-
PDF
- Split View
-
Views
-
Cite
Cite
Luca Segreti, Christopher A Rinaldi, Simon Claridge, Jesper Hastrup Svendsen, Carina Blomstrom-Lundqvist, Angelo Auricchio, Christian Butter, Nikolaos Dagres, Jean-Claude Deharo, Aldo P Maggioni, Andrzej Kutarski, Charles Kennergren, Cecile Laroche, Maciej Kempa, Andrea Magnani, Benjamin Casteigt, Maria Grazia Bongiorni, Procedural outcomes associated with transvenous lead extraction in patients with abandoned leads: an ESC-EHRA ELECTRa (European Lead Extraction ConTRolled) Registry Sub-Analysis, EP Europace, Volume 21, Issue 4, April 2019, Pages 645–654, https://doi.org/10.1093/europace/euy307
Close - Share Icon Share
Abstract
The decision to abandon or extract superfluous leads remains controversial. We sought to compare procedural outcome of patients with and without abandoned leads undergoing transvenous lead extraction (TLE).
An analysis of the ESC-EHRA European Lead Extraction ConTRolled ELECTRa registry was conducted. Patients were stratified into two groups based on the presence (Group 1) or absence (Group 2) of abandoned leads at the time for extraction. Out of 3508 TLE procedures, 422 patients (12.0%) had abandoned leads (Group 1). Group 1 patients were older and more likely to have implantable cardioverter-defibrillator devices, infection indication (78.8% vs. 49.8%), and vegetations (24.6% vs. 15.3%). Oldest lead dwelling time was longer in Group 1 (10.9 vs. 6.3 years) as was the number of extracted leads per patient (3.2 vs. 1.7). Manual traction failure (94.5% vs. 78.8%), powered sheath use (50.7% vs. 28.4%), and femoral approach were higher in Group 1 (P < 0.0001). Procedural success rate and clinical success (89.8% vs. 96.6%, P < 0.0001) were lower in Group 1. Major complication including deaths (5.5% vs. 2.3%, P = 0.0007) and procedure related major complications (3.3% vs. 1.4%, P = 0.0123) were higher in Group 1. The presence of abandoned leads at the time of TLE was an independent predictor of clinical failure [odds ratio (OR) 2.31, confidence interval (CI) 1.57–3.40] and complications [OR 1.69, CI 1.22–2.35]. receiver-operating characteristic curve analysis showed a dwell time threshold of 9 years for radiological failure and major complications.
Previously abandoned leads at the time of TLE were associated with increased procedural complexity, clinical failure, and major complication, which may have important implications for future studies regarding managing of lead failures.
The implications of abandoned leads are a greater lead burden and a greater dwell time of the abandoned lead.
Infective indications to lead extraction are common in patients with abandoned leads.
Previously abandoned leads at the time of transvenous lead extraction were associated with increased procedural complexity, clinical failure, and major complication.
Receiver-operating characteristic curve analysis showed a dwell time threshold of 9 years for radiological failure and major complications.
Introduction
In recent years, the number of cardiac implantable electronic device (CIED) complications has steadily increased due to the growing of annual device implantations, more complex devices and procedures, higher risk patients, lead malfunctions, and recalls.1
During the last decades, transvenous lead extraction (TLE) techniques have improved, becoming a complete, safe, and effective procedure. The European Heart Rhythm Association (EHRA) in 2018,2 and the Heart Rhythm Society (HRS) in 20173 published recommendations on TLE with well-defined indications and definitions allowing accurate estimation of success and complication rates. In patients with CIED infections TLE, with a goal of complete removal of all hardware, is standard of care. However, the extraction of non-infected leads, which may be abandoned and rendered superfluous, remains controversial3 with little data available to guide management. A European survey administrated by EHRA in 20144 provided a snapshot of the clinical practices in lead management and the decision-making process of malfunctioning, redundant, or recalled pacemaker (PM) and implantable cardioverter-defibrillators (ICDs) leads across Europe. The main factors influencing the decision making were patient’s age (59%), the presence of the damaged leads (44%), and the lead dwelling time (44%). Regarding the lead abandonment, the main concern (61%) was the potential greater difficulty associated with lead extraction in the future.
Finally, the ELECTRa (European Lead Extraction Controlled) Registry5 was the first and largest European Registry of consecutive patients undergoing TLE procedures conducted to reflect the real-life experience of 73 centres in 19 European countries.
The aim of this study was to compare procedural outcome of patients with and without abandoned leads undergoing TLE.
Methods
An analysis of the ELECTRa study was conducted. The executive committee in co-operation with the EURObservational Research Programme (EORP) provided the study design, protocol, and the scientific leadership of the registry under the responsibility of the EHRA Scientific Initiatives Committee.
All consecutive patients included into the registry were study subjects in the present substudy. Patients were stratified into two groups based on the presence (Group 1) or absence (Group 2) of abandoned leads. Endpoints were: the safety of TLE (as defined by procedure related major complications and deaths observed during the hospitalization), the radiological and clinical success rates of TLE and all cause in-hospital major complications as well as baseline patient and lead characteristics, indications for TLE, techniques, and tools used. Predictors of success and major complications were also evaluated. Success rates and complications were compared between Group 1 and Group 2 patients.
Definitions published in the guideline documents by EHRA2 and by HRS3 were used to define procedural approaches, techniques, and outcomes. Sheaths were classified as mechanical non-powered (polypropylene or similar material) or powered (laser, radiofrequency electrosurgical, or controlled-rotational with threaded tip devices). Transvenous lead extraction safety and efficacy were calculated by evaluating the rate of procedure related complications (major and minor) and success/failures (radiological and clinical). Major complications were defined as those related to the procedure that were life threatening or resulted in death, or any unexpected event that caused persistent or significant disability, or any event that required significant surgical intervention to prevent any of outcomes listed above. Radiological failure (considered for each lead) was defined when more than a 4 cm length of a lead was abandoned after a removal attempt, partial success when less than a 4 cm of a lead remained in the patient body and complete success when the lead was completely removed. Clinical failure (considered for each patient) was defined when, as either a procedure related major complication or a failure to achieve the clinical outcome for which the TLE was scheduled, occurred.
Statistical analysis
Descriptive analysis was applied to both continuous and categorical variables. Results were summarized by the presence (Group 1) or absence (Group 2) of abandoned leads at the time of extraction procedure. Continuous variables were reported as mean ± standard deviation and as median and interquartile range. Among-group comparisons were made using a non-parametric test (Mann–Whitney test). Categorical variables were reported as percentages (without missing values if applicable). Among-group comparisons were made using a χ2 test or the Fisher’s exact test (if any expected cell count was less than five or to compare endpoints). A stepwise algorithm was used to determine the predictors of major procedure related complications (Model A), clinical failure (Model B), and all-cause mortality (Model C) including into the models all the candidate variables (variables with P-value of <0.05 in univariate analyses, except those with more than 20% of missing data, and variables considered of relevant clinical interest). Univariate and multivariate Cox regressions were performed for models A and C where the time-to-event was respectively defined as the time from TLE to the date of the first major complication event (among death, stroke, cardiac/vascular avulsion or tear, pulmonary embolism, respiratory arrest, anaesthesia, and pacing system related infection of a previously non-infected site) for Model A and the date of death during hospital stay for Model C. Logistic regressions were performed for the clinical failure outcome. A two-sided P-value of 0.05 was considered as statistically significant. Optimal cut-off values of parameters were determined by the analysis of receiver-operating characteristic curves using the Youden index. All the analyses were performed using SAS statistical software version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
During the study period, 422 (12.02%) patients had abandoned leads (Group 1) out of 3510 who underwent TLE.
Baseline characteristics, stratified by the presence or absence of abandoned leads at the time of extraction, are reported in Tables 1 and 2. Patients in Group 1 were older [66.81 ± 13.93, 70 (60–77) vs. 64.62 ± 15.82 years, 67 (57–76), P = 0.0170] and more likely to have ICD devices (52.37% vs. 46.44%, P = 0.0220) as opposed to PM, and cardiac resynchronization therapy (CR) devices (25.59% vs. 20.23% P = 0.0190) as opposed to non-CRT devices. In Group 1, the number of total leads were higher (≥3 leads in 77.25%) than in patients in Group 2 (≥3 leads in 21.41%), P < 0.0001, and previous attempts of lead extraction was greater (11.61% in Group 1 vs. 3.95% in Group 2, P < 0.0001). Device infection as the indication of TLE (78.81% vs. 49.82%, P < 0.0001) and vegetations (24.64% vs. 15.35%, P < 0.0001) were more common in Group 1. Among non-infective indications of TLE (Table 2), the prevalence of non-functional leads and recalled leads was higher in Group 1; however, the prevalence of venous thrombosis, upgrading indications and magnetic resonance imaging indications was not higher in Group 1 in comparison to Group 2.
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Age (years), median (IQR) | 68.00 (57.00–76.00) | 70.00 (60.00–77.00) | 67.00 (57.00–76.00) | 0.0170 |
| Male gender, n/N (%) | 2539/3510 (72.34) | 319/422 (75.59) | 2220/3088 (71.89) | 0.1108 |
| Body mass index (kg/m2), median (IQR) | 26.10 (23.50–29.30) | 26.50 (24.20–29.10) | 26.10 (23.50–29.30) | 0.1750 |
| LVEF (%), median (IQR) | 50.00 (33.00–60.00) | 45.00 (32.00–56.00) | 50.00 (33.00–60.00) | 0.0719 |
| NYHA Class III–IV, n/N (%) | 486/3472 (14.00) | 68/418 (16.27) | 418/3054 (13.69) | 0.1537 |
| Coronary artery disease, n/N (%) | 1375/3482 (39.49) | 175/419 (41.77) | 1200/3063 (39.18) | 0.3092 |
| Valvular heart disease, n/N (%) | 514/3500 (14.69) | 76/422 (18.01) | 438/3078 (14.23) | 0.0396 |
| Dilated cardiomyopathy, n/N (%) | 917/3492 (26.26) | 116/420 (27.62) | 801/3072 (26.07) | 0.4997 |
| Previous sternotomy, n/N (%) | 596/3504 (17.01) | 89/422 (21.09) | 507/3082 (16.45) | 0.0173 |
| Hypertension, n/N (%) | 1888/3478 (54.28) | 222/419 (52.98) | 1666/3059 (54.46) | 0.5687 |
| Diabetes mellitus, n/N (%) | 781/3487 (22.40) | 99/419 (23.63) | 682/3068 (22.23) | 0.5196 |
| Chronic heart failure, n/N (%) | 1557/3488 (44.64) | 196/419 (46.78) | 1361/3069 (44.35) | 0.3476 |
| Chronic kidney disease, n/N (%) | 613/3493 (17.55) | 87/419 (20.76) | 526/3074 (17.11) | 0.0652 |
| Chronic obstructive pulmonary disease, n/N (%) | 297/3483 (8.53) | 37/417 (8.87) | 260/3066 (8.48) | 0.7875 |
| ICD, n/N (%) | 1655/3510 (47.15) | 221/422 (52.37) | 1434/3088 (46.44) | 0.0220 |
| CRT-D, n/N (%) | 606/1655 (36.62) | 102/221 (46.15) | 504/1434 (35.15) | 0.0109 |
| Pacemakers | 1848/3510 (52.65) | 194/422 (45.97) | 1654/3088 (53.56) | 0.0033 |
| CRT-P, n/N (%) | 127/1848 (6.87) | 6/194 (3.09) | 121/1654 (7.32) | 0.0052 |
| Number of total leads (class) ≥3, n/N (%) | 987/3509 (28.13) | 326/422 (77.25) | 661/3087 (21.41) | <0.0001 |
| Number of leads from both left and right side, n/N (%) | 179/3509 (5.10) | 60/422 (14.22) | 119/3087 (3.85) | <0.0001 |
| Vegetations (where TEE/TTE were performed), n/N (%) | 578/3510 (16.47) | 104/422 (24.64) | 474/3088 (15.35) | <0.0001 |
| Anticoagulation, n/N (%) | 1302/3510 (37.09) | 167/422 (39.57) | 1135/3088 (36.76) | 0.2609 |
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Age (years), median (IQR) | 68.00 (57.00–76.00) | 70.00 (60.00–77.00) | 67.00 (57.00–76.00) | 0.0170 |
| Male gender, n/N (%) | 2539/3510 (72.34) | 319/422 (75.59) | 2220/3088 (71.89) | 0.1108 |
| Body mass index (kg/m2), median (IQR) | 26.10 (23.50–29.30) | 26.50 (24.20–29.10) | 26.10 (23.50–29.30) | 0.1750 |
| LVEF (%), median (IQR) | 50.00 (33.00–60.00) | 45.00 (32.00–56.00) | 50.00 (33.00–60.00) | 0.0719 |
| NYHA Class III–IV, n/N (%) | 486/3472 (14.00) | 68/418 (16.27) | 418/3054 (13.69) | 0.1537 |
| Coronary artery disease, n/N (%) | 1375/3482 (39.49) | 175/419 (41.77) | 1200/3063 (39.18) | 0.3092 |
| Valvular heart disease, n/N (%) | 514/3500 (14.69) | 76/422 (18.01) | 438/3078 (14.23) | 0.0396 |
| Dilated cardiomyopathy, n/N (%) | 917/3492 (26.26) | 116/420 (27.62) | 801/3072 (26.07) | 0.4997 |
| Previous sternotomy, n/N (%) | 596/3504 (17.01) | 89/422 (21.09) | 507/3082 (16.45) | 0.0173 |
| Hypertension, n/N (%) | 1888/3478 (54.28) | 222/419 (52.98) | 1666/3059 (54.46) | 0.5687 |
| Diabetes mellitus, n/N (%) | 781/3487 (22.40) | 99/419 (23.63) | 682/3068 (22.23) | 0.5196 |
| Chronic heart failure, n/N (%) | 1557/3488 (44.64) | 196/419 (46.78) | 1361/3069 (44.35) | 0.3476 |
| Chronic kidney disease, n/N (%) | 613/3493 (17.55) | 87/419 (20.76) | 526/3074 (17.11) | 0.0652 |
| Chronic obstructive pulmonary disease, n/N (%) | 297/3483 (8.53) | 37/417 (8.87) | 260/3066 (8.48) | 0.7875 |
| ICD, n/N (%) | 1655/3510 (47.15) | 221/422 (52.37) | 1434/3088 (46.44) | 0.0220 |
| CRT-D, n/N (%) | 606/1655 (36.62) | 102/221 (46.15) | 504/1434 (35.15) | 0.0109 |
| Pacemakers | 1848/3510 (52.65) | 194/422 (45.97) | 1654/3088 (53.56) | 0.0033 |
| CRT-P, n/N (%) | 127/1848 (6.87) | 6/194 (3.09) | 121/1654 (7.32) | 0.0052 |
| Number of total leads (class) ≥3, n/N (%) | 987/3509 (28.13) | 326/422 (77.25) | 661/3087 (21.41) | <0.0001 |
| Number of leads from both left and right side, n/N (%) | 179/3509 (5.10) | 60/422 (14.22) | 119/3087 (3.85) | <0.0001 |
| Vegetations (where TEE/TTE were performed), n/N (%) | 578/3510 (16.47) | 104/422 (24.64) | 474/3088 (15.35) | <0.0001 |
| Anticoagulation, n/N (%) | 1302/3510 (37.09) | 167/422 (39.57) | 1135/3088 (36.76) | 0.2609 |
CRT-D, cardiac resynchronization therapy-defibrillator; CRT-P, cardiac resynchronization therapy-pacemaker; ICD, implantable cardioverter-defibrillator; IQR, interquartile range; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; TEE, transesophageal echocardiogram; TTE, transthoracic echocardiogram.
