-
PDF
- Split View
-
Views
-
Cite
Cite
Clovis Nkoke, Siddikatou Djibrilla, Ronald Gobina, Anastase Dzudie, A case report of Trichinella spiralis pericarditis: an unusual cause of pericardial effusion and cardiac tamponade in an immunocompetent urban black African, European Heart Journal - Case Reports, Volume 7, Issue 1, January 2023, ytac480, https://doi.org/10.1093/ehjcr/ytac480
Close - Share Icon Share
Abstract
Cardiac trichinellosis is unusual and it is associated with high mortality. We report a case of Trichinella pericarditis complicated by a large pericardial effusion and cardiac tamponade in a setting where the aetiologic diagnosis of pericardial disease is challenging.
A 27-year-old immune-competent male patient from Cameroon consulted for pleuritic chest pain associated with fever, dry cough, and gradually worsening dyspnoea on exertion of 1-month duration. Upon admission, his blood pressure was 100/73 mmHg, the heart rate was 130/min. The clinical examination revealed a pericardial friction rub, jugular venous distension, and tender hepatomegaly. There was no lower extremity oedema. The diagnosis of pericarditis was made. A two-dimensional transthoracic echocardiogram performed showed a moderate fibrinous circumferential pericardial effusion with echocardiographic signs of tamponade. Pericardiocentesis was performed and analysis of the fluid revealed multiple, motile, roundworms which were identified as Trichinella spiralis, a nematode parasite. There was no eosinophilia on complete blood count. He was treated with Albendazole 800 mg daily per os. His clinical condition improved with resolution of the symptoms and a reduction in the size of the pericardial effusion.
Trichinella spiralis is a rare cause of pericarditis which can be life-threatening. With the existing challenges in diagnosing the aetiology of pericardial disease in African resource-limited setting, the diagnosis can be missed leading to fatal outcomes.
Cardiac involvement in trichinosis is unusual and absence of eosinophilia does not rule it out.
Pericarditis caused by trichinosis can be fatal if not promptly diagnosed and treated adequately.
Even though the aetiologic diagnosis of pericardial disease in African resource-limiting setting is challenging, it is crucial to establish the diagnosis in order to reduce the risk of fatal outcomes with appropriate treatment.
Introduction
Tuberculosis (TB) is the most common cause of pericardial disease in Africa irrespective of human immunodeficiency virus (HIV) status.1 Pericardial disease in Africa is also associated with high mortality rates of up to 25%.1 The aetiological diagnosis of the pericardial disease is challenging in African resource-limited settings. Trichinella spiralis is a nematode parasite.2 Cardiac trichinellosis is unsual. Although it has been reported to affect the myocardium causing myocarditis,3 it has not been reported as a common cause of pericarditis in Africa. Due to its rarity and the aetiological diagnostic challenges of pericarditis in Africa, it can often be missed and this may lead to a fatal outcome for the patient. We report a rare case of pericarditis caused by T. spiralis in a patient from Cameroon.
Timeline
Case presentation
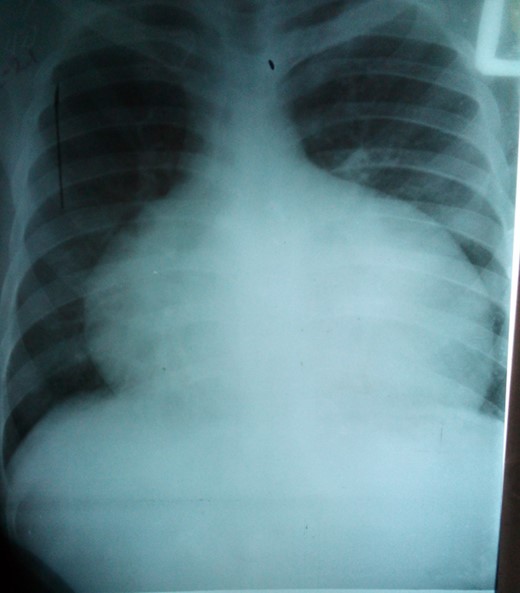
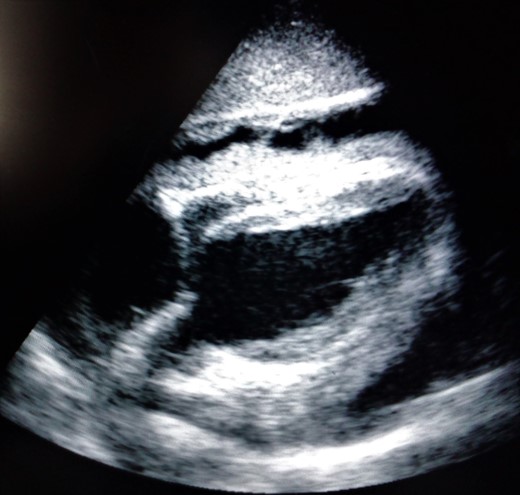
A 27-year-old male patient from Cameroon presented with precordial pleuritic chest pain of 1-month duration. The pain was associated with intermittent dry cough, low-grade fever, weight loss, and gradually worsening dyspnoea on exertion. The worsening of dyspnoea with the occurrence of paroxysmal nocturnal dyspnoea prompted consultation. He had significant medical history. He was a former inmate who had spent 10 months in prison. The symptoms started while he was in prison. The blood pressure was 100/76 mmHg and the heart rate of 130/min. The heart sounds were regular, rapid, and muffled. There was pericardial friction rub best heard along the left sternal edge. There was jugular venous distension and tender hepatomegaly. There was no lower extremity oedema. The lung examination was normal. The diagnosis of pericarditis complicated with effusion and right heart failure was made. A chest x-ray showed marked symmetric cardiomegaly (Figure 1). The lung parenchyma was normal. The electrocardiogram (ECG) showed sinus tachycardia with a complete left bundle branch block. The White cell count was 8500/mm3, haemoglobin at 9.8 g/dL, mean corpuscular volume (MCV) = 67 fl. The C-reactive protein (CRP) was 48 mg/L and the erythrocyte sedimentation rate (ESR) was 100 mm. The HIV serology was negative. A transthoracic echocardiogram showed a circumferential pericardial effusion measuring 21 mm over the inferior wall and 19 mm over the anterior wall, with a lot of fibrin. There was marked respiratory variation in mitral and tricuspid inflow. There was collapse of the right ventricular free wall. The inferior vena cava (IVC) was dilated with an absent respiratory variation. The left ventricular systolic function was normal. The diagnosis of a large fibrinous pericardial effusion with signs of hemodynamic compromise was made (Figure 2). There was no impairment of global or segmental left ventricular systolic function. He was started on empirical treatment for pericardial TB. An emergency pericardiocentesis was performed draining about 150 cc of straw-coloured fluid which was sent to the laboratory for analysis. A simple wet mount preparation of the fluid revealed motile (coiling) round worms (with slender anterior ends) identified as T. spiralis (Figure 3). An additional movie file shows this in more detail (see Additional files S2 and S3). Total protein of the pericardial fluid was 75.6 g/L which was compartible with an exudate. The anti-TB medications were stopped and the patient was started on albendazole 400 mg twice a day in association with corticosteroids. His clinical condition improved after 5 days with the improvement of dyspnoea and blood pressure. A repeat echocardiogram showed a significant regression of the effusion after 10 days of treatment. The patient was discharged but he never showed up for a follow-up visit.

