-
PDF
- Split View
-
Views
-
Cite
Cite
Juliano Casonatto, Karla F Goessler, Véronique A Cornelissen, Jefferson R Cardoso, Marcos D Polito, The blood pressure-lowering effect of a single bout of resistance exercise: A systematic review and meta-analysis of randomised controlled trials, European Journal of Preventive Cardiology, Volume 23, Issue 16, 1 November 2016, Pages 1700–1714, https://doi.org/10.1177/2047487316664147
Close - Share Icon Share
Abstract
Current exercise guidelines recommend aerobic types of exercises on most days of the week, supplemented with dynamic resistance exercise twice weekly. Whereas the blood pressure (BP)-lowering effects of a single session of aerobic exercise have been well studied, less is known about the hypotensive effect of a single bout of resistance exercise.
To evaluate the transient effect of resistance exercise on BP by means of meta-analytic techniques.
A systematic electronic search in Medline, Scientific Electronic Library Online (SciELO), Latin American and Caribbean Health Sciences Literature (LILACS), Elton B Stephens Company (EBSCO), EMBASE and SPORTDiscus was completed in March 2015 identifying randomised controlled trials investigating the effect of a single bout of resistance exercise on resting or ambulatory BP in healthy adults. A subsequent meta-analysis was performed.
The meta-analysis involved 30 studies, 81 interventions and 646 participants (normotensive (n = 505) or hypertensive (n = 141)). A single bout of resistance exercise elicited small-to-moderate reductions in office systolic BP at 60 minutes postexercise [−3.3 (−4.0 to −2.6)/−2.7 (−3.2 to −2.1) mmHg (CI 95%)], 90 minutes postexercise [−5.3 (−8.5 to −2.1)/−4.7 (−6.9 to −2.4) mmHg (CI 95%)] and in 24–hour ambulatory BP [−1.7 (−2.8 to −0.67)/−1.2 (−2.4 to −0.022) mmHg (CI 95%)] compared to a control session. The reduction in office BP was more pronounced in hypertensive compared to normotensive individuals (p < 0.01), when using larger muscle groups (p < 0.05) and when participants were recovering in the supine position (p < 0.01).
A single bout of resistance exercise can have a BP-lowering effect that last for up to 24 hours. Supine recovery and the use of larger muscle groups resulted in greater BP reductions after resistance exercise.
Introduction
Post-exercise hypotension (PEH) is defined as a sustained reduction in blood pressure (BP) after a single bout of exercise.1 This transient reduction can last up to 24 hours after completion of an exercise session.2 For that reason, PEH is today considered to be an important physiological phenomenon1 that plays a major role in BP management. However, PEH has been predominantly studied after aerobic endurance types of exercises,3–9 where reductions in BP of between −2 and −12 mmHg have been found.10 These reductions rival the reductions obtained with many first-line antihypertensive medications.11 Hence, current guidelines for hypertension management12 strongly recommend aerobic exercises on most, and preferably all, days of the week, as BP is lower on the days people perform aerobic exercises compared with the days they do not.13 Based on its numerous health-promoting effects, moderate resistance training is today recommended for persons of all ages as an important component of a comprehensive fitness programme.14 Although such exercise used to be contraindicated in hypertensive patients, more than a decade ago, meta-analytic evidence15–18 showed that resistance training performed at low to moderate intensity is also safe for hypertensive individuals and can result in clinically relevant BP reductions following 6–26 weeks of training. Since then, the number of publications addressing the effects of resistance exercise on PEH has increased dramatically. However, to date, there remain substantial shortcomings in our knowledge with regards to the BP-lowering effect of a single session of resistance exercise, which still preclude its recommendation as an equally effective non-pharmacological tool. Namely, most of the published trials employed small sample sizes, were performed in very heterogeneous populations and applied a wide variety of resistance protocols, resulting in inconsistent and inconclusive results.
Contemporary meta-analysis methodologies offer greater precision of point estimates, enhanced statistical power and may contribute to resolving uncertainty and answering questions that were not posed at the start of individual trials.19 Therefore, the main objective of this study was to use the aggregate data and apply a meta-analytic approach in order to determine the effects of a single session of resistance exercise on office and ambulatory BP in healthy adults. The second objective was to examine the effects of exercise and patient characteristics on the BP reduction induced by a single bout of resistance exercise.
Methods
Search strategy and study selection
The online databases Medline, Scientific Electronic Library Online (SciELO), Latin American and Caribbean Health Sciences Literature (LILACS), Elton B Stephens Company (EBSCO), EMBASE and SPORTDiscus were searched from their inception until March 2015 by one author [Juliano Casonatto (JC)] and checked by another author [Marcos D. Polito (MDP)]. Studies published in grey literature were not included. Search terms included a mix of Medical Subject Headings (MeSH) terms and free-text words for key concepts related to resistance exercise and PEH. As an example, the full-search strategy for the PubMed database was: (“post exercise hypotension”[MeSH Terms] OR “blood pressure” [MeSH Terms] OR “post exercise hypotension” OR “blood pressure”) AND (“resistance training”[MeSH Terms] OR “resistance training” OR “resistance exercise” OR “strength exercise” OR “weight exercise”). These were combined with a sensitive search strategy in order to identify “randomised controlled trials” performed in “humans”. No language restrictions were applied during the search.
The inclusion criteria were as follows: (1) randomised controlled studies; (2) investigating the effect of a single bout of resistance exercise on BP; (3) in healthy human adults (age ≥ 18 years); (4) reporting BP pre- and post-exercise for both the exercise and control session/group; (5) BP was measured at 60 or 90 minutes in the office or over 24 hours by means of ambulatory BP monitoring; and (6) results were published in a peer-reviewed journal up to March 2015. All studies not meeting the criteria above or duplicate publications were excluded. The authors of two studies20,21 were contacted and requested to provide missing data.
The study selection process is summarised in Figure 1. In brief, 218 potentially relevant studies were retrieved and screened by reviewing the titles and abstracts. Thirty studies that were eligible for inclusion were then subjected to data extraction.
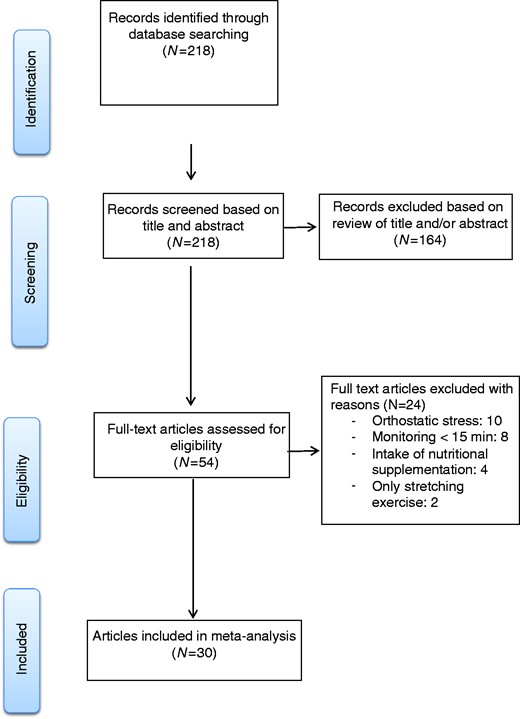
Flowchart for the inclusion of randomised controlled trials of post-exercise hypotension following resistance exercise.
Data extraction and quality assessment
The extracted study and subject data included but were not limited to variables related to publication details (first author, year and country of origin), study design, participant characteristics (BP category, training status, gender, age and number of participants in the trial), exercise characteristics (type, volume, intensity, number of exercises, used muscle mass and rest interval between sets), BP measurement (device, position and follow-up time), study quality and outcome measures (mean, SD and standard error of the mean). A standardised coding form was used and information was archived in a database.
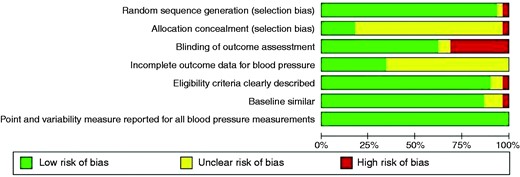
Two reviewers [JC and Karla F. Goessler (KFG)] independently assessed the risk of bias for included studies using the Cochrane Collaboration ‘risk of bias’ tool.22 For each study, the following items were evaluated: (1) random sequence generation; (2) allocation concealment; (3) blinding of outcome assessment (a low risk score was given to studies using automated devices in order to measure the BP, while studies valuating the BP by means of a finometer or by auscultatory techniques were scored as high risk); (4) incomplete outcome data (if authors showed at least 80% of the measures for BP, it was scored as low risk); (5) eligibility criteria; (6) baseline similar; and (7) point and variability measures reported for all BP measurements. Disagreements were resolved by discussion. Studies were not excluded based on their quality.
Statistical analysis
Analyses were performed using the Comprehensive Meta-Analysis software (CMA, version 2.2.064, Biostat, NJ, USA). Two-sided statistical significance was set at p < 0.05. The primary outcome measures were changes in systolic and diastolic BP. Descriptive data were reported as mean ± SD or median and range. Study data were pooled using a random effects model. Comparisons for trials with more than one intervention were disaggregated. Effect sizes were calculated for each comparison and analysed as separate studies. Inconsistencies were estimated using the I2 statistic.
Additionally, we tested nine a priori-defined hypotheses that there might be differences in the effects of resistance exercise on office PEH with regards to: (1) intensity (<50% one-repetition maximum [1RM] (low); 50–69% 1RM (moderate); >69% 1RM or repetitions until fatigue (high)); (2) workout volume (# exercises × # sets × # reps: <150 (low), 150–299 (moderate) and > 299 (high)); (3) type of training (circuit and traditional); (4) gender (male, female and both); (5) BP device (auscultatory, oscillometric and photoplethysmography); (6) training status (trained (regular training) and sedentary (no regular training)); (7) muscle mass involved (large, small and both); (8) recovery posture (supine vs. seated); and (9) clinical status (normotensive vs. hypertensive). Differences between subgroups were analysed by means of analysis of variance (Q-test-based ANOVA). A meta-regression analysis was applied in order to evaluate the effect of age on BP changes.
