-
PDF
- Split View
-
Views
-
Cite
Cite
Antonio Hernández Madrid, Tatjana S. Potpara, Nikolaos Dagres, Jian Chen, Torben B. Larsen, Heidi Estner, Derick Todd, Maria G. Bongiorni, Elena Sciaraffia, Alessandro Proclemer, Saida Cheggour, Walid Amara, Carina Blomstrom-Lundqvist, Differences in attitude, education, and knowledge about oral anticoagulation therapy among patients with atrial fibrillation in Europe: result of a self-assessment patient survey conducted by the European Heart Rhythm Association, EP Europace, Volume 18, Issue 3, March 2016, Pages 463–467, https://doi.org/10.1093/europace/euv448
Close - Share Icon Share
Abstract
The purpose of this patient survey was to analyse the knowledge about blood thinning medications relative to gender, age, education, and region of residence in patients with atrial fibrillation (AF). A total of 1147 patients with AF [mean age 66 ± 13 years, 529 (45%) women] from eight European countries responded to this survey. Most patients understood that the indication for anticoagulation therapy was to ‘thin the blood’, but 8.1% responded that the purpose of the medication was to treat the arrhythmia. Patients with college or university grades reported less frequent deviations from their target INR range compared with those without schooling (2.8% vs. 5.1%, P < 0.05). The awareness of anticoagulation-related risk of bleedings was lowest in patients without schooling (38.5%) and highest in those with college and university education (57.0%), P < 0.05. The same pattern was also observed regarding patient's awareness of non-vitamin K antagonist oral anticoagulants (NOACs): 56.5% of the patients with university education and only 20.5% of those without schooling (P < 0.05) knew about NOACs, indicating that information about new anticoagulation therapies remains well below the target. Bleeding events were statistically less frequent in patients on NOACs compared with vitamin K antagonists. The education level and patients' knowledge have a direct influence on the global management of the anticoagulation.
Introduction
Oral anticoagulation (OAC) is the most effective therapy for the prevention of ischaemic stroke or systemic embolism related to atrial fibrillation (AF).1,2 The greatest clinical benefit of OAC is achieved with active close collaboration between physicians and AF patients at risk of stroke.1,2 Shared decision making regarding the initiation of OAC, as well as long-term adherence to OAC therapy are facilitated by informed patient participation in the process of treatment.
Medical management of patients with AF is continuously improving due to the adoption to guidelines with better risk stratification, and perhaps better adherence to therapy, including non-vitamin K oral anticoagulants (NOACs). The way of transmitting the knowledge may have important implications for the adherence to guidelines and treatment outcomes. There may be regional differences regarding OAC use, although less is known about the patient's education and knowledge in different countries.
The purpose of this European Heart Rhythm Association (EHRA) survey was to analyse the knowledge and attitude towards thromboprohylactic medications in relation to gender, age, education, and region of residence among AF patients.
Methods
The survey was designed and approved by the members of the EHRA Scientific Initiatives Committee in collaboration with the French National College of Cardiologists (CNCH), as previously described.3 The understanding and ease of use of the survey questionnaire was tested in advance in clinical practice to obviate misinterpretations by participating patients. The questionnaire, consisting of 40 questions in patients' native language, was created on an online electronic platform, and the link was sent to the EHRA Electrophysiology (EP) Research Network centres. The countries invited to participate were France, Denmark, Sweden, Spain, Norway, Germany, Italy, and the UK, all of which had country coordinators in the Scientific Initiatives Committee. The EP Research Network centres were instructed to approach hospitals, outpatient clinics, and specific patient associations or organizations. In-hospital and outpatients diagnosed with AF and taking OAC were eligible. Each patient was asked to enter their individual data without any interference from medical staff. All data were collected anonymously, and the study was conducted during a 3-month period.
Statistical analysis
Values are expressed as mean ± standard deviation for continuous data and as numbers or percentages for categorical data. Distributions of categorical data were examined by the χ2 test or Fisher's exact test, as appropriate. Continuous data were compared using Student's t-test or the Mann–Whitney U test, as appropriate. The normal distribution of data was tested using the Kolmogorov–Smirnov and Shapiro–Wilk tests. The analyses were performed using SPSS software for windows, version 19.0 (IBM Corporation, Armonk, NY, USA).
Results
Patient population
Of 1147 patients participating in the survey, 529 (46.1%) were women; mean age was 66 ± 13 years. The patients were from France (386 patients, 33.6%), Denmark, (305, 26.6%), Sweden, (240, 20.9%), Spain (88, 7.7%), Norway, (51, 4.5%), Germany (43, 3.7%), UK, (25, 2.2%), and Italy (9 patients, 0.8%).
