89 | 1.17 (0.99–1.38) | - |
| 20–24 | 235 | 0.79 | 1.04 (0.90–1.19) | - |
| 25–29 | 294 | 0.80 | 1.06 (0.93–1.21) | - |
| 30–34 | 272 | 0.81 | 1.07 (0.93–1.22) | - |
| 35–39 | 144 | 0.79 | 1.03 (0.89–1.20) | - |
| 40–44 | 90 | 0.83 | 1.10 (0.94–1.28) | - |
| 45–76 | 83 | 0.76 | 1.0 | - |
| Birthplace | ||||
| In Hungary | 999 | 0.80 | 1.05 (0.95–1.16) | - |
| Outside of Hungary | 128 | 0.77 | 1.0 | - |
| Residence | ||||
| Budapest | 777 | 0.78 | 1.0 | - |
| Rest of Hungary | 365 | 0.84 | 1.08 (1.02–1.14) | - |
| Relationship status | ||||
| Single | 548 | 0.82 | 1.0 | - |
| Steady relationship with men | 550 | 0.77 | 0.94 (0.89–1.00) | - |
| Steady relationship with women only | 52 | 0.92 | 1.13 (1.03–1.23) | - |
| How do you think of yourself? | ||||
| Gay or homosexual | 935 | 0.79 | 1.0 | - |
| Bisexual | 104 | 0.87 | 1.09 (1.01–1.19) | - |
| Any other term | 13 | 0.84 | 1.07 (0.85–1.35) | - |
| I don’t usually use a term | 101 | 0.82 | 1.04 (0.94–1.15) | - |
| Of all the people you know, what proportion know you are attracted to men? | ||||
| More than a few | 789 | 0.77 | 1.0 | 1.0 |
| A few or none | 360 | 0.86 | 1.11 (1.05–1.17) | 1.09 (1.02–1.15) |
| Sexual happiness | ||||
| No | 478 | 0.83 | 1.0 | 1.0 |
| Yes | 611 | 0.78 | 0.94 (0.88–0.99) | 0.94 (0.88–0.99) |
| Location of last HIV test/HIV diagnosis | ||||
| Community-based organization | 505 | 0.72 | 1.0 | 1.0 |
| Physician’s office | 120 | 0.78 | 1.07 (0.96–1.20) | 1.10 (0.98–1.23) |
| Outpatient clinic/hospital | 380 | 0.85 | 1.18 (1.10–1.26) | 1.16 (1.08–1.25) |
| Inpatient clinic/hospital | 18 | 0.94 | 1.31 (1.16–1.48) | 1.32 (1.16–1.50) |
| Other | 130 | 0.97 | 1.34 (1.26–1.43) | 1.30 (1.22–1.39) |
| Self-reported STI testing in the prior 12 months | ||||
| No STI test | 669 | 0.85 | 1.15 (1.08–1.23) | 1.15 (1.07–1.23) |
| STI tested | 445 | 0.74 | 1.0 | 1.0 |
| Self-reported syphilis result in last 12 months among those with a blood test | ||||
| Negative | 384 | 0.75 | 1.0 | - |
| Positive | 33 | 0.67 | 0.89 (0.69–1.14) | - |
| No blood test in 12 months | 693 | 0.84 | 1.12 (1.04–1.19) | |
Note: MSM: men having sex with men; PR: prevalence ratio; aPR: adjusted prevalence ratio; STI: sexually transmitted infection.
The EMIS Network. EMIS 2010: The European Men-Who-Have-Sex-With-Men Internet Survey. Variable ‘Dissatisfaction with HIV testing’ created from four variables in table 1: dissatisfaction with confidentiality when testing, dissatisfaction with respect when testing, lack of counselling or dissatisfaction with counselling when testing, and able to talk about sexual behaviour when testing for HIV.
All variables adjusted for each other and by age, birthplace, and residence.
Proportion dissatisfied with HIV testing and counselling.
Men also reported dissatisfaction if they had HIV testing in places other than a community-based organization or a physician’s office. For example, men getting an HIV test in an inpatient hospital setting were 31% more likely to voice dissatisfaction with HIV testing and counselling compared with men testing in a community-based organization (aPR 1.32, 95% CI 1.16–1.50) (table 3). Men testing in community-based organizations compared with hospitals generally reported less dissatisfaction with test confidentiality (P = 0.05), respect (P = 0.02), counselling (P < 0.0001), and the opportunity to disclose sexual behaviour with men (P < 0.0001) (figure 1).
Discussion
In a large internet-based sample of Hungarian MSM, dissatisfaction with HIV testing and counselling was very common regardless of the kind of test site; however, men had increased dissatisfaction with hospitals and ‘other’ test sites compared to community-based organizations. In addition, in contrast to an analysis of EMIS data in the Netherlands which found that less CAI was associated with less HIV testing,20 MSM in Hungary with higher levels of CAI were less likely to have ever had HIV testing. A negative association between MSM HIV risk behaviours and testing was also observed in Portuguese EMIS data.21
Stigmatization of homosexuality and internalized homonegativity are associated with decreased HIV testing22,23 and MSM in Hungary may be exposed to increased amounts of stigmatization compared with MSM in some other European countries.12 Indeed, Hungarian MSM who reported no HIV test were 52% more likely to say that no one, or only a few people, knew they were attracted men. Closeted men were also more likely to be dissatisfied with HIV testing and counselling. It is possible that a stigmatizing experience with testing may induce men to remain closeted.23 It is also possible that closeted men are more likely to avoid HIV testing.22 In both cases, HIV testing that preserves confidentiality and is respectful of MSM may reduce barriers to initial and repeated HIV testing.
