-
PDF
- Split View
-
Views
-
Cite
Cite
Takeshi Kitai, Kitae Kim, Optimal stress testing for dynamic functional mitral regurgitation in patients with acute decompensated heart failure, European Heart Journal - Case Reports, Volume 7, Issue 3, March 2023, ytad121, https://doi.org/10.1093/ehjcr/ytad121
Close - Share Icon Share
This editorial refers to ‘Differential response to isometric handgrip depending on the heart failure condition in patients with functional mitral regurgitation: a case report’, by Y. Hamatani et al., https://doi.org/10.1093/ehjcre/ytac489.
Functional mitral regurgitation (MR) in ischaemic or non-ischaemic heart disease results from an imbalance between increased tethering forces (mitral annular dilation and papillary muscle displacement) and decreased closing forces [reduced left ventricular (LV) contractility with structurally normal mitral valve].1 Functional MR has a dynamic nature, and the severity of MR changes dramatically depending on the loading condition that modulates the LV volume and systolic function.2 Exercise Doppler echocardiography can provide useful information in patients with acute pulmonary oedema without an apparent exacerbating factor or in patients with exertional dyspnoea that cannot be explained by the severity of MR at rest.3
In the current issue of European Heart Journal Case Reports, Hamatani et al. described a 70-year-old woman with dynamic functional MR with repetitive acute heart failure (AHF).4 She was hospitalized for AHF complicated by a recent myocardial infarction and was treated with percutaneous coronary intervention for three-vessel disease and guideline-directed medical therapy. Two weeks after discharge from the index hospitalization, she was readmitted for acute pulmonary oedema with mildly elevated systolic blood pressure. After heart failure stabilization, right heart catheterization using isometric handgrip stress showed a modest increase in the mean pulmonary capillary wedge pressure (15 mmHg) with a significant increase in the V-wave (20 mmHg). Dynamic MR assessment with stress echocardiography was not performed at that time. The authors estimated that MR was unlikely to contribute to the exacerbation of HF. However, she was readmitted for severe AHF with a modest increase in body weight 1 month after discharge from the second HF hospitalization. Isometric handgrip stress echocardiography in the early phase of decompensated HF revealed MR deterioration and marked elevation of systolic pulmonary artery pressure estimated by tricuspid regurgitation pressure gradient. She underwent transcatheter edge-to-edge mitral valve repair (TEER) and had never experienced hospitalization for HF after transcatheter therapy.
That case report presents two important findings. First, because the response to exercise stress testing may differ depending on the time course of the decongestion therapy, the timing of stress testing for the assessment of functional MR and AHF should be considered. Second, patients with moderate functional MR at rest that progresses to severe MR during the exercise stress test, which is called dynamic severe MR, may benefit from TEER. To properly understand these findings, an overview of the differences in haemodynamic effects, advantages and disadvantages of various types of stress tests, and mechanism, prognosis, and management of exercise-induced functional MR is warranted and provided herein.
Type of stress echocardiography for functional mitral regurgitation
The responses of the left ventricle during exercise differ according to the type of exercise and can be classified into isotonic (dynamic) and isometric (static) (Figure 1). Isotonic exercise is characterized by the contraction of multiple muscle groups and joint movements. In such exercises, a significant reduction in systemic vascular resistance is caused by vasodilation of the muscular vasculature, and a considerable increase in venous return occurs due to skeletal muscle pump function. In healthy individuals, decreased afterload, increased preload, and increased LV contractility resulted in a significant increase in stroke volume. The LV end-diastolic volume did not increase significantly, whereas the LV end-systolic volume decreased, resulting in an increased stroke volume and LV ejection fraction.5 In patients with ischaemic or non-ischaemic cardiomyopathy, volume loading during isometric exercise was associated with increases in LV end-diastolic and systolic volumes without changing the LV ejection fraction, especially in ischaemic cardiomyopathy.6 In contrast, isometric exercises are associated with no decrease or even an increase in systemic vascular resistance. In healthy individuals, the stroke volume, LV end-diastolic volume, and systolic volume remained almost unchanged during isometric exercise stress.7 In patients with coronary artery disease and/or heart failure, arterial pressure, systemic vascular resistance, myocardial oxygen consumption, and LV end-diastolic pressure increased during handgrip stress, whereas the LV stroke work index slightly increased or even decreased with the progression of heart failure symptoms.8
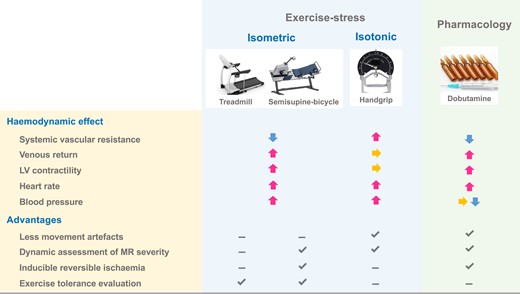
Comparisons of haemodynamic responses and advantages/disadvantages among various types of stress testing.