The survey contained the question whether a patient had an ongoing ‘blood thinning’ medication or not, and which of the listed ‘blood thinning’ agents the patient was currently taking, including country-specific trade names of anticoagulants and antiplatelet agents. There were no differences in NOAC use with respect to age or gender. A total of 160 men (25.8%) and 123 woman (23.9%) were treated with NOAC (P = 0.42). The use of specific anticoagulants differed across Europe. Among the vitamin K antagonists (VKA), warfarin was most frequently used in Denmark, Germany, Norway, Sweden, and UK than in France or Spain (88% in Norway vs. 4.7% in Spain), while acenocumarol was most frequently used in Spain (91.2%); and fluindione in France (77.1%) (P < 0.05). Aspirin as an antiplatelet agent was most commonly used in Norway (22%) and lowest in France (7%) (Figure 1). The use of clopidogrel, prasugrel, or ticagrelor was similar.
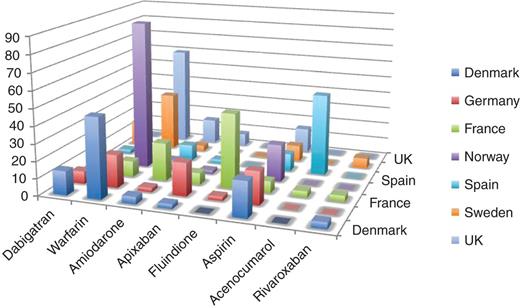
Differences in anticoagulation and antiplatelet therapies by country. Data are shown in percentage.
The use of VKAs, NOACs, and antiplatelet agents reported by patients differed across the countries. There were also regional differences regarding the preference of a certain NOAC or anticoagulant as reported by patients participating in this survey. Dabigatran was more frequently used in Denmark and Sweden, apixaban was more frequently used in Germany, and rivaroxaban was preferred in France, Spain, and Norway.
Knowledge of oral anticoagulation and the need for monitoring
When patients were asked about the purpose of their anticoagulation medication, the majority (91–94%) reported that the indication for anticoagulation therapy was to ‘thin the blood’. However, a non-negligible proportion of patients (6–9%) replied that the treatment was to control the arrhythmia. Regarding adherence to therapy, 28.7% of men and 24.5% of women (P < 0.05) reported forgetting to take their medication occasionally; younger patients were more likely to forget their medication than patients over 65 years (31.3 vs. 24%, P < 0.05).
The frequency of blood tests for monitoring of OAC therapy did not differ across countries, and monthly testing was most common. When asked about their INR targets, 91% knew that the INR target level should be kept between 2 and 3, while 3% believed it should be < 2, and 6% believed that the target INR should be > 3.
Most of the patients state they can continue their normal daily life activities, such as travelling by plane, participating in sport, driving a car or having a job, being more frequently acknowledged by men than by women (P < 0.05).
Discontinuation of anticoagulation was reported by 14.5% of participants. The reason for the withdrawal of therapy was unknown in 25.8% of the younger patients and 21.1% of the older individuals (P < 0.05), while the second most common reason was discontinuation by their doctors (8.9% in younger and 11.8% in older patients, P < 0.05), and the third most common cause was that the patient did not want regular blood test.
Of the entire cohort, 40% of the patients were informed of the availability of NOACs. However, many patients were not aware of the fact that blood tests were not necessary for testing the efficacy of NOACs, (29.6% men and 32.7% women). A minority of the patients (25.8% of men and 28.4% of women) recognized that NOACs were at least as effective as warfarin (Table 1). The knowledge about the need for regular kidney function tests and to a certain extent liver function monitoring, and potentials interactions with other drugs, which should be avoided, generally was low, ranging between 15 and 38%, particularly in patients who were not on NOACs.
