-
PDF
- Split View
-
Views
-
Cite
Cite
G.W. Rietman, J.M.A.A. van der Maaten, Y.L. Douglas, P.W. Boonstra, Echocardiographic diagnosis of left ventricular outflow tract obstruction after mitral valve replacement with subvalvular preservation, European Journal of Cardio-Thoracic Surgery, Volume 22, Issue 5, November 2002, Pages 825–827, https://doi.org/10.1016/S1010-7940(02)00465-7
Close - Share Icon Share
Abstract
We describe two cases of left ventricular outflow tract obstruction after mitral valve replacement with complete retention of the subvalvular apparatus. The first patient deteriorated immediately after insertion of a high-profile bioprosthesis. In the second patient, chronic left ventricular outflow tract obstruction developed after the insertion of a low-profile mechanical prosthesis. The clinical course of left ventricular outflow tract obstruction after mitral valve replacement with complete retention of the subvalvular apparatus may differ greatly. Evaluation of the left ventricular outflow tract by perioperative transesophageal echocardiography or epicardial echocardiography is essential in the prevention and treatment of this complication.
1 Clinical and perioperative data
The first patient, an 80-year-old woman with a 5-year-long history of cardiac failure, was admitted for increasing dyspnea and decreasing exercise capacity. Preoperative transthoracic echocardiography (TTE) revealed prolapse of the posterior mitral valve leaflet with 4+ mitral valve regurgitation. The aortic valve was calcified with a peak gradient of 45 mmHg. Left ventricular dimensions were normal with an end-diastolic diameter of 50 mm and an end-systolic diameter of 26 mm. Interventricular septum thickness was 11 mm and posterior wall thickness 10 mm.
The aortic valve was replaced by a porcine Carpentier–Edwards 21-mm SAV bioprosthesis (Baxter Healthcare Corp.). The mitral valve was replaced by a porcine Carpentier–Edwards 27-mm SAV bioprosthesis. The technique for preservation of the native leaflets and subvalvular apparatus of the mitral valve consisted of reefing the posterior leaflet. The anterior leaflet was T-shaped split and plicated to the trigonum respectively to the left and right side.
After uneventful weaning from cardiopulmonary bypass (CPB) hemodynamics deteriorated and was treated by increasing inotropic support and inserting an intra-aortic balloon pump (IABP). Transesophageal echocardiography (TEE) revealed systolic narrowing of the left ventricular outflow tract (LVOT) due to systolic anterior motion (SAM) of the leaflet remnants (Fig. 1) . Continuous wave Doppler showed a late peaking gradient of 80 mmHg over the LVOT. At reoperation, the mitral bioprosthesis was replaced by a St. Jude 27-mm mechanical prosthesis (St. Jude Medical Inc). Remnants of the preserved subvalvular apparatus of the anterior leaflet were excised without sacrificing the annulo-ventricular continuity. The patient was uneventfully weaned from CPB.
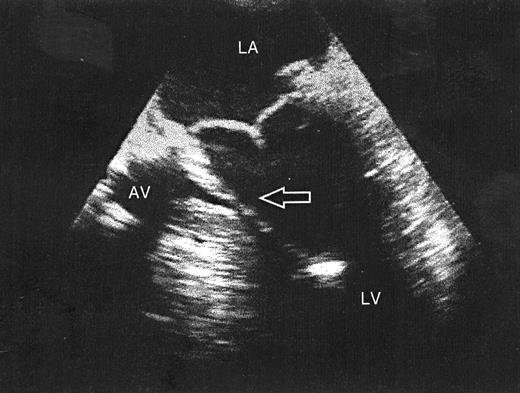
Transesophageal echocardiography five-chamber view. A structure is seen in the left ventricular outflow tract (arrow) extending from the mitral valve annulus to a papillary muscle. AV, aortic valve; LA, left atrium; LV, left ventricle.