The various types of stress echocardiography for the assessment of functional MR are summarised in Figure 1. Running on a treadmill and cycling on a bicycle ergometer are isotonic exercises, whereas handgrip is isometric. Exercise using a treadmill does not allow image acquisition at the intermediate/peak level, and there are changes in loading conditions related to post-exercise postural change, whereas semisupine exercise using a bicycle ergometer and tilted table allows continuous and dynamic assessment of LV function, MR severity, and pulmonary hypertension.3,9 Inducible reversible ischaemia can also be detected.
In contrast, handgrip is an isotonic exercise. Five-minute sustained handgrip at 50% of the maximum voluntary contraction is a commonly used protocol.10 Handgrip stress echocardiography is a simple, convenient procedure that can be performed even in frail elderly patients who cannot undergo treadmill or cycle exercises. Handgrip stress exercise can also avoid many technical challenges associated with treadmill or cycle exercise including poor image quality due to respiratory and movement artefacts. Dobutamine, an agonist for mainly β1-adrenergic receptors of the myocardium, increases LV contractility and heart rate and is not used instead of exercise for the assessment of dynamic functional MR because of its non-physiological effects on LV and MR severity, except for the purpose of detecting LV contractile reserve and inducible ischaemia.11 Activation of β2-adrenergic receptors results in a decrease in systolic blood pressure through decreased systolic vascular resistance. Venous return increases with dobutamine to a lesser extent than with isotonic exercise.
Mechanism, prognosis, and management of exercise-induced functional mitral regurgitation
The mechanism of functional MR deterioration during exercise has also been investigated. Although MR deterioration during exercise was not associated with changes in global LV function, it was associated with changes in LV local remodelling, including papillary muscle displacement and mitral valve deformation, including the coaptation distance, tenting area, and mitral annular area.12,13 Recently, three-dimensional transoesophageal echocardiography has revealed that the tenting height and volume significantly increased during handgrip exercise. Additionally, the tenting height and three-dimensional vena contracta area (3D VCA) at rest were independent predictors of the change in 3D VCA during handgrip.14 Thus, mitral valve tenting along with papillary muscle displacement, rather than a change in actual LV volume during exercise, is thought to be a more important mechanism of exercise-induced functional MR.
The impact of exercise-induced, dynamic, functional MR on prognosis or functional capacity has also been investigated, mainly using a semisupine bicycle ergometer. Lancellotti et al. demonstrated that an increase in effective regurgitant orifice (ERO) by ≥0.13 cm2 was an independent predictor of cardiac death in patients with previous myocardial infarction and LV dysfunction.15 In contrast, patients with decreased ERO during exercise had better outcomes than their counterparts.16 Exercise-induced pulmonary hypertension (systolic pulmonary artery pressure >60 mmHg) was independently associated with an increased risk of cardiac events in patients with functional MR.17 Deterioration of MR severity during exercise causes inhibition of the expected increase in forward stroke volume and elevated left atrial pressure, leading to poor exercise capacity. A study using cardiopulmonary exercise testing demonstrated that patients with exercise-induced MR (an increase in ERO by ≥0.13 cm2) had lower peak oxygen uptake (peak VO2), and the change in ERO was the strongest predictor of peak VO2 in a mixed cohort with ischaemic and dilated cardiomyopathy.18 A recent study showed prognostic differences between semisupine ergometer and handgrip exercises for functional MR. Kagiyama et al.19 reported that the change in global longitudinal strain (GLS), but not in MR during ergometer exercise, was associated with adverse events, whereas neither changes in GLS nor in MR during handgrip exercise were prognostic. Further studies are needed to elucidate the mechanism of the different prognostic impacts of semisupine ergometer and handgrip exercises.