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Age (years), median (IQR) | 68.00 (57.00–76.00) | 70.00 (60.00–77.00) | 67.00 (57.00–76.00) | 0.0170 |
| Male gender, n/N (%) | 2539/3510 (72.34) | 319/422 (75.59) | 2220/3088 (71.89) | 0.1108 |
| Body mass index (kg/m2), median (IQR) | 26.10 (23.50–29.30) | 26.50 (24.20–29.10) | 26.10 (23.50–29.30) | 0.1750 |
| LVEF (%), median (IQR) | 50.00 (33.00–60.00) | 45.00 (32.00–56.00) | 50.00 (33.00–60.00) | 0.0719 |
| NYHA Class III–IV, n/N (%) | 486/3472 (14.00) | 68/418 (16.27) | 418/3054 (13.69) | 0.1537 |
| Coronary artery disease, n/N (%) | 1375/3482 (39.49) | 175/419 (41.77) | 1200/3063 (39.18) | 0.3092 |
| Valvular heart disease, n/N (%) | 514/3500 (14.69) | 76/422 (18.01) | 438/3078 (14.23) | 0.0396 |
| Dilated cardiomyopathy, n/N (%) | 917/3492 (26.26) | 116/420 (27.62) | 801/3072 (26.07) | 0.4997 |
| Previous sternotomy, n/N (%) | 596/3504 (17.01) | 89/422 (21.09) | 507/3082 (16.45) | 0.0173 |
| Hypertension, n/N (%) | 1888/3478 (54.28) | 222/419 (52.98) | 1666/3059 (54.46) | 0.5687 |
| Diabetes mellitus, n/N (%) | 781/3487 (22.40) | 99/419 (23.63) | 682/3068 (22.23) | 0.5196 |
| Chronic heart failure, n/N (%) | 1557/3488 (44.64) | 196/419 (46.78) | 1361/3069 (44.35) | 0.3476 |
| Chronic kidney disease, n/N (%) | 613/3493 (17.55) | 87/419 (20.76) | 526/3074 (17.11) | 0.0652 |
| Chronic obstructive pulmonary disease, n/N (%) | 297/3483 (8.53) | 37/417 (8.87) | 260/3066 (8.48) | 0.7875 |
| ICD, n/N (%) | 1655/3510 (47.15) | 221/422 (52.37) | 1434/3088 (46.44) | 0.0220 |
| CRT-D, n/N (%) | 606/1655 (36.62) | 102/221 (46.15) | 504/1434 (35.15) | 0.0109 |
| Pacemakers | 1848/3510 (52.65) | 194/422 (45.97) | 1654/3088 (53.56) | 0.0033 |
| CRT-P, n/N (%) | 127/1848 (6.87) | 6/194 (3.09) | 121/1654 (7.32) | 0.0052 |
| Number of total leads (class) ≥3, n/N (%) | 987/3509 (28.13) | 326/422 (77.25) | 661/3087 (21.41) | <0.0001 |
| Number of leads from both left and right side, n/N (%) | 179/3509 (5.10) | 60/422 (14.22) | 119/3087 (3.85) | <0.0001 |
| Vegetations (where TEE/TTE were performed), n/N (%) | 578/3510 (16.47) | 104/422 (24.64) | 474/3088 (15.35) | <0.0001 |
| Anticoagulation, n/N (%) | 1302/3510 (37.09) | 167/422 (39.57) | 1135/3088 (36.76) | 0.2609 |
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Age (years), median (IQR) | 68.00 (57.00–76.00) | 70.00 (60.00–77.00) | 67.00 (57.00–76.00) | 0.0170 |
| Male gender, n/N (%) | 2539/3510 (72.34) | 319/422 (75.59) | 2220/3088 (71.89) | 0.1108 |
| Body mass index (kg/m2), median (IQR) | 26.10 (23.50–29.30) | 26.50 (24.20–29.10) | 26.10 (23.50–29.30) | 0.1750 |
| LVEF (%), median (IQR) | 50.00 (33.00–60.00) | 45.00 (32.00–56.00) | 50.00 (33.00–60.00) | 0.0719 |
| NYHA Class III–IV, n/N (%) | 486/3472 (14.00) | 68/418 (16.27) | 418/3054 (13.69) | 0.1537 |
| Coronary artery disease, n/N (%) | 1375/3482 (39.49) | 175/419 (41.77) | 1200/3063 (39.18) | 0.3092 |
| Valvular heart disease, n/N (%) | 514/3500 (14.69) | 76/422 (18.01) | 438/3078 (14.23) | 0.0396 |
| Dilated cardiomyopathy, n/N (%) | 917/3492 (26.26) | 116/420 (27.62) | 801/3072 (26.07) | 0.4997 |
| Previous sternotomy, n/N (%) | 596/3504 (17.01) | 89/422 (21.09) | 507/3082 (16.45) | 0.0173 |
| Hypertension, n/N (%) | 1888/3478 (54.28) | 222/419 (52.98) | 1666/3059 (54.46) | 0.5687 |
| Diabetes mellitus, n/N (%) | 781/3487 (22.40) | 99/419 (23.63) | 682/3068 (22.23) | 0.5196 |
| Chronic heart failure, n/N (%) | 1557/3488 (44.64) | 196/419 (46.78) | 1361/3069 (44.35) | 0.3476 |
| Chronic kidney disease, n/N (%) | 613/3493 (17.55) | 87/419 (20.76) | 526/3074 (17.11) | 0.0652 |
| Chronic obstructive pulmonary disease, n/N (%) | 297/3483 (8.53) | 37/417 (8.87) | 260/3066 (8.48) | 0.7875 |
| ICD, n/N (%) | 1655/3510 (47.15) | 221/422 (52.37) | 1434/3088 (46.44) | 0.0220 |
| CRT-D, n/N (%) | 606/1655 (36.62) | 102/221 (46.15) | 504/1434 (35.15) | 0.0109 |
| Pacemakers | 1848/3510 (52.65) | 194/422 (45.97) | 1654/3088 (53.56) | 0.0033 |
| CRT-P, n/N (%) | 127/1848 (6.87) | 6/194 (3.09) | 121/1654 (7.32) | 0.0052 |
| Number of total leads (class) ≥3, n/N (%) | 987/3509 (28.13) | 326/422 (77.25) | 661/3087 (21.41) | <0.0001 |
| Number of leads from both left and right side, n/N (%) | 179/3509 (5.10) | 60/422 (14.22) | 119/3087 (3.85) | <0.0001 |
| Vegetations (where TEE/TTE were performed), n/N (%) | 578/3510 (16.47) | 104/422 (24.64) | 474/3088 (15.35) | <0.0001 |
| Anticoagulation, n/N (%) | 1302/3510 (37.09) | 167/422 (39.57) | 1135/3088 (36.76) | 0.2609 |
CRT-D, cardiac resynchronization therapy-defibrillator; CRT-P, cardiac resynchronization therapy-pacemaker; ICD, implantable cardioverter-defibrillator; IQR, interquartile range; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; TEE, transesophageal echocardiogram; TTE, transthoracic echocardiogram.