Funnel plot asymmetry in order to identify publication bias was evaluated by visual inspection of the funnel plots. In addition, Duval and Tweedie’s trim and fill computation was used in order to estimate the effect of publication bias on the results.23
Results
Study characteristics
As shown in Figure 1, 30 randomised controlled studies were identified that fulfilled the inclusion criteria,2,5,20,21,24–49 involving 646 individuals and 81 trials (64 normotensive and 17 hypertensive individuals as predefined by the original authors). Subject and intervention characteristics are shown in Table 1. The studies were conducted between 1999 and 2015. Except for two studies,40,41 all trials used a cross-over design. Sample sizes ranged between 6 and 84 subjects. Participants ranged in age from 18 to 80 years. Eighteen studies involved only men, eight studies included only women and ten studies included both men and women. Sixty-eight exercise sessions involved conventional resistance training and 13 sessions involved a circuit model. BP post-exercise was measured in the seated (n = 57 trials) or supine position (n = 5 trials). Nineteen trials did not provide any data on the position in which BP measurements were performed.
| Study . | Subjects characteristics . | No. of exercise interventions/study design . | Exercise characteristics . | BP measurement . | Post-exercise BP effect . |
|---|---|---|---|---|---|
| Anunciação et al.24 | 10 normotensive trained men (23 ± 2 years of age) | 4/cross-over | 8 exercises; 1 or 3 sets (circuit and traditional); 18 reps; 40% 1RM; 1–2 minutes (standard) and 3–5 minutes (circuit) of rest interval | Oscillometric automatic (60 minutes) | ↓SBP, DBP and MBP to mean of 60 minutes (3 sets sessions) |
| Arazi et al.25 | 11 normotensive sedentary men (19 ± 1 years of age) | 2/cross-over | 6 exercises (circuit); 1 set; 10RM 30 and 40 seconds of rest interval | Auscultatory (80 minutes) | ↓SBP to 40, 50, 60, 70 and 80 minutes |
| Bermudes et al.26 | 25 normotensive sedentary men (44 ± 1 years of age) | 1/cross-over | 10 exercises (circuit); 3 sets; 20–35 reps; 40% 1RM; 30 seconds (exercise) and 2 minutes (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | ↓DBP during sleep |
| Brito et al.27 | 10 hypertensive sedentary women (61 ± 2 years of age) | 2/cross-over | 10 exercises; 1 set; 10 reps; 50 and 80% 1RM; 90 seconds (exercise) and 90 seconds (sets) of rest interval | Photoplethysmography (90 minutes) | ↓SBP and DBP to 10, 30, 50, 70 and 90 minutes |
| Costa et al.28 | 6 hypertensive trained men (66 ± 5 years of age); 9 hypertensive sedentary women (66 ± 4 years of age) | 2/cross over | 7 exercises; 2 sets; 10–15 reps; 10–15RM; 120 seconds (exercise) and 60 seconds (sets) of rest interval | Auscultatory (60 minutes) | ↓SBP to 30 minutes (normotensive); ↓SBP throughout period; ↓DBP to 30 minutes (hypertensive) |
| DeVan et al.29 | 16 normotensive men and women (sedentary or recreationally active) (27 ± 1 years of age) | 2/cross-over | 9 exercises; 1 set; maximum reps; 75% 1RM | Oscillometric automatic (150 minutes) | ↓DBP to 30 minutes |
| Focht and Koltyn30 | 84 normotensive trained men and women (adults) | 2/cross-over | 4 exercises; 3 sets; 4–8/12–20 reps; 80% 1RM (4–8 reps) and 50% 1RM (12–20 reps) | Oscillometric automatic (180 minutes) | NS |
| Hardy and Tucker31 | 24 hypertensive sedentary men (50 ± 10 years of age) | 2/cross-over | 7 exercises; 3 sets; 8–12RM; 1 minute of rest interval | Oscillometric automatic ABPM (23 h) | ↓SBP to 60 minutes |
| Keese et al.5 | 21 normotensive trained men (20 ± 1 years of age) | 2/cross-over | 8 exercises; 3 sets; 6–8 reps; 80% 1RM; 2 minutes of rest interval | Oscillometric automatic ABPM (120 minutes) | ↓SBP up to 80 minutes |
| Melo et al.32 | 11 hypertensive sedentary women (46 ± 1 years of age) | 1/cross-over | 6 exercises; 3 sets; 20 reps; 40% 1RM; 90 seconds (exercise) and 45 seconds (sets) of rest interval | Auscultatory (2 hours); oscillometric automatic ABPM (21 hours) | ↓SBP to 90 minutes; ↓DBP to 45, 60 and 75 minutes (auscultatory); ↓SBP and DBP for 10 hours (ABPM) |
| Moraes et al.2 | 8 normotensive sedentary men (38 ± 4 years of age); 10 hypertensive sedentary men (44 ± 2 years of age) | 2/cross-over | 7 exercises (circuit); 3 sets; 12 reps; 50% 1RM; 30 seconds (exercise) and 2 minutes (circuits) of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓SBP to 30–60 minutes and mean of 24 hours (normotensive); ↓SBP to 45 and 60 minutes; ↓DBP to 60 minutes (hypertensive) |
| Moreira et al.33 | 20 normotensive sedentary men and women (33 ± 7 years of age) | 1/cross-over | 7 exercises (circuit); 3 sets; 15 reps; 50% 1RM; 2 minutes of rest interval | Auscultatory (60 minutes) | ↓SBP, ↓DBP and ↓MBP up to 60 minutes |
| Mota et al.35 | 15 hypertensive sedentary men and women (43 ± 2 years of age) | 1/cross-over | 13 exercises (circuit); 1 set; 20 reps; 40% 1RM; 30 seconds of rest interval | Oscillometric automatic (60 minutes); oscillometric automatic ABPM (7 hours) | ↓SBP and MBP 15–60 minutes; ↓DBP to 30 minutes |
| Mota et al.34 | 32 hypertensive sedentary women (67 ± 7 years of age) | 4/cross-over | 10 exercises; 3 sets; 8–12 reps; 60–80% 1RM; 60–90 seconds of rest interval | Oscillometric automatic (60 minutes) | ↓SBP and DBP |
| Neto et al.36 | 24 normotensive trained men (22 ± 3 years of age) | 2/cross-over | 4 exercises; 1 and 4 sets; 8 and 30 reps; 80% 1RM (traditional) and 20% 1RM (blood flow restriction); 30 seconds (sets) and 60 seconds (exercises) of rest interval | Oscillometric automatic (60 minutes) | ↓SBP and DBP to 20, 30, 40, 50 and 60 minutes |
| Niemela et al.37 | 12 normotensive trained men (31 ± 3 years of age) | 4/cross-over | 4 exercises; 3 sets; 12 and 20 reps; 80% 1RM (12 reps) and 30% 1RM (20 reps) | Photoplethysmography (180 minutes) | NS |
| O’Connor et al.38 | 14 normotensive trained women (23 ± 4 years of age) | 6/cross-over | 6 exercises; 3 sets; 10 reps; 40%, 60% and 80% 10RM | Oscillometric automatic ABPM (120 minutes) | ↑SBP to 15 minutes (80% 10RM) |
| Olher et al.39 | 12 hypertensive sedentary women (64 ± 1 years of age) | 2/cross-over | 1 exercise; 4 sets; 5 reps; 30% and 60% MVC | Oscillometric automatic (60 minutes) | NS |
| Polito and Farinatti40 | Normotensive trained men: control group (n = 8; 24 ± 1 years of age), arm exercise group (n = 8; 22 ± 1 years of age), leg exercise group (n = 8; 22 ± 1 years of age) | 4/randomised controlled with parallel group | 1 exercise; 6 and 10 sets; 10 reps; 70–80% 1RM; 120 seconds of rest interval | Oscillometric semi-automatic (60 minutes) | ↓SBP throughout period |
| Polito et al.41 | Normotensive sedentary men: exercise group (n = 9; 28 ± 6 years of age), control group (n = 7; 32 ± 3 years of age) | 1/randomised controlled with parallel group | 1 exercise; 10 sets; 15 reps; 90% 15RM; 120 seconds of rest interval | Oscillometric semi-automatic (60 minutes) | ↓SBP to 10 minutes |
| Prista et al.42 | 24 normotensive sedentary men (41 ± 1 years of age) | 4/cross-over | 8 exercises; 1 set; 8–12 reps; 50–60% 1RM and 30–40% 1RM; 60 seconds of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓DBP to 30, 45 and 60 minutes; ↓SBP and DBP to 6–14 hours |
| Queiroz et al.20 | 15 normotensive sedentary men and women (25 ± 1 years of age) | 4/cross-over | 6 exercises; 3 sets; 50% 1RM; 45 seconds (sets) and 90 seconds (exercises) of rest interval | Auscultatory (60 minutes) | ↓SBP and DBP to 30, 45 and 60 minutes |
| Queiroz et al.44 | 16 normotensive trained: men (n = 5)/women (n = 11) (63 ± 1 years of age) | 3/cross-over | 9 exercises; 3 sets; 8 maximum repetitions; 180 seconds (exercises) and 120 seconds (sets) of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓SBP to 60 minutes |
| Queiroz et al.43 | 44 normotensive sedentary: men (n = 22; 25 ± 1 years of age); women (n = 22; 25 ± 1 years of age) | 2/cross-over | 6 exercises; 3 sets; 20 repetitions; 40–50% 1RM; 90 seconds (exercises) and 45 seconds (sets) of rest interval | Auscultatory (60 minutes) | ↓SBP and DBP |
| Queiroz et al.45 | Sedentary men: 14 normotensive (44 ± 3 years of age) and 12 hypertensive (50 ± 3 years of age) | 2/cross-over | 7 exercises; 3 sets; 50% 1RM; 90 seconds (exercises) and 45 seconds (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | ↓SBP and DBP |
| Rezk et al.21 | 17 normotensive sedentary men and women (23 ± 1 years of age) | 4/cross-over | 6 exercises; 3 sets; 10–20 reps; 40% and 80% 1RM; 90 seconds (exercise) and 45 seconds (sets) | Auscultatory (90 minutes) | ↓SBP on both intensities over the whole period; ↓DBP to 15 and 30 minutes to 40% 1RM |
| Roltsch et al.46 | Normotensive men and women: resistance trained (n = 12; 23 ± 2 years of age), endurance trained (n = 10; 24 ± 3 years of age), sedentary (n = 11; 20 ± 2 years of age) | 3/cross-over | 12 exercises; 2 sets; 8–12RM; 60 seconds (exercise) and 60 seconds (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | NS |
| Simoes et al.47 | Normotensive trained men: 10 healthy (52 ± 13 years of age); 10 type II diabetes (47 ± 13 years of age) | 4/cross-over | 6 exercises (circuit); 3 sets; 16 and 30 reps; 23% 1RM (30 reps) and 43% 1RM (16 reps); 20 seconds (exercise) and 120 seconds (sets) of rest interval | Oscillometric automatic (120 minutes) | ↓SBP to 30, 75, 90 and 120 minutes for 43% 1RM (healthy); ↓SBP to 30, 45 and 90 minutes (type II diabetes) |
