-
PDF
- Split View
-
Views
-
Cite
Cite
Yasuhiro Hamatani, Yuya Ide, Hirotoshi Watanabe, Masaharu Akao, Differential response to isometric handgrip depending on the heart failure condition in patients with functional mitral regurgitation: a case report, European Heart Journal - Case Reports, Volume 7, Issue 3, March 2023, ytac489, https://doi.org/10.1093/ehjcr/ytac489
Close - Share Icon Share
Abstract
Functional mitral regurgitation (MR) changes dynamically depending on the loading conditions and can cause acute heart failure (HF). Isometric handgrip is a simple stress test and can be performed during early phase of acute HF for the evaluation of MR.
A 70-year-old woman with a prior myocardial infarction four months before, and with history of recurrent HF admission with functional MR, who received optimal HF medications, was hospitalized for acute HF. On the following day of the admission, isometric handgrip stress echocardiography was performed to evaluate functional MR. During the handgrip, MR deteriorated from moderate to severe and the tricuspid regurgitation pressure gradient increased from 45 to 60 mmHg. After HF stabilization 2 weeks after admission, repeat handgrip stress echocardiography showed that the degree of MR did not significantly change being moderate and the tricuspid regurgitation pressure gradient was only mildly elevated from 25 to 30 mmHg. She underwent transcatheter edge-to-edge mitral repair, and thereafter she has not experienced the rehospitalization for acute HF.
Exercise stress test is recommended for the evaluation of functional MR in HF patients; however, exercise tests are difficult to perform during the early phase of acute HF. In this regard, handgrip test is an option to investigate the exacerbating impact of functional MR during early-phase acute HF. This case indicated that response to isometric handgrip can vary depending on HF condition, highlighting the importance of taking into account the timing of the handgrip procedure in patients with functional MR and HF.
Isometric handgrip stress test can be performed during early-phase acute heart failure and may be useful for the evaluation of functional mitral regurgitation (MR).
Response to isometric handgrip stress test may vary depending on the heart failure condition in patients with functional MR, indicating the importance of procedural timing of isometric handgrip test in patients with MR and heart failure.
Introduction
Severity of functional mitral regurgitation (MR) changes dynamically during exercise or depending on HF condition.1 This dynamic feature may be responsible for acute heart failure (HF) exacerbation in some patients, and exercise tests are recommended for their evaluation.2 However, exercise tests are difficult to perform during the early phase of acute HF.
The isometric handgrip is a simple and readily available stress test.3,4 Isometric handgrip can theoretically be performed during early phase and unmask the dynamic nature of functional MR among patients with acute HF.5 We herein present the case of a patient with functional MR and recurrent HF, in which early-phase handgrip stress echocardiography was useful for elucidating the cause of acute HF.
Timeline
| 1 week before 1st admission | The patient presented chest pain and is suspected to have had a myocardial infarction. |
| 1st admission | The patient presented orthopnea and hospitalized for acute heart failure (HF). Functional mitral regurgitation (MR) and 3 vessel coronary disease were noted. Percutaneous coronary intervention on these three vessels was performed, and β-blocker and mineralocorticoid receptor antagonist (MRA) were prescribed during hospitalization. |
| 2nd admission (2 weeks after discharge from the 1st hospitalization) | She was re-admitted for recurrent acute HF. After HF stabilization, isometric handgrip during right heart catheterization did not significantly increase pulmonary capillary wedge pressure. She was discharged with β-blocker, MRA and low-dose loop diuretic. |
