-
PDF
- Split View
-
Views
-
Cite
Cite
Thamer H. Alenazi, Hussain Al Arbash, Aiman El-Saed, Majid M. Alshamrani, Henry Baffoe-Bonnie, Yaseen M. Arabi, Sameera M. Al Johani, Ra’ed Hijazi, Adel Alothman, Hanan H. Balkhy, Identified Transmission Dynamics of Middle East Respiratory Syndrome Coronavirus Infection During an Outbreak: Implications of an Overcrowded Emergency Department, Clinical Infectious Diseases, Volume 65, Issue 4, 15 August 2017, Pages 675–679, https://doi.org/10.1093/cid/cix352
Close - Share Icon Share
Abstract
A total 130 cases of Middle East respiratory syndrome coronavirus were identified during a large hospital outbreak in Saudi Arabia; 87 patients and 43 healthcare workers. The majority (80%) of transmission was healthcare-acquired (HAI) infection, with 4 generations of HAI transmission. The emergency department was the main location of exposure.
Middle East respiratory syndrome coronavirus (MERS-CoV) has a predilection to cause healthcare-associated outbreaks. The virus caused at least 9 hospital outbreaks in Saudi Arabia between 2013 and 2015 [1–7] and a major outbreak in Korea in 2015 [8, 9]. These repeated outbreaks may indicate enhanced viral transmission in the healthcare setting. Better understanding of the viral transmission during an outbreak can potentially improve future preventive measures in similar outbreaks. Our objective in this study was to investigate the transmission pattern of MERS-CoV during the 2015 hospital outbreak in Riyadh, Saudi Arabia.
METHODS
Setting
The current study was conducted at King Abdulaziz Medical City-Riyadh (KAMC-R), Ministry of National Guard Health Affairs in Saudi Arabia. KAMC-R is a 1000-bed tertiary care facility. It has 13 intensive care units (ICUs) (single-rooms) and 36 wards (single/double/quadruple rooms). The emergency department (ED) consists of 3 sections (total 150 beds) each of which has an open bay separated by curtains/cubicles, with gender-specific common bathrooms and common waiting area. KAMC-R has 56 single negative-pressure rooms dedicated for isolation, including 10 rooms in the ED and 1–2 rooms in each ICU and most wards.
Study Design
The study design was a prospective surveillance study for all suspected patients and exposed healthcare workers (HCWs) at KAMC-R during the outbreak period of mid-June 2015 to mid-September 2015.
Infection Control Measures
At the beginning of the outbreak a ward was dedicated for isolation (droplet/contact isolation for suspected cases and airborne/contact isolation for probable and confirmed cases), and strict compliance with hand hygiene and use of personal protective equipment (PPE) was stressed in compliance with the Saudi Ministry of health guidelines. PPE included surgical masks with suspected patients and N-95 with probable or confirmed patients, in addition to gloves, yellow gowns, and eye protection. As the situation escalated, stricter measures were implemented, including airborne/contact isolation for all cases, additional locations (2 wards and 1 ICU) dedicated for isolation, more rooms converted to negative-pressure rooms, and finally shutdown of hospital services until the outbreak was cleared.
Case Definition
The case definition used was based on the definition update released by the Saudi Ministry of Health in June 2015 [10]. Exposed HCWs were defined as those who had been working in KAMC-R during the outbreak period and who had direct exposure (within 2 meters) or indirect exposure (being in the same room/department) to a confirmed or probable case with MERS-CoV infection within the last 2 weeks of exposure (regardless of symptoms) without wearing the proper PPE. Suspected patients [10] or exposed HCWs were considered confirmed or probable when a real-time polymerase chain reaction test for MERS-CoV was positive or inconclusive, respectively [10].
Transmission and Other Definitions
Community-acquired infection (CAI, primary) was defined as having confirmed or probable MERS-CoV diagnosis on admission, without prior hospital exposure over the last 2 weeks. Healthcare-acquired infection (HAI) was defined as having confirmed or probable MERS-CoV diagnosis during admission/employment in the hospital. HAI link was documented based on history and mapping the shared time and geographic locations.
