-
PDF
- Split View
-
Views
-
Cite
Cite
Chen Zhang, Yurui Shi, Shanshan Du, Hongsen Bi, Aesthetic Enhancement of the Gonial Angle and Inferior Mandibular Border in the Chinese Population, Aesthetic Surgery Journal, Volume 44, Issue 1, January 2024, Pages NP16–NP22, https://doi.org/10.1093/asj/sjad318
Close - Share Icon Share
Abstract
The current absence of a standardized mandibular body osteotomy design poses challenges in surgical planning. Traditional approaches may not suit patients with wider anterior mandibles, potentially resulting in unsatisfactory outcomes. Addressing this issue requires a rational design that combines mandibular angle and body osteotomies for improved clinical practice.
In this retrospective cohort study we aimed to analyze mandibular computed tomography (CT) data with digital methods. The goal was to establish an integrated osteotomy design for both mandibular angle and body procedures and classify prevalent mandibular types in the Chinese Han population for surgical guidance.
Included were 89 patients who underwent mandibular angle osteotomy without genioplasty between 2016 and 2022 at Peking University Third Hospital. Mimics 21.0 software facilitated CT data reconstruction and osteotomy planning. Postoperative effects were assessed through imaging, complications, and surveys, leading to mandibular type classification.
Mandibular angles were categorized by 3 types, based on osteotomy range. Type I involved mandibular body osteotomy only, type II mandibular angle osteotomy only, and type III both mandibular angle and body osteotomies. Distribution within the cohort was 2.25%, 8.99%, and 88.76% for types I, II, and III respectively. Patient satisfaction was high, with minor and major complications at 47.19% and 1.12% by Clavien-Dindo classification.
Utilizing Mimics software, we established an integrated osteotomy design and categorized mandibular types. Findings offer valuable guidance for mandibular angle surgery and contribute to understanding of Asian mandibular morphology.

According to the aesthetic standards of the East Asian population, a “square face” is often considered rough and lacking delicacy, lacking the soft beauty that is the mainstream aesthetic preference for an “oval face” or an “egg-shaped face.” Mandibular angle reduction surgery is a popular cosmetic procedure in Asian countries, specifically designed to address the wide and protruding lower jaw that is characteristic of square face syndrome.1
Prominent mandibular angle, also known as “square jaw deformity,” is primarily characterized by an enlarged lower jaw caused by excessive protrusion or outward rotation of the mandibular angles. It is often due to bony overgrowth and may also be associated with varying degrees of masseter muscle hypertrophy and cheek fullness, with the exact etiology remaining unclear. The pathological changes primarily involve abnormal mandibular bone development and thickening of the masseter muscle.2 Baek et al have indicated that the pathological changes associated with a prominent mandibular angle include abnormal mandibular angle growth and development, as well as masseter muscle hypertrophy. The degree of prominent mandibular angle can be influenced by various factors, including the angle of the mandibular angles, the angle of outward rotation of the mandibular body, and the degree of masseter muscle hypertrophy.3
There are 3 main surgical procedures currently used for mandibular angle reduction: simple masseter muscle resection, mandibular angle osteotomy, and mandibular angle osteotomy combined with masseter muscle resection. For the East Asian population, a prominent mandibular angle is primarily due to bony overgrowth of the mandibular angles rather than masseter muscle hypertrophy; therefore, mandibular angle osteotomy is often the preferred treatment method.4 Common osteotomy techniques include straight-line osteotomy, multiple straight–line osteotomy, curved osteotomy, long curved osteotomy, and vertical splitting osteotomy of the mandibular outer cortex.2,5-10 The appropriate osteotomy technique should be selected based on the patient's specific condition. However, the current mainstream surgical approach focuses on the smooth contour of the mandibular angle region and avoiding secondary mandibular angle formation after surgery. There is currently no mature and standardized osteotomy design plan for the mandibular body. For some patients with wider and poorly shaped anterior mandibles, traditional surgical plans may lead to narrower lower facial width after mandibular angle osteotomy, resulting in an excessively wide mandibular body appearance and unsatisfactory surgical outcomes. Therefore, it is important to design a rational mandibular body osteotomy plan and integrate it with the mature mandibular angle osteotomy plan in clinical practice.