| 3rd admission (1 month after discharge from the 2nd hospitalization) | She was again re-hospitalized for acute HF. During early-phase, isometric handgrip stress echocardiography revealed the deterioration of MR from moderate to severe and elevation of tricuspid regurgitation pressure gradient from 45 to 60 mmHg. We diagnosed that functional MR was a main underlying cause of her recurrent acute HF. Angiotensin converting enzyme inhibitor was added on top of β-blocker and MRA. |
| 1 month after discharge from the 3rd hospitalization | Transcatheter edge-to-edge mitral repair at specialized institution was performed. |
| 1-year follow-up | After the transcatheter therapy, MR remained trivial degree. Since then, she has never experienced HF hospitalization. |
| 1 week before 1st admission | The patient presented chest pain and is suspected to have had a myocardial infarction. |
| 1st admission | The patient presented orthopnea and hospitalized for acute heart failure (HF). Functional mitral regurgitation (MR) and 3 vessel coronary disease were noted. Percutaneous coronary intervention on these three vessels was performed, and β-blocker and mineralocorticoid receptor antagonist (MRA) were prescribed during hospitalization. |
| 2nd admission (2 weeks after discharge from the 1st hospitalization) | She was re-admitted for recurrent acute HF. After HF stabilization, isometric handgrip during right heart catheterization did not significantly increase pulmonary capillary wedge pressure. She was discharged with β-blocker, MRA and low-dose loop diuretic. |
| 3rd admission (1 month after discharge from the 2nd hospitalization) | She was again re-hospitalized for acute HF. During early-phase, isometric handgrip stress echocardiography revealed the deterioration of MR from moderate to severe and elevation of tricuspid regurgitation pressure gradient from 45 to 60 mmHg. We diagnosed that functional MR was a main underlying cause of her recurrent acute HF. Angiotensin converting enzyme inhibitor was added on top of β-blocker and MRA. |
| 1 month after discharge from the 3rd hospitalization | Transcatheter edge-to-edge mitral repair at specialized institution was performed. |
| 1-year follow-up | After the transcatheter therapy, MR remained trivial degree. Since then, she has never experienced HF hospitalization. |
| 1 week before 1st admission | The patient presented chest pain and is suspected to have had a myocardial infarction. |
| 1st admission | The patient presented orthopnea and hospitalized for acute heart failure (HF). Functional mitral regurgitation (MR) and 3 vessel coronary disease were noted. Percutaneous coronary intervention on these three vessels was performed, and β-blocker and mineralocorticoid receptor antagonist (MRA) were prescribed during hospitalization. |
| 2nd admission (2 weeks after discharge from the 1st hospitalization) | She was re-admitted for recurrent acute HF. After HF stabilization, isometric handgrip during right heart catheterization did not significantly increase pulmonary capillary wedge pressure. She was discharged with β-blocker, MRA and low-dose loop diuretic. |
| 3rd admission (1 month after discharge from the 2nd hospitalization) | She was again re-hospitalized for acute HF. During early-phase, isometric handgrip stress echocardiography revealed the deterioration of MR from moderate to severe and elevation of tricuspid regurgitation pressure gradient from 45 to 60 mmHg. We diagnosed that functional MR was a main underlying cause of her recurrent acute HF. Angiotensin converting enzyme inhibitor was added on top of β-blocker and MRA. |
| 1 month after discharge from the 3rd hospitalization | Transcatheter edge-to-edge mitral repair at specialized institution was performed. |
| 1-year follow-up | After the transcatheter therapy, MR remained trivial degree. Since then, she has never experienced HF hospitalization. |
| 1 week before 1st admission | The patient presented chest pain and is suspected to have had a myocardial infarction. |
| 1st admission | The patient presented orthopnea and hospitalized for acute heart failure (HF). Functional mitral regurgitation (MR) and 3 vessel coronary disease were noted. Percutaneous coronary intervention on these three vessels was performed, and β-blocker and mineralocorticoid receptor antagonist (MRA) were prescribed during hospitalization. |
