-
PDF
- Split View
-
Views
-
Cite
Cite
Joshua T Chai, Sam McGrath, Begoña Lopez, Rafal Dworakowski, Eosinophilic granulomatosis with polyangiitis (Churg–Strauss syndrome) masquerading as acute ST-elevation myocardial infarction with complete resolution after immunosuppressive therapy: a case report, European Heart Journal - Case Reports, Volume 2, Issue 3, September 2018, yty075, https://doi.org/10.1093/ehjcr/yty075
Close - Share Icon Share
Abstract
Eosinophilic granulomatosis with polyangiitis (EGPA, formerly known as Churg–Strauss syndrome) is a rare autoimmune condition characterized by inflammation of small- and medium-sized blood vessels, which usually presents with systemic vasculitis preceded by airway allergic hypersensitivity.
Here, we report a highly unusual case of acute ST-elevation myocardial infarction in a young and fit man with no cardiovascular risk factors. His emergency coronary angiography revealed disproportionately severe widespread coronary artery disease. We describe the diagnostic challenges with emphasis on meticulous history-taking (deep hyponasal voice, anosmia, and childhood asthma), supported by timely blood markers (peripheral eosinophilia and raised CRP), and multi-modal imaging (severe paranasal sinusitis on cranial magnetic resonance imaging and multiple lung infiltrates with small patches of ground-glass appearance on thoracic computed tomography), to reach a diagnosis of EGPA coronary vasculitis with particular reference to the American College of Rheumatology EGPA classification. Importantly, with prompt immunosuppression, his coronary lesions resolved completely without the need of any surgical or percutaneous revascularisation. He remained well and asymptomatic on maintenance immunosuppressants at 1 year follow-up.
This case highlighted the rare but recognized involvement of the coronary arteries in systemic EGPA vasculitis, which can sometimes mimic atherosclerotic coronary disease and acute coronary syndrome.
Introduction
In the presence of unusual pattern of diffuse coronary artery disease, clinicians should be alerted to the possibility of non-atherosclerotic coronary stenosis, for example, from coronary vasculitis that can sometimes represent an index presentation of eosinophilic granulomatosis with polyangiitis (EGPA)/Churg–Strauss syndrome.
Clinical acumen with meticulous history supported by timely blood markers and imaging of the paranasal sinuses and thorax often allows a diagnosis to be made with good sensitivity and specificity.
Coronary vasculitis from EGPA has been shown to be highly responsive to immunosuppressive therapy; in our case showing complete angiographic resolution of diffuse multi-vessel severe coronary stenosis within a short time of immunosuppression.
ST-elevation myocardial infarction (STEMI) is a well-defined clinical emergency, with clear international guidelines both from the ESC1 and ACC/AHA2 regarding its acute management. Although the overwhelming majority of STEMIs are caused by acute vessel closure following atherosclerotic plaque rupture and its thromboembolic complications, cardiologists, and emergency physicians should be aware of other causes of acute coronary syndrome (ACS) that present similarly, yet from entirely different pathophysiology. Eosinophilic granulomatosis with polyangiitis (EGPA, formerly known as Churg–Strauss syndrome) is a rare autoimmune condition characterized by inflammation of small- and medium-sized blood vessels, which usually presents with systemic vasculitis preceded by airway allergic hypersensitivity.3 Here, we report a case of EGPA with an index presentation masquerading as acute STEMI. Importantly, with a short course of potent immunosuppressive therapy administered in a timely fashion, his diffused coronary lesions completely resolved without the need of any percutaneous or surgical revascularisation.