In contrast to reports of the mechanism and prognostic or functional impact, data regarding mitral valve intervention for dynamic functional MR are scarce. Previous studies suggest that mitral TEER may be effective in improving symptoms and preventing adverse cardiac events in patients with dynamically fluctuating functional MR (Table 1); however, further studies are needed to elucidate the impact of mitral TEER on exercise haemodynamics and clinical outcomes.
| First author, year . | N . | Ischaemic MR . | Type of stress . | Findings . |
|---|---|---|---|---|
| Geometric determinants of increasing MR | ||||
| Lancellotti et al., 200313 | 70 | 100% | Semisupine bicycle | Changes in tenting area, mitral annular area, and wall motion score index were the independent predictors of ERO changes. |
| Giga et al., 200512 | 40 | 100% | Treadmill | Changes in tenting area and coaptation distance were the independent predictors of ERO changes. |
| Harada et al., 202114 | 40 (FMR) 36 (primary MR) | Not shown | Handgrip | In functional MR, tenting height and three-dimensional vena contracta area (3D VCA) at rest were independent predictors of the change of 3D VCA. |
| Prognostic and functional impact | ||||
| Lancellotti et al., 200313 | 98 | 100% | Semisupine bicycle | An increase in ERO by ≥13 mm2 was the independent predictor of cardiac death. |
| Lancellotti et al., 2005 | 161 | 100% | Semisupine bicycle | An increase in ERO by ≥13 mm2 and transtricuspid pressure gradient were the independent predictors of cardiac death. Only 1 of the 18 patients with a decrease in ERO during exercise died during follow-up. |
| Yamano et al., 2008 | 32 | 0% | Semisupine bicycle | Functional MR did not newly appear in nine subjects without MR at rest. Twenty-three subjects with functional MR at rest all showed exacerbations of MR. An increase in ERO was the strongest determinant of exercise duration. |
| Izumo et al., 2011 | 30 | 40% | Semisupine bicycle | Patients with exercise-induced MR (an increase in ERO by ≥13 mm2) had lower peak oxygen uptake (peak VO2). Change in ERO was the strongest predictor of peak VO2. |
| Lancellotti et al., 201516 | 159 | 81% | Semisupine bicycle | Exercise-induced PH (systolic pulmonary artery pressure >60 mmHg) was the independent predictor of cardiac event. |
| Kagiyama et al., 202119 | 53 | 45% | Comparison between semisupine bicycle and handgrip | The change in GLS but not in MR during ergometer exercise was associated with adverse events. Neither changes in GLS nor in MR during handgrip exercise were prognostic. |
| Intervention for exercise-induced secondary MR | ||||
| Chan et al., 2012 | 34 (CABG + MV repair) 39 (CABG only) | 100% | Not shown | Patients with CABG + MV repair (mean ERO at rest: 0.21 cm2 and at exercise: 0.24 cm2) showed a better improvement in exercise capacity (peak VO2: 18.1 vs. 15.9 mL/kg/min) than those in isolated CABG (mean ERO at rest: 0.18 cm2 and at exercise: 0.20 cm2). |
| Curio et al., 2020 | 55 (moderate MR at rest progressing to severe during exercise) 163 (severe MR at rest) | 62% | Handgrip | Patients with severe MR at rest had worse clinical outcomes. Residual MR after transcatheter mitral valve repair was worse in patients with severe MR at rest. A reduction of proportion of patients with heart failure hospitalization after intervention was observed in both groups. |
| Izumo et al., 202118 | 46 | 32% | Semisupine bicycle | Patients with exercise-induced secondary MR (an increase in ERO by ≥0.13 cm2) who underwent transcatheter mitral valve repair (mean ERO at rest: 0.26 cm2) had better functional capacity and lower risk of composite of death or heart failure than those who had medical therapy. |
| Others | ||||