| 2nd admission (2 weeks after discharge from the 1st hospitalization) | She was re-admitted for recurrent acute HF. After HF stabilization, isometric handgrip during right heart catheterization did not significantly increase pulmonary capillary wedge pressure. She was discharged with β-blocker, MRA and low-dose loop diuretic. |
| 3rd admission (1 month after discharge from the 2nd hospitalization) | She was again re-hospitalized for acute HF. During early-phase, isometric handgrip stress echocardiography revealed the deterioration of MR from moderate to severe and elevation of tricuspid regurgitation pressure gradient from 45 to 60 mmHg. We diagnosed that functional MR was a main underlying cause of her recurrent acute HF. Angiotensin converting enzyme inhibitor was added on top of β-blocker and MRA. |
| 1 month after discharge from the 3rd hospitalization | Transcatheter edge-to-edge mitral repair at specialized institution was performed. |
| 1-year follow-up | After the transcatheter therapy, MR remained trivial degree. Since then, she has never experienced HF hospitalization. |
Case presentation
A 70-year-old woman was admitted to our hospital with the diagnosis of acute HF (1st hospitalization). She had a history of hypertension and diabetes mellitus. Approximately one week previously, she experienced chest pains. Thereafter, exertional dyspnoea appeared, and she was transferred to our hospital. On arrival, blood pressure was 170/80 mmHg. Auscultation revealed bilateral coarse crackle and systolic murmur at apex. Juglar vein dilation and slight pitting oedema on bilateral lower extremities were noted. Chest radiography revealed pulmonary congestion (Figure 1A). A 12-lead electrocardiogram showed ST-segment elevation with Q wave at the lateral leads (Figure 1B). N-terminal pro B-type natriuretic peptide was elevated at 4528 pg/mL (normal range: <125 pg/mL). She was diagnosed with myocardial infarction and acute HF. Transthoracic echocardiography, performed after the initiation of HF therapies, revealed a reduced left ventricular ejection fraction (LVEF) of 26% with predominant posterior asynergy (Figure 1C, see Supplementary material online, Video S1). Moderate functional MR due to leaflet tethering was noted (Figure 1D, see Supplementary material online, Video S2). After HF stabilization, coronary angiography demonstrated three vessel disease (Figure 1E, F). We performed percutaneous coronary intervention on these three vessels. We prescribed bisoprolol 1.25 mg, spironolactone 25 mg, and furosemide 20 mg during hospitalization. Renin–angiotensin system inhibitor was unable to be prescribed due to hypotension after HF stabilization. Thereafter, she was transferred to another hospital to continue rehabilitation.
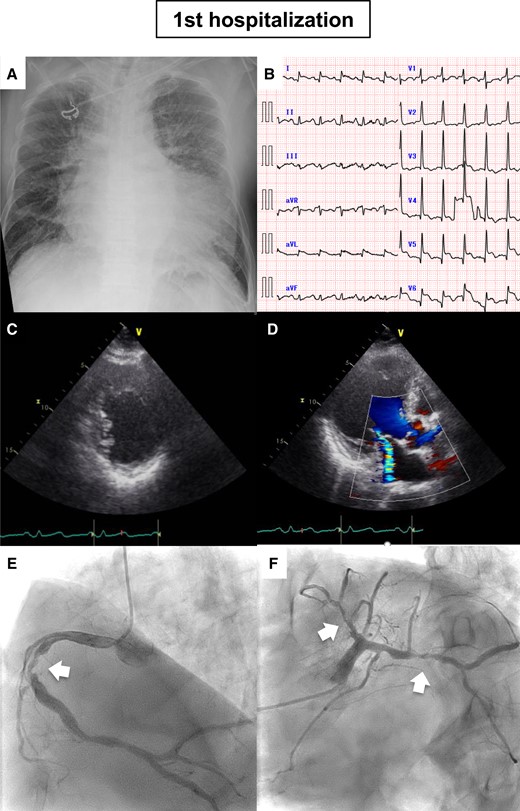
Imaging data on 1st admission. (A) Chest radiography. (B) Electrocardiography. (C) Parasternal short-axis view. Posterior asynergy was noted. (D) Apical three-chamber view. (E) Right coronary artery, (F) left coronary artery. White arrows indicate the significant stenosis.
Two weeks after hospital transfer, she suddenly experienced dyspnoea and re-transferred to our hospital (2nd hospitalization). Systolic blood pressure was elevated at 147 mmHg. Pulmonary oedema on chest radiography and elevated natriuretic peptide levels were noted. Transthoracic echocardiography, performed after HF treatment was initiated, showed reduced LVEF of 35% and moderate functional MR. After the stabilization of HF, we performed right heart catheterization with isometric handgrip stress test. At rest, pulmonary capillary wedge pressure (PCWP) and pulmonary artery pressure were normal (Figure 2A, B). During isometric handgrip for about 2 min, blood pressure increased, but PCWP and pulmonary artery pressure were within normal range albeit mildly increased (Figure 2C, D). At that time, we considered invasive procedures for MR as unnecessary. Neither angiotensin receptor-neprilysin inhibitors nor sodium glucose co-transporter 2 inhibitors had been approved for HF in Japan at that time. She was discharged with bisoprolol 1.25 mg, spironolactone 25 mg, and furosemide 20 mg.