RESULTS
During the outbreak, 130 confirmed cases were identified, including 26 (20.0%) CAI patients, 61 (46.9%) HAI patients, and 43 (33.1%) HAI HCWs. The ED was the probable location of exposure in 53.8% (N = 56/104) of the cases, followed by inpatient wards (22.1%), outpatient clinics (9.6%), ICUs (5.8%), and other hospital locations (8.7%). The attack rate for HCWs who were working in the ED (2.70%) was significantly higher (P < .001) than the attack rates for those working in other locations including ICUs (0.64%), inpatients wards (0.28%), outpatient clinics (0.31%), and other hospital locations (0.17%). The attack rates were slightly but insignificantly higher among nurses (0.58%) than physicians (0.30%) and other HCWs (0.39%) and among females (0.51%) than males (0.37%).
Four generations of HAI transmission (N = 85) were identified: 44 secondary, 25 tertiary, 13 quaternary, and 3 quinary Figure 1. The average number of MERS-CoV HAI transmissions per patient (transmissibility index) was 4.00 for CAI patients with primary transmission, 0.98 for secondary HAI, 0.64 for tertiary HAI, 0.23 for quaternary HAI, and zero for quinary HAI transmissions. On the other hand, 6 patients with MERS-CoV (4 CAI and 2 HAI) were responsible for 61 (58.7%) HAI transmissions. Although not significant, they tended to have early presentation, late diagnosis, and longer hospital stay.
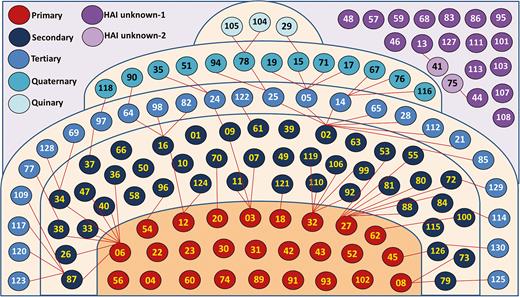
Types of transmission of Middle East respiratory syndrome infection during the outbreak. Primary (N = 26) is a community transmission, while secondary (N = 44), tertiary (N = 25), quaternary (N = 13), and quinary (N = 3) are healthcare-associated infection (HAI) transmissions. The number of cases (circles) represents the chronological sequence of onset of symptoms, not the hospital presentation. Red lines indicate identified transmission from lower to higher generation. Tertiary, quaternary, and quinary HAI transmissions were assigned only when the source patients and their generations were identified. In some secondary HAI cases, lack of connection to primary cases indicates that a source patient could not be confirmed. Unknown (violet) HAI cases indicate that the source and the generation of HAI transmission could not be identified and were mainly healthcare workers. Abbreviations: HAI, healthcare-associated infection; MERS-CoV, Middle East respiratory syndrome coronavirus.
Tracking the movements of hospitalized cases inside KAMC-R during the outbreak is shown in Figure 2. Of the 96 hospitalized cases, the ED was the source of admission in 89 (92.7%). Additionally, 63 (65.6%) had ICU admissions, 77 (80.2%) had ward admissions, and 45 (46.9%) had both ICU and ward admissions. Approximately 64 (83.1%) of the ward admissions were in designated MERS-CoV isolation wards.
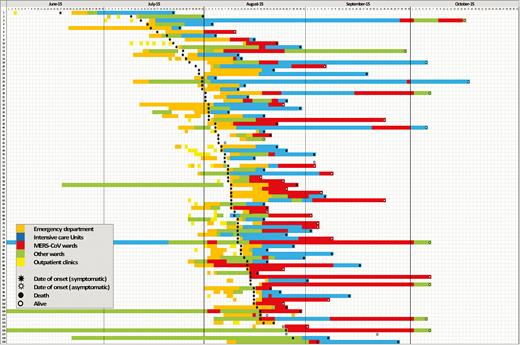
Track of movements of hospitalized cases inside the King Abdulaziz Medical City-Riyadh during the outbreak. The stars and circles show the symptoms and death status, respectively. The number of cases represents the chronological sequence of onset of symptoms. Home isolation cases were not included in the figure.
