-
PDF
- Split View
-
Views
-
Cite
Cite
Andrea Ungar, Francesca Tesi, Valentina Maddalena Chisciotti, Giuseppe Pepe, Simone Vanni, Stefano Grifoni, Daniela Balzi, Martina Rafanelli, Niccolò Marchionni, Michele Brignole, Assessment of a structured management pathway for patients referred to the Emergency Department for syncope: results in a tertiary hospital, EP Europace, Volume 18, Issue 3, March 2016, Pages 457–462, https://doi.org/10.1093/europace/euv106
Close - Share Icon Share
Abstract
High hospitalization rates (39–58% in the literature) of patients admitted to Emergency Department (ED) for transient loss of consciousness (T-LOC) suspected for syncope are still an unresolved issue. The presence of an Observation Unit has reduced hospital admissions and the duration of hospitalization in controlled studies, and a Syncope Unit (SU) in the hospital may reduce hospitalization and increase the number of diagnoses in patients with T-LOC. We assessed the effect of a structured organization on hospitalization rate and outcome.
Consecutive patients referred to the ED for a T-LOC of a suspected syncopal nature as the main diagnosis were included. The ED physician was trained to choose between: hospital admission (directly or after short observation); discharge after short (<48-h) observation; discharge on a fast track to the SU; and direct discharge without any further diagnostics. From January to June 2010, 362 patients were evaluated in the ED: 29% were admitted, 20% underwent short observation in the ED, 20% were referred to the SU, and 31% were directly discharged. Follow-up data were available on 295 patients who were discharged alive: of these, 1 (0.3%) previously hospitalized patient died within 30 days and 16 (5.4%) died within 1 year. Death rates were 12.9, 3.3, 0, and 2.5% among admitted, observation, SU, and ED-discharged patients, respectively. No death could be directly attributed to T-LOC. Re-admission within 1 year for any cause occurred in 72 (24%) patients; re-admission rates were 45.9, 19.3, 11.5, and 18.0% among admitted, observation, SU, and ED-discharged patients, respectively.
The availability of short observation and a SU seems to reduce the hospitalization rate compared with previous reported historical reports from our and other centres. Most deaths during follow-up occurred in patients who had been hospitalized. High rates of re-admission to the ED within 1 year are still an issue.
We assessed the effect of a structured management pathway ED model of organization for patients with Syncope.
The presence of a short observation and a Syncope Unit reduced hospitalizations.
The short- and long-term mortality of patients in whom syncope is the principal reason for referral is low and generally unrelated to the mechanism of syncope.
A high re-admission to ED in the year after the first access to ED remains an issue.
Introduction
Syncope is difficult to manage in the Emergency Department (ED). Consequently, hospitalization rates remain high (around 50%), despite the fact that protocols include structured pathways to increase diagnostic and therapeutic strategies (see Supplementary material online, Appendix 1).
On the basis of the European Society of Cardiology (ESC) guidelines on syncope,1 a systematic evaluation of the management of transient loss of consciousness (T-LOC) in which syncope was suspected was carried out by the EGSYS 2 Study,2 in which our hospital took part. Following that study, we created a structured pathway for patients referred to the ED for syncopal T-LOC; this involves a Short-Stay Observation Unit inside the ED and a Syncope Unit (SU) outside the ED. Short-Stay Observation has proved to reduce hospital admissions and hospital stay in controlled studies.3,4 The SU may reduce hospitalization and increase the number of diagnoses in patients with T-LOC.5 To our knowledge, there are currently no studies to confirm our results in clinical practice.
The aim of the present study was to assess the effect of a novel organizational model on hospitalization rates and outcomes in a large tertiary university hospital.
