-
PDF
- Split View
-
Views
-
Cite
Cite
Susanne S. Pedersen, Charlotte Knudsen, Karen Dilling, Niels C.F. Sandgaard, Jens Brock Johansen, Living with an implantable cardioverter defibrillator: patients' preferences and needs for information provision and care options, EP Europace, Volume 19, Issue 6, June 2017, Pages 983–990, https://doi.org/10.1093/europace/euw109
Close - Share Icon Share
Abstract
The clinical management and care of patients with an implantable cardioverter defibrillator (ICD) has shifted from face-to-face in-clinic visits to remote monitoring. Reduced interactions between patients and healthcare professionals may impede patients' transition to adapting post-implant. We examined patients' needs and preferences for information provision and care options and overall satisfaction with treatment.
Patients implanted with a first-time ICD or defibrillator with cardiac resynchronization therapy (n = 389) within the last 2 years at Odense University Hospital were asked to complete a purpose-designed and standardized set of questionnaires. The level of satisfaction with information provision was high; only 13.1% were dissatisfied. Psychological support for patients (39.9%), their relatives (43.1%), and deactivation of the ICD towards end of life (47.8%) were among the top five topics that patients reported to have received no information about. The top five care options that patients had missed were talking to the same healthcare professional (75.2%), receiving ongoing feedback via remote monitoring (61.1%), having a personal conversation with a staff member 2–3 weeks post-implant (59.6%), having an exercise tolerance test (52.5%), and staff asking how patients felt while hospitalized (50.4%). Patients with a secondary prevention indication and cardiac arrest survivors had specific needs, including a wish for a psychological consult post-discharge.
Despite a high satisfaction level with information provision, particular topics are not broached with patients (e.g. device activation) and patients have unmet needs that are not met in current clinical practice.
Despite a high level of satisfaction with treatment, implantable cardioverter defibrillator (ICD) patients have several unmet needs that relate to their in-hospital and outpatient care.
Psychological support for patients (39.9%), their relatives (43.1%), and deactivation of the ICD towards end of life (47.8%) were among the top five topics that patients had not received information about.
The top five care options that patients had missed were talking to the same healthcare professional (75.2%), receiving ongoing feedback via remote monitoring (61.1%), having a personal conversation with hospital staff 2–3 weeks post-implant (59.6%), having an exercise tolerance test (52.5%), and staff asking how patients felt while hospitalized (50.4%).
Patients with a secondary prevention indication and cardiac arrest survivors are the most vulnerable groups warranting the implementation of stratified care.
It may be time to revisit the after-care that we give to ICD patients, as some aspects might be easily changed and at a low cost.
Introduction
The implantable cardioverter defibrillator (ICD) is the first-line of treatment for the primary and secondary prevention of sudden cardiac death due to significant absolute risk reductions in mortality of up to 24.6% when compared with anti-arrhythmic therapy.1 These survival benefits have led to a significant increase in implants, with 252 implants in Europe and 675 implants in the USA per million of the population per year.2
During the last decade, there has been a shift in the management and care of ICD patients, with the majority of patients being on remote monitoring as a replacement for face-to-face in-clinic visits.3 Despite its clear advantages in terms of efficiency, timely intervention due to early detection of clinical or technical problems, and overall saved costs,4 the impact on patients' quality of life is mixed.4 Whether these mixed results can be attributed to the shift in care from face-to-face in-clinic visits to remote monitoring is not known. However, we do know that satisfaction with information provision is an important correlate of quality of life, with dissatisfied patients reporting more impaired functioning.5 We also know that anxiety and depression are important predictors of impaired physical, social, and psychological functioning and overall quality of life.6
Thus, the widespread implementation of remote monitoring may create missed opportunities for ICD patients and their relatives to ask healthcare professionals questions and to voice their concerns about their device and treatment. Remote monitoring may also limit opportunities for healthcare professionals to spot vulnerable patients and to provide the information, care, and support that help facilitate patients' transition and adaptation to living successfully with their device.7
In order to optimize the clinical management and care of ICD patients, it is important to recognize patients' needs, and how we can become better at targeting not only treatment but also information provision to patients' needs and preferences.8 Hence, using a user-centred mixed-methods design, we asked patients with an ICD implanted at one of the five university hospitals in Denmark to indicate which information they had received, which information they had missed, their preferred timing and mode for receiving information (e.g. brochure, website, app, etc.), their preference for additional care options, and their overall satisfaction with treatment.
Methods
Patient sample
Patients were eligible to participate in the current study, if they were implanted with a first-time ICD or ICD with cardiac resynchronization therapy (CRT-D) in the period between 1 August 2012 and 31 July 2014 at Odense University Hospital, Denmark, ≥18 years of age, alive, and sufficiently proficient in the Danish language to complete a questionnaire. Patients were excluded if they had a history of severe psychiatric illness (e.g. schizophrenia), had received a previous implant, or had insufficient knowledge of the Danish language.
Study design
We used a user-centred mixed-methods design, with the quantitative purpose-designed questionnaire used in the study being developed as follows.
Phase I
In the period between April and June 2014, we conducted three semi-structured, open-ended focus group interviews with ICD patients (6–8 patients in each group) with the use of a standardized interview guide. We chose an open-ended approach in order to encourage patients to share and discuss their experiences and needs for information and care post-implant. A multi-disciplinary team that included a research psychologist specialized in ICD patients (S.S.P.), an ICD nurse (K.D.), and a research assistant (C.K.) ran the focus groups. A senior consultant in cardiology (J.B.J.) was present during the first 5 min of the interviews to emphasize the value of their participation for the hospital with respect to optimizing the care and management of ICD patients. The interview guide tapped into topics on information and care with respect to timing (e.g. one time vs. repeated), mode (e.g. leaflets, self-help material, face-to-face, internet-based), contents (e.g. cardiac rehabilitation, meetings with a nurse, physician or psychologist, exercise tolerance test).