While recent HIV and STI epidemic trends in Europe indicate increased HIV and STI risk for younger MSM,4 Hungarian MSM under the age of 30 were less likely to have had an HIV test than any other age group. While increased age generally leads to increased opportunity to test, it is notable that just over 80% of MSM aged 15–19 years, and one-half of MSM aged 20–24 years reported never testing for HIV.
Almost 60% of MSM who did not report an HIV test lived outside of Budapest. Compared to men in Budapest, more than double the proportion of men outside of Budapest reported no access to free and affordable HIV testing (P < 0.0001) (data not shown). Given that more than one in five HIV-positive Hungarian men in this sample lived outside of Budapest, free and/or affordable testing for MSM in smaller cities and towns in Hungary may enhance detection of HIV infection, especially if this HIV testing is perceived as confidential and respectful of the men.
Sexual happiness was associated with decreased HIV test dissatisfaction (i.e. sexual happiness was associated with increased satisfaction in HIV-test counselling) while lack of recent STI testing was associated with increased dissatisfaction. It is plausible that HIV testing including appropriate sexual health counselling would support sexual happiness. It is also possible that stigma-related dissatisfaction with HIV testing and counselling could inhibit subsequent STI testing;22 however, the current cross-sectional study design generally precludes such conclusions. It is worth noting that Budapest has limited access to STI testing for MSM in comparison to many other European cities.24
In addition to the limitations of recall bias and social desirability bias, MSM without internet access were excluded from taking the survey which could also introduce selection bias since household internet access in 2009 in Hungary was only approximately 50%.25 In general, internet samples of MSM, when compared with convenience samples, may be more bisexually identified, younger, and more representative of MSM outside of urban centres.26 Indeed, almost one-third of the men in the current study resided outside of Budapest. However, the anonymity of the survey may have reduced social desirability bias and the internet-based platform may have increased the diversity of the men26 leading to a more representative sample.27,28 In addition, while 36% of Hungarians live outside of Budapest, over 43% of men in our sample reported living outside of Budapest providing important data about MSM health in areas in Eastern Europe outside of a large metropolitan area. EMIS data for all 38 European countries found HIV-positive men were less satisfied with confidentiality and respect during HIV testing and counselling, while HIV-negative men had less opportunity to talk about sex.4 Our sample only had 65 men who reported HIV infection precluding us from making generalizations about dissatisfaction stratified by HIV status. The EMIS data lacked a socioeconomic measure which prevented us from assessing an association between income and lack of HIV testing and dissatisfaction with HIV testing and counselling. Finally, the data were collected in 2010 and it is possible that men’s responses to questions about HIV testing and counselling satisfaction may have changed in the interim.
Men who were closeted were less likely to test and more likely to be dissatisfied with the counselling if they had ever had an HIV test. Given the high proportion of men having CAI with discordant or unknown HIV status partners, the limited HIV testing, and the limited basic knowledge about HIV, STIs, and post-exposure prophylaxis (PEP) among men who had not been tested, a substantial portion of Hungarian MSM are likely at high risk for HIV infection. Detecting that infection, and preventing future infection, is hampered by limited HIV counselling and sexual health instruction as reported by a high proportion of Hungarian MSM who have had HIV testing. Such disease prevention counselling should be implemented in test sites in order to educate men on methods of HIV and STI prevention. Indeed, successful HIV interventions in Hungary are possible even in the face of significant stigma surrounding same-sex behaviour.29 In this analysis, men reported that community-based organizations better supported confidentiality and provided more respect during HIV testing. Given that Hungarian MSM were also more likely to attend community-based organizations for HIV testing, organizations that are culturally competent with MSM should be supported in order to increase access to HIV testing.
Funding
This work was supported by a grant of the European Commission under the EU Health Programme 2008–2013. Further funding was received from CEEISCat (Centre d’Estudis Epidemiològics sobre les ITS/HIV/SIDA de Catalunya, Spain); Department of Health for England; Maastricht University (The Netherlands); Regione del Veneto (Italy); and Robert Koch Institute (Germany).
Conflicts of interest: None declared.
HIV testing among the population at highest risk for HIV in Hungary, men who have sex with men (MSM), remains suboptimal.
Dissatisfaction with HIV testing was highest among those testing in an inpatient hospital and lowest in those testing at a community-based organization.
Being closeted was strongly associated with lack of HIV testing and dissatisfaction with testing.
Community-based organizations that are culturally competent with MSM should be supported in Hungary to increase HIV testing and prevention.
Acknowledgements
We would like to acknowledge the scientists who organized and conducted EMIS between 2009 and 2011: Ulrich Marcus (Project initiation and supervision); Peter Weatherburn (Promotion co-ordination); Ford Hickson and David Reid (Technical implementation) in the European MSM Internet Survey network. We are grateful for the support of our Hungarian EMIS partners: the Hungarian Civil Liberties Union and Háttér. AGN conducted primary analysis and writing of the manuscript; MWR, FB, and AJS contributed to analysis design and manuscript review; AJS also contributed to data analysis.




Comments