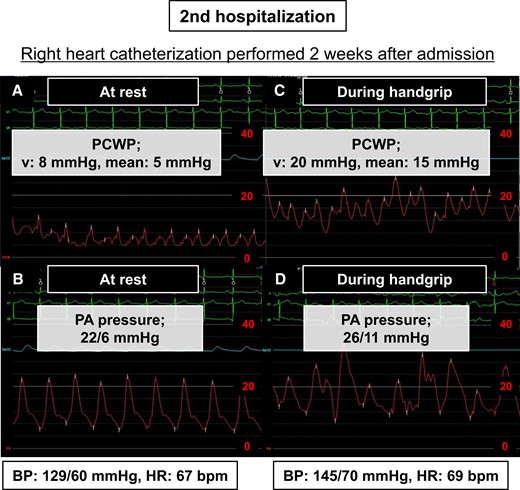
Data of right heart catheterization performed 2 weeks after 2nd admission. (A) PCWP at rest, (B) PA pressure at rest, (C) PCWP during handgrip, (D) PA pressure during handgrip. BP, blood pressure; HR, heart rate; PA, pulmonary artery; PCWP, pulmonary artery wedge pressure.
One month later, she suffered sudden-onset dyspnoea and rushed to our hospital (3rd hospitalization). On arrival, she was drowsy and arterial blood gas revealed respiratory and metabolic acidosis with pH: 6.9. Blood pressure was unmeasurable. Her weight had increased by 1 kg compared with the stable condition during 2nd hospitalization. Chest radiography showed a butterfly shadow, resulting in the diagnosis of recurrent acute HF. Focused echocardiography at emergency department described reduced LVEF and more than moderate degree MR. She was admitted to our intensive care unit and treated with non-invasive positive pressure ventilation, vasodilator and diuretics. On the following day, her condition was improving, and we performed bedside transthoracic echocardiography with isometric handgrip stress test. At rest, we observed a moderate to severe degree of functional MR and an elevated tricuspid regurgitation pressure gradient (TRPG) of 45 mmHg (Figure 3A, see Supplementary material online, Video S3). After resting measurements were obtained, sustained maximum-effort handgrip grasping was maintained for about 2 min using hand dynamometer in a left lateral decubitus position. Then, MR deteriorated to a severe degree and the TRPG was further elevated to 60 mmHg (Figure 3B, see Supplementary material online, Video S4). We diagnosed that functional MR was a main underlying cause of her recurrent acute HF. Two weeks later, transthoracic echocardiography with isometric handgrip was performed after the HF condition stabilized with dosing-up oral loop diuretic (furosemide 40 mg) and adding enalapril 5 mg on top of bisoprolol 1.25 mg and spironolactone 25 mg. Functional MR was moderate and the TRPG was 25 mmHg at rest (Figure 3C, see Supplementary material online, Video S5). During handgrip test, the degree of MR did not significantly change and the TRPG was only mildly elevated to 30 mmHg (Figure 3D, see Supplementary material online, Video S6).
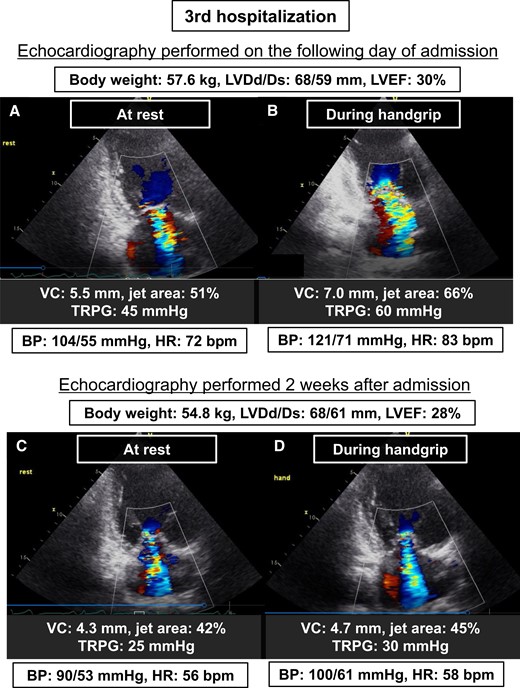
Transthoracic echocardiography at rest and during isometric handgrip, performed on the following day of the 3rd admission and after stabilizing HF condition. (A) At rest on the following day of the 3rd admission, (B) during handgrip on the following day of the 3rd admission, (C) at rest after stabilizing HF condition, (D) during handgrip after stabilizing HF condition. BP, blood pressure; HR, heart rate; LVDd/Ds, left ventricular end-diastolic diameter/end-systolic diameter; LVEF, left ventricular ejection fraction; TRPG, tricuspid regurgitation pressure gradient; VC, vena contracta width.