Timeline
| Timeline . | Events . |
|---|---|
| 6 months before presentation | Progressive nasal congestion and anosmia. |
| 4 h before presentation | Central chest pain whilst walking dog. |
| At presentation | Electrocardiogram showed inferior ST-elevation myocardial infarction. |
| 45 min after presentation | Emergency coronary angiography showed diffuse three-vessel coronary artery disease but no acute vessel closure. No primary angioplasty performed. |
| Day 1 after presentation | Heart team multidisciplinary meeting. |
| Day 2 after presentation | Started on oral prednisolone. |
| Day 3–14 after presentation | Investigation with cranial magnetic resonance imaging (MRI) showed severe paranasal sinusitis; cardiac MRI showed acute myocardial infarction in the apical anterior and anterolateral walls but no myocarditis; thoracic computed tomography showed multiple lung infiltrates with small patches of ground-glass appearance consistent with vasculitic processes. |
| 2 weeks after presentation | Changed to iv methylprednisolone for 3 days. |
| 3 weeks after presentation | Cyclophosphamide (once every 3 weeks for a total of 6 doses) with tapering prednisolone. |
| 4 weeks after presentation | Repeat coronary angiography showing complete resolution of coronary lesions. |
| 1 year follow-up | Remained well and asymptomatic on maintenance prednisolone and mycophenolate mofetil. Normal inflammatory blood markers. Normal LV function on follow-up echocardiogram. |
| Timeline . | Events . |
|---|---|
| 6 months before presentation | Progressive nasal congestion and anosmia. |
| 4 h before presentation | Central chest pain whilst walking dog. |
| At presentation | Electrocardiogram showed inferior ST-elevation myocardial infarction. |
| 45 min after presentation | Emergency coronary angiography showed diffuse three-vessel coronary artery disease but no acute vessel closure. No primary angioplasty performed. |
| Day 1 after presentation | Heart team multidisciplinary meeting. |
| Day 2 after presentation | Started on oral prednisolone. |
| Day 3–14 after presentation | Investigation with cranial magnetic resonance imaging (MRI) showed severe paranasal sinusitis; cardiac MRI showed acute myocardial infarction in the apical anterior and anterolateral walls but no myocarditis; thoracic computed tomography showed multiple lung infiltrates with small patches of ground-glass appearance consistent with vasculitic processes. |
| 2 weeks after presentation | Changed to iv methylprednisolone for 3 days. |
| 3 weeks after presentation | Cyclophosphamide (once every 3 weeks for a total of 6 doses) with tapering prednisolone. |
| 4 weeks after presentation | Repeat coronary angiography showing complete resolution of coronary lesions. |
| 1 year follow-up | Remained well and asymptomatic on maintenance prednisolone and mycophenolate mofetil. Normal inflammatory blood markers. Normal LV function on follow-up echocardiogram. |
| Timeline . | Events . |
|---|---|
| 6 months before presentation | Progressive nasal congestion and anosmia. |
| 4 h before presentation | Central chest pain whilst walking dog. |
| At presentation | Electrocardiogram showed inferior ST-elevation myocardial infarction. |
| 45 min after presentation | Emergency coronary angiography showed diffuse three-vessel coronary artery disease but no acute vessel closure. No primary angioplasty performed. |
| Day 1 after presentation | Heart team multidisciplinary meeting. |
| Day 2 after presentation | Started on oral prednisolone. |
| Day 3–14 after presentation | Investigation with cranial magnetic resonance imaging (MRI) showed severe paranasal sinusitis; cardiac MRI showed acute myocardial infarction in the apical anterior and anterolateral walls but no myocarditis; thoracic computed tomography showed multiple lung infiltrates with small patches of ground-glass appearance consistent with vasculitic processes. |
| 2 weeks after presentation | Changed to iv methylprednisolone for 3 days. |
| 3 weeks after presentation | Cyclophosphamide (once every 3 weeks for a total of 6 doses) with tapering prednisolone. |
| 4 weeks after presentation | Repeat coronary angiography showing complete resolution of coronary lesions. |
| 1 year follow-up | Remained well and asymptomatic on maintenance prednisolone and mycophenolate mofetil. Normal inflammatory blood markers. Normal LV function on follow-up echocardiogram. |
| Timeline . | Events . |
|---|---|
| 6 months before presentation | Progressive nasal congestion and anosmia. |
| 4 h before presentation | Central chest pain whilst walking dog. |