Demographic and clinical characteristics of the cases are detailed in Table 1. Compared to HAI HCWs, both CAI and HAI patients were more likely to be older, of male gender, have symptomatic disease, and have comorbidity burden. Case fatality was highest among HAI patients (N = 40/61, 65.5%) than CAI patients (N = 11/26, 42.3%), but no deaths were recorded among HAI HCWs (N = 0/43). Approximately, two-thirds of hospitalized patients required ICU admission or ventilation, with no significant differences between groups.
| Characteristic . | CAI Patients (N = 26) . | HAI Patients (N = 61) . | HAI HCWs (N = 43) . | P Value . |
|---|---|---|---|---|
| Age, y | 63.5 ± 18.9 | 64.7 ± 18.2 | 40.1 ± 11.3 | <.001a,b |
| Gender | ||||
| Male | 17 (65.4%) | 39 (63.9%) | 10 (23.3%) | <.001a,b |
| Female | 9 (34.6%) | 22 (36.1%) | 33 (76.7%) | … |
| Symptoms | ||||
| Any symptoms | 26 (100.0%) | 58 (95.1%) | 25 (58.1%) | <.001a,b |
| Respiratory | 24 (92.3%) | 56 (96.6%) | 24 (96.0%) | .828 |
| Fever | 24 (92.3%) | 47 (81.0%) | 17 (68.0%) | .103a |
| Constitutional, excluding fever | 14 (53.8%) | 38 (65.5%) | 14 (56.0%) | .521 |
| Gastrointestinal | 12 (46.2%) | 27 (46.6%) | 4 (16.0%) | .024a,b |
| Any comorbid diseases | ||||
| No | 1 (3.8%) | 0 (0.0%) | 25 (58.1%) | <.001a,b |
| Yes | 25 (96.2%) | 61 (100.0%) | 18 (41.9%) | … |
| Diagnosis | ||||
| Confirmed | 18 (69.2%) | 49 (80.3%) | 14 (32.6%) | <.001a,b |
| Probable | 8 (30.8%) | 12 (19.7%) | 29 (67.4%) | … |
| Isolation | ||||
| Home isolation | 2 (7.7%) | 1 (1.6%) | 31 (72.1%) | <.001a,b |
| Hospitalization | 24 (92.3%) | 60 (98.4%) | 12 (27.9%) | |
| Number of movements (N = 96) | ||||
| Within emergency department | 3.3 ± 2.3 | 2.7 ± 1.3 | 1.4 ± 0.7 | .005a,b |
| Within King Abdulaziz Medical City-Riyadh | 5.8 ± 3.1 | 5.2 ± 2.5 | 3.7 ± 1.6 | .048a,b |
| Duration in hospital (days, N = 96) | ||||
| Duration of hospitalization | 20.5 (10.3,45.3) | 21.0 (12.5,37.0) | 23.5 (7.0,41.8) | .969 |
| Duration of ICU admission | 8.0 (3.0,22.0) | 8.5 (5.0,19.8) | 22.0 (10.0,49.0) | .160a |
| Outcome of hospitalization (N = 96) | ||||
| Need ICU admission | 15 (62.5%) | 40 (66.7%) | 8 (66.7%) | .950 |
| Need ventilation | 15 (62.5%) | 38 (63.3%) | 7 (58.3%) | .953 |
| Expired | 11 (45.8%) | 40 (66.7%) | 0 (0.0%) | <.001a,b |
| Discharged | 13 (54.2%) | 20 (33.3%) | 12 (100.0%) | <.001a,b |
| Characteristic . | CAI Patients (N = 26) . | HAI Patients (N = 61) . | HAI HCWs (N = 43) . | P Value . |
|---|---|---|---|---|
| Age, y | 63.5 ± 18.9 | 64.7 ± 18.2 | 40.1 ± 11.3 | <.001a,b |
| Gender | ||||
| Male | 17 (65.4%) | 39 (63.9%) | 10 (23.3%) | <.001a,b |
| Female | 9 (34.6%) | 22 (36.1%) | 33 (76.7%) | … |
| Symptoms | ||||
| Any symptoms | 26 (100.0%) | 58 (95.1%) | 25 (58.1%) | <.001a,b |
| Respiratory | 24 (92.3%) | 56 (96.6%) | 24 (96.0%) | .828 |
| Fever | 24 (92.3%) | 47 (81.0%) | 17 (68.0%) | .103a |
| Constitutional, excluding fever | 14 (53.8%) | 38 (65.5%) | 14 (56.0%) | .521 |
| Gastrointestinal | 12 (46.2%) | 27 (46.6%) | 4 (16.0%) | .024a,b |