Invasive treatment of functional MR was discussed comprehensively within our heart team. She experienced HF exacerbation during hospitalization (2nd admission) and even with slight increase in body weight (3rd admission, which was a lethal HF exacerbation) under optimal medical therapy. Cardiac resynchronization therapy was not indicated considering the narrow QRS duration on electrocardiogram. Thus, we decided to proceed with transcatheter edge-to-edge repair. One month after discharge from 3rd hospitalization, one clip was deployed at the mid position of the mitral leaflet, resulting in the MR becoming trivial (Figure 4A). The patient’s post-operative course was uneventful. The 1-year follow-up transthoracic echocardiography showed trivial MR without significant mitral stenosis (Figure 4B, see Supplementary material online, Video S7). Since transcatheter mitral repair, she experienced no additional hospitalization for acute HF.

(A) Fluoroscopic image during the transcatheter edge-to-edge mitral repair, (B) transthoracic echocardiography at 1-year follow-up after the transcatheter repair.
Discussion
In this case, early-phase handgrip stress echocardiography provided an important clue for elucidating the cause of recurrent acute HF. MR is underrecognized but is associated with incident HF in patients with coronary artery disease.6 We previously reported the utility of handgrip stress tests among ambulatory patients with moderate functional MR and exertional dyspnoea.4 Of note, isometric handgrip is considered to be less physiological than the exercise stress tests such as ergometer or treadmill,7 which increases not only blood pressure and heart rate but also venous return and are the gold standard stress procedures for dynamic MR evaluation.8 However, these tests are difficult to perform in patients in early-phase acute HF.2 In this regard, isometric handgrip stress test can be easily performed at the bedside at almost anytime and anywhere, as shown in our case. We believe that this procedure is an attractive option to investigate the exacerbating impact of functional MR during early-phase acute HF.
Previous report demonstrated the utility of isometric handgrip on stable HF condition for the evaluation of functional MR in patients with a history of acute pulmonary oedema.9 Notably, our case indicated that response to isometric handgrip stress test can vary depending on the HF condition. During early phase after admission, MR deteriorated from moderate to severe and TRPG increased from 45 to 60 mmHg by the isometric handgrip. Meanwhile, MR did not significantly deviate from moderate and TRPG only mildly increased from 25 to 30 mmHg after the HF stabilized. This was retrospectively confirmed by the right heart catheterization data during the 2nd hospitalization. Hence, we cannot deny the possibility of MR deterioration during early phase even when isometric handgrip on stable condition does not increase the severity of MR. Although speculative, difference in preload and afterload might have affected the differential response to isometric handgrip between early phase and after HF stabilization. In that sense, increasing preload by leg raising or leg positive pressure during isometric handgrip could be another option to unmask the dynamic nature of MR.10 Our case highlights the importance of timing and condition in performing, and in the interpretation of isometric handgrip stress test in patients with functional MR and HF.
Conclusions
Isometric handgrip can be performed during early-phase acute HF to evaluate functional MR. Responses to isometric handgrip vary depending on HF condition, and the timing and condition of the isometric handgrip must be considered in patients with functional MR and HF.
Lead author biography
 Yasuhiro Hamatani graduated from Kyoto University and started his career in Kyoto Medical Centre. Thereafter, he trained at National Cardiovascular Centre. Currently, he worked at Kyoto Medical Centre as a staff cardiologist. His research interest is heart failure, cardiomyopathy and echocardiography.
Yasuhiro Hamatani graduated from Kyoto University and started his career in Kyoto Medical Centre. Thereafter, he trained at National Cardiovascular Centre. Currently, he worked at Kyoto Medical Centre as a staff cardiologist. His research interest is heart failure, cardiomyopathy and echocardiography.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Acknowledgements
We sincerely appreciate the efforts of medical staff of National Hospital Organization Kyoto Medical Centre and Kyoto University Hospital.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Funding: This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosures
The authors have reported that they have no conflicts of interest to disclose.
Data availability
Data available on request. The data underlying this article will be shared on reasonable request to the corresponding author.
References
Author notes
Conflict of interest: None declared.




Comments