Methods
Patients
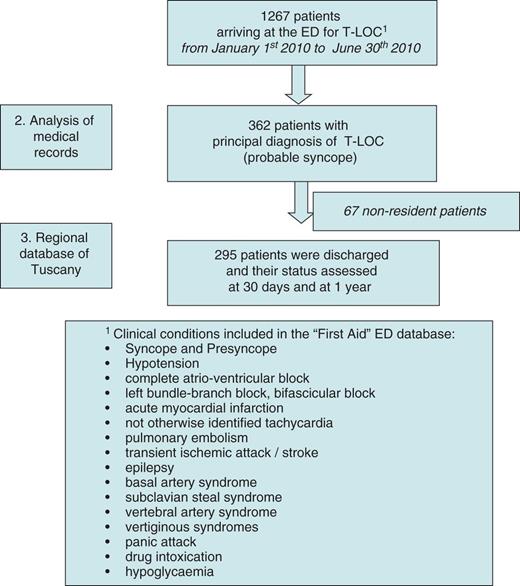
The study involved consecutive patients referred to the ED of Careggi Hospital for T-LOC in which syncope was suspected as the main diagnosis, from 1 January to 30 June 2010. Patients were identified among those who attended the ED for a condition that was ascribed to a T-LOC (Figure 1). We excluded those in whom syncope was a secondary manifestation of a different disease (i.e. syncope as a secondary diagnosis) and those who had an immediate diagnosis in the ED of non-syncopal T-LOC (epilepsy, functional, transient ischaemic attack, stroke, basal or vertebral artery syndrome, subclavian steal syndrome, vertiginous syndromes, panic attack, drug intoxication, and hypoglycaemia).
Hospital organization
On the basis of the EGSYS 22 experience, the ED adopted the following organization, and emergency physicians were trained to assign patients with T-LOC to one of the following pathways (Figure 2):
Hospital admission (directly or after a limited period of time in Short-Stay Observation).
Discharge after Short-Stay Observation (usually within 24 h, but with the possibility to extend the stay up to 48 h if needed).
Discharge with Fast-track visit scheduled in the SU (web-based scheduled directly from the ED or after Short-Stay Observation).
Discharge (directly from the ED).
During the conventional ED evaluation, which usually lasts 5 h (range 3–10 h), emergency physicians are trained to choose the best diagnostic-therapeutic pathway, based on risk stratification as a general guide, in order to assess the risk of death and life-threatening events and the risk of syncope recurrence and physical injury in the short term. Emergency physicians are advised to implement risk stratification in accordance with ESC guidelines.1 On the basis of ED evaluation, high-risk patients are hospitalized directly from the ED, intermediate-risk patients are sent to the Short-Stay Observation Unit or to the SU, as deemed appropriate, and low-risk patients are discharged.
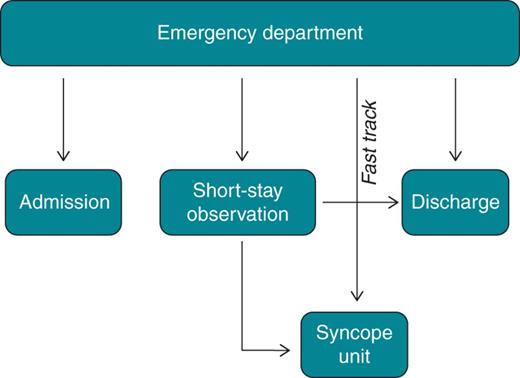
Careggi Model: different assignment after evaluation in the ED. Some of the patients assigned to Short-Stay Observation can be admitted or referred to the SU at the end of the 48-h observation, when clinically indicated. For a description of the pathways, see the text.
In Short-Stay Observation Unit, inside the ED, patients with T-LOC undergo, when necessary, continuous in-bed ECG monitoring, blood tests, echocardiography, stress testing, and vessel ultrasound examination. Neuroautonomic evaluation (Tilt Table Test and Carotid Sinus Massage) is not provided in the ED or in Short-Stay Observation, whereas it may be performed in patients admitted to the hospital. The final risk stratification and the subsequent assignment are decided by ED physicians on the basis of their clinical judgement6 and current practice. The EGSYS score2–5 was calculated in all patients a posteriori by the authors of this paper.
The SU is located in a physically separate ward.
Follow-up
For the purpose of the present study, outcome measures were: hospitalization rate, short (≤1 month) and late (1–12 months) mortality after discharge, re-admission rate within 1 year of discharge in patients admitted and discharged. Life status after hospital discharge was assessed by consulting the Registry Office of the municipalities of residence in Tuscany. Re-admissions were obtained by consulting the hospital discharge database following the index ED presentation.