In this study, we applied Mimics software to measure and analyze the mandible, developed an integrated osteotomy design plan for the mandibular angle region and body, achieved satisfactory clinical results, and subsequently classified common nonaesthetic mandibular shapes among the Chinese Han population, aiming to provide guidance for subsequent surgical treatments.
METHODS
Patients
This retrospective cohort study included 89 patients (17 males and 72 females) who underwent mandibular angle osteotomy without concurrent genioplasty surgery in the Department of Craniofacial Surgery at Peking University Third Hospital between January 2016 and January 2022. All patients were Chinese Han citizens, aged 18 to 42 years with a mean age of 26.69 ± 5.58 years. Patients with a history of facial trauma or inflammation before mandibular angle osteotomy surgery were excluded. Three-dimensional reconstruction of craniofacial CT scans was performed before and within 1 week after the surgery. All patients provided informed consent for the use of their clinical data for academic research. All patients had no complaints of facial pain and had normal jaw opening and chewing function before surgery. Real-name appearance satisfaction questionnaires (Appendix, available at www.aestheticsurgeryjournal.com) distributed by the surgeon were completed by the patients at the preoperative visit and 6 months postoperatively on paper. (In the context of patients who are unable to physically visit the medical facility due to local COVID-19 policies, the questionnaire survey was administered online.) Postoperative complications were evaluated with the Clavien-Dindo classification, with grade IIIa or higher indicating severe complications (Supplemental Table 1, available at www.aestheticsurgeryjournal.com).11 This study was approved by the Ethics Committee of Peking University Third Hospital (215-02).
Study Tools
Craniofacial 3-dimensional (3D) CT scans were performed with a dual-source CT scanner (SOMATOM Definition Flash 128 Rao; Siemens, Germany) with a voltage of 120 kV, mA of 270, slice thickness of 5 mm, exposure time of 34 seconds, and pitch of 0.531. The scan range extended from the top of the skull to the mandible. The scans were reconstructed with a slice thickness of 1 mm, a matrix size of 512 × 512, and a reconstructed field of view of 20 mm.
Patient craniofacial CT raw data were imported into Mimics 21.0 (Materialise; Leuven, Belgium) to create a 3D cranial model. Mimics measurement data were imported into SPSS 21.0 (IBM; Armonk, NY) for data analysis. The bone tissue window was set to 226-3071 HU, and 3D reconstruction of the head and skull was performed.
Data Analysis and Design of the Osteotomy Line
An extension line was drawn backward along the occlusal plane until it intersected with the posterior border line of the mandible, and the intersection point was marked as point A (Figure 1A, B). A perpendicular line was drawn from the position of the first premolar tooth along the occlusal plane, extending downward until it intersected with the lower border of the mandible, and the intersection point was marked as point B. A straight line was drawn upward and backward from point B until it intersected with the posterior border of the mandible at point C, such that ∠ACB was 120° to 140°; the specific angle was set according to the patient's needs for a gentle or sharp jawline contour. The occlusal plane line intersected with the anterior border of the mandibular ramus at point D. A perpendicular line was drawn downward from point D along the occlusal plane until it intersected with line Bc at point E. Line BE was the benchmark osteotomy line for the mandibular body, along which a straight osteotomy was performed. Line AE was the benchmark osteotomy line for the mandibular angle, along which a curved osteotomy was performed, according to the patient's needs for a gentle or sharp jawline contour. Point E was the location of the 2 osteotomy transitions, and attention was paid to ensure a smooth transition during the osteotomy to avoid the formation of a second mandibular angle (Figure 1A).