| Teixeira et al.48 | 20 normotensive sedentary men and women (26 ± 1 years of age) | 2/cross-over | 6 exercises; 3 sets; 20 reps; 50% 1RM; 45 seconds (exercise) and 90 seconds (sets) of rest interval | Auscultatory (120 minutes) | ↓SBP and DBP |
| Veloso et al.49 | 16 normotensive sedentary men (23 ± 3 years of age) | 6/cross-over | 6 exercises; 3 sets; 8 reps; 50–80% 1RM; 2 minutes (exercise) and 1–3 minutes (sets) of rest interval | Oscillometric automatic (90 minutes) | ↓DBP to 15, 30 and 90 minutes |
| Study . | Subjects characteristics . | No. of exercise interventions/study design . | Exercise characteristics . | BP measurement . | Post-exercise BP effect . |
|---|---|---|---|---|---|
| Anunciação et al.24 | 10 normotensive trained men (23 ± 2 years of age) | 4/cross-over | 8 exercises; 1 or 3 sets (circuit and traditional); 18 reps; 40% 1RM; 1–2 minutes (standard) and 3–5 minutes (circuit) of rest interval | Oscillometric automatic (60 minutes) | ↓SBP, DBP and MBP to mean of 60 minutes (3 sets sessions) |
| Arazi et al.25 | 11 normotensive sedentary men (19 ± 1 years of age) | 2/cross-over | 6 exercises (circuit); 1 set; 10RM 30 and 40 seconds of rest interval | Auscultatory (80 minutes) | ↓SBP to 40, 50, 60, 70 and 80 minutes |
| Bermudes et al.26 | 25 normotensive sedentary men (44 ± 1 years of age) | 1/cross-over | 10 exercises (circuit); 3 sets; 20–35 reps; 40% 1RM; 30 seconds (exercise) and 2 minutes (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | ↓DBP during sleep |
| Brito et al.27 | 10 hypertensive sedentary women (61 ± 2 years of age) | 2/cross-over | 10 exercises; 1 set; 10 reps; 50 and 80% 1RM; 90 seconds (exercise) and 90 seconds (sets) of rest interval | Photoplethysmography (90 minutes) | ↓SBP and DBP to 10, 30, 50, 70 and 90 minutes |
| Costa et al.28 | 6 hypertensive trained men (66 ± 5 years of age); 9 hypertensive sedentary women (66 ± 4 years of age) | 2/cross over | 7 exercises; 2 sets; 10–15 reps; 10–15RM; 120 seconds (exercise) and 60 seconds (sets) of rest interval | Auscultatory (60 minutes) | ↓SBP to 30 minutes (normotensive); ↓SBP throughout period; ↓DBP to 30 minutes (hypertensive) |
| DeVan et al.29 | 16 normotensive men and women (sedentary or recreationally active) (27 ± 1 years of age) | 2/cross-over | 9 exercises; 1 set; maximum reps; 75% 1RM | Oscillometric automatic (150 minutes) | ↓DBP to 30 minutes |
| Focht and Koltyn30 | 84 normotensive trained men and women (adults) | 2/cross-over | 4 exercises; 3 sets; 4–8/12–20 reps; 80% 1RM (4–8 reps) and 50% 1RM (12–20 reps) | Oscillometric automatic (180 minutes) | NS |
| Hardy and Tucker31 | 24 hypertensive sedentary men (50 ± 10 years of age) | 2/cross-over | 7 exercises; 3 sets; 8–12RM; 1 minute of rest interval | Oscillometric automatic ABPM (23 h) | ↓SBP to 60 minutes |
| Keese et al.5 | 21 normotensive trained men (20 ± 1 years of age) | 2/cross-over | 8 exercises; 3 sets; 6–8 reps; 80% 1RM; 2 minutes of rest interval | Oscillometric automatic ABPM (120 minutes) | ↓SBP up to 80 minutes |
| Melo et al.32 | 11 hypertensive sedentary women (46 ± 1 years of age) | 1/cross-over | 6 exercises; 3 sets; 20 reps; 40% 1RM; 90 seconds (exercise) and 45 seconds (sets) of rest interval | Auscultatory (2 hours); oscillometric automatic ABPM (21 hours) | ↓SBP to 90 minutes; ↓DBP to 45, 60 and 75 minutes (auscultatory); ↓SBP and DBP for 10 hours (ABPM) |
| Moraes et al.2 | 8 normotensive sedentary men (38 ± 4 years of age); 10 hypertensive sedentary men (44 ± 2 years of age) | 2/cross-over | 7 exercises (circuit); 3 sets; 12 reps; 50% 1RM; 30 seconds (exercise) and 2 minutes (circuits) of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓SBP to 30–60 minutes and mean of 24 hours (normotensive); ↓SBP to 45 and 60 minutes; ↓DBP to 60 minutes (hypertensive) |
| Moreira et al.33 | 20 normotensive sedentary men and women (33 ± 7 years of age) | 1/cross-over | 7 exercises (circuit); 3 sets; 15 reps; 50% 1RM; 2 minutes of rest interval | Auscultatory (60 minutes) | ↓SBP, ↓DBP and ↓MBP up to 60 minutes |
| Mota et al.35 | 15 hypertensive sedentary men and women (43 ± 2 years of age) | 1/cross-over | 13 exercises (circuit); 1 set; 20 reps; 40% 1RM; 30 seconds of rest interval | Oscillometric automatic (60 minutes); oscillometric automatic ABPM (7 hours) | ↓SBP and MBP 15–60 minutes; ↓DBP to 30 minutes |
| Mota et al.34 | 32 hypertensive sedentary women (67 ± 7 years of age) | 4/cross-over | 10 exercises; 3 sets; 8–12 reps; 60–80% 1RM; 60–90 seconds of rest interval | Oscillometric automatic (60 minutes) | ↓SBP and DBP |
| Neto et al.36 | 24 normotensive trained men (22 ± 3 years of age) | 2/cross-over | 4 exercises; 1 and 4 sets; 8 and 30 reps; 80% 1RM (traditional) and 20% 1RM (blood flow restriction); 30 seconds (sets) and 60 seconds (exercises) of rest interval | Oscillometric automatic (60 minutes) | ↓SBP and DBP to 20, 30, 40, 50 and 60 minutes |
| Niemela et al.37 | 12 normotensive trained men (31 ± 3 years of age) | 4/cross-over | 4 exercises; 3 sets; 12 and 20 reps; 80% 1RM (12 reps) and 30% 1RM (20 reps) | Photoplethysmography (180 minutes) | NS |
| O’Connor et al.38 | 14 normotensive trained women (23 ± 4 years of age) | 6/cross-over | 6 exercises; 3 sets; 10 reps; 40%, 60% and 80% 10RM | Oscillometric automatic ABPM (120 minutes) | ↑SBP to 15 minutes (80% 10RM) |
| Olher et al.39 | 12 hypertensive sedentary women (64 ± 1 years of age) | 2/cross-over | 1 exercise; 4 sets; 5 reps; 30% and 60% MVC | Oscillometric automatic (60 minutes) | NS |
| Polito and Farinatti40 | Normotensive trained men: control group (n = 8; 24 ± 1 years of age), arm exercise group (n = 8; 22 ± 1 years of age), leg exercise group (n = 8; 22 ± 1 years of age) | 4/randomised controlled with parallel group | 1 exercise; 6 and 10 sets; 10 reps; 70–80% 1RM; 120 seconds of rest interval | Oscillometric semi-automatic (60 minutes) | ↓SBP throughout period |
| Polito et al.41 | Normotensive sedentary men: exercise group (n = 9; 28 ± 6 years of age), control group (n = 7; 32 ± 3 years of age) | 1/randomised controlled with parallel group | 1 exercise; 10 sets; 15 reps; 90% 15RM; 120 seconds of rest interval | Oscillometric semi-automatic (60 minutes) | ↓SBP to 10 minutes |
| Prista et al.42 | 24 normotensive sedentary men (41 ± 1 years of age) | 4/cross-over | 8 exercises; 1 set; 8–12 reps; 50–60% 1RM and 30–40% 1RM; 60 seconds of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓DBP to 30, 45 and 60 minutes; ↓SBP and DBP to 6–14 hours |
| Queiroz et al.20 | 15 normotensive sedentary men and women (25 ± 1 years of age) | 4/cross-over | 6 exercises; 3 sets; 50% 1RM; 45 seconds (sets) and 90 seconds (exercises) of rest interval | Auscultatory (60 minutes) | ↓SBP and DBP to 30, 45 and 60 minutes |
| Queiroz et al.44 | 16 normotensive trained: men (n = 5)/women (n = 11) (63 ± 1 years of age) | 3/cross-over | 9 exercises; 3 sets; 8 maximum repetitions; 180 seconds (exercises) and 120 seconds (sets) of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓SBP to 60 minutes |
| Queiroz et al.43 | 44 normotensive sedentary: men (n = 22; 25 ± 1 years of age); women (n = 22; 25 ± 1 years of age) | 2/cross-over | 6 exercises; 3 sets; 20 repetitions; 40–50% 1RM; 90 seconds (exercises) and 45 seconds (sets) of rest interval | Auscultatory (60 minutes) | ↓SBP and DBP |
| Queiroz et al.45 | Sedentary men: 14 normotensive (44 ± 3 years of age) and 12 hypertensive (50 ± 3 years of age) | 2/cross-over | 7 exercises; 3 sets; 50% 1RM; 90 seconds (exercises) and 45 seconds (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | ↓SBP and DBP |
| Rezk et al.21 | 17 normotensive sedentary men and women (23 ± 1 years of age) | 4/cross-over | 6 exercises; 3 sets; 10–20 reps; 40% and 80% 1RM; 90 seconds (exercise) and 45 seconds (sets) | Auscultatory (90 minutes) | ↓SBP on both intensities over the whole period; ↓DBP to 15 and 30 minutes to 40% 1RM |
| Roltsch et al.46 | Normotensive men and women: resistance trained (n = 12; 23 ± 2 years of age), endurance trained (n = 10; 24 ± 3 years of age), sedentary (n = 11; 20 ± 2 years of age) | 3/cross-over | 12 exercises; 2 sets; 8–12RM; 60 seconds (exercise) and 60 seconds (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | NS |
| Simoes et al.47 | Normotensive trained men: 10 healthy (52 ± 13 years of age); 10 type II diabetes (47 ± 13 years of age) | 4/cross-over | 6 exercises (circuit); 3 sets; 16 and 30 reps; 23% 1RM (30 reps) and 43% 1RM (16 reps); 20 seconds (exercise) and 120 seconds (sets) of rest interval | Oscillometric automatic (120 minutes) | ↓SBP to 30, 75, 90 and 120 minutes for 43% 1RM (healthy); ↓SBP to 30, 45 and 90 minutes (type II diabetes) |
| Teixeira et al.48 | 20 normotensive sedentary men and women (26 ± 1 years of age) | 2/cross-over | 6 exercises; 3 sets; 20 reps; 50% 1RM; 45 seconds (exercise) and 90 seconds (sets) of rest interval | Auscultatory (120 minutes) | ↓SBP and DBP |
| Veloso et al.49 | 16 normotensive sedentary men (23 ± 3 years of age) | 6/cross-over | 6 exercises; 3 sets; 8 reps; 50–80% 1RM; 2 minutes (exercise) and 1–3 minutes (sets) of rest interval | Oscillometric automatic (90 minutes) | ↓DBP to 15, 30 and 90 minutes |
BP: blood pressure; SBP: systolic blood pressure; DBP: diastolic blood pressure; MBP: mean blood pressure; ABPM: ambulatory blood pressure monitoring; MVC: maximum voluntary contraction; ANP: atrial natriuretic peptide; RPE: rating of perceived exertion; 1RM: One-repetition maximum.