Statistical analysis
Categorical variables are presented as percentages and were compared by means of the χ2 test for multiple comparisons. As continuous variables were non-normally distributed on the Shapiro–Wilk test, they were expressed as medians and interquartile ranges (25th and 75th percentiles) and compared by using the non-parametric Wilcoxon rank-sum test. One-month hospital re-admission, 1-year hospital re-admission, and 1-year mortality risks were estimated by means of Cox proportional hazard models adjusted for age, sex, diabetes, ischaemic heart disease, depression, and EGSYS score. In Cox regression models, hazard ratios (HRs) and 95% confidence interval (CI) were calculated. Estimated hazard curves by diagnosis or by destination from the ED were evaluated by means of Cox proportional hazards methods, after adjustment for confounders. The methods proposed by Grambsch and Therneau7 and by May and Hosmer8 were used to check the proportional hazards assumption and the goodness-of-fit of the models, respectively. Statistical significance was defined as P ≤ 0.05. Analyses were performed by means of the STATA statistical package (version 11.0, Stata Corporation, College Station, TX, 2009).
Results
Baseline
We screened 1267 patients (Figure 1) from the ‘first aid’ ED database and identified 362 [mean age 62 ± 20 years (range: 15–101)] who had received a diagnosis of suspected syncopal T-LOC: 167 patients (56.6%) had prodromal symptoms, 32.5% had a history of syncope in the previous 2 years, and 75.6% had comorbidity (53.2% a cardiovascular disease) deemed not directly responsible for T-LOC.
In the follow-up study, which was based on consultation of the Regional Registry of Tuscany, 67 patients were excluded because they resided outside the region. Thus, we obtained follow-up data on 295 patients.
Diagnosis
Emergency Department diagnoses were: neurally mediated syncope in 37.3%, cardiac syncope in 9.5%, non-syncopal T-LOC in 9.5%, and unexplained syncope in 37.3% of the cases. At the end of the diagnostic work-up, neurally mediated syncope was established in 59.3% of cases, cardiac in 11.5%, non-syncopal T-LOC in 11.2%, and unexplained in 18%.
Diagnostic-therapeutic pathways
Of the 295 patients, 85 (29%) were admitted to hospital (length of hospitalization 5.2 ± 2.1 days), 60 (20%) were discharged after Short-Stay Observation, 58 (20%) were sent to the SU (via fast-track appointment), and 92 (31%) were discharged directly from the ED. Most (80%) of the 67 patients assigned to Short-Stay Observation were kept in for ≤24 h, while the remaining 20% stayed for 24–48 h. There are not differences in clinical characteristics between these two groups (data not shown). At the end of the observation period, 7 (10%) were hospitalized and 4 (6%) were referred to the SU in order to undergo Tilt Table Testing and Carotid Sinus Massage. The mean delay between ED discharge and the first visit in the SU was 24 ± 5 days.
Hospitalized patients were older (Wilcoxon rank-sum test = 50.12, P < 0.0001 vs. other groups), more frequently had cardiovascular disease or pathologic ECG and had a higher EGSYS score than the other groups (Wilcoxon rank-sum test = 35.96, P < 0.0001 vs. other groups; Table 1). In 20% of the hospitalized patients, a diagnosis of suspected cardiac syncope was made, while in 52% unexplained syncope was diagnosed. A low percentage (8.3%) of patients placed in Short-Stay Observation had a diagnosis of cardiac syncope and a higher percentage (33.4%) had unexplained syncope. More than a half (56.9%) of patients referred to the SU received no diagnosis. The majority (76.1%) of the patients discharged directly from the ED had neurally mediated syncope (Table 1).