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Lead and device history, n/N (%) | ||||
| Previous complications to CIED | 1109/3510 (31.60) | 275/422 (65.17) | 834/3088 (27.01) | <0.0001 |
| First implant | 1540/3510 (43.87) | 18/422 (4.27) | 1522/3088 (49.29) | <0.0001 |
| Revision or upgrades | 1341/3510 (38.21) | 344/422 (81.52) | 997/3088 (32.29) | <0.0001 |
| Previous attempt of lead extraction | 171/3510 (4.87) | 49/422 (11.61) | 122/3088 (3.95) | <0.0001 |
| Previous complications to CIED | 1109/3510 (31.60) | 275/422 (65.17) | 834/3088 (27.01) | <0.0001 |
| Lead number and location, n/N (%) | ||||
| Number of leads in RA: 1 | 2503/3509 (71.33) | 261/422 (61.85) | 2242/3087 (72.63) | <0.0001 |
| Number of leads in RA: ≥2 | 124/3509 (3.53) | 83/422 (18.77) | 41/3087 (1.33) | |
| Number of leads in RV: 1 | 2929/3509 (83.47) | 85/422 (20.14) | 2844/3087 (92.13) | <0.0001 |
| Number of leads in RV: ≥2 | 488/3509 (13.90) | 328/422 (77.72) | 160/3087 (5.18) | |
| Number of leads in CS: 1 | 677/3509 (19.29) | 97/422 (22.99) | 580/3087 (18.79) | <0.0001 |
| Number of leads in CS: 2 | 15/3509 (0.43) | 13/422 (3.08) | 2/3087 (0.06) | |
| Indication for lead extraction, n/N (%) | ||||
| Infections | 1865/3499 (53.30) | 331/420 (78.81) | 1534/3079 (49.82) | <0.0001 |
| Systemic infections | 680/3499 (19.43) | 113/420 (26.90) | 567/3079 (18.42) | <0.0001 |
| Local infections | 1170/3499 (33.44) | 216/420 (51.43) | 954/3079 (30.98) | <0.0001 |
| No infection | 1645/3510 (46.87) | 91/422 (21.56) | 1554/3088 (50.32) | <0.0001 |
| Non infective indications (more than 1 indication for extraction could be present in a given patient), n/N (%) | ||||
| Chronic pain | 180/3510 (5.13) | 30/422 (7.11) | 150/3088 (4.86) | 0.0492 |
| Thrombosis or venous stenosis | 160/3510 (4.56) | 20/422 (4.74) | 140/3088 (4.53) | 0.8493 |
| Signs and symptoms of venous occlusion | 105/160 (65.63) | 15/20 (75.00) | 90/140 (64.29) | 0.3453 |
| Functional leads | 2023/3510 (57.64) | 273/422 (64.69) | 1750/3088 (56.67) | 0.0017 |
| Non-functional leads | 1331/3510 (37.92) | 223/422 (52.84) | 1108/3088 (35.88) | <0.0001 |
| Recalled leads | 440/3510 (12.54) | 73/422 (17.30) | 367/3088 (11.88) | 0.0016 |
| Upgrading indication | 248/3510 (7.07) | 14/422 (3.32) | 234/3088 (7.58) | 0.0013 |
| MRI indication | 26/3510 (0.74) | 4/422 (0.95) | 22/3088 (0.71) | 0.5967 |
| Other | 54/3510 (1.54) | 4/422 (0.95) | 50/3088 (1.62) | 0.2932 |
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Lead and device history, n/N (%) | ||||
| Previous complications to CIED | 1109/3510 (31.60) | 275/422 (65.17) | 834/3088 (27.01) | <0.0001 |
| First implant | 1540/3510 (43.87) | 18/422 (4.27) | 1522/3088 (49.29) | <0.0001 |
| Revision or upgrades | 1341/3510 (38.21) | 344/422 (81.52) | 997/3088 (32.29) | <0.0001 |
| Previous attempt of lead extraction | 171/3510 (4.87) | 49/422 (11.61) | 122/3088 (3.95) | <0.0001 |
| Previous complications to CIED | 1109/3510 (31.60) | 275/422 (65.17) | 834/3088 (27.01) | <0.0001 |
| Lead number and location, n/N (%) | ||||
| Number of leads in RA: 1 | 2503/3509 (71.33) | 261/422 (61.85) | 2242/3087 (72.63) | <0.0001 |
| Number of leads in RA: ≥2 | 124/3509 (3.53) | 83/422 (18.77) | 41/3087 (1.33) | |
| Number of leads in RV: 1 | 2929/3509 (83.47) | 85/422 (20.14) | 2844/3087 (92.13) | <0.0001 |
| Number of leads in RV: ≥2 | 488/3509 (13.90) | 328/422 (77.72) | 160/3087 (5.18) | |
| Number of leads in CS: 1 | 677/3509 (19.29) | 97/422 (22.99) | 580/3087 (18.79) | <0.0001 |
| Number of leads in CS: 2 | 15/3509 (0.43) | 13/422 (3.08) | 2/3087 (0.06) | |
| Indication for lead extraction, n/N (%) | ||||
| Infections | 1865/3499 (53.30) | 331/420 (78.81) | 1534/3079 (49.82) | <0.0001 |
| Systemic infections | 680/3499 (19.43) | 113/420 (26.90) | 567/3079 (18.42) | <0.0001 |
| Local infections | 1170/3499 (33.44) | 216/420 (51.43) | 954/3079 (30.98) | <0.0001 |
| No infection | 1645/3510 (46.87) | 91/422 (21.56) | 1554/3088 (50.32) | <0.0001 |
| Non infective indications (more than 1 indication for extraction could be present in a given patient), n/N (%) | ||||
| Chronic pain | 180/3510 (5.13) | 30/422 (7.11) | 150/3088 (4.86) | 0.0492 |
| Thrombosis or venous stenosis | 160/3510 (4.56) | 20/422 (4.74) | 140/3088 (4.53) | 0.8493 |
| Signs and symptoms of venous occlusion | 105/160 (65.63) | 15/20 (75.00) | 90/140 (64.29) | 0.3453 |
| Functional leads | 2023/3510 (57.64) | 273/422 (64.69) | 1750/3088 (56.67) | 0.0017 |
| Non-functional leads | 1331/3510 (37.92) | 223/422 (52.84) | 1108/3088 (35.88) | <0.0001 |
| Recalled leads | 440/3510 (12.54) | 73/422 (17.30) | 367/3088 (11.88) | 0.0016 |
| Upgrading indication | 248/3510 (7.07) | 14/422 (3.32) | 234/3088 (7.58) | 0.0013 |
| MRI indication | 26/3510 (0.74) | 4/422 (0.95) | 22/3088 (0.71) | 0.5967 |
| Other | 54/3510 (1.54) | 4/422 (0.95) | 50/3088 (1.62) | 0.2932 |
CIED, cardiac implantable electronic device; CS, coronary sinus; MRI, magnetic resonance imaging; RA, right atrium; RV, right ventricle.
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Lead and device history, n/N (%) | ||||
| Previous complications to CIED | 1109/3510 (31.60) | 275/422 (65.17) | 834/3088 (27.01) | <0.0001 |
| First implant | 1540/3510 (43.87) | 18/422 (4.27) | 1522/3088 (49.29) | <0.0001 |
| Revision or upgrades | 1341/3510 (38.21) | 344/422 (81.52) | 997/3088 (32.29) | <0.0001 |
| Previous attempt of lead extraction | 171/3510 (4.87) | 49/422 (11.61) | 122/3088 (3.95) | <0.0001 |
| Previous complications to CIED | 1109/3510 (31.60) | 275/422 (65.17) | 834/3088 (27.01) | <0.0001 |
| Lead number and location, n/N (%) | ||||
| Number of leads in RA: 1 | 2503/3509 (71.33) | 261/422 (61.85) | 2242/3087 (72.63) | <0.0001 |
| Number of leads in RA: ≥2 | 124/3509 (3.53) | 83/422 (18.77) | 41/3087 (1.33) | |
| Number of leads in RV: 1 | 2929/3509 (83.47) | 85/422 (20.14) | 2844/3087 (92.13) | <0.0001 |
| Number of leads in RV: ≥2 | 488/3509 (13.90) | 328/422 (77.72) | 160/3087 (5.18) | |
| Number of leads in CS: 1 | 677/3509 (19.29) | 97/422 (22.99) | 580/3087 (18.79) | <0.0001 |
| Number of leads in CS: 2 | 15/3509 (0.43) | 13/422 (3.08) | 2/3087 (0.06) | |
| Indication for lead extraction, n/N (%) | ||||
| Infections | 1865/3499 (53.30) | 331/420 (78.81) | 1534/3079 (49.82) | <0.0001 |
| Systemic infections | 680/3499 (19.43) | 113/420 (26.90) | 567/3079 (18.42) | <0.0001 |
| Local infections | 1170/3499 (33.44) | 216/420 (51.43) | 954/3079 (30.98) | <0.0001 |
| No infection | 1645/3510 (46.87) | 91/422 (21.56) | 1554/3088 (50.32) | <0.0001 |
| Non infective indications (more than 1 indication for extraction could be present in a given patient), n/N (%) | ||||
| Chronic pain | 180/3510 (5.13) | 30/422 (7.11) | 150/3088 (4.86) | 0.0492 |
| Thrombosis or venous stenosis | 160/3510 (4.56) | 20/422 (4.74) | 140/3088 (4.53) | 0.8493 |
| Signs and symptoms of venous occlusion | 105/160 (65.63) | 15/20 (75.00) | 90/140 (64.29) | 0.3453 |
| Functional leads | 2023/3510 (57.64) | 273/422 (64.69) | 1750/3088 (56.67) | 0.0017 |
| Non-functional leads | 1331/3510 (37.92) | 223/422 (52.84) | 1108/3088 (35.88) | <0.0001 |
| Recalled leads | 440/3510 (12.54) | 73/422 (17.30) | 367/3088 (11.88) | 0.0016 |
| Upgrading indication | 248/3510 (7.07) | 14/422 (3.32) | 234/3088 (7.58) | 0.0013 |
| MRI indication | 26/3510 (0.74) | 4/422 (0.95) | 22/3088 (0.71) | 0.5967 |
| Other | 54/3510 (1.54) | 4/422 (0.95) | 50/3088 (1.62) | 0.2932 |
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Lead and device history, n/N (%) | ||||
| Previous complications to CIED | 1109/3510 (31.60) | 275/422 (65.17) | 834/3088 (27.01) | <0.0001 |
| First implant | 1540/3510 (43.87) | 18/422 (4.27) | 1522/3088 (49.29) | <0.0001 |
| Revision or upgrades | 1341/3510 (38.21) | 344/422 (81.52) | 997/3088 (32.29) | <0.0001 |
| Previous attempt of lead extraction | 171/3510 (4.87) | 49/422 (11.61) | 122/3088 (3.95) | <0.0001 |
| Previous complications to CIED | 1109/3510 (31.60) | 275/422 (65.17) | 834/3088 (27.01) | <0.0001 |
| Lead number and location, n/N (%) | ||||
| Number of leads in RA: 1 | 2503/3509 (71.33) | 261/422 (61.85) | 2242/3087 (72.63) | <0.0001 |
| Number of leads in RA: ≥2 | 124/3509 (3.53) | 83/422 (18.77) | 41/3087 (1.33) | |
| Number of leads in RV: 1 | 2929/3509 (83.47) | 85/422 (20.14) | 2844/3087 (92.13) | <0.0001 |
| Number of leads in RV: ≥2 | 488/3509 (13.90) | 328/422 (77.72) | 160/3087 (5.18) | |
| Number of leads in CS: 1 | 677/3509 (19.29) | 97/422 (22.99) | 580/3087 (18.79) | <0.0001 |
| Number of leads in CS: 2 | 15/3509 (0.43) | 13/422 (3.08) | 2/3087 (0.06) | |
| Indication for lead extraction, n/N (%) | ||||
| Infections | 1865/3499 (53.30) | 331/420 (78.81) | 1534/3079 (49.82) | <0.0001 |
| Systemic infections | 680/3499 (19.43) | 113/420 (26.90) | 567/3079 (18.42) | <0.0001 |
| Local infections | 1170/3499 (33.44) | 216/420 (51.43) | 954/3079 (30.98) | <0.0001 |
| No infection | 1645/3510 (46.87) | 91/422 (21.56) | 1554/3088 (50.32) | <0.0001 |
| Non infective indications (more than 1 indication for extraction could be present in a given patient), n/N (%) | ||||
| Chronic pain | 180/3510 (5.13) | 30/422 (7.11) | 150/3088 (4.86) | 0.0492 |
| Thrombosis or venous stenosis | 160/3510 (4.56) | 20/422 (4.74) | 140/3088 (4.53) | 0.8493 |
| Signs and symptoms of venous occlusion | 105/160 (65.63) | 15/20 (75.00) | 90/140 (64.29) | 0.3453 |
| Functional leads | 2023/3510 (57.64) | 273/422 (64.69) | 1750/3088 (56.67) | 0.0017 |
| Non-functional leads | 1331/3510 (37.92) | 223/422 (52.84) | 1108/3088 (35.88) | <0.0001 |
| Recalled leads | 440/3510 (12.54) | 73/422 (17.30) | 367/3088 (11.88) | 0.0016 |
| Upgrading indication | 248/3510 (7.07) | 14/422 (3.32) | 234/3088 (7.58) | 0.0013 |
| MRI indication | 26/3510 (0.74) | 4/422 (0.95) | 22/3088 (0.71) | 0.5967 |
| Other | 54/3510 (1.54) | 4/422 (0.95) | 50/3088 (1.62) | 0.2932 |
CIED, cardiac implantable electronic device; CS, coronary sinus; MRI, magnetic resonance imaging; RA, right atrium; RV, right ventricle.
Characteristics of the TLE procedures and procedural outcomes are presented in Table 3.