| Lancellotti et al., 2004 | 28 (acute pulmonary oedema) 46 (control) | 100% | Semisupine bicycle | Changes in ERO, transtricuspid pressure gradient, and LVEF were independently associated with a history of recent pulmonary oedema. |
| First author, year . | N . | Ischaemic MR . | Type of stress . | Findings . |
|---|---|---|---|---|
| Geometric determinants of increasing MR | ||||
| Lancellotti et al., 200313 | 70 | 100% | Semisupine bicycle | Changes in tenting area, mitral annular area, and wall motion score index were the independent predictors of ERO changes. |
| Giga et al., 200512 | 40 | 100% | Treadmill | Changes in tenting area and coaptation distance were the independent predictors of ERO changes. |
| Harada et al., 202114 | 40 (FMR) 36 (primary MR) | Not shown | Handgrip | In functional MR, tenting height and three-dimensional vena contracta area (3D VCA) at rest were independent predictors of the change of 3D VCA. |
| Prognostic and functional impact | ||||
| Lancellotti et al., 200313 | 98 | 100% | Semisupine bicycle | An increase in ERO by ≥13 mm2 was the independent predictor of cardiac death. |
| Lancellotti et al., 2005 | 161 | 100% | Semisupine bicycle | An increase in ERO by ≥13 mm2 and transtricuspid pressure gradient were the independent predictors of cardiac death. Only 1 of the 18 patients with a decrease in ERO during exercise died during follow-up. |
| Yamano et al., 2008 | 32 | 0% | Semisupine bicycle | Functional MR did not newly appear in nine subjects without MR at rest. Twenty-three subjects with functional MR at rest all showed exacerbations of MR. An increase in ERO was the strongest determinant of exercise duration. |
| Izumo et al., 2011 | 30 | 40% | Semisupine bicycle | Patients with exercise-induced MR (an increase in ERO by ≥13 mm2) had lower peak oxygen uptake (peak VO2). Change in ERO was the strongest predictor of peak VO2. |
| Lancellotti et al., 201516 | 159 | 81% | Semisupine bicycle | Exercise-induced PH (systolic pulmonary artery pressure >60 mmHg) was the independent predictor of cardiac event. |
| Kagiyama et al., 202119 | 53 | 45% | Comparison between semisupine bicycle and handgrip | The change in GLS but not in MR during ergometer exercise was associated with adverse events. Neither changes in GLS nor in MR during handgrip exercise were prognostic. |
| Intervention for exercise-induced secondary MR | ||||
| Chan et al., 2012 | 34 (CABG + MV repair) 39 (CABG only) | 100% | Not shown | Patients with CABG + MV repair (mean ERO at rest: 0.21 cm2 and at exercise: 0.24 cm2) showed a better improvement in exercise capacity (peak VO2: 18.1 vs. 15.9 mL/kg/min) than those in isolated CABG (mean ERO at rest: 0.18 cm2 and at exercise: 0.20 cm2). |
| Curio et al., 2020 | 55 (moderate MR at rest progressing to severe during exercise) 163 (severe MR at rest) | 62% | Handgrip | Patients with severe MR at rest had worse clinical outcomes. Residual MR after transcatheter mitral valve repair was worse in patients with severe MR at rest. A reduction of proportion of patients with heart failure hospitalization after intervention was observed in both groups. |
| Izumo et al., 202118 | 46 | 32% | Semisupine bicycle | Patients with exercise-induced secondary MR (an increase in ERO by ≥0.13 cm2) who underwent transcatheter mitral valve repair (mean ERO at rest: 0.26 cm2) had better functional capacity and lower risk of composite of death or heart failure than those who had medical therapy. |
| Others | ||||
| Lancellotti et al., 2004 | 28 (acute pulmonary oedema) 46 (control) | 100% | Semisupine bicycle | Changes in ERO, transtricuspid pressure gradient, and LVEF were independently associated with a history of recent pulmonary oedema. |
MR, mitral regurgitation; CABG, coronary artery bypass grafting; ERO, effective regurgitant orifice; LVEF, left ventricular ejection fraction; MV, mitral valve; GLS, global longitudinal strain; PH, pulmonary hypertension.