| . | Admissions (n = 85) . | Short-Stay Observation (n = 60) . | Syncope Unit (n = 58) . | Discharges (n = 92) . | P . |
|---|---|---|---|---|---|
| Age (median, interquartile range) | 77 (71–84) | 68.5 (47–79) | 62.5 (43–78) | 53.0 (32.7–74.5) | <0.001 |
| EGSYS Score (median, interquartile range) | 3 (1;3) | 2 (0;3) | 1.5 (−1;3) | 0.4 (−1;2) | <0.001 |
| Abnormal ECG, n (%a) | 23 (27.1) | 12 (20.0) | 9 (15.5) | 6 (6.5) | 0.005 |
| EGSYS score >3, n (%a) | 45 (52.9) | 17 (28.3) | 10 (17.2) | 14 (15.2) | <0.001 |
| CV disease, n (%a) | 64(75.3) | 33 (55.0) | 27 (46.6) | 32 (34.8) | <0.001 |
| Trauma, n (%a) | 22 (25.9) | 16 (26.7) | 12 (20.7) | 14 (15.2) | 0.397 |
| ED diagnosis | |||||
| Cardiac syncope, n (%a) | 17 (20.0) | 5 (8.3) | 3 (5.2) | 3 (3.2) | <0.001 |
| Neurally mediated syncope, n (%a) | 13 (15.3) | 26 (43.3) | 20 (34.5) | 70 (76.1) | <0.001 |
| Non-syncopal T-LOC, n (%a) | 11 (12.9) | 9 (15.0) | 2 (3.4) | 6 (6.5) | <0.001 |
| Unexplained syncope, n (%a) | 44 (51.8) | 20 (33.4) | 33 (56.9) | 13 (14.1) | <0.001 |
| . | Admissions (n = 85) . | Short-Stay Observation (n = 60) . | Syncope Unit (n = 58) . | Discharges (n = 92) . | P . |
|---|---|---|---|---|---|
| Age (median, interquartile range) | 77 (71–84) | 68.5 (47–79) | 62.5 (43–78) | 53.0 (32.7–74.5) | <0.001 |
| EGSYS Score (median, interquartile range) | 3 (1;3) | 2 (0;3) | 1.5 (−1;3) | 0.4 (−1;2) | <0.001 |
| Abnormal ECG, n (%a) | 23 (27.1) | 12 (20.0) | 9 (15.5) | 6 (6.5) | 0.005 |
| EGSYS score >3, n (%a) | 45 (52.9) | 17 (28.3) | 10 (17.2) | 14 (15.2) | <0.001 |
| CV disease, n (%a) | 64(75.3) | 33 (55.0) | 27 (46.6) | 32 (34.8) | <0.001 |
| Trauma, n (%a) | 22 (25.9) | 16 (26.7) | 12 (20.7) | 14 (15.2) | 0.397 |
| ED diagnosis | |||||
| Cardiac syncope, n (%a) | 17 (20.0) | 5 (8.3) | 3 (5.2) | 3 (3.2) | <0.001 |
| Neurally mediated syncope, n (%a) | 13 (15.3) | 26 (43.3) | 20 (34.5) | 70 (76.1) | <0.001 |
| Non-syncopal T-LOC, n (%a) | 11 (12.9) | 9 (15.0) | 2 (3.4) | 6 (6.5) | <0.001 |
| Unexplained syncope, n (%a) | 44 (51.8) | 20 (33.4) | 33 (56.9) | 13 (14.1) | <0.001 |
ED diagnosis in relation to assignment.
EGSYS, Evaluation of Guidelines in SYncope Study; CV, cardiovascular; ED, Emergency Department.
a% refers to patients with the same assignment.