| At presentation | Electrocardiogram showed inferior ST-elevation myocardial infarction. |
| 45 min after presentation | Emergency coronary angiography showed diffuse three-vessel coronary artery disease but no acute vessel closure. No primary angioplasty performed. |
| Day 1 after presentation | Heart team multidisciplinary meeting. |
| Day 2 after presentation | Started on oral prednisolone. |
| Day 3–14 after presentation | Investigation with cranial magnetic resonance imaging (MRI) showed severe paranasal sinusitis; cardiac MRI showed acute myocardial infarction in the apical anterior and anterolateral walls but no myocarditis; thoracic computed tomography showed multiple lung infiltrates with small patches of ground-glass appearance consistent with vasculitic processes. |
| 2 weeks after presentation | Changed to iv methylprednisolone for 3 days. |
| 3 weeks after presentation | Cyclophosphamide (once every 3 weeks for a total of 6 doses) with tapering prednisolone. |
| 4 weeks after presentation | Repeat coronary angiography showing complete resolution of coronary lesions. |
| 1 year follow-up | Remained well and asymptomatic on maintenance prednisolone and mycophenolate mofetil. Normal inflammatory blood markers. Normal LV function on follow-up echocardiogram. |
Case summary
A 42-year-old Caucasian gentleman presented to our Cardiac Catheter Laboratory directly via the ambulance primary angioplasty service with a 4 h history of central chest pain while walking his dog. His pain radiated to his left shoulder and was associated with nausea. He was previously fit and well except for a history of childhood asthma, not requiring any inhaler therapy. He did not smoke, exercised regularly, and had no family history of premature cardiovascular disease. His electrocardiogram (ECG) showed inferior ST-segment elevation, with reciprocal high lateral ST-segment depression. Of note was that the patient spoke with an unusually deep hyponasal voice, and had seen his general practitioner for persistent ‘allergic rhinitis’ for 6 months, after suffering from progressive nasal congestion and anosmia.
On examination, his blood pressure was normal at 126/74 mmHg with a pulse rate of 85 b.p.m. He was clinically euvolaemic with normal JVP and no sign of peripheral oedema. Cardiac auscultation revealed normal heart sounds. His lung bases were clear on auscultation. There were no skin lesions of note. A bedside transthoracic echocardiogram revealed inferior and apical hypokinaesia with overall preserved left ventricular function.
After loading with aspirin 300 mg and ticagrelor 180 mg, the patient underwent emergency coronary angiography, which showed severe three-vessel coronary artery disease (Figure 1). Administration of 500 μg of intracoronary glyceryl trinitrate during angiography did not alter his stenotic lesions and vessel calibre. Cardiac troponin I was elevated to >39 000 ng/L (normal <16 ng/L). His blood count revealed marked eosinophilia 3.13 × 109/L (normal 0–0.4 × 109/L, total white cell count 9.37 × 109/L), with mildly elevated CRP of 22.8 mg/L. ESR had been normal throughout. Cardiac magnetic resonance imaging (MRI) (Figure 2) performed the following day confirmed acute myocardial infarction in the apical anterior and anterolateral walls but showed no evidence of myocarditis. Subsequent cranial MRI showed severe paranasal sinusitis with total obstruction of all paranasal sinuses. A thoracic computed tomography (CT) scan also showed multiple tiny lung infiltrates and small patches of ground-glass appearance consistent with vasculitic processes. Anti-neutrophil cytoplasmic antibody (ANCA) test was negative. Since he fulfilled four out of the six American College of Rheumatology (ACR) classification criteria for EGPA, a presumptive diagnosis of EGPA-associated coronary vasculitis was made.
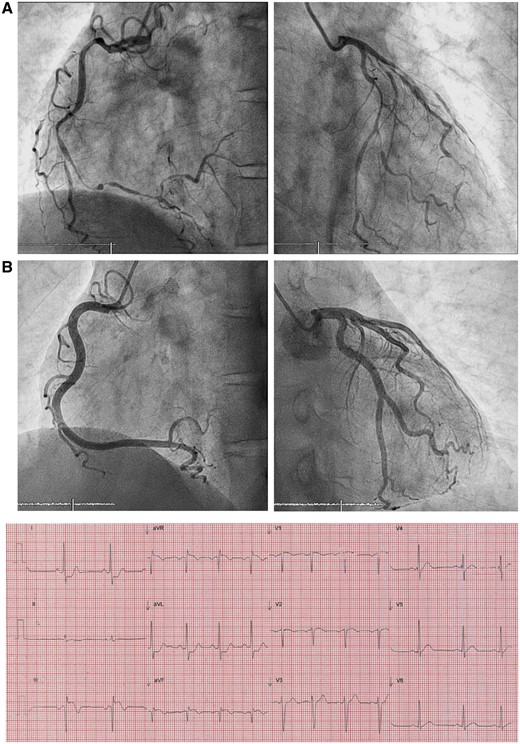
Presenting electrocardiogram and coronary angiography. Electrocardiogram showing inferior ST-segment elevation myocardial infarction. Coronary angiography at the time of presentation (A) showed unusually severe widespread luminal stenosis throughout the coronary trees despite administration of 500 μg of intracoronary glyceryl trinitrate; repeat angiography (B) after 4 weeks of immunosuppression showed complete resolution—note the smooth contour of the vessel wall devoid of atheroma (Standard LAO view for RCA and PA/slight RAO caudal view for LCA projection—please refer to Supplementary material online, Video clips for more detailed angiography).