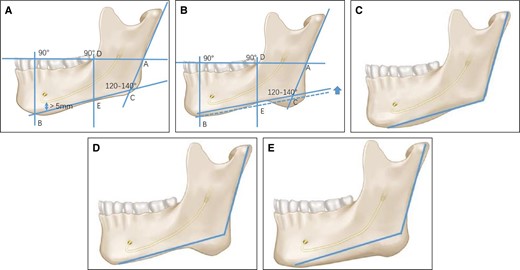
(A) Design of the osteotomy line. (B) Special situation 1 in the design of the osteotomy line: If a gap exists between line Bc and the mandibular lower border, line Bc is shifted upward in parallel while maintaining its angle with the mandibular posterior border until it intersects at point E. (C) Type I of the mandibular angle according to the osteotomy range. (D) Type II of the mandibular angle according to the osteotomy range. (E) Type III of the mandibular angle according to the osteotomy range.
There were 2 special situations: (1) If there was a gap between line Bc and the lower border of the mandible, line Bc was moved upward in parallel, and the angle between line Bc and the posterior border line of the mandible was maintained until it intersected with the lower border of the mandible at point E (Figure 1B). (2) If line Bc overlapped with the mandibular nerve canal or was within 0.5 cm below the lower border of the mandibular nerve canal, line Bc was moved downward in parallel, and the angle between line Bc and the posterior border of the mandible was maintained until line Bc no longer overlapped with the mandibular nerve canal and was at least 0.5 cm above the lower border of the mandibular nerve canal. If this standard conflicted with the first special case, the latter standard prevailed. Usually, to achieve a better surgical outcome, the thick cortical bone at the external oblique line of the mandible was also smoothed during the surgery.
Surgical Methods
All surgeries were performed under general anesthesia with the patient in the lithotomy position. On the right side, an incision was made from the anterior vestibular groove of the first premolar to the anterior border of the mandibular ramus, reaching the periosteum. Subperiosteal dissection was performed to expose the lateral aspect of the mandible, extending from the lower edge of the mandibular body to the mandibular angle, while detaching the attachment of the masseter muscle. The mandibular outer plate grinding area was delineated, and an air-powered bur was used to grind and remove excessive bone tissue while being sure not to expose the medullary bone. The mandibular osteotomy line was marked based on preoperative planning and intraoperative conditions, carefully avoiding the inferior alveolar nerve canal and the mental foramen. Bone cutting was done with an air-powered oscillating saw, following the designed osteotomy line. The same procedure was performed on the left side. Hemostasis was achieved, and the mucosal incision was sutured with 4-0 absorbable sutures (Vicryl Plus; Johnson & Johnson, New Brunswick, NJ). One drainage tube was placed on each side. An elastic compression face mask was used for pressure application and fixation.
RESULTS
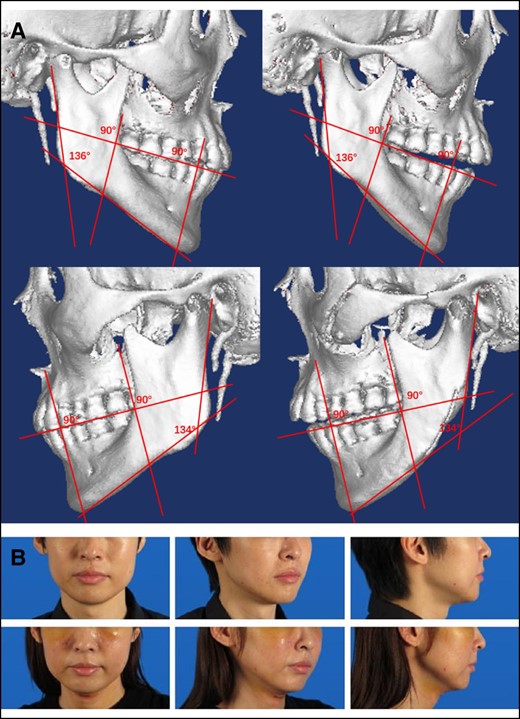
A total of 89 patients (17 males and 72 females) who underwent mandibular angle osteotomy without concurrent genioplasty surgery were included in this study. All patients were Chinese Han citizens, aged 18 to 42 years with a mean age of 26.69 ± 5.58 years. The postoperative follow-up was 6 to 12 months (average 9 months). According to the scope of bone cutting, the mandibular angle could be classified into 3 types (Figure 1C-E). Type I only required bone cutting in the mandibular body, without bone cutting in the mandibular angle (Figure 1C). Type II only required bone cutting in the mandibular angle, without bone cutting in the mandibular body (Figure 1D). Type III required bone cutting in both the mandibular body and the mandibular angle (Figure 1E). The proportions of each type are shown in Table 1. Typical cases of each type are shown in Figures 2 through 4. Postoperative CT measurements showed that the actual angle of bone cutting was 120° to 140°, with an average of 127.83 ± 5.13°. Among them, the angle for females was 120° to 140°, with an average of 128.25 ± 5.15°; for males it was 120° to 135°, with an average of 126.06 ± 4.61. There was no significant difference among the groups (P > .05).

