-
PDF
- Split View
-
Views
-
Cite
Cite
S Von Koch, M Zhou, H C Rosen, S Zwackman, J Jurga, P Grimfjard, M Gotberg, M A Mohammad, D Erlinge, Percutaneous coronary intervention of in-stent restenosis: A three-arm analysis from SWEDEHEART, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.1445, https://doi.org/10.1093/eurheartj/ehae666.1445
Close - Share Icon Share
Abstract
During the last decades, there have been substantial improvements in treatment techniques for percutaneous coronary intervention (PCI). Yet, in-stent restenosis (ISR) continues to pose significant challenges as they account for 10% of all PCI cases and are associated with worse outcome compared to de-novo lesions. When assessing ISR with PCI, balloon angioplasty with drug-coated balloons (DCB) is frequently used.
Despite frequent use of DCB, there is a lack of long-term data ensuring the safety of DCB for ISR as no randomized trial has extended beyond a 3-year follow-up. We aimed to study the long-term outcome and conducted a nationwide three-arm investigation on the outcome of ISR, comparing DCB with drug-eluting stents (DES) or plain old balloon angioplasty (POBA) within a 5-year follow-up.
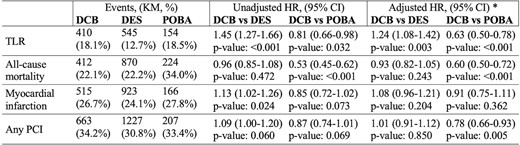
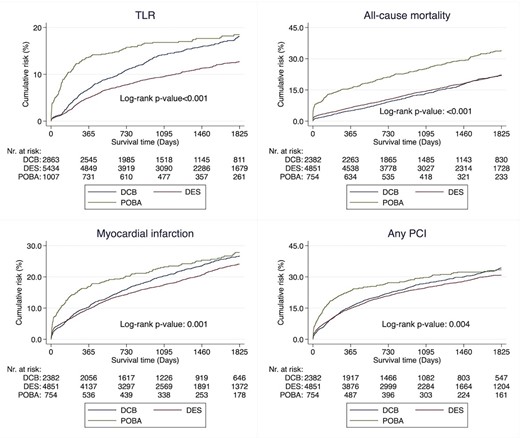
We conducted a nationwide analysis using the SWEDEHEART (Swedish Web System for Enhancement of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies) registry. The SWEDEHEART registry was used to include any ISR undergoing coronary angiography between June 11, 2013, and December 31, 2020. Target lesion revascularization (TLR) was the primary outcome. Secondary outcomes included all-cause mortality, myocardial infarction, and any PCI. The outcomes were analysed using a multivariable Cox regression model.
A total of 9304 segments from 7987 patients were eligible. Compared to POBA, the use of DCB was associated with lower rates of TLR, hazard ratio (HR) 0.62 (95% confidence interval [CI]: 0.50-0.78), all-cause mortality, HR 0.60 (95% CI: 0.50-0.72), and any PCI, HR 0.78 (95% CI: 0.66-0.93). No difference was observed for myocardial infarction. Compared to DES, the use of DCB was associated with higher rates of TLR, HR 1.24 (95% CI: 1.08-1.42). No difference was observed for all-cause mortality, cardiovascular mortality, myocardial infarction, or any PCI.
Author notes
Funding Acknowledgements: Type of funding sources: Foundation. Main funding source(s): Swedish research council and Swedish heart and lung foundation
- myocardial infarction
- percutaneous coronary intervention
- coronary angiography
- heart diseases
- balloon angioplasty
- follow-up
- safety
- arm
- mortality
- drug-eluting stents
- revascularization
- restenosis, in-stent
- cox proportional hazards models
- evidence-based practice
- cardiovascular death
- swedeheart registry
- primary outcome measure