| . | Admissions (n = 85) . | Short-Stay Observation (n = 60) . | Syncope Unit (n = 58) . | Discharges (n = 92) . | P . |
|---|---|---|---|---|---|
| Age (median, interquartile range) | 77 (71–84) | 68.5 (47–79) | 62.5 (43–78) | 53.0 (32.7–74.5) | <0.001 |
| EGSYS Score (median, interquartile range) | 3 (1;3) | 2 (0;3) | 1.5 (−1;3) | 0.4 (−1;2) | <0.001 |
| Abnormal ECG, n (%a) | 23 (27.1) | 12 (20.0) | 9 (15.5) | 6 (6.5) | 0.005 |
| EGSYS score >3, n (%a) | 45 (52.9) | 17 (28.3) | 10 (17.2) | 14 (15.2) | <0.001 |
| CV disease, n (%a) | 64(75.3) | 33 (55.0) | 27 (46.6) | 32 (34.8) | <0.001 |
| Trauma, n (%a) | 22 (25.9) | 16 (26.7) | 12 (20.7) | 14 (15.2) | 0.397 |
| ED diagnosis | |||||
| Cardiac syncope, n (%a) | 17 (20.0) | 5 (8.3) | 3 (5.2) | 3 (3.2) | <0.001 |
| Neurally mediated syncope, n (%a) | 13 (15.3) | 26 (43.3) | 20 (34.5) | 70 (76.1) | <0.001 |
| Non-syncopal T-LOC, n (%a) | 11 (12.9) | 9 (15.0) | 2 (3.4) | 6 (6.5) | <0.001 |
| Unexplained syncope, n (%a) | 44 (51.8) | 20 (33.4) | 33 (56.9) | 13 (14.1) | <0.001 |
| . | Admissions (n = 85) . | Short-Stay Observation (n = 60) . | Syncope Unit (n = 58) . | Discharges (n = 92) . | P . |
|---|---|---|---|---|---|
| Age (median, interquartile range) | 77 (71–84) | 68.5 (47–79) | 62.5 (43–78) | 53.0 (32.7–74.5) | <0.001 |
| EGSYS Score (median, interquartile range) | 3 (1;3) | 2 (0;3) | 1.5 (−1;3) | 0.4 (−1;2) | <0.001 |
| Abnormal ECG, n (%a) | 23 (27.1) | 12 (20.0) | 9 (15.5) | 6 (6.5) | 0.005 |
| EGSYS score >3, n (%a) | 45 (52.9) | 17 (28.3) | 10 (17.2) | 14 (15.2) | <0.001 |
| CV disease, n (%a) | 64(75.3) | 33 (55.0) | 27 (46.6) | 32 (34.8) | <0.001 |
| Trauma, n (%a) | 22 (25.9) | 16 (26.7) | 12 (20.7) | 14 (15.2) | 0.397 |
| ED diagnosis | |||||
| Cardiac syncope, n (%a) | 17 (20.0) | 5 (8.3) | 3 (5.2) | 3 (3.2) | <0.001 |
| Neurally mediated syncope, n (%a) | 13 (15.3) | 26 (43.3) | 20 (34.5) | 70 (76.1) | <0.001 |
| Non-syncopal T-LOC, n (%a) | 11 (12.9) | 9 (15.0) | 2 (3.4) | 6 (6.5) | <0.001 |
| Unexplained syncope, n (%a) | 44 (51.8) | 20 (33.4) | 33 (56.9) | 13 (14.1) | <0.001 |
ED diagnosis in relation to assignment.
EGSYS, Evaluation of Guidelines in SYncope Study; CV, cardiovascular; ED, Emergency Department.
a% refers to patients with the same assignment.
Follow-up
Hospital re-admissions
Early (1 month): five (14.7%) patients with a final diagnosis of cardiac syncope were re-admitted within 1 month, as were 5 (15.1%) with non-syncopal T-LOC and 6 (11.3%) without a final diagnosis; 2.9% of the patients with neurally mediated syncope were re-admitted. After adjustment for age, final assignment, final diagnosis, and EGSYS score, direct admission from the ED was the only predictor of re-admission: (HR = 5.78, 95% CI: 2.25–15.85, P < 0.001).
Late (12 months): 15 (44.1%) patients with cardiac syncope, 15 (45.4%) with non-syncopal T-LOC, and 16 (30.2%) with unexplained syncope were re-admitted. Re-admission for any cause occurred in 39 (45.9%) previously hospitalized patients, in 11 (19.3%) previously kept in Short-Stay Observation, in 6 (11.5%) previously referred to the SU, and in 16 (17.4%) previously discharged.
On multivariate analysis, the predictors of re-admission within 1 year were direct admission from the ED (HR = 2.44, 95% CI: 1.24–4.80, P < 0.001) and a final diagnosis of non-syncopal T-LOC (HR = 2.11, 95% CI: 1.04–4.28, P < 0.001).
Death
Early (1 month): the early mortality rate was 0.03% (1/295 patients). A 72-year-old man with hypertension and coronary artery disease, but low EGSYS score, was admitted for cardiac syncope and died of acute heart failure after 7 days of hospitalization.