(A) Three-dimensional computed tomography scan of a typical case of type I mandibular angle osteotomy. The upper row is on the right side, and the lower row is on the left side. (B) Preoperative (upper row) and 6-month postoperative (lower row) photographs of a 26-year-old female patient who represents a typical case of type I mandibular angle osteotomy.
(A) Three-dimensional computed tomography scan of a typical case of type II mandibular angle osteotomy. The upper row is on the right side, and the lower row is on the left side. (B) Preoperative (upper row) and 6-month postoperative (lower row) photographs of a 32-year-old male patient who represents a typical case of type II mandibular angle osteotomy.

(A) Three-dimensional computed tomography scan of a typical case of type III mandibular angle osteotomy. The upper row is on the right side, and the lower row is on the left side. (B) Preoperative (upper row) and 6-month postoperative (lower row) photographs of a 20-year-old female patient who represents a typical case of type III mandibular angle osteotomy.
| Cases . | Type I . | Type II . | Type III . |
|---|---|---|---|
| All cases | 2 | 8 | 79 |
| 2.25% | 8.99% | 88.76% | |
| Female | 1 | 7 | 64 |
| 1.39% | 9.72% | 88.89% | |
| Male | 1 | 1 | 15 |
| 5.88% | 5.88% | 88.24% |
| Cases . | Type I . | Type II . | Type III . |
|---|---|---|---|
| All cases | 2 | 8 | 79 |
| 2.25% | 8.99% | 88.76% | |
| Female | 1 | 7 | 64 |
| 1.39% | 9.72% | 88.89% | |
| Male | 1 | 1 | 15 |
| 5.88% | 5.88% | 88.24% |
| Cases . | Type I . | Type II . | Type III . |
|---|---|---|---|
| All cases | 2 | 8 | 79 |
| 2.25% | 8.99% | 88.76% | |
| Female | 1 | 7 | 64 |
| 1.39% | 9.72% | 88.89% | |
| Male | 1 | 1 | 15 |
| 5.88% | 5.88% | 88.24% |
| Cases . | Type I . | Type II . | Type III . |
|---|---|---|---|
| All cases | 2 | 8 | 79 |
| 2.25% | 8.99% | 88.76% | |
| Female | 1 | 7 | 64 |
| 1.39% | 9.72% | 88.89% | |
| Male | 1 | 1 | 15 |
| 5.88% | 5.88% | 88.24% |
Postoperative hematoma occurred in 3 cases, with 2 cases of mild hematoma that did not require special treatment and resolved within 2 weeks after surgery, with a Clavien-Dindo score of I. There was 1 case of severe hematoma that required hematoma clearance surgery under local anesthesia on the second day after surgery and resolved, with a Clavien-Dindo score of IIIa. Lip numbness occurred in 40 cases after surgery, which did not require special treatment and gradually recovered within 6 to 12 months after surgery, with a Clavien-Dindo score of I. There were no complications such as infection, accidental fracture, temporomandibular joint dysfunction, facial nerve injury, or mental nerve disconnection. The total incidence of complications was 48.31% (43 cases), with a rate of mild complications of 47.19% (42 cases) and severe complications of 1.12% (1 case), according to the Clavien-Dindo grading system.