Phase II
Information from the focus group interviews and the scientific literature was used to generate a first draft of the purpose-designed quantitative questionnaire. This draft version was shown to nurses in cardiology who see ICD patients as part of general practice. Following their input, the questionnaire was revised and administered to four ICD patients, allowing for a dialogue about the questionnaire, whether it was understandable to patients, and whether particular topics had been overlooked. Following patients' input and final adjustments, the questionnaire was ready for use in the current study and consisted of three parts: Part I: general questions about education, cardiac rehabilitation attendance, etc. and standardized and validated questionnaires, as described under psychological measures below; Part II: (i) ICD-related topics where patients received no information and (ii) ICD-related information received and satisfaction with this information; Part III: (i) patients' needs and preferences for care options that were not part of standard clinical practice and (ii) overall patient satisfaction with ICD-related information provision, treatment, and care.
Study procedure and ethics
All patients received written information about the study, with telephone numbers listed for the senior consultant in cardiology and the ICD nurse at the ICD outpatient clinic for patients to call in case they had any questions about the study. The first questionnaire together with a letter explaining the purpose of the study and a prepaid, self-addressed envelope was sent to eligible patients in the beginning of January 2015. If we did not receive the questionnaire within 4 weeks, a reminder was sent out with a new copy of the questionnaire and a prepaid, self-addressed envelope.
The study protocol was submitted to the Regional Scientific Ethical Committees for Southern Denmark, who indicated that no written consent was required by Danish law. Given that we also needed to access information from the Danish Pacemaker and ICD Register, the protocol was submitted and approved by the Danish Data Protection Agency.
Measures
Demographic and clinical variables
Information on baseline characteristics were captured from the Danish Pacemaker and ICD Register or from purpose-designed questions included in the questionnaire that patients were asked to complete. These included information on sex, age, marital status, education, working status, smoking status, participation in cardiac rehabilitation, treatment by a mental health professional, diagnosis with psychiatric disorder, and attending other outpatient clinics than the ICD clinic. Information on clinical variables includes indication for ICD implantation (primary vs. secondary), type of ICD (ICD vs. CRT-D), pacing mode, prior cardiac arrest, cardiac diagnosis at implant [i.e. ischaemic heart disease, dilated cardiomyopathy or other (e.g. Brugada, arrhythmogenic right ventricular cardiomyopathy, etc.)], defibrillation threshold testing at implant, left ventricular ejection fraction, New York Heart Association (NYHA) functional class, QRS, body mass index (BMI), previous percutaneous coronary intervention, previous coronary artery bypass graft surgery.
Psychological measures
In addition to the purpose-designed questionnaire tapping into patients' needs and preferences for information, care options, and satisfaction with treatment, patients were asked to complete the following standardized and validated questionnaires.
The eight-item ICD Patient Concerns questionnaire (ICDC) assesses device-related concerns with respect to receiving an ICD shock (e.g. ‘I am worried about my ICD firing’).9 Items are rated on a five-point Likert scale from 0 (not at all) to 4 (very much so), with total score range from 0 to 32 and a higher score indicating more device-related concerns.9 The internal consistency of the eight-item ICDC is good, as demonstrated by a Cronbach's α = 0.91. We used a cut-off of ≥13 to indicate a high level of ICD concerns.10
The Type D Scale (DS14) assesses the ‘distressed’ (Type D) personality by means of 14 items that are answered on a five-point Likert scale from 0 (false) to 4 (true), with 7 items contributing to the two components of Type D negative affectivity (e.g. ‘I often feel unhappy’) and social inhibition (e.g. ‘I find it hard to start a conversation’).11 Type D caseness is determined by means of a high score on both components, using the standardized cut-off of ≥10, which item response theory has identified as the most optimal.12 The psychometric properties of the scale are good.11 Type D personality has in previous studies on ICD patients been shown to increase the risk of poor health outcomes including mortality.10
The Patient Health Questionnaire 9 (PHQ-9) is a measure of depressive symptoms that consists of nine items that mirror the diagnostic criteria of a clinical depression.13 Items are rated on a four-point Likert scale from 0 to 3 (score range 0–27), with a higher score indicating more severe depression.13 As part of a two-stepped procedure, the American Heart Association has recommended to use the PHQ-9 in clinical practice.
Statistical analysis
Frequency distributions and mean scores were computed to quantify information received, patients' needs and preferences for information provision and additional care options, and treatment satisfaction. Student's t-test for independent samples was used to compare groups on continuous variables, while the χ2 test (Fisher's exact test if appropriate) was used to compare groups on nominal variables. PASW Statistics 23 statistical software was used to analyse the data (PASW IBM Corp., Armonk, NY, USA).