| First author, year . | N . | Ischaemic MR . | Type of stress . | Findings . |
|---|---|---|---|---|
| Geometric determinants of increasing MR | ||||
| Lancellotti et al., 200313 | 70 | 100% | Semisupine bicycle | Changes in tenting area, mitral annular area, and wall motion score index were the independent predictors of ERO changes. |
| Giga et al., 200512 | 40 | 100% | Treadmill | Changes in tenting area and coaptation distance were the independent predictors of ERO changes. |
| Harada et al., 202114 | 40 (FMR) 36 (primary MR) | Not shown | Handgrip | In functional MR, tenting height and three-dimensional vena contracta area (3D VCA) at rest were independent predictors of the change of 3D VCA. |
| Prognostic and functional impact | ||||
| Lancellotti et al., 200313 | 98 | 100% | Semisupine bicycle | An increase in ERO by ≥13 mm2 was the independent predictor of cardiac death. |
| Lancellotti et al., 2005 | 161 | 100% | Semisupine bicycle | An increase in ERO by ≥13 mm2 and transtricuspid pressure gradient were the independent predictors of cardiac death. Only 1 of the 18 patients with a decrease in ERO during exercise died during follow-up. |
| Yamano et al., 2008 | 32 | 0% | Semisupine bicycle | Functional MR did not newly appear in nine subjects without MR at rest. Twenty-three subjects with functional MR at rest all showed exacerbations of MR. An increase in ERO was the strongest determinant of exercise duration. |
| Izumo et al., 2011 | 30 | 40% | Semisupine bicycle | Patients with exercise-induced MR (an increase in ERO by ≥13 mm2) had lower peak oxygen uptake (peak VO2). Change in ERO was the strongest predictor of peak VO2. |
| Lancellotti et al., 201516 | 159 | 81% | Semisupine bicycle | Exercise-induced PH (systolic pulmonary artery pressure >60 mmHg) was the independent predictor of cardiac event. |
| Kagiyama et al., 202119 | 53 | 45% | Comparison between semisupine bicycle and handgrip | The change in GLS but not in MR during ergometer exercise was associated with adverse events. Neither changes in GLS nor in MR during handgrip exercise were prognostic. |
| Intervention for exercise-induced secondary MR | ||||
| Chan et al., 2012 | 34 (CABG + MV repair) 39 (CABG only) | 100% | Not shown | Patients with CABG + MV repair (mean ERO at rest: 0.21 cm2 and at exercise: 0.24 cm2) showed a better improvement in exercise capacity (peak VO2: 18.1 vs. 15.9 mL/kg/min) than those in isolated CABG (mean ERO at rest: 0.18 cm2 and at exercise: 0.20 cm2). |
| Curio et al., 2020 | 55 (moderate MR at rest progressing to severe during exercise) 163 (severe MR at rest) | 62% | Handgrip | Patients with severe MR at rest had worse clinical outcomes. Residual MR after transcatheter mitral valve repair was worse in patients with severe MR at rest. A reduction of proportion of patients with heart failure hospitalization after intervention was observed in both groups. |
| Izumo et al., 202118 | 46 | 32% | Semisupine bicycle | Patients with exercise-induced secondary MR (an increase in ERO by ≥0.13 cm2) who underwent transcatheter mitral valve repair (mean ERO at rest: 0.26 cm2) had better functional capacity and lower risk of composite of death or heart failure than those who had medical therapy. |
| Others | ||||
| Lancellotti et al., 2004 | 28 (acute pulmonary oedema) 46 (control) | 100% | Semisupine bicycle | Changes in ERO, transtricuspid pressure gradient, and LVEF were independently associated with a history of recent pulmonary oedema. |
| First author, year . | N . | Ischaemic MR . | Type of stress . | Findings . |
|---|---|---|---|---|