Late (12 months): the late mortality rate was 5.4% (16/295): 4 (11.8%) patients with cardiac syncope, 4 (12.1%) with non-syncopal T-LOC; 11 (12.9%) previously hospitalized, 2 (3.3%) previously sent to Short-Stay Observation, 3 (3.3%) discharged patients, and none of those previously referred to the SU. The causes of death are reported in Table 2; two of the patients with cardiac syncope died of a cardiovascular event. Causes of death in patients with unexplained syncope were not related to the syncope itself. In a multivariate COX model, adjusted for age, sex, diabetes, hypertension, ischaemic heart disease, depression, and EGSYS score, predictors of death within 12 months were: age [HR (95% CI) = 1.10 (1.03–1.16)], final diagnosis of cardiac syncope [HR (95% CI) = 8.31 (0.91–75.86), P = 0.061), final diagnosis of non-syncopal T-LOC [HR (95% CI) = 19.17 (2.14–171.78)], and diagnosis of unexplained syncope [HR (95% CI) = 11.19 (1.35–92.98)].
Causes of death in 16 patients who died within 1 year after first ED evaluation
| Final diagnosis . | Age . | Period of time between ED admission and death . | Cause of death . |
|---|---|---|---|
| Cardiac | 84 | 6 months | Stroke |
| Cardiac | 93 | 8 months | Ab ingestis pneumonia |
| Cardiac | 72 | 7 days | Ischaemic heart disease |
| Cardiac | 91 | 4 months | Cognitive decay |
| Non-syncopal T-LOC | 79 | 7 months | Pulmonary embolism |
| Non-syncopal T-LOC | 86 | 5 months | Cerebral Ischaemia |
| Non-syncopal T-LOC | 63 | 3 months | Ventricular fibrillation |
| Non-syncopal T-LOC | 87 | 4 months | Malignant gastric tumour |
| Unexplained | 85 | 2 months | Malignant brain tumour |
| Unexplained | 91 | 7 months | Senile dementia |
| Unexplained | 82 | 8 months | Senile dementia |
| Unexplained | 79 | 12 months | Viral meningitis |
| Unexplained | 81 | 3 months | Bronchopneumonia |
| Unexplained | 93 | 9 months | Non-specified heart disease |
| Unexplained | 93 | 7 months | Stroke |
| Neurally mediated | 83 | 5 months | Ischaemic heart disease |
| Final diagnosis . | Age . | Period of time between ED admission and death . | Cause of death . |
|---|---|---|---|
| Cardiac | 84 | 6 months | Stroke |
| Cardiac | 93 | 8 months | Ab ingestis pneumonia |
| Cardiac | 72 | 7 days | Ischaemic heart disease |
| Cardiac | 91 | 4 months | Cognitive decay |
| Non-syncopal T-LOC | 79 | 7 months | Pulmonary embolism |
| Non-syncopal T-LOC | 86 | 5 months | Cerebral Ischaemia |
| Non-syncopal T-LOC | 63 | 3 months | Ventricular fibrillation |
| Non-syncopal T-LOC | 87 | 4 months | Malignant gastric tumour |
| Unexplained | 85 | 2 months | Malignant brain tumour |
| Unexplained | 91 | 7 months | Senile dementia |
| Unexplained | 82 | 8 months | Senile dementia |
| Unexplained | 79 | 12 months | Viral meningitis |
| Unexplained | 81 | 3 months | Bronchopneumonia |
| Unexplained | 93 | 9 months | Non-specified heart disease |
| Unexplained | 93 | 7 months | Stroke |
| Neurally mediated | 83 | 5 months | Ischaemic heart disease |
Causes of death in 16 patients who died within 1 year after first ED evaluation
| Final diagnosis . | Age . | Period of time between ED admission and death . | Cause of death . |
|---|---|---|---|
| Cardiac | 84 | 6 months | Stroke |
| Cardiac | 93 | 8 months | Ab ingestis pneumonia |
| Cardiac | 72 | 7 days | Ischaemic heart disease |
| Cardiac | 91 | 4 months | Cognitive decay |
| Non-syncopal T-LOC | 79 | 7 months | Pulmonary embolism |
| Non-syncopal T-LOC | 86 | 5 months | Cerebral Ischaemia |
| Non-syncopal T-LOC | 63 | 3 months | Ventricular fibrillation |
| Non-syncopal T-LOC | 87 | 4 months | Malignant gastric tumour |
| Unexplained | 85 | 2 months | Malignant brain tumour |
| Unexplained | 91 | 7 months | Senile dementia |
| Unexplained | 82 | 8 months | Senile dementia |
| Unexplained | 79 | 12 months | Viral meningitis |
| Unexplained | 81 | 3 months | Bronchopneumonia |
| Unexplained | 93 | 9 months | Non-specified heart disease |
| Unexplained | 93 | 7 months | Stroke |
| Neurally mediated | 83 | 5 months | Ischaemic heart disease |
| Final diagnosis . | Age . | Period of time between ED admission and death . | Cause of death . |