| Any comorbid diseases | ||||
| No | 1 (3.8%) | 0 (0.0%) | 25 (58.1%) | <.001a,b |
| Yes | 25 (96.2%) | 61 (100.0%) | 18 (41.9%) | … |
| Diagnosis | ||||
| Confirmed | 18 (69.2%) | 49 (80.3%) | 14 (32.6%) | <.001a,b |
| Probable | 8 (30.8%) | 12 (19.7%) | 29 (67.4%) | … |
| Isolation | ||||
| Home isolation | 2 (7.7%) | 1 (1.6%) | 31 (72.1%) | <.001a,b |
| Hospitalization | 24 (92.3%) | 60 (98.4%) | 12 (27.9%) | |
| Number of movements (N = 96) | ||||
| Within emergency department | 3.3 ± 2.3 | 2.7 ± 1.3 | 1.4 ± 0.7 | .005a,b |
| Within King Abdulaziz Medical City-Riyadh | 5.8 ± 3.1 | 5.2 ± 2.5 | 3.7 ± 1.6 | .048a,b |
| Duration in hospital (days, N = 96) | ||||
| Duration of hospitalization | 20.5 (10.3,45.3) | 21.0 (12.5,37.0) | 23.5 (7.0,41.8) | .969 |
| Duration of ICU admission | 8.0 (3.0,22.0) | 8.5 (5.0,19.8) | 22.0 (10.0,49.0) | .160a |
| Outcome of hospitalization (N = 96) | ||||
| Need ICU admission | 15 (62.5%) | 40 (66.7%) | 8 (66.7%) | .950 |
| Need ventilation | 15 (62.5%) | 38 (63.3%) | 7 (58.3%) | .953 |
| Expired | 11 (45.8%) | 40 (66.7%) | 0 (0.0%) | <.001a,b |
| Discharged | 13 (54.2%) | 20 (33.3%) | 12 (100.0%) | <.001a,b |
Data are presented as number and percentage except age, which is presented as mean ± standard deviation, and duration in hospital, which is presented as median and interquartile range (IQR). χ2 or Fisher exact tests, as appropriate, were used to test significant differences of categorical variables while analysis of variance or Kruskal-Wallis test, as appropriate, were used to test significant differences of continuous variables.
Abbreviations: CAI, community-acquired infection; HAI, healthcare-acquired infection; HCW, healthcare worker; ICU, intensive care unit.
aIndicates significant difference between CAI patients and HAI HCWs.
bIndicates significant difference between HAI patients and HAI HCWs.
| Characteristic . | CAI Patients (N = 26) . | HAI Patients (N = 61) . | HAI HCWs (N = 43) . | P Value . |
|---|---|---|---|---|
| Age, y | 63.5 ± 18.9 | 64.7 ± 18.2 | 40.1 ± 11.3 | <.001a,b |
| Gender | ||||
| Male | 17 (65.4%) | 39 (63.9%) | 10 (23.3%) | <.001a,b |
| Female | 9 (34.6%) | 22 (36.1%) | 33 (76.7%) | … |
| Symptoms | ||||
| Any symptoms | 26 (100.0%) | 58 (95.1%) | 25 (58.1%) | <.001a,b |
| Respiratory | 24 (92.3%) | 56 (96.6%) | 24 (96.0%) | .828 |
| Fever | 24 (92.3%) | 47 (81.0%) | 17 (68.0%) | .103a |
| Constitutional, excluding fever | 14 (53.8%) | 38 (65.5%) | 14 (56.0%) | .521 |
| Gastrointestinal | 12 (46.2%) | 27 (46.6%) | 4 (16.0%) | .024a,b |
| Any comorbid diseases | ||||
| No | 1 (3.8%) | 0 (0.0%) | 25 (58.1%) | <.001a,b |
| Yes | 25 (96.2%) | 61 (100.0%) | 18 (41.9%) | … |
| Diagnosis | ||||
| Confirmed | 18 (69.2%) | 49 (80.3%) | 14 (32.6%) | <.001a,b |
| Probable | 8 (30.8%) | 12 (19.7%) | 29 (67.4%) | … |
| Isolation | ||||
| Home isolation | 2 (7.7%) | 1 (1.6%) | 31 (72.1%) | <.001a,b |
| Hospitalization | 24 (92.3%) | 60 (98.4%) | 12 (27.9%) | |
