-
PDF
- Split View
-
Views
-
Cite
Cite
Naruhiko Ito, Manabu Kurabayashi, Kaoru Okishige, Kenzo Hirao, Subcutaneous implantable cardioverter-defibrillator implantation for ventricular fibrillation caused by coronary artery spasm: a case report, European Heart Journal - Case Reports, Volume 2, Issue 3, September 2018, yty074, https://doi.org/10.1093/ehjcr/yty074
Close - Share Icon Share
Abstract
Coronary artery spasm usually has a good prognosis, except when it induces lethal ventricular arrhythmias. Implantable cardioverter-defibrillator (ICD) implantation in addition to optimal medical therapy including prescription of coronary vasodilators and smoking cessation is a therapeutic option for coronary artery spasm patients who present with lethal ventricular arrhythmia. Subcutaneous ICDs are now available as an alternative to conventional transvenous ICDs.
We report the first case of a 50-year-old Japanese male without any structural heart disease who presented with ventricular fibrillation caused by coronary artery spasm, and underwent subcutaneous ICD implantation for secondary prevention of sudden cardiac death (SCD). We attributed his aborted SCD to coronary artery spasm based on findings of cardiac catheterization including acetylcholine provocation test and cardiac electrophysiological study. During the 1 year of follow-up, the patient discharged on calcium channel blockers and nicorandil has been free of angina, ventricular arrhythmias, and appropriate ICD therapy.
Coronary artery spasm patients with aborted SCD may be good candidates for implantation of subcutaneous ICDs, because most of them have no need for concomitant bradycardia therapy, cardiac resynchronization therapy, or anti-tachycardia pacing therapy.
Implantation of implantable cardioverter-defibrillator (ICD) with optimal medical therapy is an appropriate therapeutic option for coronary artery spasm patients with aborted sudden cardiac death (SCD).
Most coronary artery spasm patients with aborted SCD have normal left ventricular ejection fraction and do not have arrhythmogenic substrates, so they may be good candidates for the implantation of subcutaneous ICD.
Introduction
Coronary artery spasm is more common in Japanese and Koreans than in Caucasians.1 Its clinical presentation varies widely from stable angina to sudden cardiac death (SCD).1,2 For those who have experienced aborted SCD (ASCD), implantable cardioverter-defibrillator (ICD) implantation in addition to optimal medical therapy is a therapeutic option.3 However, transvenous ICD implantation comes with risk of complications, associated with morbidity and financial cost.4 Subcutaneous ICD systems have become readily available as an alternative to conventional transvenous ICD systems in select clinical settings.5 To our knowledge, there have not been any published reports discussing implantation of subcutaneous ICD for lethal arrhythmia due to coronary artery spasm. We, therefore, present for the first time, the case of a coronary artery spasm patient with ASCD who was treated with implantation of subcutaneous ICD for secondary prevention of SCD.
Timeline
| Time . | Events . |
|---|---|
| Day 0 | A 50-year-old man collapsed on his way to work at 8 AM. |
| After chest compression, an automated external defibrillator detected ventricular fibrillation (VF). Six electrical shocks were required to terminate VF. | |
| He was intubated and started on mechanical ventilation management at the emergency room. | |
| Emergency cardiac catheterization showed normal coronary artery and left ventricular contraction. | |
| Targeted temperature management and intravenous injection of nicorandil was started in the intensive care unit setting. | |
| Day 2 | He was withdrawn from mechanical ventilation management. |
| Day 13 | Acetylcholine provocation test: positive |
| Day 15 | Cardiac electrophysiological study: negative |
| Day 26 | Subcutaneous implantable cardioverter-defibrillator implantation |
| Day 33 | Discharge from hospital with no residual neurological deficits |
| Time . | Events . |
|---|---|
| Day 0 | A 50-year-old man collapsed on his way to work at 8 AM. |
| After chest compression, an automated external defibrillator detected ventricular fibrillation (VF). Six electrical shocks were required to terminate VF. | |
| He was intubated and started on mechanical ventilation management at the emergency room. | |
| Emergency cardiac catheterization showed normal coronary artery and left ventricular contraction. | |
| Targeted temperature management and intravenous injection of nicorandil was started in the intensive care unit setting. | |
| Day 2 | He was withdrawn from mechanical ventilation management. |
| Day 13 | Acetylcholine provocation test: positive |
| Day 15 | Cardiac electrophysiological study: negative |
| Day 26 | Subcutaneous implantable cardioverter-defibrillator implantation |
| Day 33 | Discharge from hospital with no residual neurological deficits |
| Time . | Events . |
|---|---|
| Day 0 | A 50-year-old man collapsed on his way to work at 8 AM. |
