-
PDF
- Split View
-
Views
-
Cite
Cite
K R An, D Vervoort, F Qiu, D Y Tam, R V Rocha, L Harik, S Hirji, S E Fremes, H C Wijeysundera, M F L Gaudino, Long-term outcomes of percutaneous coronary intervention versus coronary artery bypass grafting in women with severe coronary artery disease, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.1446, https://doi.org/10.1093/eurheartj/ehae666.1446
Close - Share Icon Share
Abstract
The optimal revascularization strategy for severe coronary artery disease (CAD) in women remains controversial. Despite differences between women and men in the development of CAD, there remains a paucity of comparative real-world observational evidence comparing percutaneous coronary intervention (PCI) to coronary artery bypass grafting (CABG) in women.
We evaluated short and long-term outcomes of PCI and CABG in women with severe CAD.
We conducted a propensity score-matched retrospective cohort study using linked clinical and administrative databases in Ontario, Canada to obtain records of women with left main, 3-vessel disease, or 2-vessel disease with proximal left anterior descending artery involvement undergoing PCI or CABG from April 1st, 2012 to December 31st, 2021. Patients who were >80 years of age and patients who underwent urgent or emergent procedures were excluded for the primary analysis. The primary outcome was a composite of myocardial infarction, stroke, repeat revascularization, and death (MACCE). Secondary outcomes included the individual components of MACCE and a composite of readmission for MI, heart failure, and stroke. Following multiple imputation and propensity score-matching, the Cox proportional hazards model and Fine-Gray sub-distribution hazard model with robust variance estimators accounting for death as a competing risk were used to evaluate long-term outcomes.
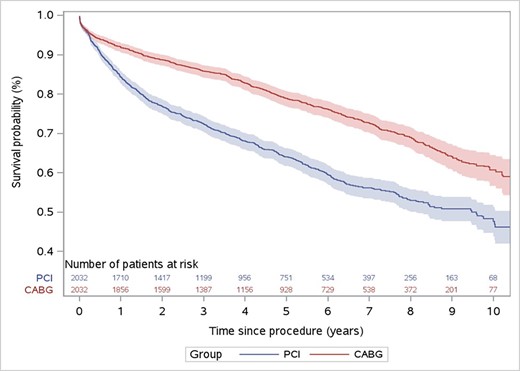
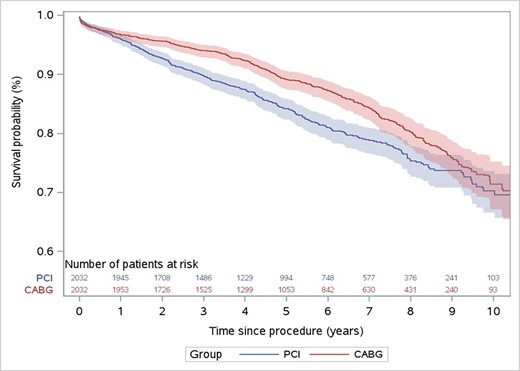
In the primary cohort, 2469 patients underwent PCI and 3,721 patients underwent CABG. After propensity score matching, including by coronary disease territory, 2,033 well-balanced pairs were identified, with standardized mean differences <0.10 for all covariates. In-hospital death and stroke were significantly lower with PCI than with CABG (0.7% vs 1.5%, p=0.036) and (<0.2% vs 1.4%, p<0.001), respectively, and there was no difference in perioperative MI between PCI and CABG (1.1% vs 0.6%, p=0.121). At a median (IQR) of 5.1 (2.9-7.5) years, major adverse cardiac and cerebrovascular events (MACCE) was higher with PCI compared with CABG (37.7% vs 23.3%, HR 1.79, [95% CI: 1.66-1.91], p<0.001) (Figure 1). All-cause mortality was higher with PCI compared with CABG (17.8% vs 13.4%, HR 1.33, [95% CI: 1.21-1.45], p<0.001) (Figure 2). The composite readmission outcome (MI, heart failure, stroke) was higher with PCI compared with CABG (16.2% vs 11.2%, HR 1.42, [95% CI: 1.37-1.48], p<0.001).
Author notes
Funding Acknowledgements: Type of funding sources: Private grant(s) and/or Sponsorship. Main funding source(s): This research is funded by a partnership between the Canadian Cardiovascular Society (CCS) and Bayer Inc. and by Weill Cornell Medicine Institutional Funds.
- myocardial infarction
- percutaneous coronary intervention
- coronary artery bypass surgery
- coronary arteriosclerosis
- anterior descending branch of left coronary artery
- cerebrovascular accident
- ischemic stroke
- heart failure
- canada
- hospital mortality
- patient readmission
- heart
- mortality
- coronary heart disease
- revascularization
- ontario
- perioperative myocardial infarction
- multiple imputation
- primary outcome measure



