-
PDF
- Split View
-
Views
-
Cite
Cite
Riku Kato, Soh Hosoba, Masayuki Kuroda, Kenichiro Yasuda, Transcatheter mitral valve repair for a patient with double inferior vena cava: case report, European Heart Journal - Case Reports, Volume 8, Issue 5, May 2024, ytae221, https://doi.org/10.1093/ehjcr/ytae221
Close - Share Icon Share
Abstract
A transcatheter edge-to-edge repair (TEER) is disseminating gradually as a treatment for primary and secondary mitral regurgitation (MR) in patients with high surgical risk. In performing TEER, securing a safe access route is crucial. We report a case with a challenging access route due to the presence of a double inferior vena cava (IVC) and the patient’s small body habitus.
An 84-year-old female presented with congestive heart failure due to severe MR. Despite receiving optimal medical therapy, her symptoms did not improve significantly. Transcatheter edge-to-edge repair was deemed challenging due to her extremely small body habitus [height: 131 cm; body surface area: 1.17 m2] and the presence of double IVC. However, considering her inoperable risk for surgical repair, she underwent TEER after a multidisciplinary heart team discussion. The steering guide catheter (SGC) encountered resistance, but gradual advancement and use of a bougie with a large bore sheath dilator successfully delivered the SGC to the right atrium. Following the TEER, there was a significant improvement in the symptoms.
Extremely small venous system in a small patient with double IVC presented a unique technical hurdle. Transcatheter edge-to-edge repair is potentially feasible even in such a patient by cautiously applying the technique described.
Pre-operative examination for access route is essential when a transcatheter edge-to-edge repair is planned. The optimal access route must be carefully selected.
Transcatheter edge-to-edge repair can be an alternative option even for a patient with a relatively small venous system.
Introduction
Transcatheter edge-to-edge repair (TEER) has emerged as an effective treatment option for mitral regurgitation (MR) in certain patients who are at high risk for conventional surgery.1,2 The minimally invasive nature of TEER allows for its application in individuals with severe frailty. Because reliable access is needed to perform TEER safely, patients with small inferior vena cava (IVC) pose a challenge. Herein, we describe a case of a successful TEER in a small woman with double IVC. We describe technical tips to overcome such anatomical challenges.
Summary figure
Case
An 85-year-old woman was admitted to the hospital with congestive heart failure due to severe MR and pneumonia. Her medical history included chronic obstructive pulmonary disease requiring a steroid inhaler. Her dyspnoea persisted after she recovered from pneumonia with antibiotic therapy. She was then re-admitted twice for exacerbation of her heart failure regardless administration of drugs (loop diuretics, sodium-glucose co-transporter 2 inhibitor, and tolvaptan). The chest X-ray showed pulmonary congestion and right pleural effusion and the electrocardiogram demonstrated sinus rhythm. The transoesophageal echocardiogram (TEE) revealed severe degenerative MR due to posterior mitral leaflet prolapse (Figure 1), and the suitable mitral valve characteristics for TEER (mitral valve area: 2.94 cm2; length of posterior leaflet: 7.56 mm; basal mean trans-mitral gradients: 4.5 mmHg; and fossa co-aptation height: 33 mm). Mitral valve intervention was deemed necessary, but she was not considered a candidate for surgical mitral repair due to both obstructive and restrictive lung disease and advanced age. The heart team ultimately concluded she was a candidate for TEER. A pre-TEER computed tomography scan revealed no coronary artery disease but a persistent left superior vena cava (SVC) and double IVC (Figure 2; Supplementary material online, Video S1). She had a small body habitus (height: 131 cm; weight: 41.1 kg; body surface area: 1.17 m2), and the right IVC, with a diameter of 4.6 mm, was considered small for TEER device delivery. Despite these challenges, TEER was pursued since she was deemed a high surgical risk.
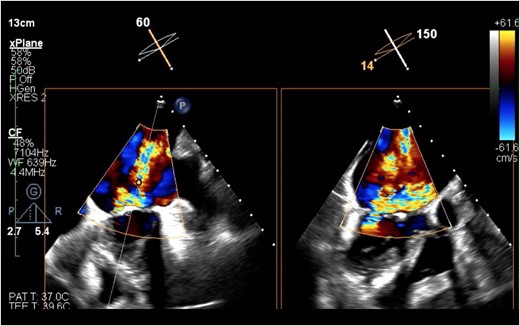
The transoesophageal echocardiography revealed severe mitral regurgitation.
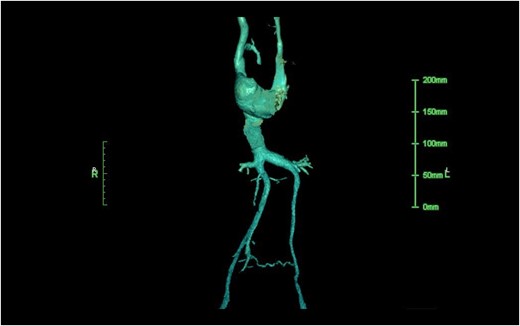
The contrasted computed tomography demonstrated the persisted left superior vena cava and the duplicated inferior vena cava. The diameter of her right inferior vena cava was 4.6 mm.
