-
PDF
- Split View
-
Views
-
Cite
Cite
Shinichi Mizutani, Akihiko Usui, Toshiaki Akita, Yuichi Ueda, The value of caval division in the maze procedure with valve surgery, European Journal of Cardio-Thoracic Surgery, Volume 22, Issue 5, November 2002, Pages 822–824, https://doi.org/10.1016/S1010-7940(02)00483-9
Close - Share Icon Share
Abstract
Operative predictors for successful elimination of atrial fibrillation (AF) following the maze procedure are not yet known. We have often divided the superior vena cava (SVC) during the maze procedure, not to eliminate AF but in order to explore the mitral valve. However, in multivariate analysis of 79 patients, the division of SVC, as well as the duration of AF, was found to be the strongest predictor of AF elimination. The explanation of this observation is not clear, but denervation of the cardiac autonomic nervous system or the existence of paroxysmal AF originating from the SVC could be involved.
1 Introduction
Cox's maze procedure and its modifications are now a common surgical technique for eliminating atrial fibrillation (AF). Some predictors for successful conversion of AF to sinus rhythm have been discovered [1–3]. Many of these predictors involved the preoperative profile of the patient. However, surgery-related predictors for AF conversion have not yet been found. We have often performed division of the superior vena cava (SVC) in cases where it is difficult to explore the mitral valve. We came to suspect that patients who had undergone SVC division were likely to recover their sinus rhythm after the maze procedure. To test this hypothesis, we retrospectively evaluated the charts of patients who underwent the maze procedure concomitant with valve surgery. We discuss the procedure of SVC division and its clinical efficacy for AF conversion.
2 Surgical procedure
The patient was placed on cardiopulmonary bypass with bicaval venous drainage and arterial return involving the ascending aorta. A metal tip venous cannula was inserted directly into the SVC and both vena cava were snared. The intraatrial groove was dissected and the right sided left atrium was exposed. This dissection was extended under the SVC towards the cranial side of the left atrium so as to strip off the SVC. After aortic cross-clamping, the heart was arrested with cold blood cardioplegia. The left atrial appendage was resected, and an extended right-sided left atriotomy was made. Then the SVC was divided about 2 cm above the cavo-atrial junction in cases where it is difficult to explore the mitral valve (Fig. 1) . Cryoablation at −60°C was delivered for 90 s at the left margin of both left pulmonary venous orifices towards the left atriotomy ridge in order to isolate all four pulmonary venous orifices. Cryoablation was also directed next to the center of the posterior mitral valve annulus and the base of the excised left atrial appendage. The necessary valve surgery was then performed. In patients undergoing the modified Cox's maze III procedure, the right atrial appendage was resected and a L-shape right atriotomy was made. Atriotomy towards the inferior vena cava (IVC) in the maze III procedure was replaced by cryoablation. In patients undergoing the left atrial partial Maze procedure (LA maze), further cryoablation was delivered toward the anatomical right atrial isthmus between the tricuspid valvular annulus and the IVC.
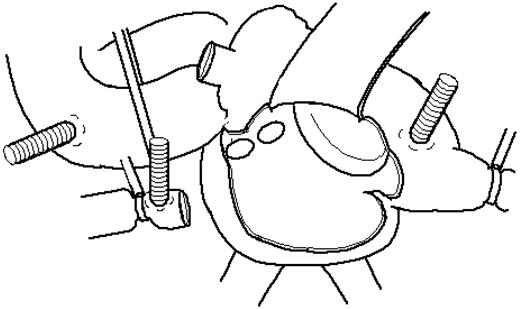
Schema of the superior vena cava (SVC) division. SVC is divided at about 2 cm above the cavo-atrial junction.
The left atriotomy was closed first, and aortic cross-clamping was removed. The right atriotomy was usually closed after declamping. Thereafter the SVC was anastomosed end to end.
3 Predictors of AF conversion
Between 1993 and 2000, 79 patients underwent AF elimination procedures, of which 32 underwent modified maze III and 47 LA maze, together with valve surgeries. A retrospective review was undertaken to assess predictors of AF elimination using univariate and multivariate unconditional logistic regression. Six months after surgery, 63 patients (80%) had ceased AF; the remaining 16 patients (20%) still showed AF.
Variables associated with cessation of AF were as follows: duration of AF, cardio-thoracic ratio, left atrial diameter (LAD), AF wave on V1 and tricuspid regurgitation (patient factors); and SVC division and Tricuspid annuloplasty (operative factors). Multivariate analysis found only two significant predictors: division of SVC and shorter duration of AF.
4 Discussion
SVC division is not a special technique in mitral valve surgery. This simple procedure provides better mitral valve exposure, especially in patients with a small left atrium or deep pericardial wall. We performed SVC division not to eliminate AF, but rather to explore the mitral valve. Of all the factors considered above, SVC division was the strongest predictor for successful conversion from AF to sinus rhythm. The duration of AF has been reported to be a predictor influencing the AF conversion rate of the maze procedure [1,3], but the clinical efficacy of SVC division for AF elimination has not been clarified.
It is assumed that SVC division is performed preferentially on patients with a smaller left atrium. A larger LAD was reported to be one of the predictors of failure to eliminate AF [1,2]. However, the present study found no statistically significant relation between SVC division and LAD. The explanation of the higher elimination rate of AF is not clear. Nevertheless it may be supposed that denervation of the cardiac autonomic nervous system, as a result of dissecting the right and cranial side of the left atrium and dividing SVC, affects AF elimination. Some reports have been made concerning denervation after the maze procedure [4–6], but no investigations exist of its effect for AF elimination. It was recently reported that partial cardiac denervation reduces the incidence of AF after coronary surgery. Furthermore, focal paroxysmal AF has been reported originating from the SVC [7,8]. Tsai reported that ectopic beats initiating paroxysmal AF can originate from the SVC. Although all the patients in the present study had chronic AF, the contribution of paroxysmal AF foci to AF elimination cannot be ignored.
We do not recommend SVC division for every case of maze procedure. However, it can provide a better surgical view for mitral valve surgery and is the strongest predictor of successful AF conversion to sinus rhythm.