| Questions . | Male . | Female . | P-value . | Younger . | Elderly . | P-value . |
|---|---|---|---|---|---|---|
| Awareness of NOACS | 40.60 | 41.20 | ns | 57.3 | 30.0 | <0.05 for age |
| Patient knowledge about NOACS | ||||||
| No blood tests are necessary | 29.60 | 32.70 | ns | 41.1 | 34.1 | <0.05 for age |
| Kidney function needs to be tested | 17 | 18.50 | ns | 23.6 | 13.8 | <0.05 for age |
| The risk of serious bleeding | 18 | 19.30 | ns | 26.0 | 13.6 | <0.05 for age |
| NOACS are as effective as warfarin | 24.80 | 28.40 | <0.05 | 35.1 | 21.3 | <0.05 for age |
| Not for mechanical heart valves | 9.80 | 7.50 | ns | 11.0 | 7.2 | ns |
| Questions . | Male . | Female . | P-value . | Younger . | Elderly . | P-value . |
|---|---|---|---|---|---|---|
| Awareness of NOACS | 40.60 | 41.20 | ns | 57.3 | 30.0 | <0.05 for age |
| Patient knowledge about NOACS | ||||||
| No blood tests are necessary | 29.60 | 32.70 | ns | 41.1 | 34.1 | <0.05 for age |
| Kidney function needs to be tested | 17 | 18.50 | ns | 23.6 | 13.8 | <0.05 for age |
| The risk of serious bleeding | 18 | 19.30 | ns | 26.0 | 13.6 | <0.05 for age |
| NOACS are as effective as warfarin | 24.80 | 28.40 | <0.05 | 35.1 | 21.3 | <0.05 for age |
| Not for mechanical heart valves | 9.80 | 7.50 | ns | 11.0 | 7.2 | ns |
Data are shown as percentages of patient's knowledge of a certain question.
| Questions . | Male . | Female . | P-value . | Younger . | Elderly . | P-value . |
|---|---|---|---|---|---|---|
| Awareness of NOACS | 40.60 | 41.20 | ns | 57.3 | 30.0 | <0.05 for age |
| Patient knowledge about NOACS | ||||||
| No blood tests are necessary | 29.60 | 32.70 | ns | 41.1 | 34.1 | <0.05 for age |
| Kidney function needs to be tested | 17 | 18.50 | ns | 23.6 | 13.8 | <0.05 for age |
| The risk of serious bleeding | 18 | 19.30 | ns | 26.0 | 13.6 | <0.05 for age |
| NOACS are as effective as warfarin | 24.80 | 28.40 | <0.05 | 35.1 | 21.3 | <0.05 for age |
| Not for mechanical heart valves | 9.80 | 7.50 | ns | 11.0 | 7.2 | ns |
| Questions . | Male . | Female . | P-value . | Younger . | Elderly . | P-value . |
|---|---|---|---|---|---|---|
| Awareness of NOACS | 40.60 | 41.20 | ns | 57.3 | 30.0 | <0.05 for age |
| Patient knowledge about NOACS | ||||||
| No blood tests are necessary | 29.60 | 32.70 | ns | 41.1 | 34.1 | <0.05 for age |
| Kidney function needs to be tested | 17 | 18.50 | ns | 23.6 | 13.8 | <0.05 for age |
| The risk of serious bleeding | 18 | 19.30 | ns | 26.0 | 13.6 | <0.05 for age |
| NOACS are as effective as warfarin | 24.80 | 28.40 | <0.05 | 35.1 | 21.3 | <0.05 for age |
| Not for mechanical heart valves | 9.80 | 7.50 | ns | 11.0 | 7.2 | ns |
Data are shown as percentages of patient's knowledge of a certain question.
Role of education
The use of aspirin was reported by 10.1–20% of the patients, most frequently by those with some college credit and less commonly by patients with college or university education and patients with nursery school to 8th grade patients. The use of NOACs ranged from 29.5% in patients with some college credit to 17.9% in patients without schooling (P < 0.05%).
The educational level did not differ between patients who were aware of the purpose of the OAC therapy ‘to thin the blood’ and those who believed that the drugs were used for the arrhythmia per se. Patients with a high educational level (college or university degree) more frequently managed their dosing themselves compared with other groups (21.9 vs. 12.9% in patients without schooling; P < 0.05). Patients have also been asked whether INR ever go higher than the upper limit of the target level. Patients without schooling were more likely to report that INR exceeded the upper limit several times a month (5.1 vs. 2.8% of college or university-educated patients, P < 0.05).
The majority (80.2%) of patients with university education knew that they could continue their normal daily activities such as travelling by plane, sports, driving a car, or having a job, compared with patients without schooling (51.8%, P < 0.05).
A higher proportion (56.5%) of patients with university education have heard about NOACs as opposed to only 20.5% of patients without schooling (P < 0.05); thus, this awareness remains relatively low; 15.3% of the patients without schooling did not know that blood tests were not necessary for NOACs, in contrast to what was required for warfarin. The fact NOACs are at least as effective as warfarin was recognized by 2.5% of patients without schooling and 25% of patients with trade/technical education, and up to 42.4% of patients with university education (P < 0.05).
