-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroto Tamaru, Shin Takiuchi, Kasumi Ishibuchi, Satoru Otsuji, Optical frequency domain images of neointimal tissue in a self-expanding stent-graft 10 months after implantation in the superficial femoral artery: a case report, European Heart Journal - Case Reports, Volume 7, Issue 3, March 2023, ytad084, https://doi.org/10.1093/ehjcr/ytad084
Close - Share Icon Share
A 90-year-old woman was admitted with chronic limb-threatening ischaemia of the right leg. Angiography revealed chronic total occlusion (CTO) in the distal segment of the superficial femoral artery and severe stenosis in the popliteal artery (Figure 1A). Therefore, a 6 × 150 mm stent-graft (GORE VIABAHN; Gore Medical, Newark, Delaware) was deployed in the CTO lesion after balloon angioplasty (Figure 1B). Despite dual antiplatelet therapy for 10 months, she had recurrent rest pain in the right leg. Re-angiography identified significant restenosis at the stent-graft’s proximal edge (Figure 1C). Optical frequency domain imaging (OFDI) showed a double lumen appearance of the heterogeneous neointima with gradual signal attenuation at the proximal restenotic segment and speckled heterogeneous tissue at the distal segment of the stent-graft (Figure 1D–F). The restenosis at the stent margin was successfully treated with drug-coated 4- and 6-mm balloons (Figure 1G).
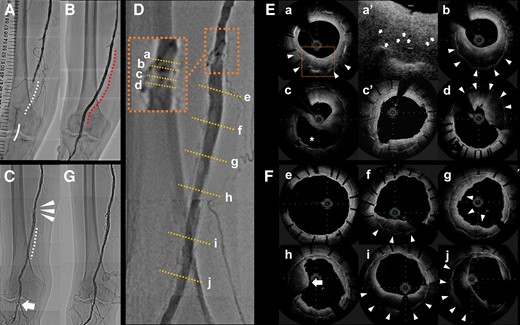
Superficial femoral artery in the lower right leg: (A–D, G) angiographies; (E, F) optimal frequency domain imaging. (A) Before treatment: chronic total occlusion in the distal segment (dotted line) and severe stenosis in the popliteal artery (solid line). (B) After stent-graft implantation (dotted line). (C) Stent-graft with significant restenosis at the edge of the proximal segment (arrowheads) and mild stenosis in the mid to distal segment (dotted line), and restenosis at the site of previous balloon angioplasty in the popliteal artery (arrow). (D) Magnification of the proximal edge (a–d) and the superficial femoral artery (e–j). (E, F) Evaluation of the morphological features of the heterogenous neointima in the restenotic stent-graft. (a) Proximal segment: gradual signal attenuation with outer and inner bands of low and high signal intensity, respectively (arrowheads). (a′) Magnification (dotted square): microvessels within the outer layer (arrows). (b) Mid-segment: greater proportion of low-signal-intensity band (arrowheads). (c) Double lumen appearance, from which the low-signal-intensity band seems to move away (asterisk), and heterogeneous neointima. (c′) Postoperative dilation of restenosis after compression of the neointima at the same cross-section of (c). (d) Distal segment: protruding mass with irregular borders and relatively strong signal attenuation with visible strut suggesting recent thrombus (arrowheads). (e) Proximal segment of the stent’s midsection: cover of the thin endothelium. (f, i) Gradual signal attenuation of heterogeneous neointima, similar to (b) but with a thinner high-intensity inner band. A gradual increase of low-signal-intensity band from the proximal to the distal segment of mild neointimal hyperplasia (arrowheads). (g) Irregular luminal margins implicating small mural thrombi on the surface (arrow). (h) Protruding mass with irregular surface and relatively strong signal attenuation, similar to (d) (arrow). (j) Heterogeneous tissue, mostly with low backscatter and speckled pattern with a visible strut (arrowheads). (G) Final image after treating the restenosis.
Heterogeneous tissue with a visible strut that exhibits gradual signal attenuation or is speckled usually indicates an organized thrombus and extracellular matrix with variably distributed smooth muscle cells; conversely, neoatherosclerotic tissue also appears heterogeneous with a highly attenuated area and an invisible strut.1 Eccentrically speckled heterogeneous tissue can change to be concentric with signal attenuation for 11 months.2 Therefore, speckled heterogeneous tissue and heterogeneous tissue with signal attenuation may indicate an organized thrombus in the early phase and the late phase, respectively. The appearance of multiple large and small channels within the stent may indicate the recanalization of the thrombus.3 Alternatively, the other potential mechanism of channel formation may be an intimal rupture and subsequent flowing out of the intra-neointimal lipid.
Optical frequency domain imaging takes high-resolution images with an axial resolution of approximately 10 μm. It is superior to intravascular ultrasound and, in our case, showed advantages in measuring dimensions but also in evaluating neointimal characteristics and microvessels based on optical signal intensity. Our report highlights the importance of patient-specific therapeutic strategies, including the prevention of distal thrombotic emboli after endovascular procedures and the duration of dual antiplatelet therapy to treat thrombotic and restenotic complications after stent-graft implantation.
Acknowledgements
We would like to thank the staff in the catheterization laboratory in Higashi Takarazuka Satoh Hospital for their excellent assistance and Editage (www.editage.com) for English language editing.
Consent: The authors confirm that written consent for submission and publication of this case report, including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Funding: None declared.
References
Author notes
Conflict of interest: None declared.




Comments