-
PDF
- Split View
-
Views
-
Cite
Cite
Holly B. Vince, Charles R. Tomson, Eric J. Loveday, Paul A. Lear, John B. Eastwood, Nutcracker phenomenon presenting as loin pain haematuria syndrome, NDT Plus, Volume 4, Issue 6, December 2011, Pages 418–420, https://doi.org/10.1093/ndtplus/sfr152
Close - Share Icon Share
Abstract
A 19-year-old female presented with bilateral severe loin pain associated with recurrent macroscopic haematuria. A provisional diagnosis of loin pain haematuria syndrome was made; the severity and frequency of pain led to referral to the pain management service. Alternative diagnoses were considered. Although previous reports of obstruction of the left renal vein have not described pain of this severity, magnetic resonance angiography was performed; it showed obstruction of the left renal vein as it passed between the superior mesenteric artery and aorta, i.e. the nutcracker phenomenon. Both pain and haematuria resolved fully after autotransplantation.
Background
Loin pain haematuria syndrome was first described in 1967 [1] as a syndrome of visceral loin pain and fever, associated with microscopic or macroscopic haematuria. The authors drew attention to abnormalities of the peripheral arterial circulation on renal angiography. A number of reports have emphasized psychiatric disturbances and factitious illness in some patients with the syndrome and have suggested that the condition has some characteristics of a somatoform disorder [2–4]. The arteriographic abnormalities have not proved to be a constant feature of the syndrome, and psychiatric disturbance cannot explain the presence of haematuria. Some patients with proven glomerulonephritis experience loin pain during episodes of macroscopic haematuria, possibly due to oedema with stretching of the renal capsule, but most patients with loin pain and haematuria do not have glomerulonephritis.
The anatomical abnormality causing compression as the left renal vein passes between the aorta and the superior mesenteric artery was first described in 1950 [5]. Twenty years later, Chait et al. [6] noted vascular impressions (varicosities) indenting the left ureter on urography. The term ‘nutcracker phenomenon’ was coined by de Schepper in 1972 [7] to describe the anatomical problem. A recent comprehensive review summarizes the presentation and treatment of the condition [8]. Severe pain was not a prominent feature in these reports.
What is important about the case presented here is that the predominant symptom was pain; symptoms of venous obstruction—other than macroscopic haematuria—were not prominent. The case therefore resembled ‘loin pain haematuria syndrome’ so it is important that the distinction between the two conditions is made more widely known.
Case report
A 19-year-old female anatomy student (H.B.V.) was referred for further evaluation of recurrent macroscopic haematuria, without clots, and severe bilateral flank pain, with a provisional diagnosis of loin pain haematuria syndrome. Twelve months earlier, she had been evaluated elsewhere, with negative urine culture, ultrasound and plain radiology and cystoscopy; the symptoms resolved for several months but then returned, and at presentation, she was passing visibly blood-stained urine nearly every day. She had a history of chrondromalacia patellae, for which she had taken regular non-steroidal anti-inflammatory drugs. Loin pain and haematuria had worsened shortly after switching from ibuprofen to diclofenac for an exacerbation of knee pain which had continued despite successful arthroscopic knee surgery. There was a family history of von Willebrand’s disease, however, the patient’s clotting studies were normal. Repeat imaging had excluded nephrolithiasis. The pain was just manageable with regular morphine and amitriptyline. Estimated glomerular filtration rate was 96 mL/min/1.73m2 and urine protein:creatinine ratio was 33 mg/mmol.
The frequency and severity of macroscopic haematuria were atypical for glomerulonephritis, papillary necrosis or loin pain haematuria syndrome; the severity of the pain was atypical for renal arteriovenous malformations or nutcracker phenomenon. She was referred to a pain management service, and in view of the atypical presentation, magnetic resonance angiography was performed. There was evidence of partial occlusion of the left renal vein just before it entered the inferior vena cava as it passed between the aorta and superior mesenteric artery (Figures 1 and 2).