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Clinical success, n/N (%) | 3362/3510 (95.78) | 379/422 (89.81) | 2983/3088 (96.60) | <0.0001 |
| Major complications including death, n/N (%) | 95/3510 (2.71) | 23/422 (5.45) | 72/3088 (2.33) | 0.0007 |
| Radiological failure, n/N (%) | 72/3510 (2.05) | 20/422 (4.74) | 52/3086 (1.69) | 0.0003 |
| Procedure related major complications including deaths, n/N (%) | 58/3510 (1.65) | 14/422 (3.32) | 44/3088 (1.42) | 0.0123 |
| Intraprocedural, n/N (%) | 37/3510 (1.05) | 12/422 (2.84) | 25/3088 (0.81) | 0.0009 |
| Postprocedural, n/N (%) | 21/3510 (0.60) | 2/422 (0.47) | 19/3088 (0.62) | 1.0000 |
| All cause in-hospital major complications without deaths, n/N (%) | 95/3510 (2.71) | 23/422 (5.45) | 72/3088 (2.33) | 0.0007 |
| All cause in-hospital deaths, n/N (%) | 50/3510 (1.42) | 10/422 (2.37) | 40/3088 (1.30) | 0.1197 |
| Minor complications, n/N (%) | 174/3510 (4.96) | 35/422 (8.29) | 139/3088 (4.50) | 0.0017 |
| Number of leads extracted per patient, median (IQR) | 2.00 (1.00–2.00) | 3.00 (3.00–4.00) | 2.00 (1.00–2.00) | <0.0001 |
| Procedural time per patient (min), median (IQR) | 83.00 (57.00–120.00) | 120.00 (77.00–168.00) | 80.00 (55.00–120.00) | <0.0001 |
| Oldest lead dwelling time (years), median (IQR) | 6.00 (3.00–9.00) | 10.00 (6.00–15.00) | 5.00 (2.00–8.00) | <0.0001 |
| Oldest targeted lead dwelling time >5 years, n/N (%) | 685/3487 (19.64) | 188/418 (44.98) | 497/3069 (16.19) | <0.0001 |
| Patients with target ICD lead, n/N (%) | 1457/3508 (41.53) | 213/422 (50.47) | 1244/3086 (40.31) | <0.0001 |
| Femoral approach for at least one lead, n/N (%) | 150/3510 (4.27) | 44/422 (10.43) | 106/3088 (3.43) | <0.0001 |
| Powered sheaths, n/N (%) | 1091/3508 (31.10) | 214/422 (50.71) | 877/3086 (28.42) | <0.0001 |
| TLE with traction alone (for all leads), n/N (%) | 670/3463 (19.35) | 23/419 (5.49) | 647/3044 (21.25) | <0.0001 |
| Abandoned leads as solution for partial or failed extraction, n/N (%) | 197/3508 (5.62) | 55/422 (13.03) | 142/3086 (4.60) | <0.0001 |
| CIED implanted during hospital stay, n/N (%) | 2379/3510 (67.78) | 264/422 (62.56) | 2115/3088 (68.49) | 0.0144 |
| Number of total leads after reimplantation (class), ≥3, n/N (%) | 542/3454 (15.69) | 56/409 (13.69) | 486/3045 (15.96) | 0.2362 |
| Length of hospitalization (days), median (IQR) | 7.00 (3.00–14.00) | 11.00 (5.50–20.00) | 6.00 (3.00–13.00) | <0.0001 |
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Clinical success, n/N (%) | 3362/3510 (95.78) | 379/422 (89.81) | 2983/3088 (96.60) | <0.0001 |
| Major complications including death, n/N (%) | 95/3510 (2.71) | 23/422 (5.45) | 72/3088 (2.33) | 0.0007 |
| Radiological failure, n/N (%) | 72/3510 (2.05) | 20/422 (4.74) | 52/3086 (1.69) | 0.0003 |
| Procedure related major complications including deaths, n/N (%) | 58/3510 (1.65) | 14/422 (3.32) | 44/3088 (1.42) | 0.0123 |
| Intraprocedural, n/N (%) | 37/3510 (1.05) | 12/422 (2.84) | 25/3088 (0.81) | 0.0009 |
| Postprocedural, n/N (%) | 21/3510 (0.60) | 2/422 (0.47) | 19/3088 (0.62) | 1.0000 |
| All cause in-hospital major complications without deaths, n/N (%) | 95/3510 (2.71) | 23/422 (5.45) | 72/3088 (2.33) | 0.0007 |
| All cause in-hospital deaths, n/N (%) | 50/3510 (1.42) | 10/422 (2.37) | 40/3088 (1.30) | 0.1197 |
| Minor complications, n/N (%) | 174/3510 (4.96) | 35/422 (8.29) | 139/3088 (4.50) | 0.0017 |
| Number of leads extracted per patient, median (IQR) | 2.00 (1.00–2.00) | 3.00 (3.00–4.00) | 2.00 (1.00–2.00) | <0.0001 |
| Procedural time per patient (min), median (IQR) | 83.00 (57.00–120.00) | 120.00 (77.00–168.00) | 80.00 (55.00–120.00) | <0.0001 |
| Oldest lead dwelling time (years), median (IQR) | 6.00 (3.00–9.00) | 10.00 (6.00–15.00) | 5.00 (2.00–8.00) | <0.0001 |
| Oldest targeted lead dwelling time >5 years, n/N (%) | 685/3487 (19.64) | 188/418 (44.98) | 497/3069 (16.19) | <0.0001 |
| Patients with target ICD lead, n/N (%) | 1457/3508 (41.53) | 213/422 (50.47) | 1244/3086 (40.31) | <0.0001 |
| Femoral approach for at least one lead, n/N (%) | 150/3510 (4.27) | 44/422 (10.43) | 106/3088 (3.43) | <0.0001 |
| Powered sheaths, n/N (%) | 1091/3508 (31.10) | 214/422 (50.71) | 877/3086 (28.42) | <0.0001 |
| TLE with traction alone (for all leads), n/N (%) | 670/3463 (19.35) | 23/419 (5.49) | 647/3044 (21.25) | <0.0001 |
| Abandoned leads as solution for partial or failed extraction, n/N (%) | 197/3508 (5.62) | 55/422 (13.03) | 142/3086 (4.60) | <0.0001 |
| CIED implanted during hospital stay, n/N (%) | 2379/3510 (67.78) | 264/422 (62.56) | 2115/3088 (68.49) | 0.0144 |
| Number of total leads after reimplantation (class), ≥3, n/N (%) | 542/3454 (15.69) | 56/409 (13.69) | 486/3045 (15.96) | 0.2362 |
| Length of hospitalization (days), median (IQR) | 7.00 (3.00–14.00) | 11.00 (5.50–20.00) | 6.00 (3.00–13.00) | <0.0001 |
CIED, cardiac implantable electronic device; ICD, implantable cardioverter-defibrillator; IQR, interquartile range; TLE, transvenous lead extraction.
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Clinical success, n/N (%) | 3362/3510 (95.78) | 379/422 (89.81) | 2983/3088 (96.60) | <0.0001 |
| Major complications including death, n/N (%) | 95/3510 (2.71) | 23/422 (5.45) | 72/3088 (2.33) | 0.0007 |
| Radiological failure, n/N (%) | 72/3510 (2.05) | 20/422 (4.74) | 52/3086 (1.69) | 0.0003 |
| Procedure related major complications including deaths, n/N (%) | 58/3510 (1.65) | 14/422 (3.32) | 44/3088 (1.42) | 0.0123 |
| Intraprocedural, n/N (%) | 37/3510 (1.05) | 12/422 (2.84) | 25/3088 (0.81) | 0.0009 |
| Postprocedural, n/N (%) | 21/3510 (0.60) | 2/422 (0.47) | 19/3088 (0.62) | 1.0000 |
| All cause in-hospital major complications without deaths, n/N (%) | 95/3510 (2.71) | 23/422 (5.45) | 72/3088 (2.33) | 0.0007 |
| All cause in-hospital deaths, n/N (%) | 50/3510 (1.42) | 10/422 (2.37) | 40/3088 (1.30) | 0.1197 |
| Minor complications, n/N (%) | 174/3510 (4.96) | 35/422 (8.29) | 139/3088 (4.50) | 0.0017 |
| Number of leads extracted per patient, median (IQR) | 2.00 (1.00–2.00) | 3.00 (3.00–4.00) | 2.00 (1.00–2.00) | <0.0001 |
| Procedural time per patient (min), median (IQR) | 83.00 (57.00–120.00) | 120.00 (77.00–168.00) | 80.00 (55.00–120.00) | <0.0001 |
| Oldest lead dwelling time (years), median (IQR) | 6.00 (3.00–9.00) | 10.00 (6.00–15.00) | 5.00 (2.00–8.00) | <0.0001 |
| Oldest targeted lead dwelling time >5 years, n/N (%) | 685/3487 (19.64) | 188/418 (44.98) | 497/3069 (16.19) | <0.0001 |
| Patients with target ICD lead, n/N (%) | 1457/3508 (41.53) | 213/422 (50.47) | 1244/3086 (40.31) | <0.0001 |
| Femoral approach for at least one lead, n/N (%) | 150/3510 (4.27) | 44/422 (10.43) | 106/3088 (3.43) | <0.0001 |
| Powered sheaths, n/N (%) | 1091/3508 (31.10) | 214/422 (50.71) | 877/3086 (28.42) | <0.0001 |
| TLE with traction alone (for all leads), n/N (%) | 670/3463 (19.35) | 23/419 (5.49) | 647/3044 (21.25) | <0.0001 |
| Abandoned leads as solution for partial or failed extraction, n/N (%) | 197/3508 (5.62) | 55/422 (13.03) | 142/3086 (4.60) | <0.0001 |
| CIED implanted during hospital stay, n/N (%) | 2379/3510 (67.78) | 264/422 (62.56) | 2115/3088 (68.49) | 0.0144 |
| Number of total leads after reimplantation (class), ≥3, n/N (%) | 542/3454 (15.69) | 56/409 (13.69) | 486/3045 (15.96) | 0.2362 |
| Length of hospitalization (days), median (IQR) | 7.00 (3.00–14.00) | 11.00 (5.50–20.00) | 6.00 (3.00–13.00) | <0.0001 |
| Variables . | Total (N = 3510) . | Patients with abandoned leads (N = 422) . | Patients without abandoned leads (N = 3088) . | P-value . |
|---|---|---|---|---|
| Clinical success, n/N (%) | 3362/3510 (95.78) | 379/422 (89.81) | 2983/3088 (96.60) | <0.0001 |
| Major complications including death, n/N (%) | 95/3510 (2.71) | 23/422 (5.45) | 72/3088 (2.33) | 0.0007 |
| Radiological failure, n/N (%) | 72/3510 (2.05) | 20/422 (4.74) | 52/3086 (1.69) | 0.0003 |
| Procedure related major complications including deaths, n/N (%) | 58/3510 (1.65) | 14/422 (3.32) | 44/3088 (1.42) | 0.0123 |
| Intraprocedural, n/N (%) | 37/3510 (1.05) | 12/422 (2.84) | 25/3088 (0.81) | 0.0009 |
| Postprocedural, n/N (%) | 21/3510 (0.60) | 2/422 (0.47) | 19/3088 (0.62) | 1.0000 |
| All cause in-hospital major complications without deaths, n/N (%) | 95/3510 (2.71) | 23/422 (5.45) | 72/3088 (2.33) | 0.0007 |
| All cause in-hospital deaths, n/N (%) | 50/3510 (1.42) | 10/422 (2.37) | 40/3088 (1.30) | 0.1197 |
| Minor complications, n/N (%) | 174/3510 (4.96) | 35/422 (8.29) | 139/3088 (4.50) | 0.0017 |
| Number of leads extracted per patient, median (IQR) | 2.00 (1.00–2.00) | 3.00 (3.00–4.00) | 2.00 (1.00–2.00) | <0.0001 |
| Procedural time per patient (min), median (IQR) | 83.00 (57.00–120.00) | 120.00 (77.00–168.00) | 80.00 (55.00–120.00) | <0.0001 |
| Oldest lead dwelling time (years), median (IQR) | 6.00 (3.00–9.00) | 10.00 (6.00–15.00) | 5.00 (2.00–8.00) | <0.0001 |
| Oldest targeted lead dwelling time >5 years, n/N (%) | 685/3487 (19.64) | 188/418 (44.98) | 497/3069 (16.19) | <0.0001 |
| Patients with target ICD lead, n/N (%) | 1457/3508 (41.53) | 213/422 (50.47) | 1244/3086 (40.31) | <0.0001 |
| Femoral approach for at least one lead, n/N (%) | 150/3510 (4.27) | 44/422 (10.43) | 106/3088 (3.43) | <0.0001 |
| Powered sheaths, n/N (%) | 1091/3508 (31.10) | 214/422 (50.71) | 877/3086 (28.42) | <0.0001 |
| TLE with traction alone (for all leads), n/N (%) | 670/3463 (19.35) | 23/419 (5.49) | 647/3044 (21.25) | <0.0001 |
| Abandoned leads as solution for partial or failed extraction, n/N (%) | 197/3508 (5.62) | 55/422 (13.03) | 142/3086 (4.60) | <0.0001 |
| CIED implanted during hospital stay, n/N (%) | 2379/3510 (67.78) | 264/422 (62.56) | 2115/3088 (68.49) | 0.0144 |
| Number of total leads after reimplantation (class), ≥3, n/N (%) | 542/3454 (15.69) | 56/409 (13.69) | 486/3045 (15.96) | 0.2362 |
| Length of hospitalization (days), median (IQR) | 7.00 (3.00–14.00) | 11.00 (5.50–20.00) | 6.00 (3.00–13.00) | <0.0001 |
CIED, cardiac implantable electronic device; ICD, implantable cardioverter-defibrillator; IQR, interquartile range; TLE, transvenous lead extraction.
Given the presence of abandoned leads in Group 1, the dwell time of the oldest extracted lead was significantly longer in this group [10.94 ± 6.41 vs. 6.32 ± 5.28 years, 10 (6.00–15.00) vs. 5 (2.00–8.00) years, P < 0.0001], and the total number of extracted leads per patient [3.23 ± 0.86 vs. 1.66 ± 0.68, 3 (3.00–4.00) vs. 2 (1.00–2.00), P < 0.0001] was greater. Only a minority of leads in both groups were removed with simple traction whereas the vast majority of the cohort required simple and advanced extraction tools including powered sheaths and femoral approach. The need for extraction tools (94.51% vs. 78.75%, P < 0.0001), powered sheaths (50.71% vs. 28.42%, P < 0.0001), and femoral approach (10.43% vs. 3.43%, P < 0.0001) was significantly more common in Group 1.
Clinical failure (10.19% vs. 3.4%, P < 0.0001) and radiological failure (4.74% vs. 1.96%, P = 0.0003), major complication including deaths (5.45% vs. 2.33%, P = 0.0007) and procedure related major complications (3.32% vs. 1.42%, P = 0.0123) were significantly higher in Group 1.