| Study . | Subjects characteristics . | No. of exercise interventions/study design . | Exercise characteristics . | BP measurement . | Post-exercise BP effect . |
|---|---|---|---|---|---|
| Anunciação et al.24 | 10 normotensive trained men (23 ± 2 years of age) | 4/cross-over | 8 exercises; 1 or 3 sets (circuit and traditional); 18 reps; 40% 1RM; 1–2 minutes (standard) and 3–5 minutes (circuit) of rest interval | Oscillometric automatic (60 minutes) | ↓SBP, DBP and MBP to mean of 60 minutes (3 sets sessions) |
| Arazi et al.25 | 11 normotensive sedentary men (19 ± 1 years of age) | 2/cross-over | 6 exercises (circuit); 1 set; 10RM 30 and 40 seconds of rest interval | Auscultatory (80 minutes) | ↓SBP to 40, 50, 60, 70 and 80 minutes |
| Bermudes et al.26 | 25 normotensive sedentary men (44 ± 1 years of age) | 1/cross-over | 10 exercises (circuit); 3 sets; 20–35 reps; 40% 1RM; 30 seconds (exercise) and 2 minutes (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | ↓DBP during sleep |
| Brito et al.27 | 10 hypertensive sedentary women (61 ± 2 years of age) | 2/cross-over | 10 exercises; 1 set; 10 reps; 50 and 80% 1RM; 90 seconds (exercise) and 90 seconds (sets) of rest interval | Photoplethysmography (90 minutes) | ↓SBP and DBP to 10, 30, 50, 70 and 90 minutes |
| Costa et al.28 | 6 hypertensive trained men (66 ± 5 years of age); 9 hypertensive sedentary women (66 ± 4 years of age) | 2/cross over | 7 exercises; 2 sets; 10–15 reps; 10–15RM; 120 seconds (exercise) and 60 seconds (sets) of rest interval | Auscultatory (60 minutes) | ↓SBP to 30 minutes (normotensive); ↓SBP throughout period; ↓DBP to 30 minutes (hypertensive) |
| DeVan et al.29 | 16 normotensive men and women (sedentary or recreationally active) (27 ± 1 years of age) | 2/cross-over | 9 exercises; 1 set; maximum reps; 75% 1RM | Oscillometric automatic (150 minutes) | ↓DBP to 30 minutes |
| Focht and Koltyn30 | 84 normotensive trained men and women (adults) | 2/cross-over | 4 exercises; 3 sets; 4–8/12–20 reps; 80% 1RM (4–8 reps) and 50% 1RM (12–20 reps) | Oscillometric automatic (180 minutes) | NS |
| Hardy and Tucker31 | 24 hypertensive sedentary men (50 ± 10 years of age) | 2/cross-over | 7 exercises; 3 sets; 8–12RM; 1 minute of rest interval | Oscillometric automatic ABPM (23 h) | ↓SBP to 60 minutes |
| Keese et al.5 | 21 normotensive trained men (20 ± 1 years of age) | 2/cross-over | 8 exercises; 3 sets; 6–8 reps; 80% 1RM; 2 minutes of rest interval | Oscillometric automatic ABPM (120 minutes) | ↓SBP up to 80 minutes |
| Melo et al.32 | 11 hypertensive sedentary women (46 ± 1 years of age) | 1/cross-over | 6 exercises; 3 sets; 20 reps; 40% 1RM; 90 seconds (exercise) and 45 seconds (sets) of rest interval | Auscultatory (2 hours); oscillometric automatic ABPM (21 hours) | ↓SBP to 90 minutes; ↓DBP to 45, 60 and 75 minutes (auscultatory); ↓SBP and DBP for 10 hours (ABPM) |
| Moraes et al.2 | 8 normotensive sedentary men (38 ± 4 years of age); 10 hypertensive sedentary men (44 ± 2 years of age) | 2/cross-over | 7 exercises (circuit); 3 sets; 12 reps; 50% 1RM; 30 seconds (exercise) and 2 minutes (circuits) of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓SBP to 30–60 minutes and mean of 24 hours (normotensive); ↓SBP to 45 and 60 minutes; ↓DBP to 60 minutes (hypertensive) |
| Moreira et al.33 | 20 normotensive sedentary men and women (33 ± 7 years of age) | 1/cross-over | 7 exercises (circuit); 3 sets; 15 reps; 50% 1RM; 2 minutes of rest interval | Auscultatory (60 minutes) | ↓SBP, ↓DBP and ↓MBP up to 60 minutes |
| Mota et al.35 | 15 hypertensive sedentary men and women (43 ± 2 years of age) | 1/cross-over | 13 exercises (circuit); 1 set; 20 reps; 40% 1RM; 30 seconds of rest interval | Oscillometric automatic (60 minutes); oscillometric automatic ABPM (7 hours) | ↓SBP and MBP 15–60 minutes; ↓DBP to 30 minutes |
| Mota et al.34 | 32 hypertensive sedentary women (67 ± 7 years of age) | 4/cross-over | 10 exercises; 3 sets; 8–12 reps; 60–80% 1RM; 60–90 seconds of rest interval | Oscillometric automatic (60 minutes) | ↓SBP and DBP |
| Neto et al.36 | 24 normotensive trained men (22 ± 3 years of age) | 2/cross-over | 4 exercises; 1 and 4 sets; 8 and 30 reps; 80% 1RM (traditional) and 20% 1RM (blood flow restriction); 30 seconds (sets) and 60 seconds (exercises) of rest interval | Oscillometric automatic (60 minutes) | ↓SBP and DBP to 20, 30, 40, 50 and 60 minutes |
| Niemela et al.37 | 12 normotensive trained men (31 ± 3 years of age) | 4/cross-over | 4 exercises; 3 sets; 12 and 20 reps; 80% 1RM (12 reps) and 30% 1RM (20 reps) | Photoplethysmography (180 minutes) | NS |
| O’Connor et al.38 | 14 normotensive trained women (23 ± 4 years of age) | 6/cross-over | 6 exercises; 3 sets; 10 reps; 40%, 60% and 80% 10RM | Oscillometric automatic ABPM (120 minutes) | ↑SBP to 15 minutes (80% 10RM) |
| Olher et al.39 | 12 hypertensive sedentary women (64 ± 1 years of age) | 2/cross-over | 1 exercise; 4 sets; 5 reps; 30% and 60% MVC | Oscillometric automatic (60 minutes) | NS |
| Polito and Farinatti40 | Normotensive trained men: control group (n = 8; 24 ± 1 years of age), arm exercise group (n = 8; 22 ± 1 years of age), leg exercise group (n = 8; 22 ± 1 years of age) | 4/randomised controlled with parallel group | 1 exercise; 6 and 10 sets; 10 reps; 70–80% 1RM; 120 seconds of rest interval | Oscillometric semi-automatic (60 minutes) | ↓SBP throughout period |
| Polito et al.41 | Normotensive sedentary men: exercise group (n = 9; 28 ± 6 years of age), control group (n = 7; 32 ± 3 years of age) | 1/randomised controlled with parallel group | 1 exercise; 10 sets; 15 reps; 90% 15RM; 120 seconds of rest interval | Oscillometric semi-automatic (60 minutes) | ↓SBP to 10 minutes |
| Prista et al.42 | 24 normotensive sedentary men (41 ± 1 years of age) | 4/cross-over | 8 exercises; 1 set; 8–12 reps; 50–60% 1RM and 30–40% 1RM; 60 seconds of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓DBP to 30, 45 and 60 minutes; ↓SBP and DBP to 6–14 hours |
| Queiroz et al.20 | 15 normotensive sedentary men and women (25 ± 1 years of age) | 4/cross-over | 6 exercises; 3 sets; 50% 1RM; 45 seconds (sets) and 90 seconds (exercises) of rest interval | Auscultatory (60 minutes) | ↓SBP and DBP to 30, 45 and 60 minutes |
| Queiroz et al.44 | 16 normotensive trained: men (n = 5)/women (n = 11) (63 ± 1 years of age) | 3/cross-over | 9 exercises; 3 sets; 8 maximum repetitions; 180 seconds (exercises) and 120 seconds (sets) of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓SBP to 60 minutes |
| Queiroz et al.43 | 44 normotensive sedentary: men (n = 22; 25 ± 1 years of age); women (n = 22; 25 ± 1 years of age) | 2/cross-over | 6 exercises; 3 sets; 20 repetitions; 40–50% 1RM; 90 seconds (exercises) and 45 seconds (sets) of rest interval | Auscultatory (60 minutes) | ↓SBP and DBP |