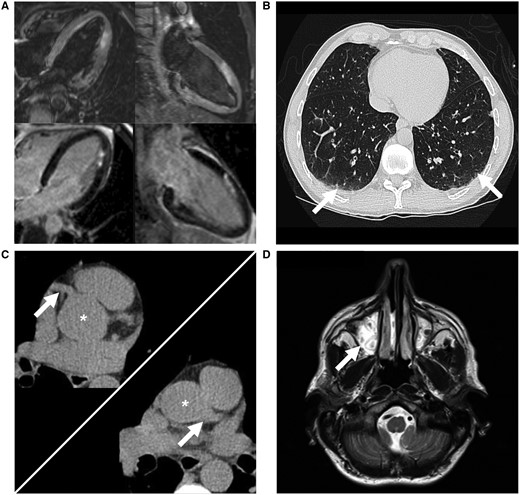
Multi-modal investigation to support eosinophilic granulomatosis with polyangiitis diagnosis. Cardiac magnetic resonance imaging (A) showing acute myocardial infarction in the apical anterior and anterolateral walls but no myocarditis; computed tomography thorax (B) showing multiple tiny pulmonary nodules and small patches of ground-glass appearance (arrows) in the lung bases; cardiac computed tomography (C) showing no coronary calcification with an Agatston score of zero; asterisk denotes aortic root with left arrow at the right coronary artery and right arrow at the left main coronary artery; head magnetic resonance imaging (D) showing complete opacification of the maxillary sinuses (arrow).
No primary angioplasty was attempted at the time of emergency angiography as there was no complete vessel closure and his chest pain was subsiding. Due to concerns that his asthma being previously triggered by aspirin, his antiplatelet regimen was switched to clopidogrel 75 mg alone with subcutaneous fondaparinux 2.5 mg once daily (for 7 days). He also initially received bisoprolol and ramipril, but these were down-titrated due to hypotension and eventually discontinued. After discussion at the Heart Team multidisciplinary meeting, the consensus was to defer revascularisation pending a trial of immunosuppressive therapy. He was started on intravenous methylprednisolone (500 mg/day) for 3 days, followed by his first dose of cyclophosphamide (CYCLOPS regime, 15 mg/kg infusion), which was repeated every 3 weeks for a total of 6 doses eventually. Whilst on CYCLOPS regime, his was given prednisolone 50 mg (1 mg/kg orally) gradually tapering down to 20 mg once daily.
The patient remained well in hospital and his nasal congestion and anosmia rapidly improved. His eosinophil count and CRP also responded rapidly to immunosuppression and returned to within normal range 1 week after his first dose of methylprednisolone. A repeat coronary angiogram performed 10 days after his first dose of cyclophosphamide (4 weeks after his initial presentation) showed complete resolution of his previously critical coronary lesions (Figure 1). He was discharged from hospital to complete his CYCLOPS regime uneventfully as an outpatient. As to maintenance immunosuppresion, he was initially put on azathioprine 4 weeks after his last dose of CYCLOPS, whilst continuing his tapering dose of prednisolone. Due to side-effect tolerability issues, he was eventually put on mycophenolate mofetil with low-dose prednisolone as maintenance and remained well and asymptomatic, with normal CRP, ESR, and eosinophil count, at 1 year follow-up. Follow-up echocardiogram at 1 year showed completely normal left ventricular function with no regional wall motion abnormality. He continued on clopidogrel as a single antiplatelet agent to reduce future chances of occlusive thrombotic complication.