|---|---|---|---|
| Cardiac | 84 | 6 months | Stroke |
| Cardiac | 93 | 8 months | Ab ingestis pneumonia |
| Cardiac | 72 | 7 days | Ischaemic heart disease |
| Cardiac | 91 | 4 months | Cognitive decay |
| Non-syncopal T-LOC | 79 | 7 months | Pulmonary embolism |
| Non-syncopal T-LOC | 86 | 5 months | Cerebral Ischaemia |
| Non-syncopal T-LOC | 63 | 3 months | Ventricular fibrillation |
| Non-syncopal T-LOC | 87 | 4 months | Malignant gastric tumour |
| Unexplained | 85 | 2 months | Malignant brain tumour |
| Unexplained | 91 | 7 months | Senile dementia |
| Unexplained | 82 | 8 months | Senile dementia |
| Unexplained | 79 | 12 months | Viral meningitis |
| Unexplained | 81 | 3 months | Bronchopneumonia |
| Unexplained | 93 | 9 months | Non-specified heart disease |
| Unexplained | 93 | 7 months | Stroke |
| Neurally mediated | 83 | 5 months | Ischaemic heart disease |
Discussion
The present study showed that the implementation of Short-Stay Observation and fast-track referral to the SU is feasible in a general ED and is effective in reducing unnecessary hospital admissions. To confirm this, we compared our results with those from a systematic review (see Supplementary material online, Appendix 1). In all of the studies reviewed, the rate of hospitalization after ED presentation for syncope was higher9 (on average, 51.0% on using conventional admission practice and 48.2% on using structured pathways) than that in our experience. Before the diffusion of the ESC guidelines on syncope,1 the admission rate was very high: 63% in the study by Blanc et al.10 Application of the American College of Emergency Physicians (ACEP) recommendations reduced hospital admissions to 57.5%.11 On applying the ESC guidelines on syncope,1 admission rates declined to 42–50%.9–20 In the EGSYS 1 study,12 the use of a standardized approach reduced the admission rate to 43%. Implementation of the ESC guidelines and the creation of structured and dedicated pathways yielded a reduction in admissions to 39% in the EGSYS 2 study.2 In the study by Grossman et al.,13 implementation of the Boston Syncope Criteria after in-service training, safely reduced admissions from 69 to 58%. Our centre participated to the EGSYS 2 study;2 at that time the hospitalization rate was 39%. In that period structured syncope pathways in observational unit were absent. Thus, the above figure, which may be used as historical control of our centre, suggests a 26% relative reduction of admissions after the introduction of the observational unit.
The literature supports the importance of Short-Stay Observation within the ED. In the SEEDS4 study, a prospective, randomized, single-centre study, patients were randomly allocated to two evaluation arms: 6-h observation in a SU inside the ED and the usual care. The former strategy significantly improved the diagnostic yield in the ED and reduced admissions (from 98 to 43%) and the total length of hospital stay without increasing mortality. However, this study enrolled only intermediate-risk patients—2.9% of the patients with syncope at the ED—and cannot be compared with population studies such as the present one. In a randomized clinical trial performed in five American EDs, and involving 12–24 h of ED observation vs. routine inpatient admission, Sun et al.3 observed a reduction from 92 to 15% in admissions of patients with intermediate-risk syncope (mean age 65 years), without an increase in mortality. However, this study also enrolled only a minority of intermediate-risk patients and the results are difficult to compare with those of the present study. ‘Implementing short-stay observation reduces hospital admissions and hospital stay, with consequent cost saving for healthcare services. Indeed, Sun et al.3 showed that index hospital costs in the group of patients who underwent an ED observation protocol were lower than in the routine admission group, while safety was undiminished. Moreover, the significant decrease in the length of hospitalization after evaluation in an observation unit provides further evidence of the cost-effectiveness of this strategy for clinical practice (SEEDS4)’.