| After chest compression, an automated external defibrillator detected ventricular fibrillation (VF). Six electrical shocks were required to terminate VF. | |
| He was intubated and started on mechanical ventilation management at the emergency room. | |
| Emergency cardiac catheterization showed normal coronary artery and left ventricular contraction. | |
| Targeted temperature management and intravenous injection of nicorandil was started in the intensive care unit setting. | |
| Day 2 | He was withdrawn from mechanical ventilation management. |
| Day 13 | Acetylcholine provocation test: positive |
| Day 15 | Cardiac electrophysiological study: negative |
| Day 26 | Subcutaneous implantable cardioverter-defibrillator implantation |
| Day 33 | Discharge from hospital with no residual neurological deficits |
| Time . | Events . |
|---|---|
| Day 0 | A 50-year-old man collapsed on his way to work at 8 AM. |
| After chest compression, an automated external defibrillator detected ventricular fibrillation (VF). Six electrical shocks were required to terminate VF. | |
| He was intubated and started on mechanical ventilation management at the emergency room. | |
| Emergency cardiac catheterization showed normal coronary artery and left ventricular contraction. | |
| Targeted temperature management and intravenous injection of nicorandil was started in the intensive care unit setting. | |
| Day 2 | He was withdrawn from mechanical ventilation management. |
| Day 13 | Acetylcholine provocation test: positive |
| Day 15 | Cardiac electrophysiological study: negative |
| Day 26 | Subcutaneous implantable cardioverter-defibrillator implantation |
| Day 33 | Discharge from hospital with no residual neurological deficits |
Case report
A 50-year-old Japanese male with a medical history of thoracic haemangioma who was taking no medications and was regularly followed by computed tomography suddenly collapsed on his way to work at 8 AM. He had no history of angina and no risk factors for arteriosclerosis, such as hypertension, diabetes mellitus, or smoking. He had no prior history of syncope or a family history of syncope or juvenile SCD. Chest compression was immediately performed by bystanders. After several minutes’ resuscitation effort, he was connected to an automated external defibrillator (AED). The AED detected ventricular fibrillation (VF) and delivered the appropriate electrical shock, but VF continued. On the fourth electrical shock delivery, VF was terminated transiently, but recurred immediately (Figure 1A). Two additional shocks finally terminated the VF, and the ECG recorded by the AED showed ST-segment elevation (Figure 1B). After return of spontaneous circulation, the patient was brought to the emergency room. At presentation to the emergency room, he was unconscious with Glasgow coma scale score of 5/15 (e1, v1, and m3). His heart rate was 136 b.p.m., blood pressure was 157/110 mmHg, and there was no cardiac murmur or extra sound. He arrived ventilated by a laryngeal tube which we removed so he could be intubated, and placed on mechanical ventilation. His ECG showed ST-segment elevation in the lateral leads and ST-segment depression in the inferior leads (Figure 1C). Laboratory analysis revealed normal values for complete blood cell count, electrolytes, and cardiac enzymes. As for electrolytes, he had a potassium level of 3.9 mEq/L (normal: 3.6–5.0 mEq/L), sodium of 139 mEq/L (136–147 mEq/L), calcium of 10.0 mg/dL (8.7–10.1 mg/dL), and magnesium of 2.0 mg/dL (1.8–2.6 mg/dL). As for cardiac enzymes, CK was 177 U/L (57–197 U/L), CK-MB was 77 U/L (0–25U/L), and troponin I was 0.0070 ng/mL (<0.040 ng/mL). We immediately performed emergency cardiac catheterization, which showed normal left ventricular contraction and no significant stenosis or thrombosis of the coronary arteries. After the acute phase passed, his ECG was completely normal, it displayed; normal QT interval, and lacked T-wave alternans, notched T-wave, and early repolarization including a J-wave (Figure 1D). Therefore, this patient did not satisfy any of the diagnostic criteria for long QT syndrome.6 Based on these ECG and catheterization results, we gave a tentative diagnosis of coronary artery spasm. He was admitted to the intensive care unit and treated with targeted temperature management (target temperature of 34°C for 24 h) for the neurological defects under sedation with fentanyl, propofol, and dexmedetomidine. Intravenous injection of nicorandil (2 mg/h) was used for the prevention of coronary artery spasm.
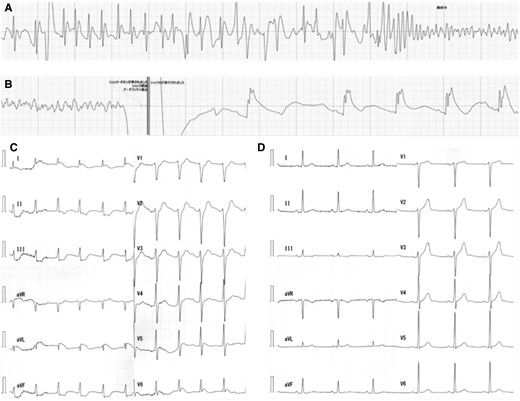
(A) After appropriate electrical cardioversion was delivered four times, transient sinus rhythm was obtained but ventricular fibrillation returned. (B) After two more shocks, the automated external defibrillator ECG showed termination of ventricular fibrillation and ST-segment elevation. (C) After termination of ventricular fibrillation, 12 lead ECG showed ST-segment elevation in the lateral leads and ST-segment depression in the inferior leads. (D) After the acute phase passed, his ECG was completely normal.