Results
Of 480 patients who fulfilled the eligibility criteria, 389 (81% response rate) agreed to participate. Responders and non-responders did not differ systematically on any of the baseline characteristics, as presented in Table 1, except that responders were older (65 ± 11 vs. 61 ± 14 years, P= 0.009), less likely to have a primary prevention indication (35.5 vs. 47.3%, P= 0.037) and to smoke (27.5 vs. 29.2%, P= 0.014). The mean BMI for responders was lower than that for non-responders (27.0 ± 4.7 vs. 28.4 ± 5.0, P= 0.014).
| Characteristics . | Valid cases . | % (n)a . |
|---|---|---|
| Demographics | ||
| Men | 389 | 81.5% (317) |
| Age, mean ± SD | 389 | 65 ± 11 |
| Single/no partner | 384 | 22.1% (85) |
| Lower educational levelb | 380 | 75.0% (285) |
| Working | 382 | 23.0% (88) |
| Clinical | ||
| Primary prevention indication | 376 | 36.7% (138) |
| Type of ICD | 389 | |
| ICD | 72.5% (282) | |
| CRT-D | 27.5% (107) | |
| Pacing mode | 389 | |
| Single chamber | 64.5% (251) | |
| Dual chamber or biventricular | 35.5% (138) | |
| Prior cardiac arrest | 377 | 31.6% (119) |
| Cardiac diagnosis at implant | 376 | |
| Ischaemic heart disease | 70.2% (264) | |
| Dilated cardiomyopathy | 10.9% (41) | |
| Other (e.g. Brugada, ARVC, long QT) | 18.9% (71) | |
| Defibrillation threshold testing at implant | 311 | 69.2% (269) |
| LVEF | 377 | 37.4 ± 14.2 |
| Symptomatic heart failure (NYHA III–IV) | 373 | 11.5% (43) |
| QRS (ms) | 377 | 114.6 ± 28.3 |
| BMI, mean ± SD | 389 | 27.0 ± 4.74 |
| Previous PCI | 377 | 44.0% (166) |
| Previous CABG | 376 | 24.5% (92) |
| Smoking | 385 | 17.7% (68) |
| Treatment by a mental health professional | ||
| Before the ICD implant | 385 | 9.4% (36) |
| After the ICD implant | 385 | 7.5% (29) |
| Diagnosed with a psychiatric disorder | 385 | 8.3% (32) |
| Participated in cardiac rehabilitation | 378 | 49.2% (186) |
| Attending other outpatient clinics | 377 | 46.2% (174) |
| Psychological | ||
| Type D personality | 378 | 18% (68) |
| Depressive symptoms | 370 | |
| None to mild (score ≤14) | 81.9% (303) | |
| Moderate to severe (score >15) | 18.1% (67) | |
| High levels of ICD concerns (score >13) | 382 | 16.8% (64) |
| Characteristics . | Valid cases . | % (n)a . |
|---|---|---|
| Demographics | ||
| Men | 389 | 81.5% (317) |
| Age, mean ± SD | 389 | 65 ± 11 |
| Single/no partner | 384 | 22.1% (85) |
| Lower educational levelb | 380 | 75.0% (285) |
| Working | 382 | 23.0% (88) |
| Clinical | ||
| Primary prevention indication | 376 | 36.7% (138) |
| Type of ICD | 389 | |
| ICD | 72.5% (282) | |
| CRT-D | 27.5% (107) | |
| Pacing mode | 389 | |
| Single chamber | 64.5% (251) | |
| Dual chamber or biventricular | 35.5% (138) | |
| Prior cardiac arrest | 377 | 31.6% (119) |
| Cardiac diagnosis at implant | 376 | |
| Ischaemic heart disease | 70.2% (264) | |
| Dilated cardiomyopathy | 10.9% (41) | |
| Other (e.g. Brugada, ARVC, long QT) | 18.9% (71) | |
| Defibrillation threshold testing at implant | 311 | 69.2% (269) |
| LVEF | 377 | 37.4 ± 14.2 |
| Symptomatic heart failure (NYHA III–IV) | 373 | 11.5% (43) |
| QRS (ms) | 377 | 114.6 ± 28.3 |
| BMI, mean ± SD | 389 | 27.0 ± 4.74 |
| Previous PCI | 377 | 44.0% (166) |
| Previous CABG | 376 | 24.5% (92) |
| Smoking | 385 | 17.7% (68) |
| Treatment by a mental health professional | ||
| Before the ICD implant | 385 | 9.4% (36) |
| After the ICD implant | 385 | 7.5% (29) |
| Diagnosed with a psychiatric disorder | 385 | 8.3% (32) |
| Participated in cardiac rehabilitation | 378 | 49.2% (186) |
| Attending other outpatient clinics | 377 | 46.2% (174) |
| Psychological | ||
| Type D personality | 378 | 18% (68) |
| Depressive symptoms | 370 | |
| None to mild (score ≤14) | 81.9% (303) | |
| Moderate to severe (score >15) | 18.1% (67) | |
| High levels of ICD concerns (score >13) | 382 | 16.8% (64) |
ARVC, arrhythmogenic right ventricular cardiomyopathy; CABG, coronary artery bypass graft surgery; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association functional class; PCI, percutaneous coronary intervention.
aResults are presented as % (n) unless otherwise indicated.
b≤13 years.