In Table 4 are reported extracted leads characteristics in patient with abandoned and non-abandoned leads.
| Variables . | Total (N = 6495) . | Leads in patients with abandoned leads (N = 1363) . | Leads in patients without abandoned leads (N = 5132) . | P-value . |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Pacing leads (pacing and LV leads), unipolar, n/N (%) | 433/4917 (8.81) | 136/1060 (12.83) | 297/3857 (7.70) | <0.0001 |
| Pacing leads (pacing and LV leads), bipolar, n/N (%) | 4401/4917 (89.51) | 909/1060 (85.75) | 3492/3857 (90.54) | |
| Pacing leads (pacing and LV leads), tripolar, n/N (%) | 18/4917 (0.37) | 1/1060 (0.09) | 17/3857 (0.44) | |
| Pacing leads (pacing and LV leads), quadripolar, n/N (%) | 65/4917 (1.32) | 14/1060 (1.32) | 51/3857 (1.32) | |
| ICD leads, single coil, n/N (%) | 580/1576 (36.80) | 118/303 (38.94) | 462/1273 (36.29) | 0.3896 |
| ICD leads, dual coil, n/N (%) | 996/1576 (63.20) | 185/303 (61.06) | 811/1273 (63.71) | |
| Lead tip location, right atrium, n/N (%) | 2219/6493 (34.18) | 435/1363 (31.91) | 1784/5130 (34.78) | 0.0862 |
| Lead tip location, right ventricle, n/N (%) | 3587/6493 (55.24) | 775/1363 (56.86) | 2812/5130 (54.81) | |
| Lead tip location, coronary sinus/branches, n/N (%) | 547/6493 (8.42) | 115/1363 (8.44) | 432/5130 (8.42) | |
| Lead tip location, other, n/N (%) | 140/6493 (2.16) | 38/1363 (2.79) | 102/5130 (1.99) | |
| Fixation type, active, n/N (%) | 3381/6333 (53.39) | 687/1312 (52.36) | 2694/5021 (53.65) | 0.4035 |
| Fixation type, passive, n/N (%) | 2952/6333 (46.61) | 625/1312 (47.64) | 2327/5021 (46.35) | |
| Dwelling time (years), median (IQR) | 5.00 (2.00–9.00) | 7.00 (3.00–11.00) | 5.00 (2.00–8.00) | <0.0001 |
| Procedural characteristics, n/N (%) | ||||
| Technical issues during extraction | 971/6492 (14.96) | 247/1362 (18.14) | 724/5130 (14.11) | 0.0002 |
| Radiological outcome, complete | 6212/6493 (95.67) | 1269/1363 (93.10) | 4943/5130 (96.35) | <0.0001 |
| Radiological outcome, partial | 184/6493 (2.83) | 57/1363 (4.18) | 127/5130 (2.48) | |
| Radiological outcome, failure | 97/6493 (1.49) | 37/1363 (2.71) | 60/5130 (1.17) | |
| Lead removed with traction alone | 1741/6376 (27.31) | 323/1336 (24.18) | 1418/5040 (28.13) | 0.0038 |
| Mechanical not powered sheaths | 2359/6492 (36.34) | 390/1362 (28.63) | 1969/5130 (38.38) | <0.0001 |
| Powered sheaths | 1757/6492 (27.06) | 468/1362 (34.36) | 1289/5130 (25.13) | <0.0001 |
| Laser sheaths | 1250/6492 (19.25) | 340/1362 (24.96) | 910/5130 (17.74) | <0.0001 |
| Evolution mechanical dilator sheaths | 500/6492 (7.70) | 126/1362 (9.25) | 374/5130 (7.29) | 0.0158 |
| Outcomes, n/N (%) | ||||
| Clinical success | 6380/6493 (98.26) | 1311/1363 (96.18) | 5069/5130 (98.81) | <0.0001 |
| Complications | 601/6495 (9.25) | 207/1363 (15.19) | 394/5132 (7.68) | <0.0001 |
| Procedure related major complications including deaths | 127/6495 (1.96) | 46/1363 (3.37) | 81/5132 (1.58) | <0.0001 |
| Intraprocedural | 83/6495 (1.28) | 38/1363 (2.79) | 45/5132 (0.88) | <0.0001 |
| Postprocedural | 44/6495 (0.68) | 8/1363 (0.59) | 36/5132 (0.70) | 0.8524 |
| Variables . | Total (N = 6495) . | Leads in patients with abandoned leads (N = 1363) . | Leads in patients without abandoned leads (N = 5132) . | P-value . |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Pacing leads (pacing and LV leads), unipolar, n/N (%) | 433/4917 (8.81) | 136/1060 (12.83) | 297/3857 (7.70) | <0.0001 |
| Pacing leads (pacing and LV leads), bipolar, n/N (%) | 4401/4917 (89.51) | 909/1060 (85.75) | 3492/3857 (90.54) | |
| Pacing leads (pacing and LV leads), tripolar, n/N (%) | 18/4917 (0.37) | 1/1060 (0.09) | 17/3857 (0.44) | |
| Pacing leads (pacing and LV leads), quadripolar, n/N (%) | 65/4917 (1.32) | 14/1060 (1.32) | 51/3857 (1.32) | |
| ICD leads, single coil, n/N (%) | 580/1576 (36.80) | 118/303 (38.94) | 462/1273 (36.29) | 0.3896 |
| ICD leads, dual coil, n/N (%) | 996/1576 (63.20) | 185/303 (61.06) | 811/1273 (63.71) | |
| Lead tip location, right atrium, n/N (%) | 2219/6493 (34.18) | 435/1363 (31.91) | 1784/5130 (34.78) | 0.0862 |
| Lead tip location, right ventricle, n/N (%) | 3587/6493 (55.24) | 775/1363 (56.86) | 2812/5130 (54.81) | |
| Lead tip location, coronary sinus/branches, n/N (%) | 547/6493 (8.42) | 115/1363 (8.44) | 432/5130 (8.42) | |
| Lead tip location, other, n/N (%) | 140/6493 (2.16) | 38/1363 (2.79) | 102/5130 (1.99) | |
| Fixation type, active, n/N (%) | 3381/6333 (53.39) | 687/1312 (52.36) | 2694/5021 (53.65) | 0.4035 |
| Fixation type, passive, n/N (%) | 2952/6333 (46.61) | 625/1312 (47.64) | 2327/5021 (46.35) | |
| Dwelling time (years), median (IQR) | 5.00 (2.00–9.00) | 7.00 (3.00–11.00) | 5.00 (2.00–8.00) | <0.0001 |
| Procedural characteristics, n/N (%) | ||||
| Technical issues during extraction | 971/6492 (14.96) | 247/1362 (18.14) | 724/5130 (14.11) | 0.0002 |
| Radiological outcome, complete | 6212/6493 (95.67) | 1269/1363 (93.10) | 4943/5130 (96.35) | <0.0001 |
| Radiological outcome, partial | 184/6493 (2.83) | 57/1363 (4.18) | 127/5130 (2.48) | |
| Radiological outcome, failure | 97/6493 (1.49) | 37/1363 (2.71) | 60/5130 (1.17) | |
| Lead removed with traction alone | 1741/6376 (27.31) | 323/1336 (24.18) | 1418/5040 (28.13) | 0.0038 |
| Mechanical not powered sheaths | 2359/6492 (36.34) | 390/1362 (28.63) | 1969/5130 (38.38) | <0.0001 |
| Powered sheaths | 1757/6492 (27.06) | 468/1362 (34.36) | 1289/5130 (25.13) | <0.0001 |
| Laser sheaths | 1250/6492 (19.25) | 340/1362 (24.96) | 910/5130 (17.74) | <0.0001 |
| Evolution mechanical dilator sheaths | 500/6492 (7.70) | 126/1362 (9.25) | 374/5130 (7.29) | 0.0158 |
| Outcomes, n/N (%) | ||||
| Clinical success | 6380/6493 (98.26) | 1311/1363 (96.18) | 5069/5130 (98.81) | <0.0001 |
| Complications | 601/6495 (9.25) | 207/1363 (15.19) | 394/5132 (7.68) | <0.0001 |
| Procedure related major complications including deaths | 127/6495 (1.96) | 46/1363 (3.37) | 81/5132 (1.58) | <0.0001 |
| Intraprocedural | 83/6495 (1.28) | 38/1363 (2.79) | 45/5132 (0.88) | <0.0001 |
| Postprocedural | 44/6495 (0.68) | 8/1363 (0.59) | 36/5132 (0.70) | 0.8524 |
ICD, implantable cardioverter-defibrillator; IQR, interquartile range; LV, left ventricle.
| Variables . | Total (N = 6495) . | Leads in patients with abandoned leads (N = 1363) . | Leads in patients without abandoned leads (N = 5132) . | P-value . |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Pacing leads (pacing and LV leads), unipolar, n/N (%) | 433/4917 (8.81) | 136/1060 (12.83) | 297/3857 (7.70) | <0.0001 |
| Pacing leads (pacing and LV leads), bipolar, n/N (%) | 4401/4917 (89.51) | 909/1060 (85.75) | 3492/3857 (90.54) | |
| Pacing leads (pacing and LV leads), tripolar, n/N (%) | 18/4917 (0.37) | 1/1060 (0.09) | 17/3857 (0.44) | |
| Pacing leads (pacing and LV leads), quadripolar, n/N (%) | 65/4917 (1.32) | 14/1060 (1.32) | 51/3857 (1.32) | |
| ICD leads, single coil, n/N (%) | 580/1576 (36.80) | 118/303 (38.94) | 462/1273 (36.29) | 0.3896 |
| ICD leads, dual coil, n/N (%) | 996/1576 (63.20) | 185/303 (61.06) | 811/1273 (63.71) | |
| Lead tip location, right atrium, n/N (%) | 2219/6493 (34.18) | 435/1363 (31.91) | 1784/5130 (34.78) | 0.0862 |
| Lead tip location, right ventricle, n/N (%) | 3587/6493 (55.24) | 775/1363 (56.86) | 2812/5130 (54.81) | |
| Lead tip location, coronary sinus/branches, n/N (%) | 547/6493 (8.42) | 115/1363 (8.44) | 432/5130 (8.42) | |
| Lead tip location, other, n/N (%) | 140/6493 (2.16) | 38/1363 (2.79) | 102/5130 (1.99) | |
| Fixation type, active, n/N (%) | 3381/6333 (53.39) | 687/1312 (52.36) | 2694/5021 (53.65) | 0.4035 |
| Fixation type, passive, n/N (%) | 2952/6333 (46.61) | 625/1312 (47.64) | 2327/5021 (46.35) | |
| Dwelling time (years), median (IQR) | 5.00 (2.00–9.00) | 7.00 (3.00–11.00) | 5.00 (2.00–8.00) | <0.0001 |
| Procedural characteristics, n/N (%) | ||||
| Technical issues during extraction | 971/6492 (14.96) | 247/1362 (18.14) | 724/5130 (14.11) | 0.0002 |
| Radiological outcome, complete | 6212/6493 (95.67) | 1269/1363 (93.10) | 4943/5130 (96.35) | <0.0001 |
| Radiological outcome, partial | 184/6493 (2.83) | 57/1363 (4.18) | 127/5130 (2.48) | |
| Radiological outcome, failure | 97/6493 (1.49) | 37/1363 (2.71) | 60/5130 (1.17) | |
| Lead removed with traction alone | 1741/6376 (27.31) | 323/1336 (24.18) | 1418/5040 (28.13) | 0.0038 |
| Mechanical not powered sheaths | 2359/6492 (36.34) | 390/1362 (28.63) | 1969/5130 (38.38) | <0.0001 |
| Powered sheaths | 1757/6492 (27.06) | 468/1362 (34.36) | 1289/5130 (25.13) | <0.0001 |
| Laser sheaths | 1250/6492 (19.25) | 340/1362 (24.96) | 910/5130 (17.74) | <0.0001 |
| Evolution mechanical dilator sheaths | 500/6492 (7.70) | 126/1362 (9.25) | 374/5130 (7.29) | 0.0158 |
| Outcomes, n/N (%) | ||||
| Clinical success | 6380/6493 (98.26) | 1311/1363 (96.18) | 5069/5130 (98.81) | <0.0001 |
| Complications | 601/6495 (9.25) | 207/1363 (15.19) | 394/5132 (7.68) | <0.0001 |
| Procedure related major complications including deaths | 127/6495 (1.96) | 46/1363 (3.37) | 81/5132 (1.58) | <0.0001 |
| Intraprocedural | 83/6495 (1.28) | 38/1363 (2.79) | 45/5132 (0.88) | <0.0001 |
| Postprocedural | 44/6495 (0.68) | 8/1363 (0.59) | 36/5132 (0.70) | 0.8524 |
| Variables . | Total (N = 6495) . | Leads in patients with abandoned leads (N = 1363) . | Leads in patients without abandoned leads (N = 5132) . | P-value . |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Pacing leads (pacing and LV leads), unipolar, n/N (%) | 433/4917 (8.81) | 136/1060 (12.83) | 297/3857 (7.70) | <0.0001 |
| Pacing leads (pacing and LV leads), bipolar, n/N (%) | 4401/4917 (89.51) | 909/1060 (85.75) | 3492/3857 (90.54) | |
| Pacing leads (pacing and LV leads), tripolar, n/N (%) | 18/4917 (0.37) | 1/1060 (0.09) | 17/3857 (0.44) | |
| Pacing leads (pacing and LV leads), quadripolar, n/N (%) | 65/4917 (1.32) | 14/1060 (1.32) | 51/3857 (1.32) | |
| ICD leads, single coil, n/N (%) | 580/1576 (36.80) | 118/303 (38.94) | 462/1273 (36.29) | 0.3896 |
| ICD leads, dual coil, n/N (%) | 996/1576 (63.20) | 185/303 (61.06) | 811/1273 (63.71) | |
| Lead tip location, right atrium, n/N (%) | 2219/6493 (34.18) | 435/1363 (31.91) | 1784/5130 (34.78) | 0.0862 |
| Lead tip location, right ventricle, n/N (%) | 3587/6493 (55.24) | 775/1363 (56.86) | 2812/5130 (54.81) | |
| Lead tip location, coronary sinus/branches, n/N (%) | 547/6493 (8.42) | 115/1363 (8.44) | 432/5130 (8.42) | |
| Lead tip location, other, n/N (%) | 140/6493 (2.16) | 38/1363 (2.79) | 102/5130 (1.99) | |
| Fixation type, active, n/N (%) | 3381/6333 (53.39) | 687/1312 (52.36) | 2694/5021 (53.65) | 0.4035 |
| Fixation type, passive, n/N (%) | 2952/6333 (46.61) | 625/1312 (47.64) | 2327/5021 (46.35) | |
| Dwelling time (years), median (IQR) | 5.00 (2.00–9.00) | 7.00 (3.00–11.00) | 5.00 (2.00–8.00) | <0.0001 |
| Procedural characteristics, n/N (%) | ||||
| Technical issues during extraction | 971/6492 (14.96) | 247/1362 (18.14) | 724/5130 (14.11) | 0.0002 |
| Radiological outcome, complete | 6212/6493 (95.67) | 1269/1363 (93.10) | 4943/5130 (96.35) | <0.0001 |
| Radiological outcome, partial | 184/6493 (2.83) | 57/1363 (4.18) | 127/5130 (2.48) | |
| Radiological outcome, failure | 97/6493 (1.49) | 37/1363 (2.71) | 60/5130 (1.17) | |
| Lead removed with traction alone | 1741/6376 (27.31) | 323/1336 (24.18) | 1418/5040 (28.13) | 0.0038 |
| Mechanical not powered sheaths | 2359/6492 (36.34) | 390/1362 (28.63) | 1969/5130 (38.38) | <0.0001 |
| Powered sheaths | 1757/6492 (27.06) | 468/1362 (34.36) | 1289/5130 (25.13) | <0.0001 |
| Laser sheaths | 1250/6492 (19.25) | 340/1362 (24.96) | 910/5130 (17.74) | <0.0001 |
| Evolution mechanical dilator sheaths | 500/6492 (7.70) | 126/1362 (9.25) | 374/5130 (7.29) | 0.0158 |
| Outcomes, n/N (%) | ||||
| Clinical success | 6380/6493 (98.26) | 1311/1363 (96.18) | 5069/5130 (98.81) | <0.0001 |
| Complications | 601/6495 (9.25) | 207/1363 (15.19) | 394/5132 (7.68) | <0.0001 |
| Procedure related major complications including deaths | 127/6495 (1.96) | 46/1363 (3.37) | 81/5132 (1.58) | <0.0001 |
| Intraprocedural | 83/6495 (1.28) | 38/1363 (2.79) | 45/5132 (0.88) | <0.0001 |
| Postprocedural | 44/6495 (0.68) | 8/1363 (0.59) | 36/5132 (0.70) | 0.8524 |
ICD, implantable cardioverter-defibrillator; IQR, interquartile range; LV, left ventricle.