Under general anaesthesia, the right femoral vein was punctured, and the guidewire successfully advanced into the SVC. After puncturing the mid-posterior fossa ovalis, the steering guide catheter (SGC) encountered a gradual increase in resistance, which prohibited the advancement of the SGC at the mid-abdominal level. The SGC was retrieved once, and a bougie with a large bore sheath dilator (24Fr, 15 cm) was gently advanced. Venography demonstrated no injury to the venous system. After a careful bougie manoeuvre, the SGC reached the right and left atrium without significant difficulty after very slow and cautious advancement over 10 min (Figure 3). The ‘puncture-to-mitral co-aptation’ height was 41.6 mm. Using three-dimensional TEE guidance, the clip (MitraClip NT; Abbott Vascular, Menlo Park, CA, USA) was navigated into the left ventricle, capturing the A2-P2 segments and achieving an excellent reduction of MR from severe to trivial (Figure 4). The mean trans-mitral gradient was 3 mmHg, which was considered acceptable. The SGC was removed carefully. After the removal, the completion venography again demonstrated no injury (see Supplementary material online, Video S2). After TEER, the symptoms and exercise tolerance significantly improved. She was transferred to a rehabilitation facility on post-procedure Day 15 with heart failure medications.
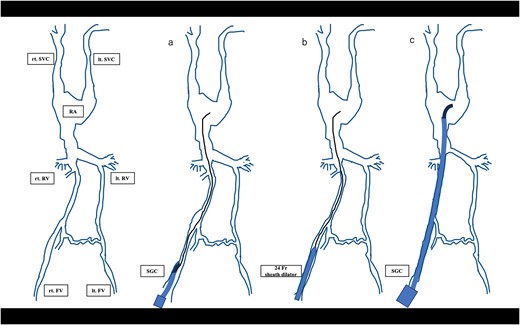
A schematic diagram of the bougie manoeuvre (rt. SVC, right superior vena cava. lt. SVC, left superior vena cava; RA, right atrium. rt. RV, right renal vein. lt. RV, left renal vein. rt. FV, right femoral vein. lt. FV, left femoral vein.).
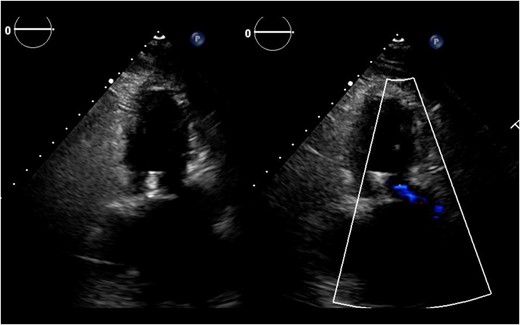
Post-operative transthoracic echocardiography revealed a significant reduction of mitral regurgitation.
Discussion
Double IVC is a very rare congenital vascular condition in which the IVCs fail to unify during the embryonic phase.3,4 The remnant left IVC drains from the abdominal organs. The right IVC remains small, as it contributes to less venous drainage. Our patient had persistent left SVC and left IVC. The right IVC had communication to the left internal iliac vein and to the left renal vein separately (Figure 2; Supplementary material online, Video S1). She had a small body habitus, and the venous system was overall small, which made the delivery of the SGC challenging. To our knowledge, there has not been a report of TEER for patients with double IVC. Despite the patient having a small venous calibre, the case suggests that TEER should remain a consideration.
The optimal approach in case the SGC cannot be advanced smoothly remains controversial. Several solutions have been described. Edupuganti et al.5 and Fam et al.6 performed TEER via the left femoral vein and trans-jugular vein because of vein obstruction. Frerker et al.7 and Tiroch et al.8 utilized the right atrium approach and pulmonary vein approach through a right mini-thoracotomy because of agenesis of the IVC. In this case, the left IVC was even smaller than the right and partially pushed by the abdominal aorta. The right-side venous approach was deemed to be preferable in this particular case. For small venous calibre, enlarging the route with a large bore sheath is practical, but extra caution is needed because abdominal or thoracic venous rupture is often a fatal complication.9 The attempt was made to enlarge the route, and very slow advancement was the key to success in our case. Once the left atrium was reached, the technical nuance of the procedure was the same as usual, including the usual steering of the system. Completion venography showed no injury to the vein.
The TEER for the case with double IVC could be possible with proper strategy and extra caution in advancing the SGC.
Lead author biography

Riku Kato has served as a Cardiovascular Surgery Fellow at Japanese Red Cross Aichi Medical Center Nagoya Daiichi Hospital since 2016. With involvement in over 500 cases of minimally invasive cardiovascular surgery, he has gained extensive experience in this specialized field. His commitment to learning spans across all areas of cardiovascular surgery.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Acknowledgements
We would like to thank the treating physicians, nurses, and clinical and laboratory staff at our centre.
Consent: Informed written patient consent has been obtained, in line with the COPE best practice guidelines, and the individual who is being reported is aware of the possible consequences of that reporting.
Funding: None declared.
Data availability
The data underlying this article are available in the article. Any additional readers’ inquiries relating to this article will be shared on reasonable request to the corresponding author.
References
Author notes
Conflict of interest: S.H. has a financial relationship with Abbott and Ethicon Inc. All other authors declared no conflict of interest.
- mitral valve insufficiency
- right atrium
- congestive heart failure
- dilators
- operative risk
- body surface area
- drug administration routes
- surgical procedures, operative
- inferior vena cava
- heart
- intravascular guiding catheters
- mitral valve repair, edge-to-edge
- bougie
- assessment of body build
- transcatheter mitral valve repair





Comments