| Characteristics . | Valid cases . | % (n)a . |
|---|---|---|
| Demographics | ||
| Men | 389 | 81.5% (317) |
| Age, mean ± SD | 389 | 65 ± 11 |
| Single/no partner | 384 | 22.1% (85) |
| Lower educational levelb | 380 | 75.0% (285) |
| Working | 382 | 23.0% (88) |
| Clinical | ||
| Primary prevention indication | 376 | 36.7% (138) |
| Type of ICD | 389 | |
| ICD | 72.5% (282) | |
| CRT-D | 27.5% (107) | |
| Pacing mode | 389 | |
| Single chamber | 64.5% (251) | |
| Dual chamber or biventricular | 35.5% (138) | |
| Prior cardiac arrest | 377 | 31.6% (119) |
| Cardiac diagnosis at implant | 376 | |
| Ischaemic heart disease | 70.2% (264) | |
| Dilated cardiomyopathy | 10.9% (41) | |
| Other (e.g. Brugada, ARVC, long QT) | 18.9% (71) | |
| Defibrillation threshold testing at implant | 311 | 69.2% (269) |
| LVEF | 377 | 37.4 ± 14.2 |
| Symptomatic heart failure (NYHA III–IV) | 373 | 11.5% (43) |
| QRS (ms) | 377 | 114.6 ± 28.3 |
| BMI, mean ± SD | 389 | 27.0 ± 4.74 |
| Previous PCI | 377 | 44.0% (166) |
| Previous CABG | 376 | 24.5% (92) |
| Smoking | 385 | 17.7% (68) |
| Treatment by a mental health professional | ||
| Before the ICD implant | 385 | 9.4% (36) |
| After the ICD implant | 385 | 7.5% (29) |
| Diagnosed with a psychiatric disorder | 385 | 8.3% (32) |
| Participated in cardiac rehabilitation | 378 | 49.2% (186) |
| Attending other outpatient clinics | 377 | 46.2% (174) |
| Psychological | ||
| Type D personality | 378 | 18% (68) |
| Depressive symptoms | 370 | |
| None to mild (score ≤14) | 81.9% (303) | |
| Moderate to severe (score >15) | 18.1% (67) | |
| High levels of ICD concerns (score >13) | 382 | 16.8% (64) |
| Characteristics . | Valid cases . | % (n)a . |
|---|---|---|
| Demographics | ||
| Men | 389 | 81.5% (317) |
| Age, mean ± SD | 389 | 65 ± 11 |
| Single/no partner | 384 | 22.1% (85) |
| Lower educational levelb | 380 | 75.0% (285) |
| Working | 382 | 23.0% (88) |
| Clinical | ||
| Primary prevention indication | 376 | 36.7% (138) |
| Type of ICD | 389 | |
| ICD | 72.5% (282) | |
| CRT-D | 27.5% (107) | |
| Pacing mode | 389 | |
| Single chamber | 64.5% (251) | |
| Dual chamber or biventricular | 35.5% (138) | |
| Prior cardiac arrest | 377 | 31.6% (119) |
| Cardiac diagnosis at implant | 376 | |
| Ischaemic heart disease | 70.2% (264) | |
| Dilated cardiomyopathy | 10.9% (41) | |
| Other (e.g. Brugada, ARVC, long QT) | 18.9% (71) | |
| Defibrillation threshold testing at implant | 311 | 69.2% (269) |
| LVEF | 377 | 37.4 ± 14.2 |
| Symptomatic heart failure (NYHA III–IV) | 373 | 11.5% (43) |
| QRS (ms) | 377 | 114.6 ± 28.3 |
| BMI, mean ± SD | 389 | 27.0 ± 4.74 |
| Previous PCI | 377 | 44.0% (166) |
| Previous CABG | 376 | 24.5% (92) |
| Smoking | 385 | 17.7% (68) |
| Treatment by a mental health professional | ||
| Before the ICD implant | 385 | 9.4% (36) |
| After the ICD implant | 385 | 7.5% (29) |
| Diagnosed with a psychiatric disorder | 385 | 8.3% (32) |
| Participated in cardiac rehabilitation | 378 | 49.2% (186) |
| Attending other outpatient clinics | 377 | 46.2% (174) |
| Psychological | ||
| Type D personality | 378 | 18% (68) |
| Depressive symptoms | 370 | |
| None to mild (score ≤14) | 81.9% (303) | |
| Moderate to severe (score >15) | 18.1% (67) | |
| High levels of ICD concerns (score >13) | 382 | 16.8% (64) |
ARVC, arrhythmogenic right ventricular cardiomyopathy; CABG, coronary artery bypass graft surgery; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association functional class; PCI, percutaneous coronary intervention.
aResults are presented as % (n) unless otherwise indicated.
b≤13 years.
Baseline characteristics
Baseline characteristics of the patient sample included in the analyses are presented in Table 1. The majority of the patients were men (81.5%) and had a lower educational level (75.0%). Of all patients, 18.1% suffered from moderate to severe depression (PHQ-9 score >15), while 16.8% reported high levels of ICD concerns (i.e. fears about whether the ICD would shock).
Information provision
Figure 1 presents the proportion of patients who received no information on specific ICD-related topics. The top five topics that patients did not receive information on were ‘whom to contact with social and work-related questions’ (48.9%), ‘the ICD can be deactivated towards end of life’ (47.8%), ‘the impact on obtaining insurance’ (43.5%), ‘psychological support for my relatives’ (43.1%), ‘psychological support for myself’ (39.9%).
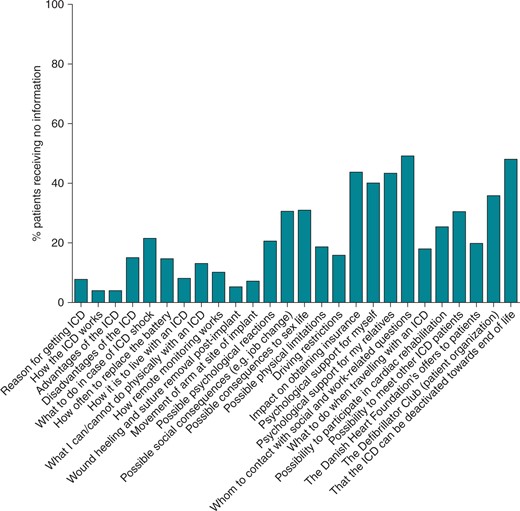
Proportion of patients who received no information on specific ICD-related topics (n = 352–372).