| Number of movements (N = 96) | ||||
| Within emergency department | 3.3 ± 2.3 | 2.7 ± 1.3 | 1.4 ± 0.7 | .005a,b |
| Within King Abdulaziz Medical City-Riyadh | 5.8 ± 3.1 | 5.2 ± 2.5 | 3.7 ± 1.6 | .048a,b |
| Duration in hospital (days, N = 96) | ||||
| Duration of hospitalization | 20.5 (10.3,45.3) | 21.0 (12.5,37.0) | 23.5 (7.0,41.8) | .969 |
| Duration of ICU admission | 8.0 (3.0,22.0) | 8.5 (5.0,19.8) | 22.0 (10.0,49.0) | .160a |
| Outcome of hospitalization (N = 96) | ||||
| Need ICU admission | 15 (62.5%) | 40 (66.7%) | 8 (66.7%) | .950 |
| Need ventilation | 15 (62.5%) | 38 (63.3%) | 7 (58.3%) | .953 |
| Expired | 11 (45.8%) | 40 (66.7%) | 0 (0.0%) | <.001a,b |
| Discharged | 13 (54.2%) | 20 (33.3%) | 12 (100.0%) | <.001a,b |
| Characteristic . | CAI Patients (N = 26) . | HAI Patients (N = 61) . | HAI HCWs (N = 43) . | P Value . |
|---|---|---|---|---|
| Age, y | 63.5 ± 18.9 | 64.7 ± 18.2 | 40.1 ± 11.3 | <.001a,b |
| Gender | ||||
| Male | 17 (65.4%) | 39 (63.9%) | 10 (23.3%) | <.001a,b |
| Female | 9 (34.6%) | 22 (36.1%) | 33 (76.7%) | … |
| Symptoms | ||||
| Any symptoms | 26 (100.0%) | 58 (95.1%) | 25 (58.1%) | <.001a,b |
| Respiratory | 24 (92.3%) | 56 (96.6%) | 24 (96.0%) | .828 |
| Fever | 24 (92.3%) | 47 (81.0%) | 17 (68.0%) | .103a |
| Constitutional, excluding fever | 14 (53.8%) | 38 (65.5%) | 14 (56.0%) | .521 |
| Gastrointestinal | 12 (46.2%) | 27 (46.6%) | 4 (16.0%) | .024a,b |
| Any comorbid diseases | ||||
| No | 1 (3.8%) | 0 (0.0%) | 25 (58.1%) | <.001a,b |
| Yes | 25 (96.2%) | 61 (100.0%) | 18 (41.9%) | … |
| Diagnosis | ||||
| Confirmed | 18 (69.2%) | 49 (80.3%) | 14 (32.6%) | <.001a,b |
| Probable | 8 (30.8%) | 12 (19.7%) | 29 (67.4%) | … |
| Isolation | ||||
| Home isolation | 2 (7.7%) | 1 (1.6%) | 31 (72.1%) | <.001a,b |
| Hospitalization | 24 (92.3%) | 60 (98.4%) | 12 (27.9%) | |
| Number of movements (N = 96) | ||||
| Within emergency department | 3.3 ± 2.3 | 2.7 ± 1.3 | 1.4 ± 0.7 | .005a,b |
| Within King Abdulaziz Medical City-Riyadh | 5.8 ± 3.1 | 5.2 ± 2.5 | 3.7 ± 1.6 | .048a,b |
| Duration in hospital (days, N = 96) | ||||
| Duration of hospitalization | 20.5 (10.3,45.3) | 21.0 (12.5,37.0) | 23.5 (7.0,41.8) | .969 |
| Duration of ICU admission | 8.0 (3.0,22.0) | 8.5 (5.0,19.8) | 22.0 (10.0,49.0) | .160a |
| Outcome of hospitalization (N = 96) | ||||
| Need ICU admission | 15 (62.5%) | 40 (66.7%) | 8 (66.7%) | .950 |
| Need ventilation | 15 (62.5%) | 38 (63.3%) | 7 (58.3%) | .953 |
| Expired | 11 (45.8%) | 40 (66.7%) | 0 (0.0%) | <.001a,b |
| Discharged | 13 (54.2%) | 20 (33.3%) | 12 (100.0%) | <.001a,b |
Data are presented as number and percentage except age, which is presented as mean ± standard deviation, and duration in hospital, which is presented as median and interquartile range (IQR). χ2 or Fisher exact tests, as appropriate, were used to test significant differences of categorical variables while analysis of variance or Kruskal-Wallis test, as appropriate, were used to test significant differences of continuous variables.