The second patient, a 58-year-old man, was admitted for increasing dyspnea of 2 years’ duration. Preoperative TTE revealed 4+ mitral valve regurgitation due to prolapse of the posterior mitral valve leaflet with normal left and right ventricular systolic function. There was no left ventricular hypertrophy (LVH) with a left ventricular mass index (LVMI) of 119 g/m2. Quadrangular resection of the P2 segment was performed and a Carpentier 32-mm annuloplasty ring (Baxter Healthcare Corp.) was inserted. After weaning from CPB, significant mitral valve regurgitation was noted on TEE caused by SAM of the elongated anterior leaflet. During a second pump run, the mitral valve was replaced by a St. Jude 27-mm mechanical prosthesis (St. Jude Medical Inc.) with preservation of the entire subvalvular apparatus using the same technique as described in the first patient. Acoustic shadowing by the mechanical mitral valve prosthesis hindered TEE imaging of the LVOT. Epicardial echocardiography was not performed.
Because of a residual apical systolic murmur, a TTE was performed 3 months postoperatively. It revealed LVOT obstruction involving the remnant of the mitral valve resulting in a late peaking gradient of over 100 mmHg. There was severe LVH with an LVMI of 143 g/m2 (Fig. 2) .
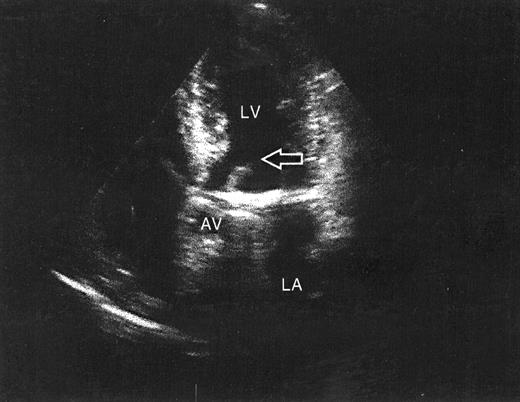
Transthoracic echocardiography apical long-axis view of the left ventricle. A rim of tissue, apparently the preserved anterior subvalvular apparatus of the mitral valve, is seen in the left ventricular outflow tract (arrow). AV, aortic valve; LA, left atrium; LV, left ventricle.
At reoperation, remnants of the preserved subvalvular apparatus of the anterior leaflet were excised through the aortic valve without sacrificing the annulo-ventricular continuity. Epicardial echocardiography was performed after weaning from CPB and revealed a 20-mmHg residual gradient over the LVOT due to thickened interventricular septum. Further clinical course was unremarkable.
2 Discussion
Preservation of the subvalvular apparatus during mitral valve replacement has proven to be superior to standard mitral valve replacement without retention of the subvalvular apparatus. It has been shown to be beneficial for preservation of left ventricular (LV) function and improvement in long-term survival [1–5].
The routine use of this technique has potential complications including LV inflow and outflow obstruction by interference between the prosthetic valve and the subvalvular apparatus. LVOT obstruction most frequently results from implantation of a high-profile bioprosthesis [6,7], but is also reported after implantation of a low-profile mechanical prosthesis [8]. Additionally, a number of risk factors for the development of LVOT obstruction after mitral valve replacement with preservation of the subvalvular apparatus has been identified including small left ventricular cavity [8], LVH and septal hypertrophy [7].
We describe two patients who developed LVOT obstruction after mitral valve replacement with preservation of the subvalvular apparatus. Echocardiography correctly identified the mechanism of LVOT obstruction.
In the first patient, LVOT obstruction causing direct postoperative hemodynamic deterioration was recognized as SAM of the remnants of the native anterior leaflet and subvalvular apparatus. Direct excision of these remnants resulted in complete recovery. In the second patient, LVOT obstruction was not recognized by intraoperative TEE because of acoustic shadowing of the LVOT by the mechanical prosthesis. LVOT obstruction was related to thickened interventricular septum.
These cases illustrate that the clinical course of LVOT obstruction after mitral valve replacement with preservation of the subvalvular apparatus is potentially deleterious. The clinical course may be asymptomatic and varies from an unrecognized cause with fatal outcome [6] to early recognition and surgical correction during the same operation [3]. Prevention is the most effective treatment of this complication. We recommend intraoperative echocardiographic screening for LVOT abnormalities after mitral valve replacement with preservation of the complete subvalvular apparatus. If imaging of the LVOT is hindered, epicardial echocardiography is mandatory to exclude obstruction. Furthermore, echocardiography may identify patients amenable for this surgical technique. To prevent LVOT obstruction, we do not recommend this technique in case of thickening or bulging of the interventricular septum.