Figure 2 presents patients' endorsements with respect to satisfaction with information, if they had received the information. The largest number of patients who were either very dissatisfied or somewhat dissatisfied was 13.1%, indicating an overall large satisfaction with information provision in our cohort.
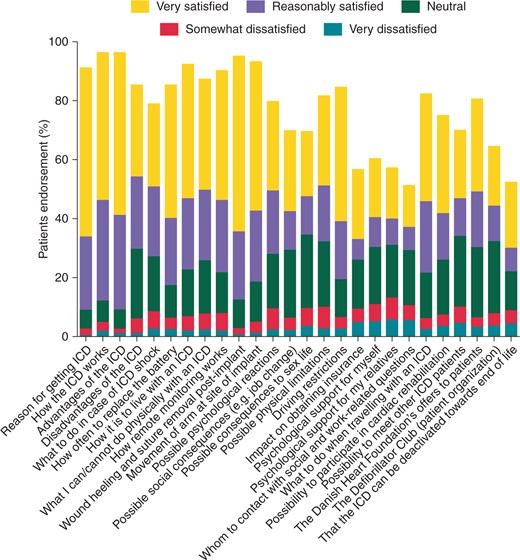
Patient satisfaction with information if they had received the information (n = 352–372).
Patients' needs and preferences for care options not part of standard clinical practice
Figure 3 presents patients' needs and preferences for care options that were not part of standard clinical practice. The top five preferences were ‘same doctor/nurse who talk to me every time’ (75.2%), ‘ongoing feedback via remote monitoring system’ (61.1%), ‘personal conversation with nurse/doctor 2–3 weeks post-implant’ (59.6%), ‘exercise tolerance test’ (52.5%), and ‘doctors and nurses ask how I feel while hospitalized’ (50.4%).
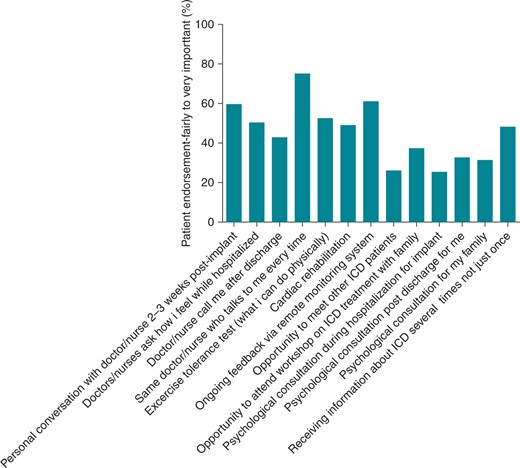
Patients' preferences for care options that were not part of standard clinical practice (n = 351–375).
Table 2 presents patients' needs and preferences for care options that were not part of standard clinical practice, stratified by a priori defined subgroups (i.e. gender, ICD indication, and sudden cardiac arrest) that based on the literature and the focus groups interviews suggest might differ in their needs. These results indicated that women would have preferred to have the opportunity to consult with a mental health professional post-discharge when compared with men (43.1 vs. 30.3%, P= 0.048). Patients with a secondary indication were more likely to have missed that hospital staff asked them how they felt while hospitalized for their ICD implant (54.8 vs. 40.2%, P= 0.007), that they had the opportunity to undergo an exercise tolerance test (59.1 vs. 43.2%, P= 0.003), to attend an ICD workshop with their families (41.3 vs. 30.0%, P= 0.033), to have a psychological consult while hospitalized (28.6 vs. 19.0%, P= 0.050) and post-discharge for themselves (38.5 vs. 21.3%, P= 0.001) and a psychological consult post-discharge for their family (37.3 vs. 21.3%, P= 0.002), and receiving ICD-related information several times rather than once (55.7 vs. 33.6%, P< 0.0001). Patients who had experienced a sudden cardiac arrest also indicated that they would have liked to have the opportunity to have a psychological consult post-discharge for themselves (42.3 vs. 27.5%, P= 0.006) and for their families (45.5 vs. 24.8% P< 0.0001), and to receive ICD-related information several times rather than once (59.5 vs. 42.1%, P= 0.003).