Abbreviations: CAI, community-acquired infection; HAI, healthcare-acquired infection; HCW, healthcare worker; ICU, intensive care unit.
aIndicates significant difference between CAI patients and HAI HCWs.
bIndicates significant difference between HAI patients and HAI HCWs.
DISCUSSION
We identified a significant level of in-hospital transmission of MERS-CoV during management of a major outbreak in the summer of 2015. We identified 4 generations of in-hospital transmission, obviously with decreasing number of newly infected cases (transmissibility index) in each next higher generation. This was slightly more than what has been described in previous outbreaks but still within the expected range considering the size of our outbreak. In fact, secondary and tertiary cases have been reported in community clusters and hospital outbreaks in Saudi Arabia [2, 11]. Moreover, secondary, tertiary, and quaternary in-hospital transmissions were reported in the Korean outbreak [9]. A recent risk assessment of MERS-CoV cases from the Korean and Middle East outbreaks estimated the risks of having secondary, tertiary, quaternary, quinary, and beyond quinary hospital transmission at 22.7%, 10.5%, 6.1%, 3.9%, and 2%, respectively [12]. In the current outbreak, tertiary, quaternary, and quinary generations represented 24%, 13%, and 3% of all hospital-acquired transmissions. It appeared that the longer the delay in interrupting the chain of transmission through proper infection control measures, the more generations of transmission will take place [9].
We could not identify the source of infection or the generation of transmission for 19 HAI cases. They were mainly HCWs (N = 16/19, 84.2%) who moved around the hospital and were probably exposed to multiple symptomatic and asymptomatic cases and probably unrecognized cases. It is important to mention that elucidating the source and generation of transmission is not always an easy and accurate job as may be thought, especially during a large hospital outbreak with busy dynamic units and a large number of new cases in a short period of time [9]. Additionally, we cannot exclude environmental contamination as a potential source of transmission [13].
Community cases in the current study continued to introduce the virus into the hospital throughout the outbreak and represent the main source of infection. The current percentage of CAI was similar to what was observed in the large multihospital MERS-CoV outbreak in Jeddah, Saudi Arabia, in the first half of 2014 [3]. Additionally, it is not uncommon that very few community-acquired cases can lead to a major outbreak [1, 14]. Before the outbreak, a seroprevalence study projected that 0.15% of the community in Saudi Arabia has been exposed to the virus [15]. However, due to the lack of accurate and continuous community monitoring [16], we cannot prove or exclude the presence of a community outbreak at the time of our hospital outbreak.
More than half of our HAI cases probably were infected in the ED. This was probably due to overcrowding, high traffic, poor layout of the ED that allowed transmission, inadequate triage, and multiple movements within the ED sections. Interestingly, the current data show that cases who were infected while in the ED had significantly longer hospital stays and higher mortality outcomes. The role of the ED in spreading healthcare-related MERS-CoV infection has been reported previously [2, 4, 17]. For example, in the largest single hospital cluster in the 2015 Korean MERS-CoV outbreak, 81 (89%) of the 91 HAI cases were infected in the ED [17]. Overcrowded healthcare facilities, particularly EDs, were identified as a major cause for MERS-CoV outbreaks, which by default means poor compliance with infection control practices [4, 7, 18].
In summary, we reconfirm the high preference of MERS-CoV for the healthcare environment, which can at times lead to explosive outbreaks. We report several generations of intrahospital transmission with significant transmission in our busy ED. Hospitals are encouraged to set strong infection control practices and effective crowd control, triage systems, and surveillance programs to evade such catastrophes, regardless of the type of seasonal or emerging respiratory pathogen.
Notes
Acknowledgments. We greatly appreciate the contributions of all data collectors, who made this study possible.
Potential conflicts of interests. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
Author notes
T. H. A. and H. A. contributed equally to this work.
Correspondence: H. H. Balkhy, Pediatric Infectious Disease, King Saud bin Abdulaziz University for Health Sciences; Infectious Diseases, King Abdullah International Medical Research Center; Infection Prevention and Control, King Abdulaziz Medical City, Riyadh, Saudi Arabia P.O. Box 22490, Riyadh 11426, Kingdom of Saudi Arabia ([email protected], [email protected]).