Patients without schooling reported the highest rate of bleeding on anticoagulant, and the highest rate of previous stroke (2.6% as compared with 0.71% in those with college and university education, P < 0.05) (Table 2). These patients also had the lowest use of VKAs or NOACs for prevention of stroke, even after correction for other possible factors that may influence appropriate OAC therapy. The use of NOACs was also less frequent, than the use of VKAs, ranging from 17.9% in patients without schooling to the 25.8% in patients with college or university education and 29.1% in patients with some college credit.
| . | Yes . | No . | P-value . |
|---|---|---|---|
| Age >65 (n = 652) | 22.4 | 77.6 | 0.20 |
| Age <65 (n = 469) | 19.6 | 80.4 | |
| Gender male (n = 620) | 20.6 | 79.4 | 0.81 |
| Gender female (n = 517) | 21.3 | 78.7 | |
| No schooling (n = 39) | 23 | 77 | 0.51 |
| College university (n = 283) | 18.7 | 81.3 | |
| VKA (n = 579) | 26.8 | 73.2 | 0.0003 |
| NOAC (n = 283) | 17.7 | 82.3 |
| . | Yes . | No . | P-value . |
|---|---|---|---|
| Age >65 (n = 652) | 22.4 | 77.6 | 0.20 |
| Age <65 (n = 469) | 19.6 | 80.4 | |
| Gender male (n = 620) | 20.6 | 79.4 | 0.81 |
| Gender female (n = 517) | 21.3 | 78.7 | |
| No schooling (n = 39) | 23 | 77 | 0.51 |
| College university (n = 283) | 18.7 | 81.3 | |
| VKA (n = 579) | 26.8 | 73.2 | 0.0003 |
| NOAC (n = 283) | 17.7 | 82.3 |
| . | Yes . | No . | P-value . |
|---|---|---|---|
| Age >65 (n = 652) | 22.4 | 77.6 | 0.20 |
| Age <65 (n = 469) | 19.6 | 80.4 | |
| Gender male (n = 620) | 20.6 | 79.4 | 0.81 |
| Gender female (n = 517) | 21.3 | 78.7 | |
| No schooling (n = 39) | 23 | 77 | 0.51 |
| College university (n = 283) | 18.7 | 81.3 | |
| VKA (n = 579) | 26.8 | 73.2 | 0.0003 |
| NOAC (n = 283) | 17.7 | 82.3 |
| . | Yes . | No . | P-value . |
|---|---|---|---|
| Age >65 (n = 652) | 22.4 | 77.6 | 0.20 |
| Age <65 (n = 469) | 19.6 | 80.4 | |
| Gender male (n = 620) | 20.6 | 79.4 | 0.81 |
| Gender female (n = 517) | 21.3 | 78.7 | |
| No schooling (n = 39) | 23 | 77 | 0.51 |
| College university (n = 283) | 18.7 | 81.3 | |
| VKA (n = 579) | 26.8 | 73.2 | 0.0003 |
| NOAC (n = 283) | 17.7 | 82.3 |
Bleeding events
History of bleeding was reported by 13% of patients. More than half the patients (54%) declared that anticoagulation was associated with increased risk of minor bleeding, while 26% believed that it increased risk of all bleedings (including major bleeding). The perception of low risk of anticoagulation, as well as the perception of no risk at all, was similar in all countries. The only statistically significant parameter was the intake of NOAC, which was associated with a lower rate of bleeding than that observed in patients taking VKA (P < 0.05).
Discussion
According to the results of our survey, there were no age-related differences regarding the use of VKAs and NOACs. There was a significant proportion of patients (around 8%) who did not understand the purpose of anticoagulation correctly. Surprisingly, the number of patients who were aware of NOACs was also quite small. A small percentage of patients used ‘self-medication’, i.e. managing the dose of VKAs themselves, both among the younger and older patients.
Gender-related differences in the clinical presentation and outcome seem to relate to differences in platelet biology and coagulation reactions, resulting in different rates of thromboembolic and bleeding events, according to previous studies.4–6 However, the understanding and management of anticoagulation could also be important. Similar proportions of men and women discontinued anticoagulation therapy, which was most frequently related to the advice from their doctors. In our survey, there were no significant differences in the management of OAC treatment by gender, apart from the observation that men more frequently than women managed the dosing themselves.