| Geometric determinants of increasing MR | ||||
| Lancellotti et al., 200313 | 70 | 100% | Semisupine bicycle | Changes in tenting area, mitral annular area, and wall motion score index were the independent predictors of ERO changes. |
| Giga et al., 200512 | 40 | 100% | Treadmill | Changes in tenting area and coaptation distance were the independent predictors of ERO changes. |
| Harada et al., 202114 | 40 (FMR) 36 (primary MR) | Not shown | Handgrip | In functional MR, tenting height and three-dimensional vena contracta area (3D VCA) at rest were independent predictors of the change of 3D VCA. |
| Prognostic and functional impact | ||||
| Lancellotti et al., 200313 | 98 | 100% | Semisupine bicycle | An increase in ERO by ≥13 mm2 was the independent predictor of cardiac death. |
| Lancellotti et al., 2005 | 161 | 100% | Semisupine bicycle | An increase in ERO by ≥13 mm2 and transtricuspid pressure gradient were the independent predictors of cardiac death. Only 1 of the 18 patients with a decrease in ERO during exercise died during follow-up. |
| Yamano et al., 2008 | 32 | 0% | Semisupine bicycle | Functional MR did not newly appear in nine subjects without MR at rest. Twenty-three subjects with functional MR at rest all showed exacerbations of MR. An increase in ERO was the strongest determinant of exercise duration. |
| Izumo et al., 2011 | 30 | 40% | Semisupine bicycle | Patients with exercise-induced MR (an increase in ERO by ≥13 mm2) had lower peak oxygen uptake (peak VO2). Change in ERO was the strongest predictor of peak VO2. |
| Lancellotti et al., 201516 | 159 | 81% | Semisupine bicycle | Exercise-induced PH (systolic pulmonary artery pressure >60 mmHg) was the independent predictor of cardiac event. |
| Kagiyama et al., 202119 | 53 | 45% | Comparison between semisupine bicycle and handgrip | The change in GLS but not in MR during ergometer exercise was associated with adverse events. Neither changes in GLS nor in MR during handgrip exercise were prognostic. |
| Intervention for exercise-induced secondary MR | ||||
| Chan et al., 2012 | 34 (CABG + MV repair) 39 (CABG only) | 100% | Not shown | Patients with CABG + MV repair (mean ERO at rest: 0.21 cm2 and at exercise: 0.24 cm2) showed a better improvement in exercise capacity (peak VO2: 18.1 vs. 15.9 mL/kg/min) than those in isolated CABG (mean ERO at rest: 0.18 cm2 and at exercise: 0.20 cm2). |
| Curio et al., 2020 | 55 (moderate MR at rest progressing to severe during exercise) 163 (severe MR at rest) | 62% | Handgrip | Patients with severe MR at rest had worse clinical outcomes. Residual MR after transcatheter mitral valve repair was worse in patients with severe MR at rest. A reduction of proportion of patients with heart failure hospitalization after intervention was observed in both groups. |
| Izumo et al., 202118 | 46 | 32% | Semisupine bicycle | Patients with exercise-induced secondary MR (an increase in ERO by ≥0.13 cm2) who underwent transcatheter mitral valve repair (mean ERO at rest: 0.26 cm2) had better functional capacity and lower risk of composite of death or heart failure than those who had medical therapy. |
| Others | ||||
| Lancellotti et al., 2004 | 28 (acute pulmonary oedema) 46 (control) | 100% | Semisupine bicycle | Changes in ERO, transtricuspid pressure gradient, and LVEF were independently associated with a history of recent pulmonary oedema. |
MR, mitral regurgitation; CABG, coronary artery bypass grafting; ERO, effective regurgitant orifice; LVEF, left ventricular ejection fraction; MV, mitral valve; GLS, global longitudinal strain; PH, pulmonary hypertension.