| Queiroz et al.45 | Sedentary men: 14 normotensive (44 ± 3 years of age) and 12 hypertensive (50 ± 3 years of age) | 2/cross-over | 7 exercises; 3 sets; 50% 1RM; 90 seconds (exercises) and 45 seconds (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | ↓SBP and DBP |
| Rezk et al.21 | 17 normotensive sedentary men and women (23 ± 1 years of age) | 4/cross-over | 6 exercises; 3 sets; 10–20 reps; 40% and 80% 1RM; 90 seconds (exercise) and 45 seconds (sets) | Auscultatory (90 minutes) | ↓SBP on both intensities over the whole period; ↓DBP to 15 and 30 minutes to 40% 1RM |
| Roltsch et al.46 | Normotensive men and women: resistance trained (n = 12; 23 ± 2 years of age), endurance trained (n = 10; 24 ± 3 years of age), sedentary (n = 11; 20 ± 2 years of age) | 3/cross-over | 12 exercises; 2 sets; 8–12RM; 60 seconds (exercise) and 60 seconds (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | NS |
| Simoes et al.47 | Normotensive trained men: 10 healthy (52 ± 13 years of age); 10 type II diabetes (47 ± 13 years of age) | 4/cross-over | 6 exercises (circuit); 3 sets; 16 and 30 reps; 23% 1RM (30 reps) and 43% 1RM (16 reps); 20 seconds (exercise) and 120 seconds (sets) of rest interval | Oscillometric automatic (120 minutes) | ↓SBP to 30, 75, 90 and 120 minutes for 43% 1RM (healthy); ↓SBP to 30, 45 and 90 minutes (type II diabetes) |
| Teixeira et al.48 | 20 normotensive sedentary men and women (26 ± 1 years of age) | 2/cross-over | 6 exercises; 3 sets; 20 reps; 50% 1RM; 45 seconds (exercise) and 90 seconds (sets) of rest interval | Auscultatory (120 minutes) | ↓SBP and DBP |
| Veloso et al.49 | 16 normotensive sedentary men (23 ± 3 years of age) | 6/cross-over | 6 exercises; 3 sets; 8 reps; 50–80% 1RM; 2 minutes (exercise) and 1–3 minutes (sets) of rest interval | Oscillometric automatic (90 minutes) | ↓DBP to 15, 30 and 90 minutes |
| Study . | Subjects characteristics . | No. of exercise interventions/study design . | Exercise characteristics . | BP measurement . | Post-exercise BP effect . |
|---|---|---|---|---|---|
| Anunciação et al.24 | 10 normotensive trained men (23 ± 2 years of age) | 4/cross-over | 8 exercises; 1 or 3 sets (circuit and traditional); 18 reps; 40% 1RM; 1–2 minutes (standard) and 3–5 minutes (circuit) of rest interval | Oscillometric automatic (60 minutes) | ↓SBP, DBP and MBP to mean of 60 minutes (3 sets sessions) |
| Arazi et al.25 | 11 normotensive sedentary men (19 ± 1 years of age) | 2/cross-over | 6 exercises (circuit); 1 set; 10RM 30 and 40 seconds of rest interval | Auscultatory (80 minutes) | ↓SBP to 40, 50, 60, 70 and 80 minutes |
| Bermudes et al.26 | 25 normotensive sedentary men (44 ± 1 years of age) | 1/cross-over | 10 exercises (circuit); 3 sets; 20–35 reps; 40% 1RM; 30 seconds (exercise) and 2 minutes (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | ↓DBP during sleep |
| Brito et al.27 | 10 hypertensive sedentary women (61 ± 2 years of age) | 2/cross-over | 10 exercises; 1 set; 10 reps; 50 and 80% 1RM; 90 seconds (exercise) and 90 seconds (sets) of rest interval | Photoplethysmography (90 minutes) | ↓SBP and DBP to 10, 30, 50, 70 and 90 minutes |
| Costa et al.28 | 6 hypertensive trained men (66 ± 5 years of age); 9 hypertensive sedentary women (66 ± 4 years of age) | 2/cross over | 7 exercises; 2 sets; 10–15 reps; 10–15RM; 120 seconds (exercise) and 60 seconds (sets) of rest interval | Auscultatory (60 minutes) | ↓SBP to 30 minutes (normotensive); ↓SBP throughout period; ↓DBP to 30 minutes (hypertensive) |
| DeVan et al.29 | 16 normotensive men and women (sedentary or recreationally active) (27 ± 1 years of age) | 2/cross-over | 9 exercises; 1 set; maximum reps; 75% 1RM | Oscillometric automatic (150 minutes) | ↓DBP to 30 minutes |
| Focht and Koltyn30 | 84 normotensive trained men and women (adults) | 2/cross-over | 4 exercises; 3 sets; 4–8/12–20 reps; 80% 1RM (4–8 reps) and 50% 1RM (12–20 reps) | Oscillometric automatic (180 minutes) | NS |
| Hardy and Tucker31 | 24 hypertensive sedentary men (50 ± 10 years of age) | 2/cross-over | 7 exercises; 3 sets; 8–12RM; 1 minute of rest interval | Oscillometric automatic ABPM (23 h) | ↓SBP to 60 minutes |
| Keese et al.5 | 21 normotensive trained men (20 ± 1 years of age) | 2/cross-over | 8 exercises; 3 sets; 6–8 reps; 80% 1RM; 2 minutes of rest interval | Oscillometric automatic ABPM (120 minutes) | ↓SBP up to 80 minutes |
| Melo et al.32 | 11 hypertensive sedentary women (46 ± 1 years of age) | 1/cross-over | 6 exercises; 3 sets; 20 reps; 40% 1RM; 90 seconds (exercise) and 45 seconds (sets) of rest interval | Auscultatory (2 hours); oscillometric automatic ABPM (21 hours) | ↓SBP to 90 minutes; ↓DBP to 45, 60 and 75 minutes (auscultatory); ↓SBP and DBP for 10 hours (ABPM) |
| Moraes et al.2 | 8 normotensive sedentary men (38 ± 4 years of age); 10 hypertensive sedentary men (44 ± 2 years of age) | 2/cross-over | 7 exercises (circuit); 3 sets; 12 reps; 50% 1RM; 30 seconds (exercise) and 2 minutes (circuits) of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓SBP to 30–60 minutes and mean of 24 hours (normotensive); ↓SBP to 45 and 60 minutes; ↓DBP to 60 minutes (hypertensive) |
| Moreira et al.33 | 20 normotensive sedentary men and women (33 ± 7 years of age) | 1/cross-over | 7 exercises (circuit); 3 sets; 15 reps; 50% 1RM; 2 minutes of rest interval | Auscultatory (60 minutes) | ↓SBP, ↓DBP and ↓MBP up to 60 minutes |
| Mota et al.35 | 15 hypertensive sedentary men and women (43 ± 2 years of age) | 1/cross-over | 13 exercises (circuit); 1 set; 20 reps; 40% 1RM; 30 seconds of rest interval | Oscillometric automatic (60 minutes); oscillometric automatic ABPM (7 hours) | ↓SBP and MBP 15–60 minutes; ↓DBP to 30 minutes |
| Mota et al.34 | 32 hypertensive sedentary women (67 ± 7 years of age) | 4/cross-over | 10 exercises; 3 sets; 8–12 reps; 60–80% 1RM; 60–90 seconds of rest interval | Oscillometric automatic (60 minutes) | ↓SBP and DBP |
| Neto et al.36 | 24 normotensive trained men (22 ± 3 years of age) | 2/cross-over | 4 exercises; 1 and 4 sets; 8 and 30 reps; 80% 1RM (traditional) and 20% 1RM (blood flow restriction); 30 seconds (sets) and 60 seconds (exercises) of rest interval | Oscillometric automatic (60 minutes) | ↓SBP and DBP to 20, 30, 40, 50 and 60 minutes |
| Niemela et al.37 | 12 normotensive trained men (31 ± 3 years of age) | 4/cross-over | 4 exercises; 3 sets; 12 and 20 reps; 80% 1RM (12 reps) and 30% 1RM (20 reps) | Photoplethysmography (180 minutes) | NS |
| O’Connor et al.38 | 14 normotensive trained women (23 ± 4 years of age) | 6/cross-over | 6 exercises; 3 sets; 10 reps; 40%, 60% and 80% 10RM | Oscillometric automatic ABPM (120 minutes) | ↑SBP to 15 minutes (80% 10RM) |
| Olher et al.39 | 12 hypertensive sedentary women (64 ± 1 years of age) | 2/cross-over | 1 exercise; 4 sets; 5 reps; 30% and 60% MVC | Oscillometric automatic (60 minutes) | NS |