Patients' preferences for care options that were not part of standard clinical practice, stratified by a priori defined subgroups*
| Care options . | Women . | Men . | P . | Primary prevention . | Secondary prevention . | P . | SCA . | No SCA . | P . |
|---|---|---|---|---|---|---|---|---|---|
| Personal conversation with doctor/nurse 2–3 weeks post-implant | 63.2% (42) | 58.8% (180) | 0.502 | 50.0% (70) | 62.4% (1439 | 0.080 | 60.3% (70) | 58.5% (144) | 0.744 |
| Doctors/nurses ask how I feel while hospitalized | 60.9% (42) | 48.0% (146) | 0.054 | 40.2% (53) | 54.8% (125) | 0.007 | 52.2% (60) | 48.4% (119) | 0.501 |
| Doctor/nurse calls me post-discharge | 52.2% (36) | 40.5% (124) | 0.077 | 39.1% (52) | 44.1% (101) | 0.353 | 43.1% (50) | 42.1% (104) | 0.858 |
| Same doctor/nurse who talks to me every time | 82.9% (58) | 73.4% (224) | 0.226 | 74.8% (98) | 74.9% (173) | 0.986 | 70.9% (83) | 76.8% (189) | 0.226 |
| Exercise tolerance test | 53.6% (37) | 52.3% (160) | 0.841 | 43.2% (57) | 59.1% (136) | 0.003 | 59.0% (69) | 50.8% (125) | 0. 145 |
| Cardiac rehabilitation | 44.8% (30) | 50.2% (152) | 0.425 | 48.5% (63) | 48.9% (111) | 0.937 | 51.7% (60) | 47.5% (115) | 0.456 |
| Ongoing feedback via remote monitoring system | 64.2% (43) | 60.4% (183) | 0.565 | 58.0% (76) | 63.3% (143) | 0.325 | 60.3% (70) | 62.0% (150) | 0. 766 |
| Opportunity to meet other ICD patients | 33.3% (23) | 24.4% (75) | 0.128 | 25.0% (33) | 26.4% (61) | 0.768 | 24.8% (29) | 26.7% (66) | 0.695 |
| Opportunity to attend ICD workshop with family | 44.9% (31) | 35.5% (108) | 0.145 | 30.0% (39) | 41.3% (95) | 0.033 | 41.9% (49) | 34.8% (85) | 0.195 |
| Psychological consult while hospitalized | 31.7% (20) | 24.0% (69) | 0.198 | 19.0% (23) | 28.6% (63) | 0.050 | 31.3% (35) | 22.2% (51) | 0.069 |
| Psychological consult post-discharge for me | 43.1% (28) | 30.3% (88) | 0.048 | 21.3% (26) | 38.5% (85) | 0.001 | 42.3% (47) | 27.5% (64) | 0.006 |
| Psychological consult post-discharge for my family | 33.3% (21) | 30.9% (89) | 0.706 | 21.3% (26) | 37.3% (81) | 0.002 | 45.5% (50) | 24.8% (57) | <0.0001 |
| Receiving ICD-related information several times rather than once | 56.3% (36) | 46.4% (135) | 0.153 | 33.6% (41) | 55.7% (123) | <0.0001 | 59.5% (66) | 42.1% (98) | 0.003 |
| Care options . | Women . | Men . | P . | Primary prevention . | Secondary prevention . | P . | SCA . | No SCA . | P . |
|---|---|---|---|---|---|---|---|---|---|
| Personal conversation with doctor/nurse 2–3 weeks post-implant | 63.2% (42) | 58.8% (180) | 0.502 | 50.0% (70) | 62.4% (1439 | 0.080 | 60.3% (70) | 58.5% (144) | 0.744 |
| Doctors/nurses ask how I feel while hospitalized | 60.9% (42) | 48.0% (146) | 0.054 | 40.2% (53) | 54.8% (125) | 0.007 | 52.2% (60) | 48.4% (119) | 0.501 |
| Doctor/nurse calls me post-discharge | 52.2% (36) | 40.5% (124) | 0.077 | 39.1% (52) | 44.1% (101) | 0.353 | 43.1% (50) | 42.1% (104) | 0.858 |
| Same doctor/nurse who talks to me every time | 82.9% (58) | 73.4% (224) | 0.226 | 74.8% (98) | 74.9% (173) | 0.986 | 70.9% (83) | 76.8% (189) | 0.226 |
| Exercise tolerance test | 53.6% (37) | 52.3% (160) | 0.841 | 43.2% (57) | 59.1% (136) | 0.003 | 59.0% (69) | 50.8% (125) | 0. 145 |
| Cardiac rehabilitation | 44.8% (30) | 50.2% (152) | 0.425 | 48.5% (63) | 48.9% (111) | 0.937 | 51.7% (60) | 47.5% (115) | 0.456 |
| Ongoing feedback via remote monitoring system | 64.2% (43) | 60.4% (183) | 0.565 | 58.0% (76) | 63.3% (143) | 0.325 | 60.3% (70) | 62.0% (150) | 0. 766 |
| Opportunity to meet other ICD patients | 33.3% (23) | 24.4% (75) | 0.128 | 25.0% (33) | 26.4% (61) | 0.768 | 24.8% (29) | 26.7% (66) | 0.695 |
| Opportunity to attend ICD workshop with family | 44.9% (31) | 35.5% (108) | 0.145 | 30.0% (39) | 41.3% (95) | 0.033 | 41.9% (49) | 34.8% (85) | 0.195 |
| Psychological consult while hospitalized | 31.7% (20) | 24.0% (69) | 0.198 | 19.0% (23) | 28.6% (63) | 0.050 | 31.3% (35) | 22.2% (51) | 0.069 |
| Psychological consult post-discharge for me | 43.1% (28) | 30.3% (88) | 0.048 | 21.3% (26) | 38.5% (85) | 0.001 | 42.3% (47) | 27.5% (64) | 0.006 |
| Psychological consult post-discharge for my family | 33.3% (21) | 30.9% (89) | 0.706 | 21.3% (26) | 37.3% (81) | 0.002 | 45.5% (50) | 24.8% (57) | <0.0001 |
| Receiving ICD-related information several times rather than once | 56.3% (36) | 46.4% (135) | 0.153 | 33.6% (41) | 55.7% (123) | <0.0001 | 59.5% (66) | 42.1% (98) | 0.003 |
* Numbers highlighted in bold-face indicate statistically significant differences between groups.