Treatment strategy for dynamic mitral regurgitation and acute heart failure
When considering therapies for functional MR, one should focus not only on resting conditions, but also on the dynamic component due to changes in LV loading conditions. Moreover, the functional MR phenotype may differ among patients. Patients with exertional dyspnoea that cannot be explained by the severity of MR at rest clearly benefit from stress testing. In these patients, a more physiological exercise using a treadmill or ergometer rather than handgrip exercise may be useful to unmask dynamic functional MR. However, in patients with acute pulmonary oedema without an apparent exacerbating factor, it is unclear which stress test is optimal to help decide whether to perform surgical or transcatheter treatment of functional MR. A prospective matched-pair cohort study including 28 patients with acute pulmonary oedema and LV systolic dysfunction and 46 patients without a history of acute pulmonary oedema demonstrated that changes in ERO and the resulting increase in pulmonary artery pressure during semisupine bicycle exercise were independently associated with a history of recent pulmonary edema.20 The development of acute pulmonary oedema is triggered by increases in preload and afterload associated with vasoconstriction caused by enhanced activity of the sympathetic nervous system. Vasopressor responses to isometric handgrip exercise are mediated by the sympathetic release of norepinephrine and activation of alpha-adrenergic receptors.21 Therefore, the isometric handgrip exercise may be a useful alternative despite less physiological response than treadmill or ergometer exercise in patients with acute pulmonary oedema, without an apparent exacerbating factor. As isometric handgrip exercise does not significantly increase venous return, it could be insufficient to unmask functional MR that may have triggered acute pulmonary oedema. The addition of stress testing to increase the LV preload such as leg raising or leg positive pressure22 during isometric handgrip stress echocardiography may be useful to unmask the dynamic functional MR. In the current issue, although the authors highlighted the importance of timing and condition of heart failure in the interpretation of the isometric handgrip stress test, it is still controversial whether an early-phase stress test is useful to unmask dynamic functional MR that may benefit from surgical or transcatheter mitral valve intervention; thus, further studies are needed.
Right heart catheterization during isometric handgrip stress can reveal an increase in the mean pulmonary capillary wedge pressure with a prominent V-wave in patients with dynamic MR. However, an increase in the mean pulmonary capillary wedge pressure with a prominent V-wave during exercise does not necessarily mean the contribution of dynamic severe MR. In patients with decreased left atrial compliance, the left atrium cannot accommodate atrial filling from the right ventricular contraction and pulmonary veins, resulting in an accentuated V-wave (stiff left atrial syndrome).23 One should consider both the left atrial compliance and MR when assessing the pulmonary capillary wedge pressure. When both elevated pulmonary capillary wedge pressure with a prominent V-wave and MR progression are observed during exercise stress, MR is likely to be a significant contributor to heart failure exacerbation. Further research is needed to better understand the optimal stress tests for dynamic functional MR that may benefit from mitral valve intervention for the improvement of quality of life and clinical outcomes in patients with this challenging pathophysiology.
Lead author biography
 Dr Kitai is Director of the Section of Heart Failure and Structural Heart Disease at National Cerebral and Cardiovascular Center in Japan. As a clinician-scientist and practicing heart failure/transplant cardiologist, Dr Kitai's translational research focuses on understanding the cellular and molecular mechanisms that contribute to disease progression in heart failure and cardiomyopathies, and valvular heart diseases. Email: [email protected].
Dr Kitai is Director of the Section of Heart Failure and Structural Heart Disease at National Cerebral and Cardiovascular Center in Japan. As a clinician-scientist and practicing heart failure/transplant cardiologist, Dr Kitai's translational research focuses on understanding the cellular and molecular mechanisms that contribute to disease progression in heart failure and cardiomyopathies, and valvular heart diseases. Email: [email protected].
Funding: None declared.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal – Case Reports or of the European Society of Cardiology.
Conflict of interest: None declared.




Comments