Independent predictors of clinical and radiological failure, procedure-related major complications, and of all-cause mortality were checked for patient and leads. The presence of abandoned leads at the time of TLE was an independent predictor of clinical failure (Figure 1 and Table 5) [odds ratio (OR) 2.31, confidence interval (CI) 1.57–3.40] and complications [OR 1.69, CI 1.22–2.35] (Table 5). Receiver-operating characteristic curve analysis showed a dwell time threshold of 9 years for radiological failure and major complications (Figure 2): accordingly leads were defined young or old if their dwell time was respectively shorter or greater than 9 years. A summary table of extracted leads is provided in Table 6.
Multivariate logistic regression after stepwise algorithm selection on clinical failure and complications
| Covariables . | Odds ratio (95% CI) . | P-value . |
|---|---|---|
| Multivariate logistic regression after stepwise algorithm selection on patients dataset with events: clinical failure (n = 147/3585) | ||
| Abandoned leads | 2.31 (1.57–3.40) | <0.0001 |
| Saint Jude RIATA | 1.28 (0.73–2.26) | 0.3867 |
| Powered sheaths | 1.96 (1.39–2.78) | 0.0001 |
| Oldest targeted lead dwelling time >5 years | 2.13 (1.42–3.20) | 0.0003 |
| Multivariate logistic regression after stepwise algorithm selection on leads dataset with events: complications (n = 186/5555) | ||
| Leads (all) in patients with abandoned leads | 1.69 (1.22–2.35) | 0.0018 |
| Saint Jude RIATA | 1.92 (0.99–3.72) | 0.0526 |
| Age (class) <68 years | 0.58 (0.41–0.82) | 0.0019 |
| NYHA Class III–IV | 2.04 (1.44–2.89) | 0.0001 |
| Chronic kidney disease | 1.86 (1.32–2.61) | 0.0004 |
| Dwelling time >5 years | 1.89 (1.33–2.70) | 0.0004 |
| Insertion body side, right | 0.65 (0.45–0.94) | 0.0222 |
| Indication to lead extraction, systemic infection | 1.92 (1.25–2.94) | 0.0048 |
| EDS sheaths use | 6.96 (1.19–40.54) | 0.0310 |
| Covariables . | Odds ratio (95% CI) . | P-value . |
|---|---|---|
| Multivariate logistic regression after stepwise algorithm selection on patients dataset with events: clinical failure (n = 147/3585) | ||
| Abandoned leads | 2.31 (1.57–3.40) | <0.0001 |
| Saint Jude RIATA | 1.28 (0.73–2.26) | 0.3867 |
| Powered sheaths | 1.96 (1.39–2.78) | 0.0001 |
| Oldest targeted lead dwelling time >5 years | 2.13 (1.42–3.20) | 0.0003 |
| Multivariate logistic regression after stepwise algorithm selection on leads dataset with events: complications (n = 186/5555) | ||
| Leads (all) in patients with abandoned leads | 1.69 (1.22–2.35) | 0.0018 |
| Saint Jude RIATA | 1.92 (0.99–3.72) | 0.0526 |
| Age (class) <68 years | 0.58 (0.41–0.82) | 0.0019 |
| NYHA Class III–IV | 2.04 (1.44–2.89) | 0.0001 |
| Chronic kidney disease | 1.86 (1.32–2.61) | 0.0004 |
| Dwelling time >5 years | 1.89 (1.33–2.70) | 0.0004 |
| Insertion body side, right | 0.65 (0.45–0.94) | 0.0222 |
| Indication to lead extraction, systemic infection | 1.92 (1.25–2.94) | 0.0048 |
| EDS sheaths use | 6.96 (1.19–40.54) | 0.0310 |
Selected variables for clinical failure: abandoned leads, Saint Jude RIATA, Powered Sheats and Lead Dwelling Time >5 years.
CI, confidence interval; NYHA, New York Heart Association.
Multivariate logistic regression after stepwise algorithm selection on clinical failure and complications
| Covariables . | Odds ratio (95% CI) . | P-value . |
|---|---|---|
| Multivariate logistic regression after stepwise algorithm selection on patients dataset with events: clinical failure (n = 147/3585) | ||
| Abandoned leads | 2.31 (1.57–3.40) | <0.0001 |
| Saint Jude RIATA | 1.28 (0.73–2.26) | 0.3867 |
| Powered sheaths | 1.96 (1.39–2.78) | 0.0001 |
| Oldest targeted lead dwelling time >5 years | 2.13 (1.42–3.20) | 0.0003 |
| Multivariate logistic regression after stepwise algorithm selection on leads dataset with events: complications (n = 186/5555) | ||
| Leads (all) in patients with abandoned leads | 1.69 (1.22–2.35) | 0.0018 |
| Saint Jude RIATA | 1.92 (0.99–3.72) | 0.0526 |
| Age (class) <68 years | 0.58 (0.41–0.82) | 0.0019 |
| NYHA Class III–IV | 2.04 (1.44–2.89) | 0.0001 |
| Chronic kidney disease | 1.86 (1.32–2.61) | 0.0004 |
| Dwelling time >5 years | 1.89 (1.33–2.70) | 0.0004 |
| Insertion body side, right | 0.65 (0.45–0.94) | 0.0222 |
| Indication to lead extraction, systemic infection | 1.92 (1.25–2.94) | 0.0048 |
| EDS sheaths use | 6.96 (1.19–40.54) | 0.0310 |
| Covariables . | Odds ratio (95% CI) . | P-value . |
|---|---|---|
| Multivariate logistic regression after stepwise algorithm selection on patients dataset with events: clinical failure (n = 147/3585) | ||
| Abandoned leads | 2.31 (1.57–3.40) | <0.0001 |
| Saint Jude RIATA | 1.28 (0.73–2.26) | 0.3867 |
| Powered sheaths | 1.96 (1.39–2.78) | 0.0001 |
| Oldest targeted lead dwelling time >5 years | 2.13 (1.42–3.20) | 0.0003 |
| Multivariate logistic regression after stepwise algorithm selection on leads dataset with events: complications (n = 186/5555) | ||
| Leads (all) in patients with abandoned leads | 1.69 (1.22–2.35) | 0.0018 |
| Saint Jude RIATA | 1.92 (0.99–3.72) | 0.0526 |
| Age (class) <68 years | 0.58 (0.41–0.82) | 0.0019 |
| NYHA Class III–IV | 2.04 (1.44–2.89) | 0.0001 |
| Chronic kidney disease | 1.86 (1.32–2.61) | 0.0004 |
| Dwelling time >5 years | 1.89 (1.33–2.70) | 0.0004 |
| Insertion body side, right | 0.65 (0.45–0.94) | 0.0222 |
| Indication to lead extraction, systemic infection | 1.92 (1.25–2.94) | 0.0048 |
| EDS sheaths use | 6.96 (1.19–40.54) | 0.0310 |
Selected variables for clinical failure: abandoned leads, Saint Jude RIATA, Powered Sheats and Lead Dwelling Time >5 years.
CI, confidence interval; NYHA, New York Heart Association.