Patients' preferences for care options that were not part of standard clinical practice, stratified by a priori defined subgroups*
| Care options . | Women . | Men . | P . | Primary prevention . | Secondary prevention . | P . | SCA . | No SCA . | P . |
|---|---|---|---|---|---|---|---|---|---|
| Personal conversation with doctor/nurse 2–3 weeks post-implant | 63.2% (42) | 58.8% (180) | 0.502 | 50.0% (70) | 62.4% (1439 | 0.080 | 60.3% (70) | 58.5% (144) | 0.744 |
| Doctors/nurses ask how I feel while hospitalized | 60.9% (42) | 48.0% (146) | 0.054 | 40.2% (53) | 54.8% (125) | 0.007 | 52.2% (60) | 48.4% (119) | 0.501 |
| Doctor/nurse calls me post-discharge | 52.2% (36) | 40.5% (124) | 0.077 | 39.1% (52) | 44.1% (101) | 0.353 | 43.1% (50) | 42.1% (104) | 0.858 |
| Same doctor/nurse who talks to me every time | 82.9% (58) | 73.4% (224) | 0.226 | 74.8% (98) | 74.9% (173) | 0.986 | 70.9% (83) | 76.8% (189) | 0.226 |
| Exercise tolerance test | 53.6% (37) | 52.3% (160) | 0.841 | 43.2% (57) | 59.1% (136) | 0.003 | 59.0% (69) | 50.8% (125) | 0. 145 |
| Cardiac rehabilitation | 44.8% (30) | 50.2% (152) | 0.425 | 48.5% (63) | 48.9% (111) | 0.937 | 51.7% (60) | 47.5% (115) | 0.456 |
| Ongoing feedback via remote monitoring system | 64.2% (43) | 60.4% (183) | 0.565 | 58.0% (76) | 63.3% (143) | 0.325 | 60.3% (70) | 62.0% (150) | 0. 766 |
| Opportunity to meet other ICD patients | 33.3% (23) | 24.4% (75) | 0.128 | 25.0% (33) | 26.4% (61) | 0.768 | 24.8% (29) | 26.7% (66) | 0.695 |
| Opportunity to attend ICD workshop with family | 44.9% (31) | 35.5% (108) | 0.145 | 30.0% (39) | 41.3% (95) | 0.033 | 41.9% (49) | 34.8% (85) | 0.195 |
| Psychological consult while hospitalized | 31.7% (20) | 24.0% (69) | 0.198 | 19.0% (23) | 28.6% (63) | 0.050 | 31.3% (35) | 22.2% (51) | 0.069 |
| Psychological consult post-discharge for me | 43.1% (28) | 30.3% (88) | 0.048 | 21.3% (26) | 38.5% (85) | 0.001 | 42.3% (47) | 27.5% (64) | 0.006 |
| Psychological consult post-discharge for my family | 33.3% (21) | 30.9% (89) | 0.706 | 21.3% (26) | 37.3% (81) | 0.002 | 45.5% (50) | 24.8% (57) | <0.0001 |
| Receiving ICD-related information several times rather than once | 56.3% (36) | 46.4% (135) | 0.153 | 33.6% (41) | 55.7% (123) | <0.0001 | 59.5% (66) | 42.1% (98) | 0.003 |
| Care options . | Women . | Men . | P . | Primary prevention . | Secondary prevention . | P . | SCA . | No SCA . | P . |
|---|---|---|---|---|---|---|---|---|---|
| Personal conversation with doctor/nurse 2–3 weeks post-implant | 63.2% (42) | 58.8% (180) | 0.502 | 50.0% (70) | 62.4% (1439 | 0.080 | 60.3% (70) | 58.5% (144) | 0.744 |
| Doctors/nurses ask how I feel while hospitalized | 60.9% (42) | 48.0% (146) | 0.054 | 40.2% (53) | 54.8% (125) | 0.007 | 52.2% (60) | 48.4% (119) | 0.501 |
| Doctor/nurse calls me post-discharge | 52.2% (36) | 40.5% (124) | 0.077 | 39.1% (52) | 44.1% (101) | 0.353 | 43.1% (50) | 42.1% (104) | 0.858 |
| Same doctor/nurse who talks to me every time | 82.9% (58) | 73.4% (224) | 0.226 | 74.8% (98) | 74.9% (173) | 0.986 | 70.9% (83) | 76.8% (189) | 0.226 |
| Exercise tolerance test | 53.6% (37) | 52.3% (160) | 0.841 | 43.2% (57) | 59.1% (136) | 0.003 | 59.0% (69) | 50.8% (125) | 0. 145 |
| Cardiac rehabilitation | 44.8% (30) | 50.2% (152) | 0.425 | 48.5% (63) | 48.9% (111) | 0.937 | 51.7% (60) | 47.5% (115) | 0.456 |
| Ongoing feedback via remote monitoring system | 64.2% (43) | 60.4% (183) | 0.565 | 58.0% (76) | 63.3% (143) | 0.325 | 60.3% (70) | 62.0% (150) | 0. 766 |
| Opportunity to meet other ICD patients | 33.3% (23) | 24.4% (75) | 0.128 | 25.0% (33) | 26.4% (61) | 0.768 | 24.8% (29) | 26.7% (66) | 0.695 |
| Opportunity to attend ICD workshop with family | 44.9% (31) | 35.5% (108) | 0.145 | 30.0% (39) | 41.3% (95) | 0.033 | 41.9% (49) | 34.8% (85) | 0.195 |
| Psychological consult while hospitalized | 31.7% (20) | 24.0% (69) | 0.198 | 19.0% (23) | 28.6% (63) | 0.050 | 31.3% (35) | 22.2% (51) | 0.069 |
| Psychological consult post-discharge for me | 43.1% (28) | 30.3% (88) | 0.048 | 21.3% (26) | 38.5% (85) | 0.001 | 42.3% (47) | 27.5% (64) | 0.006 |
| Psychological consult post-discharge for my family | 33.3% (21) | 30.9% (89) | 0.706 | 21.3% (26) | 37.3% (81) | 0.002 | 45.5% (50) | 24.8% (57) | <0.0001 |
| Receiving ICD-related information several times rather than once | 56.3% (36) | 46.4% (135) | 0.153 | 33.6% (41) | 55.7% (123) | <0.0001 | 59.5% (66) | 42.1% (98) | 0.003 |
* Numbers highlighted in bold-face indicate statistically significant differences between groups.