| Polito and Farinatti40 | Normotensive trained men: control group (n = 8; 24 ± 1 years of age), arm exercise group (n = 8; 22 ± 1 years of age), leg exercise group (n = 8; 22 ± 1 years of age) | 4/randomised controlled with parallel group | 1 exercise; 6 and 10 sets; 10 reps; 70–80% 1RM; 120 seconds of rest interval | Oscillometric semi-automatic (60 minutes) | ↓SBP throughout period |
| Polito et al.41 | Normotensive sedentary men: exercise group (n = 9; 28 ± 6 years of age), control group (n = 7; 32 ± 3 years of age) | 1/randomised controlled with parallel group | 1 exercise; 10 sets; 15 reps; 90% 15RM; 120 seconds of rest interval | Oscillometric semi-automatic (60 minutes) | ↓SBP to 10 minutes |
| Prista et al.42 | 24 normotensive sedentary men (41 ± 1 years of age) | 4/cross-over | 8 exercises; 1 set; 8–12 reps; 50–60% 1RM and 30–40% 1RM; 60 seconds of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓DBP to 30, 45 and 60 minutes; ↓SBP and DBP to 6–14 hours |
| Queiroz et al.20 | 15 normotensive sedentary men and women (25 ± 1 years of age) | 4/cross-over | 6 exercises; 3 sets; 50% 1RM; 45 seconds (sets) and 90 seconds (exercises) of rest interval | Auscultatory (60 minutes) | ↓SBP and DBP to 30, 45 and 60 minutes |
| Queiroz et al.44 | 16 normotensive trained: men (n = 5)/women (n = 11) (63 ± 1 years of age) | 3/cross-over | 9 exercises; 3 sets; 8 maximum repetitions; 180 seconds (exercises) and 120 seconds (sets) of rest interval | Auscultatory (60 minutes); oscillometric automatic ABPM (24 hours) | ↓SBP to 60 minutes |
| Queiroz et al.43 | 44 normotensive sedentary: men (n = 22; 25 ± 1 years of age); women (n = 22; 25 ± 1 years of age) | 2/cross-over | 6 exercises; 3 sets; 20 repetitions; 40–50% 1RM; 90 seconds (exercises) and 45 seconds (sets) of rest interval | Auscultatory (60 minutes) | ↓SBP and DBP |
| Queiroz et al.45 | Sedentary men: 14 normotensive (44 ± 3 years of age) and 12 hypertensive (50 ± 3 years of age) | 2/cross-over | 7 exercises; 3 sets; 50% 1RM; 90 seconds (exercises) and 45 seconds (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | ↓SBP and DBP |
| Rezk et al.21 | 17 normotensive sedentary men and women (23 ± 1 years of age) | 4/cross-over | 6 exercises; 3 sets; 10–20 reps; 40% and 80% 1RM; 90 seconds (exercise) and 45 seconds (sets) | Auscultatory (90 minutes) | ↓SBP on both intensities over the whole period; ↓DBP to 15 and 30 minutes to 40% 1RM |
| Roltsch et al.46 | Normotensive men and women: resistance trained (n = 12; 23 ± 2 years of age), endurance trained (n = 10; 24 ± 3 years of age), sedentary (n = 11; 20 ± 2 years of age) | 3/cross-over | 12 exercises; 2 sets; 8–12RM; 60 seconds (exercise) and 60 seconds (sets) of rest interval | Oscillometric automatic ABPM (24 hours) | NS |
| Simoes et al.47 | Normotensive trained men: 10 healthy (52 ± 13 years of age); 10 type II diabetes (47 ± 13 years of age) | 4/cross-over | 6 exercises (circuit); 3 sets; 16 and 30 reps; 23% 1RM (30 reps) and 43% 1RM (16 reps); 20 seconds (exercise) and 120 seconds (sets) of rest interval | Oscillometric automatic (120 minutes) | ↓SBP to 30, 75, 90 and 120 minutes for 43% 1RM (healthy); ↓SBP to 30, 45 and 90 minutes (type II diabetes) |
| Teixeira et al.48 | 20 normotensive sedentary men and women (26 ± 1 years of age) | 2/cross-over | 6 exercises; 3 sets; 20 reps; 50% 1RM; 45 seconds (exercise) and 90 seconds (sets) of rest interval | Auscultatory (120 minutes) | ↓SBP and DBP |
| Veloso et al.49 | 16 normotensive sedentary men (23 ± 3 years of age) | 6/cross-over | 6 exercises; 3 sets; 8 reps; 50–80% 1RM; 2 minutes (exercise) and 1–3 minutes (sets) of rest interval | Oscillometric automatic (90 minutes) | ↓DBP to 15, 30 and 90 minutes |
BP: blood pressure; SBP: systolic blood pressure; DBP: diastolic blood pressure; MBP: mean blood pressure; ABPM: ambulatory blood pressure monitoring; MVC: maximum voluntary contraction; ANP: atrial natriuretic peptide; RPE: rating of perceived exertion; 1RM: One-repetition maximum.
Risk of bias within studies
Figure 2 shows the risk of bias for the included studies. The kappa correlation showed a good overall agreement between the researchers (κ = 0.647; 95% confidence interval (CI): 0.544–0.740; p < 0.001). All studies reported point and variability measures for BP; in one study, baseline BP was not similar between sessions and three studies did not report baseline comparisons. The allocation was concealed in only four studies and only 18 studies used automatic devices in order to measure the BP.
Risk of bias across studies
The potential for publication bias was assessed through visual inspection of the funnel plots (Supplementary File 1). Duval and Tweedie’s correction model23 was applied to the normotensive study groups for both systolic and diastolic BP. In both cases, no trimmed studies could be identified.
Sensitivity analyses
A leave-one-out sensitivity analysis was used in order to investigate the effect of excluding the study that reported a significantly larger effect on systolic and diastolic BP (90 minutes).27 The sensitivity analysis was [mmHg (95% CI)] −5.28 (−8.49 to −2.05) versus −3.90 (−6.07 to −1.74) for systolic BP and −4.67 (−6.94 to −2.41) versus −3.42 (−4.95 to −1.88) for diastolic BP (Supplementary File 2).
Main outcomes
Figures 3 and 4 show the forest plots for systolic BP and diastolic BP at 60 minutes, 90 minutes and over a 24–hour period after a single session of resistance exercise. At 1 hour following a resistance exercise session, we observed an overall reduction in BP of −3.3 (−4.0 to −2.6)/−2.7 (−3.2 to −2.1) mmHg (CI 95%) compared to the control session. Similar results were observed at 90 minutes post-exercise (−5.3 (−8.5 to −2.1)/−4.6 (−6.9 to −2.4) mmHg) and over the course of 24–hour monitoring (−1.7 (−2.8 to −0.67)/−1.2 (−2.4 to −0.022) mmHg (CI 95%)). The BP reduction was not different at 60 or 90 minutes after exercise (p = 0.234 for systolic BP and p = 0.092 for diastolic BP).
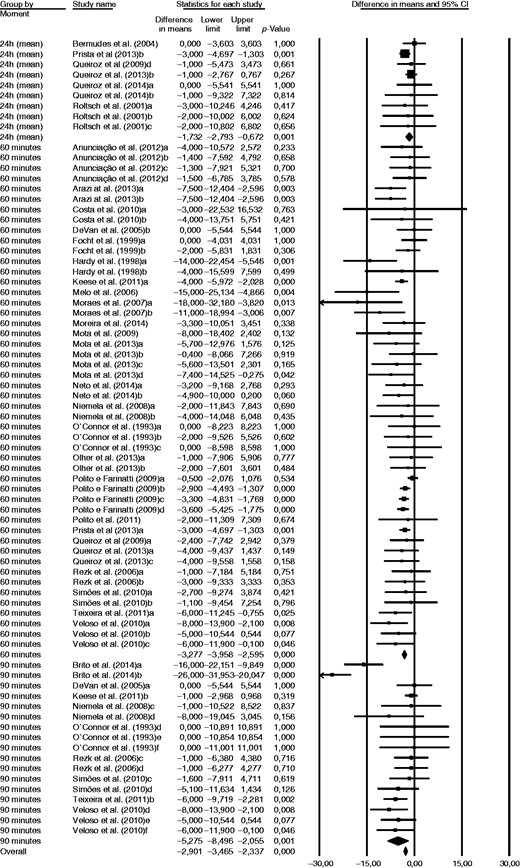
Changes in systolic blood pressure (mmHg) following a single session of resistance exercise.
CI: confidence interval.
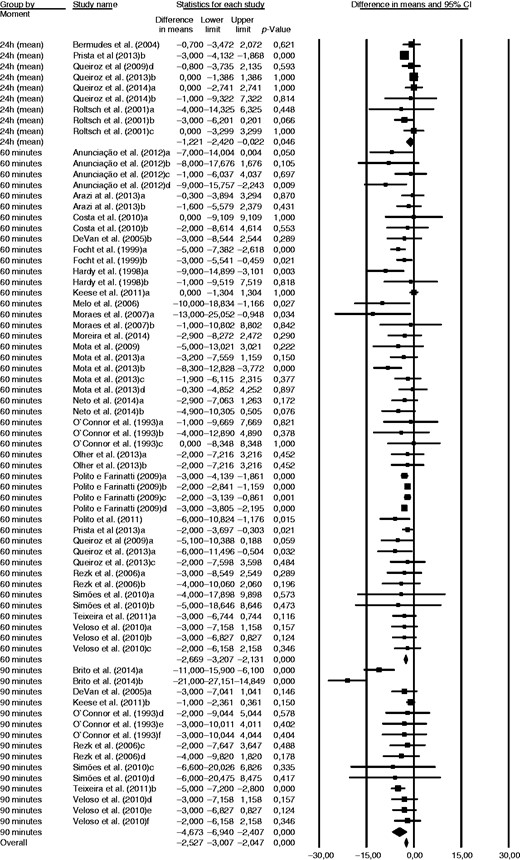
Changes in diastolic blood pressure (mmHg) following a single session of resistance exercise.
CI: confidence interval.
Table 2 summarises the results of the subgroup analyses for the BP reductions following 60–90 minutes of recovery. A more pronounced BP reduction was observed in hypertensive compared to normotensive individuals (p < 0.01 for both systolic BP and diastolic BP). Furthermore, resistance training involving large muscle groups promoted larger reductions in systolic BP and diastolic BP compared to sessions that involved only the use of small muscle groups (p < 0.05 for both). Finally, compared with recovery in a seated position, the supine position promoted a larger exercise-induced BP reduction (p < 0.01 for both).