In our study, the length of stay in Observation Unit was slightly longer than in the above American experiences.3,4 Indeed Italian standards for Observation Unit is 24 h. In the present study, this standard was achieved in 80% of cases while in 20% of cases the patients remained up to 48 h mainly for logistic problems (e.g. admission during week end, lack of available beds in hospital, etc.). However, we did not observe any clinical difference in these patients compared with those discharged within 24 h.
In a single-centre retrospective trial, Daccarett et al.14 found that the introduction of standardized guideline-based algorithms coupled with decision-making software (the new Faint-Algorithm) reduced the number of admissions to the Observation Unit and In-patient Unit from 46 to 22%. However, this new strategy is not currently applied in clinical practice and needs further evaluation.
Both the ESC guidelines on syncope1 and a recent statement from the Canadian Cardiovascular Society20 support the creation of SUs, through the implementation of a shared diagnostic and therapeutic protocol aimed at increasing diagnostic efficacy and accuracy and reducing inappropriate hospitalizations and the average length of stay. The EGSYS 2 studies2–15 specifically aimed to show the benefit of a SU strictly linked to ED evaluation.
Mortality and re-hospitalization
The present study showed that short- and long-term mortality among patients in whom syncope is the main reason for referral is low and generally unrelated to the mechanism of syncope. Most of the patients at risk of death were identified in the ED and admitted; death occurred despite hospitalization.21 It is important to underline that we enrolled only patients with a ‘primary’ diagnosis of syncope, and excluded those in whom syncope was secondary to other clear diagnoses (e.g. myocardial infarction with other clear cardiac symptoms). Finally, we showed that a high rate of re-admission to the ED in the first year is still an issue. Re-admission occurs in all categories of patients, but is more likely in those who have been hospitalized. As shown in Table 1, the majority of the hospitalized patients was high-risk subjects, according to ESC1 and ACEP guidelines.11
The strategy adopted at Careggi Hospital yielded good outcomes, thanks to the application of ESC guidelines, which were implemented through our institution's active involvement in the EGSYS 2 study.2 Trained ED physicians chose the best strategy for patients with suspected syncope, thereby reducing hospitalization without engendering any further risk for patients. The relative safety of the current model emerges from the analysis of the time between ED discharge and evaluation in the SU in accordance with the Fast-Track modality. Although this time-lag (mean of 24 days) may seem long, no unfavourable events occurred during the waiting time and none of the patients died in the following 12 months. Our registry suggests that implementation of the ESC guidelines in clinical practice is feasible, even in a complex setting like the ED of a third-level hospital.
Limitations of the study
Our study did not include a formal control group, thus limiting the value of our results. However, as discussed earlier, we could benefit of historical control data of our hospital which allowed us to estimate a 26% relative reduction of admissions after the introduction of the observational unit.
In addition, there was a variance in observation period vs. American comparative study. As discussed earlier, the reasons of a longer stay in Observation Unit in our hospital is mainly due to a different organization of Italian health system and to logistic issues rather than to clinical reasons.
The results of the present study were obtained in a tertiary hospital that implemented protocols based on international guidelines. For this reason, the results may not be directly applicable to other types of organization.
We did not perform a formal cost analysis. However, it is well known that hospitalization accounts for ∼75% of the total costs of syncope evaluation.1 In the present study, the rate of admissions was lower than that reported in the literature and the duration of Short-Stay Observation (<24 h in 80% and 24–48 h in 20% of patients) was shorter than the >5 days of hospitalization of admitted patients. We can therefore infer that our strategy determined an important cost saving.
Conclusions
In conclusion, the availability of a Short-Stay Observation Unit and a SU seems to reduce the hospitalization rate compared with previous reported historical reports from our and other centres. Most deaths during follow-up occurred in patients who had been hospitalized. High rates of re-admission to the ED within 1 year are still an issue.
Supplementary material
Supplementary material is available at Europace online.
References