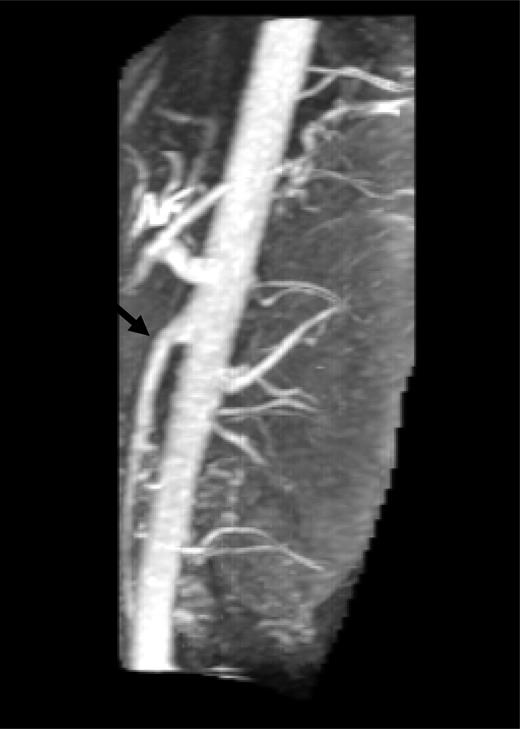
Lateral reconstruction of magnetic resonance imaging showing acute angle and narrow space (arrow) between superior mesenteric artery and aorta.
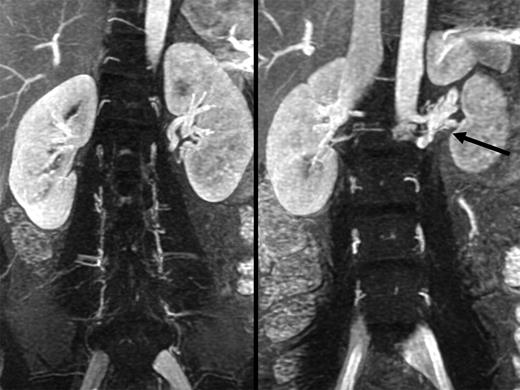
Composite coronal venous phase magnetic resonance angiogram images showing kidneys of equal size with venous congestion at the hilum of the left kidney. Congested partially obstructed left renal veins (arrow) are shown at the lateral margin of the aorta with poorly developed collaterals to lumbar veins. The absence of either a lieno-renal pathway or an incompetent ovarian vein may explain the severity of her symptoms.
After discussion of the relative risks and benefits of renal venous stenting and autotransplantation, the patient opted for the latter. Haematuria resolved 2 days after transplantation of the left kidney into the pelvis, and 2 months later, she was pain free and back to normal student life. There have been no post-operative complications in >3 years of follow-up, and renal excretory function remains normal.
Discussion
The loin pain haematuria syndrome is essentially a diagnosis of exclusion, particularly of urinary tract infection, nephrolithiasis, papillary necrosis and glomerulonephritis. We believe that this is the first time that the nutcracker phenomenon has been shown to mimic the condition.
The symptoms of nutcracker syndrome are a consequence of chronic obstruction of the left renal vein and its tributaries, which are the veins of the renal hilum, the suprarenal vein from above and the testicular or ovarian vein from below. Left-sided renal venous hypertension leads to dilatation of the tributaries and development of collaterals around the kidney and its ureter, and perhaps the venous congestion is responsible for the left flank pain. Rupture of venules in the collecting system leads to the typical unilateral haematuria and sometimes proteinuria, with pain in the left flank.
Obstruction to ovarian vein flow can cause the ‘pelvic congestion syndrome’—dysmenorrhoea, post-coital ache, dyspareunia and the formation of ovarian, pelvic, vulvar and sometimes gluteal vein varicosities [9]. There may even be venous involvement of the left lower limb. In the male, varicocoele is common. In a study of 93 patients with varicocoele, 28 were found to have obstruction to the left renal vein—compared with 2 of 76 controls [10].
In the case of the patient described here, it is possible that the severity of the symptoms was a result of her particular anatomy. The lack of either a lienorenal pathway or of collaterals between the left renal vein and lumbar veins on imaging meant that there was no ‘run-off’ to dissipate the high venous pressure. Imaging also demonstrated that the valve at the junction of the left ovarian vein with the left renal vein was not incompetent.
Our case illustrates the importance of keeping an open mind when seeing patients with loin pain and haematuria.
Conflict of interest statement. None declared.





Comments