His ECG monitor during hospitalization showed no ventricular premature beats. Transthoracic echo cardiogram and contrast enhancement magnetic resonance imaging (MRI) did not detect any structural heart disease. Two days after admission, sedative drugs were interrupted, and he was able to be weaned from mechanical ventilation. At that point, although his consciousness was completely clear with Glasgow coma scale score of 15/15 (e4, v5, and m6), he had a slight disturbance of short-term memory. A brain MRI conducted 5 days after admission, revealed no abnormalities. Thirteen days after admission, we performed acetylcholine provocation test after >24 h discontinuation of calcium channel blocker (CCB) and nicorandil.7 Intracoronary injection of 20 μg of acetylcholine into the left coronary artery induced coronary artery spasm of the distal portion of the left anterior descending coronary artery (Figure 2, black arrows). Fifteen days after his event, we performed cardiac electrophysiological study, while he was on nifedipine (20 mg/day) and nicorandil (15 mg/day).7 Programmed stimulation with triple extra-stimuli at the right ventricular apex and outflow did not induce any lethal ventricular arrhythmia. A drug challenge with intravenous pilsicainide did not show any ECG indications of Brugada syndrome. The patient’s neurological status gradually improved and by discharge, he had no residual neurological deficits.
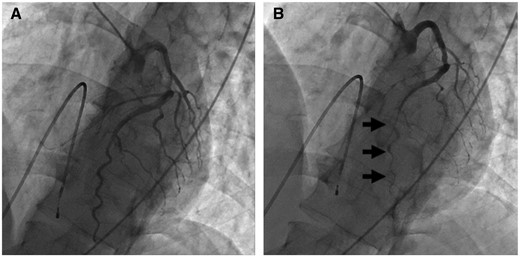
(A) LAO cranial view of the left coronary artery at baseline. (B) LAO cranial view of the left coronary artery after intracoronary injection of 20 μg of acetylcholine into it. It induced spasm of the distal portion of the left anterior descending artery (black arrows).
Taking all of the findings together, we attributed the patient's ASCD to coronary artery spasm and implanted a subcutaneous ICD under general anaesthesia for secondary prevention of SCD (Figure 3). The patient was discharged on nifedipine and nicorandil. During the 1 year of follow-up, the patient has been free of angina. Implantable cardioverter-defibrillator interrogation revealed no ventricular arrhythmias and appropriate ICD therapy.
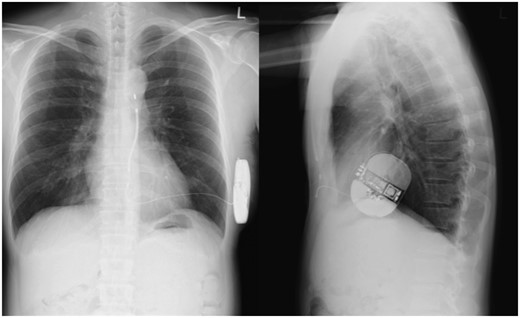
The chest X-ray after implantation of the subcutaneous implantable cardioverter-defibrillator.
Discussion
Recent studies report that appropriate medical treatment including prescription of CCB and smoking cessation can achieve good long-term outcomes for coronary artery spasm patients,1 even those who have suffered ASCD.8 However, it is also true that in three recent large scale observational studies, lethal ventricular arrhythmic events were found to recur in about one in four cases of coronary artery spasm patients with ASCD.9–11 The first of these found a non-significant trend towards fewer cardiac deaths in the patients who had received an ICD as opposed to those who had not (4% vs. 19%, P = 0.15).9 Nevertheless, the authors concluded that ICDs were likely beneficial, and that the P-value did not reach significance due to small sample size. Another study found that coronary artery spasm patients with lethal ventricular arrhythmia were not always saved by appropriate cardioversion,12 especially those who were current smokers or who discontinued medication.13 We ourselves believe that based on the high recurrence rate of ventricular tachyarrhythmias, implantation of ICD with optimal medical therapy is an appropriate therapeutic option for coronary artery spasm patients with ASCD, especially if the less invasive subcutaneous ICD is deployed.
A recent research study reported that the rate of all complications from implantation of transvenous dual chamber ICD was 14.1% and the rate of major complications requiring re-intervention was 6.7%.5 Another study reported that subcutaneous ICD had less frequent lead complications and longer lead survival than transvenous ICD, whereas there was no significant difference in the rate of appropriate shock between transvenous ICD and subcutaneous ICD.14 Subcutaneous ICD is indicated for prevention of SCD in patients who have no need for concomitant bradycardia therapy, cardiac resynchronization therapy, or anti-tachycardia pacing therapy.5 Unlike patients with prior myocardial infarction or cardiomyopathy, most coronary artery spasm patients with ASCD have normal left ventricular ejection fraction and do not have arrhythmogenic substrates. Therefore, they may be good candidates for the implantation of subcutaneous ICD.
Conclusion
We reported the first case of a coronary artery spasm patient without structural heart disease who underwent implantation of a subcutaneous ICD after surviving VF. Coronary artery spasm patients may be good candidates for implantation of subcutaneous ICD.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.




Comments