Overall patient satisfaction with implantable cardioverter defibrillator-related information provision, treatment, and care
Of the 389 patients, 372 (95.6%) completed an item that tapped into patients' overall satisfaction with their ICD-related treatment and care at the hospital, with 91.1% (n = 339) rating it as extremely or predominantly good, 7.0% (n = 26) as neither good nor bad, and 1.8% (n = 7) as predominantly to considerably bad.
Discussion
In the current study using a mixed-methods design, we examined patients' needs and preferences for information provision and care options and overall satisfaction. We found a high level of satisfaction with information provision, with only 13.1% of patients being either somewhat or very dissatisfied. This is consistent with a recent Dutch study on information provision and satisfaction with information in patients with an ICD.14 However, other studies, such as in patients with prostate cancer, found a higher proportion (i.e. 34%) of patients who were dissatisfied with information provision, which in turn was associated with poorer emotional, social, physical, and role functioning and global health.5
Despite a high level of satisfaction with information provision and treatment in our cohort of ICD patients, several topics were not broached with patients in clinical practice.15 As many as 40% of patients had neither received information about where to obtain psychological support for themselves and their relatives nor information about deactivation of the ICD towards the end of life. The former may be understandable, as few ICD clinics in Denmark have a psychologist or other mental health professionals on board in the multi-disciplinary team. However, the latter finding is disappointing given the two Expert Consensus Statements from the Heart Rhythm Society and the European Heart Rhythm Association published in 2010 recommending that cardiologists discuss the issue of deactivation with patients several times, including prior to implantation.16,17
With respect to patients' preferences and needs for care options, there were several unmet needs that are currently not part of standard clinical practice at Odense University Hospital. As many as 75.2% of patients had missed continuity in care and being able to talk to the same healthcare professional every time. The majority of patients (61.1%) also indicated that they would have preferred to receive continuous feedback via remote monitoring rather than ‘no news is good news’. Although studies have shown that patients tend to be satisfied with remote monitoring,18 others have indicated the downside of missing out on one-on-one contact as well as the risk of co-morbidities going unnoticed by this shift in care.19 In our patient cohort, as many as 59.6% indicated that they would have liked to have a personal conversation with a staff member 2–3 weeks post-implant, which is not part of standard practice due to this shift in care. Other issues that may go unnoticed and undiagnosed is psychological distress, such as anxiety and depression. Although ICD patients in Denmark are not standardly screened for distress in clinical practice, such distress might have been caught in face-to-face interactions between patients and healthcare professionals. Such distress not only impacts on patients' quality of life but also increases the risk of premature death despite state-of-the-art treatment with the ICD.9
More than half of the patients in our study also voiced a preference for undergoing an exercise tolerance test, as part of standard practice post-implant, in order to ascertain how much they were able to do physically. Likely, this also contains a psychological component that relates to fear of shock, loss of confidence, and how much patients can do physically without setting off the ICD.20 Fear of shock has previously been implicated as a predictor not only of persistent depression in ICD patients but also of mortality in patients who had received no prior shocks.9 Particularly women, patients with a secondary prevention indication, and patients who had experienced a sudden cardiac arrest voiced the importance of a psychological consult post-discharge that is currently not available as part of standard practice. Patients having experienced a sudden cardiac arrest also indicated a need for receiving information several times rather than once due to cognitive difficulties, as also described by others.21–24 This subset of patient constitutes a particularly vulnerable subgroup that may have a greater need for person-to-person care, as they also need to come to terms with what has happened, which is particularly dramatic if the arrest was the first onset of symptoms.25
The results of this study should be interpreted with some caution, as it is based on data from a single centre. However, strengths of this study include the use of a mixed-methods design involving patients in the development of the purpose-designed questionnaire, the response rate of 81% when compared with a recent Dutch study with a response rate of 51%,14 and the stratified analyses on a priori determined patient groups to ascertain if needs and preferences for care options differ.
In conclusion, our results emphasize the need to tailor not only information provision but also care options to the individual needs and preferences of patients that may vary with age, sex, health literacy, indication for ICD implantation, and comorbidities, as also suggested by others.7,20 We also identified several unmet needs of patients and their need for care options that are not part of standard practice in our hospital. Despite current challenges to the healthcare system in Denmark and across the world, it might be possible to meet some of the patients' unmet needs, including offering patients an exercise tolerance test and a personal follow-up phone call 2–3 weeks post-implant.
Acknowledgement
We would like to thank all patients for their participation in the study.
Conflict of interest: none declared.
References
- cardiac arrest
- consultation
- implantable defibrillators
- exercise stress test
- feedback
- health personnel
- hospitals, university
- survivors
- terminally ill
- secondary prevention
- cardiac resynchronization therapy
- defibrillators
- medical devices
- emotional support
- implants
- telemonitoring
- conversation
- dissatisfaction