| . | Number of leads . | Pacing time (months), mean (SD) . | Radiological outcome . | Clinical success . | Major complications (including deaths) . | Mortality . | Manual traction . | Mechanical sheaths . | Alternative approach . | Extraction time (min), mean (SD) . |
|---|---|---|---|---|---|---|---|---|---|---|
| RA leads | ||||||||||
| Active | 1362 | 70.23 (58.20) | 1332/1362 (97.80%) | 1349/1362 (99.05%) | 42/1362 (3.08%) | 24/1362 (1.76%) | 493/1332 (37.01%) | 334/1362 (24.52%) | 74/1362 (5.43%) | 30.26 (39.05) |
| Passive | 805 | 99.77 (73.14) | 757/805 (94.04%) | 788/805 (97.89%) | 33/805 (4.10%) | 13/805 (1.61%) | 103/797 (12.92%) | 469/805 (58.26%) | 46/805 (5.71%) | 41.69 (41.80) |
| CS leads | ||||||||||
| Active | 45 | 61.42 (30.13) | 43/45 (95.56%) | 44/45 (97.78%) | 2/45 (4.44%) | 2/45 (4.44%) | 9/44 (20.45%) | 22/45 (48.89%) | 0/45 (0.00%) | 41.50 (35.66) |
| Passive | 487 | 49.57 (35.64) | 477/487 (97.95%) | 484/487 (99.38%) | 25/487 (5.13%) | 21/487 (4.31%) | 250/483 (51.76%) | 112/487 (23.00%) | 20/487 (4.11%) | 38.04 (44.53) |
| RV pacing | ||||||||||
| Active | 1932 | 56.97 (47.36) | 1874/1932 (97.00%) | 1911/1932 (98.91%) | 53/1932 (2.74%) | 33/1932 (1.71%) | 611/1897 (32.21%) | 574/1932 (29.71%) | 84/1932 (4.35%) | 28.92 (37.92) |
| Passive | 1580 | 105.21 (75.40) | 1475/1580 (93.35%) | 1533/1580 (97.03%) | 56/1580 (3.54%) | 25/1580 (1.58%) | 178/1551 (11.48%) | 796/1579 (50.41%) | 152/1579 (9.63%) | 38.11 (44.14) |
| ICD leads | ||||||||||
| Active | 1062 | 53.58 (36.05) | 1038/1062 (97.74%) | 1053/1062 (99.15%) | 29/1062 (2.73%) | 18/1062 (1.69%) | 249/1051 (23.69%) | 351/1062 (33.05%) | 40/1062 (3.77%) | 31.24 (39.87) |
| Passive | 498 | 80.49 (45.20) | 482/498 (96.79%) | 488/498 (97.99%) | 17/498 (3.41%) | 10/498 (2.01%) | 39/493 (7.91%) | 272/498 (54.62%) | 45/498 (9.04%) | 39.63 (43.72) |
| Single coil | 580 | 54.44 (43.66) | 564/580 (97.24%) | 573/580 (98.79%) | 15/580 (2.59%) | 10/580 (1.72%) | 175/574 (30.49%) | 180/580 (31.03%) | 30/580 (5.17%) | 32.92 (39.95) |
| Dual coil | 996 | 66.89 (39.04) | 971/996 (97.49%) | 984/996 (98.80%) | 33/996 (3.31%) | 18/996 (1.81%) | 115/986 (11.66%) | 447/996 (44.88%) | 58/996 (5.82%) | 34.58 (42.13) |
| Sprint Fidelis leads | 228 | 83.21 (14.45) | 224/228 (98.25%) | 227/228 (99.56%) | 5/228 (2.19%) | 5/228 (2.19%) | 8/220 (3.64%) | 114/228 (50.00%) | 8/228 (3.51%) | 30.31 (43.77) |
| RIATA leads | 218 | 81.47 (19.41) | 209/218 (95.87%) | 214/218 (98.17%) | 12/218 (5.50%) | 5/218 (2.29%) | 5/218 (2.29%) | 111/218 (50.92%) | 21/218 (9.63%) | 42.21 (51.83) |
| Infected Sprint Fidelis leads | 96 | 81.77 (21.02) | 94/96 (97.92%) | 94/96 (97.92%) | 6/96 (6.25%) | 5/96 (5.21%) | 2/96 (2.08%) | 49/96 (51.04%) | 10/96 (10.42%) | 44.03 (44.71) |
| Infected RIATA leads | 64 | 82.11 (15.38) | 64/64 (100.00%) | 63/64 (98.44%) | 5/64 (7.81%) | 5/64 (7.81%) | 4/62 (6.45%) | 28/64 (43.75%) | 1/64 (1.56%) | 43.55 (49.64) |
| . | Number of leads . | Pacing time (months), mean (SD) . | Radiological outcome . | Clinical success . | Major complications (including deaths) . | Mortality . | Manual traction . | Mechanical sheaths . | Alternative approach . | Extraction time (min), mean (SD) . |
|---|---|---|---|---|---|---|---|---|---|---|
| RA leads | ||||||||||
| Active | 1362 | 70.23 (58.20) | 1332/1362 (97.80%) | 1349/1362 (99.05%) | 42/1362 (3.08%) | 24/1362 (1.76%) | 493/1332 (37.01%) | 334/1362 (24.52%) | 74/1362 (5.43%) | 30.26 (39.05) |
| Passive | 805 | 99.77 (73.14) | 757/805 (94.04%) | 788/805 (97.89%) | 33/805 (4.10%) | 13/805 (1.61%) | 103/797 (12.92%) | 469/805 (58.26%) | 46/805 (5.71%) | 41.69 (41.80) |
| CS leads | ||||||||||
| Active | 45 | 61.42 (30.13) | 43/45 (95.56%) | 44/45 (97.78%) | 2/45 (4.44%) | 2/45 (4.44%) | 9/44 (20.45%) | 22/45 (48.89%) | 0/45 (0.00%) | 41.50 (35.66) |
| Passive | 487 | 49.57 (35.64) | 477/487 (97.95%) | 484/487 (99.38%) | 25/487 (5.13%) | 21/487 (4.31%) | 250/483 (51.76%) | 112/487 (23.00%) | 20/487 (4.11%) | 38.04 (44.53) |
| RV pacing | ||||||||||
| Active | 1932 | 56.97 (47.36) | 1874/1932 (97.00%) | 1911/1932 (98.91%) | 53/1932 (2.74%) | 33/1932 (1.71%) | 611/1897 (32.21%) | 574/1932 (29.71%) | 84/1932 (4.35%) | 28.92 (37.92) |
| Passive | 1580 | 105.21 (75.40) | 1475/1580 (93.35%) | 1533/1580 (97.03%) | 56/1580 (3.54%) | 25/1580 (1.58%) | 178/1551 (11.48%) | 796/1579 (50.41%) | 152/1579 (9.63%) | 38.11 (44.14) |
| ICD leads | ||||||||||
| Active | 1062 | 53.58 (36.05) | 1038/1062 (97.74%) | 1053/1062 (99.15%) | 29/1062 (2.73%) | 18/1062 (1.69%) | 249/1051 (23.69%) | 351/1062 (33.05%) | 40/1062 (3.77%) | 31.24 (39.87) |
| Passive | 498 | 80.49 (45.20) | 482/498 (96.79%) | 488/498 (97.99%) | 17/498 (3.41%) | 10/498 (2.01%) | 39/493 (7.91%) | 272/498 (54.62%) | 45/498 (9.04%) | 39.63 (43.72) |
| Single coil | 580 | 54.44 (43.66) | 564/580 (97.24%) | 573/580 (98.79%) | 15/580 (2.59%) | 10/580 (1.72%) | 175/574 (30.49%) | 180/580 (31.03%) | 30/580 (5.17%) | 32.92 (39.95) |
| Dual coil | 996 | 66.89 (39.04) | 971/996 (97.49%) | 984/996 (98.80%) | 33/996 (3.31%) | 18/996 (1.81%) | 115/986 (11.66%) | 447/996 (44.88%) | 58/996 (5.82%) | 34.58 (42.13) |
| Sprint Fidelis leads | 228 | 83.21 (14.45) | 224/228 (98.25%) | 227/228 (99.56%) | 5/228 (2.19%) | 5/228 (2.19%) | 8/220 (3.64%) | 114/228 (50.00%) | 8/228 (3.51%) | 30.31 (43.77) |
| RIATA leads | 218 | 81.47 (19.41) | 209/218 (95.87%) | 214/218 (98.17%) | 12/218 (5.50%) | 5/218 (2.29%) | 5/218 (2.29%) | 111/218 (50.92%) | 21/218 (9.63%) | 42.21 (51.83) |
| Infected Sprint Fidelis leads | 96 | 81.77 (21.02) | 94/96 (97.92%) | 94/96 (97.92%) | 6/96 (6.25%) | 5/96 (5.21%) | 2/96 (2.08%) | 49/96 (51.04%) | 10/96 (10.42%) | 44.03 (44.71) |
| Infected RIATA leads | 64 | 82.11 (15.38) | 64/64 (100.00%) | 63/64 (98.44%) | 5/64 (7.81%) | 5/64 (7.81%) | 4/62 (6.45%) | 28/64 (43.75%) | 1/64 (1.56%) | 43.55 (49.64) |
CS, coronary sinus; ICD, implantable cardioverter-defibrillator; RA, right atrium; RV, right ventricle; SD, standard deviation.
| . | Number of leads . | Pacing time (months), mean (SD) . | Radiological outcome . | Clinical success . | Major complications (including deaths) . | Mortality . | Manual traction . | Mechanical sheaths . | Alternative approach . | Extraction time (min), mean (SD) . |
|---|---|---|---|---|---|---|---|---|---|---|
| RA leads | ||||||||||
| Active | 1362 | 70.23 (58.20) | 1332/1362 (97.80%) | 1349/1362 (99.05%) | 42/1362 (3.08%) | 24/1362 (1.76%) | 493/1332 (37.01%) | 334/1362 (24.52%) | 74/1362 (5.43%) | 30.26 (39.05) |
| Passive | 805 | 99.77 (73.14) | 757/805 (94.04%) | 788/805 (97.89%) | 33/805 (4.10%) | 13/805 (1.61%) | 103/797 (12.92%) | 469/805 (58.26%) | 46/805 (5.71%) | 41.69 (41.80) |
| CS leads | ||||||||||
| Active | 45 | 61.42 (30.13) | 43/45 (95.56%) | 44/45 (97.78%) | 2/45 (4.44%) | 2/45 (4.44%) | 9/44 (20.45%) | 22/45 (48.89%) | 0/45 (0.00%) | 41.50 (35.66) |
| Passive | 487 | 49.57 (35.64) | 477/487 (97.95%) | 484/487 (99.38%) | 25/487 (5.13%) | 21/487 (4.31%) | 250/483 (51.76%) | 112/487 (23.00%) | 20/487 (4.11%) | 38.04 (44.53) |
| RV pacing | ||||||||||
| Active | 1932 | 56.97 (47.36) | 1874/1932 (97.00%) | 1911/1932 (98.91%) | 53/1932 (2.74%) | 33/1932 (1.71%) | 611/1897 (32.21%) | 574/1932 (29.71%) | 84/1932 (4.35%) | 28.92 (37.92) |
| Passive | 1580 | 105.21 (75.40) | 1475/1580 (93.35%) | 1533/1580 (97.03%) | 56/1580 (3.54%) | 25/1580 (1.58%) | 178/1551 (11.48%) | 796/1579 (50.41%) | 152/1579 (9.63%) | 38.11 (44.14) |
| ICD leads | ||||||||||
| Active | 1062 | 53.58 (36.05) | 1038/1062 (97.74%) | 1053/1062 (99.15%) | 29/1062 (2.73%) | 18/1062 (1.69%) | 249/1051 (23.69%) | 351/1062 (33.05%) | 40/1062 (3.77%) | 31.24 (39.87) |
| Passive | 498 | 80.49 (45.20) | 482/498 (96.79%) | 488/498 (97.99%) | 17/498 (3.41%) | 10/498 (2.01%) | 39/493 (7.91%) | 272/498 (54.62%) | 45/498 (9.04%) | 39.63 (43.72) |
| Single coil | 580 | 54.44 (43.66) | 564/580 (97.24%) | 573/580 (98.79%) | 15/580 (2.59%) | 10/580 (1.72%) | 175/574 (30.49%) | 180/580 (31.03%) | 30/580 (5.17%) | 32.92 (39.95) |
| Dual coil | 996 | 66.89 (39.04) | 971/996 (97.49%) | 984/996 (98.80%) | 33/996 (3.31%) | 18/996 (1.81%) | 115/986 (11.66%) | 447/996 (44.88%) | 58/996 (5.82%) | 34.58 (42.13) |
| Sprint Fidelis leads | 228 | 83.21 (14.45) | 224/228 (98.25%) | 227/228 (99.56%) | 5/228 (2.19%) | 5/228 (2.19%) | 8/220 (3.64%) | 114/228 (50.00%) | 8/228 (3.51%) | 30.31 (43.77) |
| RIATA leads | 218 | 81.47 (19.41) | 209/218 (95.87%) | 214/218 (98.17%) | 12/218 (5.50%) | 5/218 (2.29%) | 5/218 (2.29%) | 111/218 (50.92%) | 21/218 (9.63%) | 42.21 (51.83) |
| Infected Sprint Fidelis leads | 96 | 81.77 (21.02) | 94/96 (97.92%) | 94/96 (97.92%) | 6/96 (6.25%) | 5/96 (5.21%) | 2/96 (2.08%) | 49/96 (51.04%) | 10/96 (10.42%) | 44.03 (44.71) |
| Infected RIATA leads | 64 | 82.11 (15.38) | 64/64 (100.00%) | 63/64 (98.44%) | 5/64 (7.81%) | 5/64 (7.81%) | 4/62 (6.45%) | 28/64 (43.75%) | 1/64 (1.56%) | 43.55 (49.64) |
| . | Number of leads . | Pacing time (months), mean (SD) . | Radiological outcome . | Clinical success . | Major complications (including deaths) . | Mortality . | Manual traction . | Mechanical sheaths . | Alternative approach . | Extraction time (min), mean (SD) . |
|---|---|---|---|---|---|---|---|---|---|---|
| RA leads | ||||||||||
| Active | 1362 | 70.23 (58.20) | 1332/1362 (97.80%) | 1349/1362 (99.05%) | 42/1362 (3.08%) | 24/1362 (1.76%) | 493/1332 (37.01%) | 334/1362 (24.52%) | 74/1362 (5.43%) | 30.26 (39.05) |
| Passive | 805 | 99.77 (73.14) | 757/805 (94.04%) | 788/805 (97.89%) | 33/805 (4.10%) | 13/805 (1.61%) | 103/797 (12.92%) | 469/805 (58.26%) | 46/805 (5.71%) | 41.69 (41.80) |
| CS leads | ||||||||||
| Active | 45 | 61.42 (30.13) | 43/45 (95.56%) | 44/45 (97.78%) | 2/45 (4.44%) | 2/45 (4.44%) | 9/44 (20.45%) | 22/45 (48.89%) | 0/45 (0.00%) | 41.50 (35.66) |
| Passive | 487 | 49.57 (35.64) | 477/487 (97.95%) | 484/487 (99.38%) | 25/487 (5.13%) | 21/487 (4.31%) | 250/483 (51.76%) | 112/487 (23.00%) | 20/487 (4.11%) | 38.04 (44.53) |
| RV pacing | ||||||||||
| Active | 1932 | 56.97 (47.36) | 1874/1932 (97.00%) | 1911/1932 (98.91%) | 53/1932 (2.74%) | 33/1932 (1.71%) | 611/1897 (32.21%) | 574/1932 (29.71%) | 84/1932 (4.35%) | 28.92 (37.92) |
| Passive | 1580 | 105.21 (75.40) | 1475/1580 (93.35%) | 1533/1580 (97.03%) | 56/1580 (3.54%) | 25/1580 (1.58%) | 178/1551 (11.48%) | 796/1579 (50.41%) | 152/1579 (9.63%) | 38.11 (44.14) |
| ICD leads | ||||||||||
| Active | 1062 | 53.58 (36.05) | 1038/1062 (97.74%) | 1053/1062 (99.15%) | 29/1062 (2.73%) | 18/1062 (1.69%) | 249/1051 (23.69%) | 351/1062 (33.05%) | 40/1062 (3.77%) | 31.24 (39.87) |
| Passive | 498 | 80.49 (45.20) | 482/498 (96.79%) | 488/498 (97.99%) | 17/498 (3.41%) | 10/498 (2.01%) | 39/493 (7.91%) | 272/498 (54.62%) | 45/498 (9.04%) | 39.63 (43.72) |
| Single coil | 580 | 54.44 (43.66) | 564/580 (97.24%) | 573/580 (98.79%) | 15/580 (2.59%) | 10/580 (1.72%) | 175/574 (30.49%) | 180/580 (31.03%) | 30/580 (5.17%) | 32.92 (39.95) |
| Dual coil | 996 | 66.89 (39.04) | 971/996 (97.49%) | 984/996 (98.80%) | 33/996 (3.31%) | 18/996 (1.81%) | 115/986 (11.66%) | 447/996 (44.88%) | 58/996 (5.82%) | 34.58 (42.13) |
| Sprint Fidelis leads | 228 | 83.21 (14.45) | 224/228 (98.25%) | 227/228 (99.56%) | 5/228 (2.19%) | 5/228 (2.19%) | 8/220 (3.64%) | 114/228 (50.00%) | 8/228 (3.51%) | 30.31 (43.77) |
| RIATA leads | 218 | 81.47 (19.41) | 209/218 (95.87%) | 214/218 (98.17%) | 12/218 (5.50%) | 5/218 (2.29%) | 5/218 (2.29%) | 111/218 (50.92%) | 21/218 (9.63%) | 42.21 (51.83) |
| Infected Sprint Fidelis leads | 96 | 81.77 (21.02) | 94/96 (97.92%) | 94/96 (97.92%) | 6/96 (6.25%) | 5/96 (5.21%) | 2/96 (2.08%) | 49/96 (51.04%) | 10/96 (10.42%) | 44.03 (44.71) |
| Infected RIATA leads | 64 | 82.11 (15.38) | 64/64 (100.00%) | 63/64 (98.44%) | 5/64 (7.81%) | 5/64 (7.81%) | 4/62 (6.45%) | 28/64 (43.75%) | 1/64 (1.56%) | 43.55 (49.64) |
CS, coronary sinus; ICD, implantable cardioverter-defibrillator; RA, right atrium; RV, right ventricle; SD, standard deviation.