Subgroup analyses of the effect of resistance exercise on post-exercise systolic and diastolic blood pressure.
| . | . | Systolic blood pressure I2 = 42.7 p for heterogeneity < 0.001 . | . | Diastolic blood pressure I2 = 39.5 p for heterogeneity = 0.001 . |
|---|---|---|---|---|
| . | n . | Effect size (95% CI) . | n . | Effect size (95% CI) . |
| Exercise intensity | ||||
| High | 24 | −4.00 (−5.43 to −2.56) | 22 | −2.43 (−3.27 to −1.59) |
| Moderate | 18 | −5.35 (−4.67 to −1.41) | 18 | −4.18 (−5.36 to −2.99) |
| Low | 24 | −3.04 (−7.12 to −3.54) | 22 | −3.55 (−4.91 to −2.18) |
| Exercise volume | ||||
| <150 | 24 | −4.90 (−6.35 to −3.45) | 22 | −3.25 (−4.10 to −2.41) |
| 150–299 | 25 | −3.85 (−5.57 to −2.12) | 23 | −2.24 (−3.42 to −1.07) |
| ≥300 | 12 | −3.74 (−5.91 to −1.57) | 12 | −4.64 (−6.37 to −2.91) |
| Type of training | ||||
| Circuit | 12 | −5.16 (−7.56 to −2.77) | 12 | −3.23 (−5.47 to −0.99) |
| Traditional | 54 | −3.84 (−4.84 to −2.84) | 50 | −3.19 (−3.87 to −2.51) |
| Gender | ||||
| Male | 37 | −3.99 (−5.14 to −2.84) | 33 | −2.50 (−3.25 to −1.74) |
| Female | 16 | −6.21 (−8.34 to −4.02) | 16 | −4.64 (−6.20 to −3.09) |
| Blood pressure equipment | ||||
| Auscultatory | 24 | −3.09 (−3.83 to −2.36) | 24 | −2.66 (−3.22 to −2.04) |
| Oscillometric Photoplethysmography | 51 6 | −2.46 (−3.11 to −1.82) −10.03 (−18.85 to −1.20) | 51 2 | −2.26 (−2.77 to −1.75) −12.82 (−25.61 to 1.03) |
| Training status | ||||
| Trained | 29 | −3.66 (−5.04 to −2.28) | 25 | −2.99 (−3.96 to −2.02) |
| Sedentary | 37 | −4.37 (−5.64 to −3.11) | 37 | −3.32 (−4.17 to −2.47) |
| Muscle mass | ||||
| Small | 4 | −1.66 (−4.61 to + 1.29) | 4 | −2.38 (−4.35 to −0.41) |
| Large | 22 | −2.97 (−4.68 to −1.25)a | 22 | −3.41 (−4.63 to −2.20) |
| Both | 40 | −4.96 (−6.15 to −3.77)a | 36 | −3.34 (−4.25 to −2.43) |
| Recovery posture | ||||
| Supine | 5 | −9.08 (−12.36 to −5.80)b | 5 | −7.75 (−10.15 to −5.34)c |
| Seated | 57 | −3.37 (−4.26 to −2.48) | 53 | −2.70 (−3.30 to −2.10) |
| Clinical status | ||||
| Hypertensive | 15 | −9.05 (−11.34 to −6.75)d | 15 | −5.45 (−7.07 to −3.84)e |
| Normotensive | 51 | −3.17 (−4.05 to −2.29) | 47 | −2.73 (−3.38 to −2.08) |
| . | . | Systolic blood pressure I2 = 42.7 p for heterogeneity < 0.001 . | . | Diastolic blood pressure I2 = 39.5 p for heterogeneity = 0.001 . |
|---|---|---|---|---|
| . | n . | Effect size (95% CI) . | n . | Effect size (95% CI) . |
| Exercise intensity | ||||
| High | 24 | −4.00 (−5.43 to −2.56) | 22 | −2.43 (−3.27 to −1.59) |
| Moderate | 18 | −5.35 (−4.67 to −1.41) | 18 | −4.18 (−5.36 to −2.99) |
| Low | 24 | −3.04 (−7.12 to −3.54) | 22 | −3.55 (−4.91 to −2.18) |
| Exercise volume | ||||
| <150 | 24 | −4.90 (−6.35 to −3.45) | 22 | −3.25 (−4.10 to −2.41) |
| 150–299 | 25 | −3.85 (−5.57 to −2.12) | 23 | −2.24 (−3.42 to −1.07) |
| ≥300 | 12 | −3.74 (−5.91 to −1.57) | 12 | −4.64 (−6.37 to −2.91) |
| Type of training | ||||
| Circuit | 12 | −5.16 (−7.56 to −2.77) | 12 | −3.23 (−5.47 to −0.99) |
| Traditional | 54 | −3.84 (−4.84 to −2.84) | 50 | −3.19 (−3.87 to −2.51) |
| Gender | ||||
| Male | 37 | −3.99 (−5.14 to −2.84) | 33 | −2.50 (−3.25 to −1.74) |
| Female | 16 | −6.21 (−8.34 to −4.02) | 16 | −4.64 (−6.20 to −3.09) |
| Blood pressure equipment | ||||
| Auscultatory | 24 | −3.09 (−3.83 to −2.36) | 24 | −2.66 (−3.22 to −2.04) |
| Oscillometric Photoplethysmography | 51 6 | −2.46 (−3.11 to −1.82) −10.03 (−18.85 to −1.20) | 51 2 | −2.26 (−2.77 to −1.75) −12.82 (−25.61 to 1.03) |
| Training status | ||||
| Trained | 29 | −3.66 (−5.04 to −2.28) | 25 | −2.99 (−3.96 to −2.02) |
| Sedentary | 37 | −4.37 (−5.64 to −3.11) | 37 | −3.32 (−4.17 to −2.47) |
| Muscle mass | ||||
| Small | 4 | −1.66 (−4.61 to + 1.29) | 4 | −2.38 (−4.35 to −0.41) |
| Large | 22 | −2.97 (−4.68 to −1.25)a | 22 | −3.41 (−4.63 to −2.20) |
| Both | 40 | −4.96 (−6.15 to −3.77)a | 36 | −3.34 (−4.25 to −2.43) |
| Recovery posture | ||||
| Supine | 5 | −9.08 (−12.36 to −5.80)b | 5 | −7.75 (−10.15 to −5.34)c |
| Seated | 57 | −3.37 (−4.26 to −2.48) | 53 | −2.70 (−3.30 to −2.10) |
| Clinical status | ||||
| Hypertensive | 15 | −9.05 (−11.34 to −6.75)d | 15 | −5.45 (−7.07 to −3.84)e |
| Normotensive | 51 | −3.17 (−4.05 to −2.29) | 47 | −2.73 (−3.38 to −2.08) |
Difference compared to small muscle mass (p < 0.05).
Difference compared to seated position (p = 0.001).
Difference compared to seated position (p < 0.001).
Difference compared to normotensive (p < 0.001).
Difference compared to normotensive (p = 0.002).
CI: confidence interval.
Subgroup analyses of the effect of resistance exercise on post-exercise systolic and diastolic blood pressure.
| . | . | Systolic blood pressure I2 = 42.7 p for heterogeneity < 0.001 . | . | Diastolic blood pressure I2 = 39.5 p for heterogeneity = 0.001 . |
|---|---|---|---|---|
| . | n . | Effect size (95% CI) . | n . | Effect size (95% CI) . |
| Exercise intensity | ||||
| High | 24 | −4.00 (−5.43 to −2.56) | 22 | −2.43 (−3.27 to −1.59) |
| Moderate | 18 | −5.35 (−4.67 to −1.41) | 18 | −4.18 (−5.36 to −2.99) |
| Low | 24 | −3.04 (−7.12 to −3.54) | 22 | −3.55 (−4.91 to −2.18) |
| Exercise volume | ||||
| <150 | 24 | −4.90 (−6.35 to −3.45) | 22 | −3.25 (−4.10 to −2.41) |
| 150–299 | 25 | −3.85 (−5.57 to −2.12) | 23 | −2.24 (−3.42 to −1.07) |
| ≥300 | 12 | −3.74 (−5.91 to −1.57) | 12 | −4.64 (−6.37 to −2.91) |
| Type of training | ||||
| Circuit | 12 | −5.16 (−7.56 to −2.77) | 12 | −3.23 (−5.47 to −0.99) |
| Traditional | 54 | −3.84 (−4.84 to −2.84) | 50 | −3.19 (−3.87 to −2.51) |
| Gender | ||||
| Male | 37 | −3.99 (−5.14 to −2.84) | 33 | −2.50 (−3.25 to −1.74) |
| Female | 16 | −6.21 (−8.34 to −4.02) | 16 | −4.64 (−6.20 to −3.09) |
| Blood pressure equipment | ||||
| Auscultatory | 24 | −3.09 (−3.83 to −2.36) | 24 | −2.66 (−3.22 to −2.04) |
| Oscillometric Photoplethysmography | 51 6 | −2.46 (−3.11 to −1.82) −10.03 (−18.85 to −1.20) | 51 2 | −2.26 (−2.77 to −1.75) −12.82 (−25.61 to 1.03) |
| Training status | ||||
| Trained | 29 | −3.66 (−5.04 to −2.28) | 25 | −2.99 (−3.96 to −2.02) |
| Sedentary | 37 | −4.37 (−5.64 to −3.11) | 37 | −3.32 (−4.17 to −2.47) |
| Muscle mass | ||||
| Small | 4 | −1.66 (−4.61 to + 1.29) | 4 | −2.38 (−4.35 to −0.41) |
| Large | 22 | −2.97 (−4.68 to −1.25)a | 22 | −3.41 (−4.63 to −2.20) |
| Both | 40 | −4.96 (−6.15 to −3.77)a | 36 | −3.34 (−4.25 to −2.43) |
| Recovery posture | ||||
| Supine | 5 | −9.08 (−12.36 to −5.80)b | 5 | −7.75 (−10.15 to −5.34)c |
| Seated | 57 | −3.37 (−4.26 to −2.48) | 53 | −2.70 (−3.30 to −2.10) |
| Clinical status | ||||
| Hypertensive | 15 | −9.05 (−11.34 to −6.75)d | 15 | −5.45 (−7.07 to −3.84)e |
| Normotensive | 51 | −3.17 (−4.05 to −2.29) | 47 | −2.73 (−3.38 to −2.08) |
| . | . | Systolic blood pressure I2 = 42.7 p for heterogeneity < 0.001 . | . | Diastolic blood pressure I2 = 39.5 p for heterogeneity = 0.001 . |
|---|---|---|---|---|
| . | n . | Effect size (95% CI) . | n . | Effect size (95% CI) . |
| Exercise intensity | ||||
| High | 24 | −4.00 (−5.43 to −2.56) | 22 | −2.43 (−3.27 to −1.59) |
| Moderate | 18 | −5.35 (−4.67 to −1.41) | 18 | −4.18 (−5.36 to −2.99) |
| Low | 24 | −3.04 (−7.12 to −3.54) | 22 | −3.55 (−4.91 to −2.18) |
| Exercise volume | ||||
| <150 | 24 | −4.90 (−6.35 to −3.45) | 22 | −3.25 (−4.10 to −2.41) |
| 150–299 | 25 | −3.85 (−5.57 to −2.12) | 23 | −2.24 (−3.42 to −1.07) |
| ≥300 | 12 | −3.74 (−5.91 to −1.57) | 12 | −4.64 (−6.37 to −2.91) |
| Type of training | ||||
| Circuit | 12 | −5.16 (−7.56 to −2.77) | 12 | −3.23 (−5.47 to −0.99) |
| Traditional | 54 | −3.84 (−4.84 to −2.84) | 50 | −3.19 (−3.87 to −2.51) |
| Gender | ||||
| Male | 37 | −3.99 (−5.14 to −2.84) | 33 | −2.50 (−3.25 to −1.74) |
| Female | 16 | −6.21 (−8.34 to −4.02) | 16 | −4.64 (−6.20 to −3.09) |
| Blood pressure equipment | ||||
| Auscultatory | 24 | −3.09 (−3.83 to −2.36) | 24 | −2.66 (−3.22 to −2.04) |
| Oscillometric Photoplethysmography | 51 6 | −2.46 (−3.11 to −1.82) −10.03 (−18.85 to −1.20) | 51 2 | −2.26 (−2.77 to −1.75) −12.82 (−25.61 to 1.03) |
| Training status | ||||
| Trained | 29 | −3.66 (−5.04 to −2.28) | 25 | −2.99 (−3.96 to −2.02) |
| Sedentary | 37 | −4.37 (−5.64 to −3.11) | 37 | −3.32 (−4.17 to −2.47) |
| Muscle mass | ||||
| Small | 4 | −1.66 (−4.61 to + 1.29) | 4 | −2.38 (−4.35 to −0.41) |
| Large | 22 | −2.97 (−4.68 to −1.25)a | 22 | −3.41 (−4.63 to −2.20) |
| Both | 40 | −4.96 (−6.15 to −3.77)a | 36 | −3.34 (−4.25 to −2.43) |
| Recovery posture | ||||
| Supine | 5 | −9.08 (−12.36 to −5.80)b | 5 | −7.75 (−10.15 to −5.34)c |
| Seated | 57 | −3.37 (−4.26 to −2.48) | 53 | −2.70 (−3.30 to −2.10) |
| Clinical status | ||||
| Hypertensive | 15 | −9.05 (−11.34 to −6.75)d | 15 | −5.45 (−7.07 to −3.84)e |
| Normotensive | 51 | −3.17 (−4.05 to −2.29) | 47 | −2.73 (−3.38 to −2.08) |
Difference compared to small muscle mass (p < 0.05).