Wet mount preparation of pericardial fluid showing Trichinella spiralis.
Discussion
This case reports a rare and potentially life-threatening cause of pericardial disease in an African patient and highlights the importance of an aetiological diagnosis of pericardial disease. To the best of our knowledge, this first reported case of T. spiralis pericarditis with tamponade in our setting where the diagnosis of pericardial disease is challenging.
In Africa, TB is the most common cause of the pericardial disease.1 The aetiological diagnosis of pericardial disease in an African resource-limited setting is challenging. Usually, there is no definitive diagnosis, and patients are treated empirically.1,4 Due to its rarity and the inherent diagnostic challenges, uncommon aetiologies like T. spiralis may be missed. Our patient was started on empirical treatment for pericardial TB based on the clinical presentation and on epidemiological reports which indicate that TB is the most common cause of pericardial disease in sub-Saharan Africa (SSA).1 After a simple laboratory test that confirmed the aetiology to be trichinellosis, he was treated with a relatively inexpensive medication (albendazole).
Trichinella spiralis is a round worm that causes trichinellosis. It has a worldwide distribution including Asia, Africa, and South America.5 It is transmitted by eating poorly cooked meat. The patient’s symptoms started when he was in prison suggesting that the cooking conditions in the prison might be a predisposing factor for infestation in the patient. When the larva gets into the intestines, it enters the bloodstream through the lymphatic circulation and spreads to skeletal muscle, cardiac muscle, and other tissues.6 Myocarditis and neurological disorders are the most serious complication of human infestation by T. spiralis, and myocarditis may lead to death without treatment.7 In this patient, we did not assess for markers of myocardial injury. So it was difficult to determine if there was underlying associated myocarditis. The ECG, however, showed a complete left bundle branch block that can be suggestive of myocardial injury.8 Global or segmental left ventricular systolic dysfunction can be present in myocarditis, but it was absent in this patient. A complete blood count can show leukocytosis and eosinophilia, which correlates with the number of worms causing the infection.9 In our patient, there was no leukocytosis nor eosinophilia. Eosinophilia has been observed in almost every case of trichinelosis.10
This case report emphasizes the importance of the aetiological diagnosis of pericardial disease even in endemic areas for TB where TB is the most common cause of pericardial disease. Although the aetiological diagnosis of pericardial disease is challenging in Africa, relatively inexpensive and available laboratory investigations and medications can be useful as shown in this case report.
Conclusion
Cardiac trichinellosis is an usual cause of life-threatening pericarditis with tamponade. Even though the etiologic diagnosis of pericardial disease in African resource-limiting setting is challenging, it is crucial to establish the diagnosis in order to reduce the risk of fatal outcomes with appropriate treatment.
Lead author biography
 Dr Clovis Nkoke is a cardiologist from Cameroon. He is currently a lecturer at the Faculty of Health Sciences of the University of Buea in Cameroon. He completed his residency in general cardiology in 2015. He is passionate about cardiovascular diseases research. In 2019, the Salim Yusuf World Heart Federation emerging leader program selected him as a World Federation Emerging leader. In 2021, he was elected Fellow of the European Society of cardiology as a recognition of his significant contribution to cardiovascular medicine. He is an ex-co member of the African Heart Failure Association (AHFA) of PASCAR.
Dr Clovis Nkoke is a cardiologist from Cameroon. He is currently a lecturer at the Faculty of Health Sciences of the University of Buea in Cameroon. He completed his residency in general cardiology in 2015. He is passionate about cardiovascular diseases research. In 2019, the Salim Yusuf World Heart Federation emerging leader program selected him as a World Federation Emerging leader. In 2021, he was elected Fellow of the European Society of cardiology as a recognition of his significant contribution to cardiovascular medicine. He is an ex-co member of the African Heart Failure Association (AHFA) of PASCAR.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written informed consent for the publication of this case report was obtained from the patient in line with Committee on Publication Ethics (COPE) guidelines.
Funding: None declared.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
References
Author notes
Conflict of interest: None declared.





Comments