Discussion
Coronary vasculitis in eosinophilic granulomatosis with polyangiitis
Eosinophilic granulomatosis with polyangiitis is a rare vasculitic disorder defined by granulomatous, eosinophil-rich inflammation of the respiratory tract, coupled with necrotizing vasculitis of small to medium-sized vessels.3 It is commonly associated with asthma.4 The incidence is estimated at 2.4–6.8 per 1 000 000 cases per year.5 Its pathogenesis typically follows three phases—the first being a Type 1 hypersensitivity disorder such as asthma or allergic rhinitis; the second phase presents months to years later and is characterized by eosinophilic infiltrative disease usually with the presence of pulmonary infiltrates; finally, the third (late) phase of EGPA is systemic vasculitis.6
The prevalence of cardiac involvement in EGPA is well reported7; however, coronary vasculitis as the index presentation to hospital is extremely rare with only a handful of cases being described in the literature to date. Cardiac involvement in EGPA can also vary in presentation, which might include peri/myocarditis, ACSs, and heart failure.8 This cohort of EGPA patients with cardiac involvement have been shown to have an overall increased morbidity and mortality compared with those without cardiac involvement.7 Furthermore, it has been shown that ANCA-negative EGPA patients are more likely to have cardiopulmonary manifestations, whereas ANCA-positive patients more commonly present with other small vessel vasculitis.4
Eosinophilic granulomatosis with polyangiitis masquerading as ST-elevation myocardial infarction—the American College of Rheumatology classification
The ACR Classification of EGPA was developed in 19909; four out of the six criteria listed must be present to classify EGPA in a patient with vasculitis. The six criteria listed by the ACR are (i) asthma; (ii) eosinophilia > 10% on white blood cell differential count; (iii) mono-/polyneuropathy; (iv) migratory/transient pulmonary infiltrates detected radiographically; (v) paranasal sinus abnormality; and (vi) biopsy containing blood vessel with extravascular eosinophils.
Our patient presented with chest pain and STEMI in the absence of any classic cardiovascular risk factors. His coronary angiography, however, revealed disproportionately severe widespread lesions throughout his coronary tree. After subsequent investigation, he had >30% peripheral eosinophilia, nasal sinusitis and pulmonary infiltrates on CT, combined with a past history of asthma. This meant he fulfilled four out of the six ACR classification criteria for EGPA. According to the ACR classification, the presence of four or more of the six criteria has a sensitivity of 85% and a specificity of 99.7% for EGPA.9 Furthermore, he was also found to be ANCA-negative, which is more commonly associated with cardiac/coronary involvement in EGPA.4
Whilst previous series reported EGPA patients diagnosed with non-ST-elevation ACS based on presentation of chest pain, enzyme rise, and/or evidence on imaging,10,11 none presented acutely with ST-elevation ECG changes, mimicking a STEMI, that triggered the pathway for consideration of emergency primary percutaneous coronary intervention. To the best our knowledge, our patient was the first reported case in the literature of an index presentation of a previously undiagnosed EGPA masquerading as a STEMI with severe triple vessel disease, which completely resolved with immunosuppression.
Kounis syndrome (Type 1), also known as allergic hypersensitivity coronary vasospasm, is an important differential diagnosis here.12 This is thought to be triggered by mast cell activation from known or unidentified allergens (often drugs) that cause severe coronary vasospasm that can mimic ACS. In our case, there was no improvement in his coronary lesions after administration of 500 μg of intracoronary glyceryl trinitrate during angiography. There was also no precipitant/allergic culprit reported or identified.
Conclusion
This case highlighted that in the presence of unusual pattern of diffuse coronary artery disease, clinicians should be alerted to the possibility of non-atherosclerotic coronary stenosis, for example, from coronary vasculitis that can sometimes represent an index presentation of EGPA. Clinical acumen from meticulous history supported by timely blood markers and imaging of the paranasal sinuses and thorax often allows a diagnosis to be made with good sensitivity and specificity. Coronary vasculitis from EGPA has been shown to be highly responsive to immunosuppressive therapy; in our case showing complete angiographic resolution of diffuse multi-vessel severe coronary stenosis within a few weeks of immunosuppression.
Acknowledgements
The authors would like to acknowledge the generosity and assistance from Dr Annette Maznyczka and Dr Patrick Gordon in the preparation of this manuscript. This work was supported in part by a National Institute for Health Research Biomedical Research Centre award to Guy's & St Thomas' Hospital and King's College London in partnership with King's College Hospital.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.




Comments