Difference compared to seated position (p = 0.001).
Difference compared to seated position (p < 0.001).
Difference compared to normotensive (p < 0.001).
Difference compared to normotensive (p = 0.002).
CI: confidence interval.
Meta-regression analysis did not show any association between age and systolic BP (p = 0.70) or diastolic BP (p = 0.39) at 60–90 minutes post-exercise, nor between age and systolic BP (p = 0.54) or diastolic BP (p = 0.23) at 24 hours following exercise session.
Discussion
The major findings of this meta-analysis showed that one bout of resistance exercise can induce a transient reduction in BP in healthy adults that is more pronounced in hypertensive individuals, when large muscle groups are used and when patients recover in a supine position.
The observation that 24–hour BP was lower following a resistance exercise session compared to a sedentary control session adds further evidence to the BP-lowering potential of dynamic resistance exercise in BP management.50 Of interest is that the BP reductions were greater in individuals with hypertension compared to their normotensive counterparts. This is consistent with the findings observed following acute and chronic aerobic exercise interventions.13 As such, one session of resistance training can promote important cardiovascular protection by lowering BP to within more normal ranges during the day.51 However, some adverse effects of PEH should be highlighted. Namely, PEH syncope represents a failure of integrative physiology during recovery from exercise and might be developed by healthy individuals, including athletes, or in individuals with autonomic disorders. PEH syncope is most often neutrally mediated syncope during recovery from exercise, with a combination of factors associated with PEH and loss of the muscle pump contributing to the onset of the event.
However, despite the fact that our findings confirm that a single bout of dynamic resistance exercise might be a good alternative to a daily aerobic exercise session for helping to manage BP, the physiological mechanisms associated with the reduction in BP may be different for aerobic52,53 and resistance exercises.21 Furthermore, it is widely accepted that, independent of the physiological mechanism that might influence PEH, not all individuals respond in the same way. Approximately 65% of the individuals experienced a fall in BP following exercise.54 It has previously been demonstrated that 17% of the reduction in systolic BP after training can be explained by genetic polymorphisms.55 However, only a few studies have investigated the genetic influence on BP response to resistance exercise. Furthermore, these studies also demonstrated a lack of power to identify these associations; thus, larger randomised controlled trials are warranted.
The PEH length after resistance exercise was significantly different between the time points. There was a reduction in both systolic and diastolic BP after exercise for 60 and 90 minutes. However, the reduction in the 24-hour average was only significant for diastolic BP. One explanation for this may be that the measures at 60 and 90 minutes were performed in a controlled environment (laboratory) with patients at rest, which facilitates the identification of major cardiovascular adjustments.56 Regarding the results of the 24–hour measures, the reduction in diastolic BP suggests haemodynamic alterations that persist with time, but the physiological mechanisms related to this reduction are still unknown. Future studies should be conducted in order to examine the behaviour of BP at 24 hours following resistance exercise sessions.
Subgroup analyses of office BP further demonstrated that resistance training sessions involving large muscle groups induced greater PEH compared to sessions involving only small muscle groups. However, notably, only four trials were included with small muscles and more research is warranted. Furthermore, the size of the muscle group involved in the resistance exercise per se may be subjective in a certain way. In the present study, exercises were considered to use large muscle groups if they involved multi-joint movements or if large muscles were used in a single-joint movement, such as the quadriceps or latissimus dorsi. One possible explanation for our results could be that baroreflex resetting is proportional to the muscle mass involved in the exercise.57 Baroreflex resetting is related to lower sympathetic activity via greater inhibition of the rostral ventral lateral medulla,57 which can enhance PEH.
Other resistance training characteristics did not significantly affect the BP reduction following exercise. It is of great interest that both low- and high-intensity resistance exercises induce similar BP reductions. These data increase the applicability of resistance exercise prescription for large groups of patients, including hypertensive patients, who are advised not to perform such exercise at high intensities.58 Concerning the total volume, we computed exercises × sets × repetitions due to the methodological differences in resistance exercise sessions (i.e. number of sets, repetitions and exercises). Nevertheless, the literature does not provide enough data to explain the physiological mechanisms related to exercise volume and BP after resistance exercise. On the other hand, the minimum workout volume that is required in order to induce PEH after a resistance exercise session remains unclear.
In addition, neither the physical fitness status of the participants (trained or sedentary) nor gender affected the BP reductions following resistance exercise. Regardless of our results, some data suggest that chronic resistance training can decrease PEH magnitude.59,60 Nevertheless, these studies did not report increased muscle strength, which would be expected after a resistance training period. In this context, the results of these studies should not be related to resistance training or other physiological alterations, regardless of the gains in muscle strength. Therefore, the present study did not include references involving chronic training, and the definition of participants as trained or sedentary was extracted from the trial data. Concerning gender, to our knowledge, only one study has investigated the BP responses of men and women after a resistance training session.44 The authors concluded that PEH was similar between genders, but the physiological mechanisms related to PEH were different. In this context, systemic vascular resistance was reduced in women, while cardiac output was decreased in men, and these responses were accompanied by a decrease in stroke volume in men and a more pronounced increase in heart rate in men than in women.
Whereas the device used in order to assess BP did not affect PEH, the recovery position did. The significantly larger reduction in BP when measured in the supine position can be explained by the fact that the supine position allows for better blood distribution, with a consequent reduction in peripheral vascular resistance.61 The seated position may require greater vascular compression of the lower limbs due to gravity.61 Regardless of these explanations, only five trials performed an analysis in the supine position, while more than 50 trials used the seated position. Therefore, the definitive conclusion that the supine position favours PEH requires further investigation.
Some limitations must be mentioned. First, there are only a small number of studies involving hypertensive patients or patients using anti-hypertensive medication, which limits the generalisability of the results. Furthermore, our meta-analysis showed a moderate degree of heterogeneity; however, since systematic reviews bring together studies that are both clinically and methodologically diverse, heterogeneity in the results is to be expected.62 Next, in line with our previous meta-analyses and in order to allow for comparison with other meta-analyses in the field, we restricted the inclusion criteria for the current meta-analysis to full publications in peer-reviewed journals because data from abstracts that remain unpublished may not be reliable and usually contain insufficient information; in addition, it is not possible to identify all of the relevant unpublished material.63 However, we do acknowledge that because of this, our results might slightly overestimate the observed effect in the current meta-analysis. Namely, it has been shown that effect size estimates of published research are approximately a third larger than those of unpublished studies.63 Yet, given that we did not find any signs of significant asymmetry in the funnel plots, we believe that is it reasonable to assume that publication bias did not affect our results.
In conclusion, effect sizes were significant in both normotensive and hypertensive subjects, although hypertensive subjects exhibited greater BP reductions than normotensive subjects. Exercise sessions involving large or a combination of large and small muscle groups elicited larger BP reductions than the use of only small muscle groups. The lack of differences with regards to intensity, total volume, type of training (traditional or circuit), physical fitness status (trained or sedentary) or gender offers significant opportunities for the prescription of resistance training, taking into account individual preferences.
Author contribution
JC, JRC and MDP contributed to the conception of the work. JC, KFG, VAC and MDP contributed to the design of the work. JC and KFG contributed to the acquisition of the data. JC, KFG, VAC and MDP drafted and critically revised the manuscript.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: this study was partially supported by grants from the Brazilian Council for Research Development (CNPq). MDP is supported by grants from the Brazilian Council for Research Development (number 303566/2013-2). KFG is a postdoctoral research fellow supported by Brazilian Council for Research Development (200453/2015-7). VAC is a postdoctoral research fellow supported by the Research Foundation Flanders (FWO). VAC is supported by a research grant (Krediet aan Navorsers) of the Research Foundation Flanders (FWO) Process number 1502214N.
References
Author notes
These authors contributed equally to this work.




Comments