This survey provides some insights into the current patient's knowledge, education, and compliance regarding OAC therapy. Despite the widespread guidelines on management of AF,4,5 there are significant regional differences regarding age, gender, country, and educational level among AF patients across Europe. The EHRA Practical Guide for NOAC use6,7 recommends mandatory regular monitoring of renal function on a yearly basis in patients with normal or mild renal impairment and more frequently in patients with moderate renal impairment. Widespread education programmes on AF and anticoagulation are needed for physicians, as well as user friendly patient educational material to overcome regional differences in OAC therapy.
The prospective study by Poli et al.8 found no differences regarding the quality of anticoagulation or bleeding risk between the genders (P = 0.5). The higher rate of embolic events in women compared with men was confirmed using Cox regression analysis after correction for age (P = 0.009). Strokes occurring in women were more disabling, and relative risk (RR) for severe and fatal stroke, defined according to the modified Rankin scale, in women vs. men was 3.1 [95% confidence intervals (CI) 1.3–6.5; P = 0.001], despite the similar quality of anticoagulation.
Medical management of patients with AF is continuously improving because of better adherence to the guidelines, better risk stratification, and perhaps a quick adoption of NOACs. The PREFER in AF (PREvention oF thromboembolic events—European Registry in Atrial Fibrillation) registry analysed 7243 consecutive patients with AF in seven European countries in 2012–13.9,10 Patients were older than in our survey (mean age 71.5 ± 10.7 years) and had a higher mean CHA2DS2–VASc score (3.4). The study showed important differences in the use of anticoagulation across countries. Warfarin was used predominantly in the UK (74.9%), phenprocoumon in Germany (74.1%), acenocoumarol in Spain (67.3%), and fluindione in France (61.8%).
The NOAC use ranged from 31.9% in Swedish patients to 8.2% in Norway (P < 0.05%) in our survey. There were regional differences regarding the preference for certain anticoagulants. Dabigatran was more frequently used in Denmark and Sweden, apixaban in Germany, and rivaroxaban was more frequently used in France, Spain, and Norway. These differences may be difficult to interpret, but could at least in part be related to problems in introducing a new product into the market by each government and also due to differences in reimbursement among countries.
Temporary VKA discontinuation and bridging with other anticoagulants was frequent, and time in the therapeutic range defined as at least two of the last three available INR values between 2.0 and 3.0 prior to enrolment, ranged from 70.3% in Spain to 81.4% in Germany. The global quality of anticoagulation management was relatively homogenous across countries.
Educational differences
Patients with the highest educational level were more frequently treated with NOACs [29.5% in patients with some college credit to 17.9% in patients without schooling (P < 0.05%)]. The continuation of OAC therapy may be affected by diet modifications, other drugs, co-morbidities, compliance, and patient's education.11–14 In our survey, there were important education-related differences regarding information given about anticoagulation, management, and permitted patient activities. Even among university-educated patients not all knew about NOACs. The perception of risk imposed by anticoagulants was also different.
The study on patient's education with respect to OAC therapy showed that a greater emphasis should be given to educational courses for anticoagulated patients; administration of the questionnaire leads to a significant improvement in anticoagulation quality.15 Educational interventions significantly influence the patient's knowledge and perception of AF. Other surveys emphasized the need for structured educational programs to improve the use of OAC. Recently, an EHRA consensus document emphasized the need for education of patients with AF.16
Conclusion
The differences in the educational level may compromise the safety and efficacy of anticoagulants. The results of this survey show that there is still a place for improvement of education and compliance among patients on OAC. Education of AF patients should be reinforced to improve anticoagulation in clinical practice. Of particular interest, there is a need of education for patients taking NOACs.
Acknowledgements
The production of this EP wire document is under the responsibility of the Scientific Initiative Committee of the European Heart Rhythm Association: Carina Blomström-Lundqvist (chairman), Maria Grazia Bongiorni (co-chair), Jian Chen, Nikolaos Dagres, Heidi Estner, Antonio Hernandez-Madrid, Melèze Hocini, Torben Bjerregaard Larsen, Laurent Pison, Tatjana Potpara, Alessandro Proclemer, Elena Sciaraffia, Derrik Todd. Document reviewer for EP-Europace: Irene Savelieva (St George's University of London, London, UK). We acknowledge the EHRA Research Network centres participating in this EP wire and the collaboration with chairs/presidents of National Workings Groups/Societies of Arrhythmias and the Collaboration with The French National College of Cardiologists. A list of the collaboration can be found on EHRA website.
Conflict of interest: none declared.