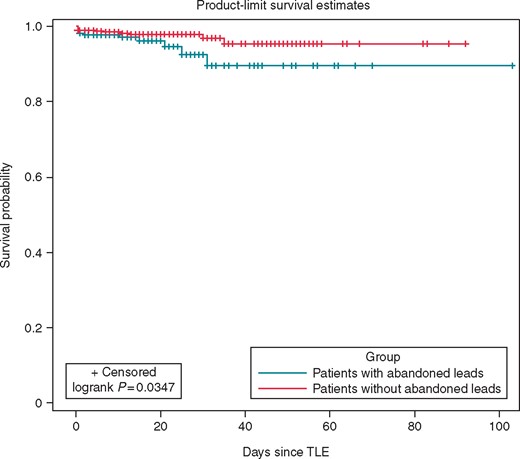
Kaplan–Meier freedom of clinical failure and procedure related complications including deaths in patients with vs. without abandoned leads.

Receiver-operating characteristic curve analysis on events. (A) Procedure related major complications (N = 58) according to mean dwelling time per patients. (B) Radiological failure (N = 97) according to lead dwelling time. Best cut-off determined by the Youden index.
Discussion
The ELECTRa registry5 was the first, large, prospective controlled registry on consecutive TLE procedures in Europe. It has been conducted by an independent scientific society (EHRA/ESC) and represents the largest study of the current practice of TLE to date. In the ELECTRa population, approximately 12.0% had abandoned leads at the time of extraction.
The management of patients with non-infected leads is controversial and much debated. The debate considers the options to either cap and abandon the lead, or to extract it.6–8 Guidelines2,3 give no Class 1 recommendation for the extraction and management of these superfluous leads. Therefore, clinicians frequently have to make their own decisions regarding superfluous lead management. Abandoning leads is a common practice4 that also avoids the procedural risk of TLE. However, multiple studies showed that abandoned leads can pose long-term risks.9
The practice of abandoning leads has many implications. Studies report a greater lead burden, a greater dwell time for the abandoned lead, and an increased risk of infection.10–13 Scenarios including more than two pacing leads, and procedures including CRT, increased the risk of CIED infection.2 Reports show that 11% of young patients with abandoned leads experience CIED infection, compared with 2% of all PM patients.11 Lead migration, lead abrasion, and lead related endocarditis have also been reported recently, as a consequence of lead abandonment..14,15 According to the authors, lead abrasions, through metal exposure, may also have been the initiator of vegetation development.16 In turn, this might explain the more frequent appearance of infective endocarditis in patients with abandoned leads.
The most compelling long-term argument in favour of extracting superfluous leads is the concern that extraction may become more difficult as time passes. Future TLE, in the presence of infections, for example, is likely to be more difficult. Risk also increased where there are additional leads with longer dwell times.17 With increasing lead dwell times, there were also increases in instances of lead adherence and fibrous tissue.18 This makes future extraction procedures higher risk, resulting in a two-fold increase in the risk of extraction failure, for every 3 years that the implant remains.19 Removal of multiple leads was more difficult and more dangerous.2,3 Following TLE, long-term survival rates decline, in relation to an increase in the number of leads requiring extraction.20
Our findings showed that device infection and vegetations were more common in Group 1. Among non-infective indications of TLE (Table 2), the prevalence of non-functional leads and recalled leads was higher in Group 1. This data indicates that patients with abandoned leads had a stronger indication for extraction. This suggests that abandoned leads did not represent the initial indication for TLE but were mainly ‘bystanders’ in infective indications for extractions. This was confirmed by the higher number of leads extracted per patient in Group 1 and by a comparable number of total leads after reimplantation in both groups (Table 3). Patients with abandoned leads were more likely to have CRT devices, and a higher incidence of cardiac resynchronization therapy-defibrillator. This might be explained by a higher prevalence of abandoned, malfunctioning ICD leads. The higher infection, the lower clinical success. Then higher complication rates may explain the significant increase in hospital stay in patients with abandoned leads.
It is unclear whether the additional complications are directly related to the attempts to remove the abandoned leads. Multivariable analysis performed in patients with abandoned leads showed that the extraction of each lead, irrespective of whether it was abandoned or not, was associated with increased risk of complications by 69% [OR 1.69 (1.22–2.35)] (Table 5). Moreover, since abandoned leads had higher pacing time in comparison to non-abandoned leads, a direct relationship between abandoned leads and complications is also very likely.
Merchant et al.17 reported increased procedural complexities and lower clinical success rates in lead extraction cases, in which patients had abandoned leads, whether infected or non-infected. Hussein et al.13 compared outcomes of TLE performed specifically for infectious indications among those with and without abandoned leads. They associated abandoned leads with a lower rate of procedural success, frequent need for extraction tools and a significantly higher rate of procedural complications. These findings are similar to our own results. Our data provided additional information to those reported by Hussein’s13 cohort by extending the findings to include both infective and non-infective indications. Moreover, we found an increased mortality in patients with abandoned leads undergoing TLE procedures. To our knowledge, this is the first reported observation of its kind.
Our analysis showed that a lead dwell time longer than 9 years was associated with an increased extraction failure and complications. Accordingly, we defined leads as young or old, if their dwell time was shorter or greater than nine years, respectively. The complexities of TLE in patients with previously abandoned leads and the lower success rates corresponded to longer dwell time, the significant burden of intravascular adhesions, and lead-on-lead binding. Therefore, these risks cannot be ignored when a decision is made to abandon leads. Especially in light of the current findings and the fact that many patients may require future extraction for complications related to lead abandonment.13
Nonetheless, a recently published report7 showed that the extraction of non-infected superfluous leads is feasible and successful. Such procedures have lower complication rates compared with the extraction of infected leads, which supports the practice of lead extraction for system revision or upgrade. Compared with the general population of TLE at the same centre, those performed at the time of device upgrade were less complex and more likely to be successful, with lower complication rates. The technical aspects of the extraction procedures reflected lower numbers of extracted leads, fewer previously abandoned leads and shorter dwell times observed with this strategy.
The decision to extract or abandon an unnecessary non-infected lead is multifactorial and should consider many procedural TLE complexities. These TLE factors include patient age, co-morbidities, lead dwell time, and the centre’s extraction volume and experience, since long-term data is not yet available. The best strategy is to make decisions case by case, favouring lead extraction in younger patients. However, according to the European survey administrated by EHRA in 2014,4 a clear age cut-off is still undefined and there is no agreement between participants.4 Our results prompt us to define ’young’ patients as 60 or younger, given the median age of 70 years of patients with abandoned leads, and the lead dwell time threshold of nine years for radiological failure and major complications.
This study shows that previously abandoned leads at the time of TLE were associated with increased procedural complexity, procedural failure, and major complication, and may be associated with higher mortality. Accordingly, consideration should be given to extracting ‘young’ leads (dwell time <9 years), instead of abandoning them, and to avoiding the unnecessary extraction of ‘old’ (dwell time >9 years), abandoned leads.
Limitations
The ELECTRa findings are subject to the limitations inherent to observational studies, including the possibility of unknown confounders and bias in management strategy. To ensure data integrity source data and database quality control was performed by dedicated data monitors to ensure that all consecutive patients were included in participating centres. Operators also had to state an intention to treat with the number of leads targeted for extraction thus defining clinical success in advance of the procedure. The participation in the ELECTRa registry was based on a voluntary basis: and complication rates may therefore be underestimated since there are centres, physicians and surgeons performing lead extraction that did not participate in the Registry. Although there was participation from all of the major centres/countries performing extraction the patients recruited may not represent the practice of lead extraction in all countries. Similarly patients with an indication for TLE who were referred for open surgical extraction were excluded from the study. The purpose of ELECTRa was to offer a multicentre prospective overview of TLE safety and efficacy in Europe. Predictors of outcomes were identified and discussed although the exact cause-effect relationships remain speculative.
Conclusions
Previously abandoned leads at the time of TLE were associated with increased procedural complexity, clinical failure and major complication, which may have important implications for future recommendations regarding the choice and timing for abandoning or extracting leads.
Acknowledgements
Registry Executive Committee of the EURObservational Research Programme (EORP). Data collection was conducted by the EORP department from the ESC by Myriam Glemot as Project Officer, Maryna Andarala as Data Manager. Statistical analyses were performed by Cécile Laroche. Overall activities were coordinated and supervised by Doctor Aldo P. Maggioni (EORP Scientific Coordinator).
All investigators listed in the Supplementary material online, Appendix S1.
Funding
This work was supported by the Boston Scientific, Cook Medical, Medtronic, Spectranetics and Zoll.
Conflict of interest: C.B. declares lecture fees (ABBOTT, Medtronic, Berlin Chemie, Daiichi), Consultant for Edwards Impulse Dynamics, Microport CRM, Philips. No stocks. A.A. declares to be Consultant for Abbott, Biosense Webster, Daiichi-Sankyo, Boston Scientific, Cardiotek-Schwarzer, Cordis Biologics Delivery Systems, Medtronic, Microport CRM, Philips. Declares speaker fee from Daiichi-Sankyo, Boston Scientific, Medtronic, Microport CRM. C.A.R. declares being member of speaker bureau at Jon Phillips Spectanetrics. J.H.S. declares conducting research sponsored by Medtronic, Gilead, Biotronik. He is member of Speaker bureau for Medtronic and member of advisory boards for Medtronic. M.G.B. declares conflict of interest as follows: Medtronic, Boston Scientific, Zoll (in the past 2 years). S.C. is a member of the speaker bureau for Abbott. N.D. declares research grants from Abbott, Biotronik, Boston Scientific & Medtronic to the Institution (Heart Center, Leipzig), outside the submitted work without personal financial benefits. C.K. declares having consulted for, performed studies with and presented on behalf of Biotronik, Boston Scientific, Medtronic, St Jude Abbott and Spectranetics. All other authors declared no conflict of interest.
References
Author notes
A complete list of the ELECTRa Investigators is provided in the Supplementary material online, Appendix S1.