A questionnaire was used to investigate the satisfaction rate before and 6 months after surgery, which was divided into 4 levels (“very dissatisfied,” “dissatisfied,” “satisfied,” and “very satisfied,” with scores ranging from 1 to 4). There were no statistically significant differences in satisfaction rates among the groups before and after surgery (P < .05; Table 2).
| Scores . | 1 . | 2 . | 3 . | 4 . |
|---|---|---|---|---|
| Preoperative score of all cases | 68 | 21 | 0 | 0 |
| Postoperative score of all cases | 0 | 0 | 13 | 76 |
| Preoperative score of females | 53 | 19 | 0 | 0 |
| Postoperative score of females | 0 | 0 | 10 | 62 |
| Preoperative score of males | 15 | 2 | 0 | 0 |
| Postoperative score of males | 0 | 0 | 3 | 14 |
| Scores . | 1 . | 2 . | 3 . | 4 . |
|---|---|---|---|---|
| Preoperative score of all cases | 68 | 21 | 0 | 0 |
| Postoperative score of all cases | 0 | 0 | 13 | 76 |
| Preoperative score of females | 53 | 19 | 0 | 0 |
| Postoperative score of females | 0 | 0 | 10 | 62 |
| Preoperative score of males | 15 | 2 | 0 | 0 |
| Postoperative score of males | 0 | 0 | 3 | 14 |
aScores ranged from 1 to 4, with 1 indicating “very dissatisfied” and 4 indicating “very satisfied.”
| Scores . | 1 . | 2 . | 3 . | 4 . |
|---|---|---|---|---|
| Preoperative score of all cases | 68 | 21 | 0 | 0 |
| Postoperative score of all cases | 0 | 0 | 13 | 76 |
| Preoperative score of females | 53 | 19 | 0 | 0 |
| Postoperative score of females | 0 | 0 | 10 | 62 |
| Preoperative score of males | 15 | 2 | 0 | 0 |
| Postoperative score of males | 0 | 0 | 3 | 14 |
| Scores . | 1 . | 2 . | 3 . | 4 . |
|---|---|---|---|---|
| Preoperative score of all cases | 68 | 21 | 0 | 0 |
| Postoperative score of all cases | 0 | 0 | 13 | 76 |
| Preoperative score of females | 53 | 19 | 0 | 0 |
| Postoperative score of females | 0 | 0 | 10 | 62 |
| Preoperative score of males | 15 | 2 | 0 | 0 |
| Postoperative score of males | 0 | 0 | 3 | 14 |
aScores ranged from 1 to 4, with 1 indicating “very dissatisfied” and 4 indicating “very satisfied.”
DISCUSSION
In 1949, Adams et al first proposed an extraoral approach for mandibular angle osteotomy combined with partial resection of the masseter muscle. However, this surgical method has been abandoned due to the formation of prominent skin scars at the extraoral incision site, especially in yellow-skinned individuals who are more prone to scarring than white-skinned individuals.12 Converse et al proposed a single-line mandibular angle osteotomy through an intraoral approach, which solved the disadvantage of prominent skin scars caused by an extraoral incision and allowed the technique to be promoted and popularized.5 However, after a single-line osteotomy, a second mandibular angle is easily formed, resulting in a “horse-face” appearance and a less smooth and delicate lateral facial contour. Building on the work of previous researchers, Yang et al and Baek et al proposed a multiple-line osteotomy of the mandibular angle, which had a more curved contour on the side than a single-line osteotomy.2,6 However, the operation was more complex, and there was a risk of forming 2 or more mandibular angles and uneven cutting edges of the mandibular bone, with further complications. It had certain limitations and was suitable for patients with moderate to severe mandibular angle protrusion. In 1991, Jin et al reported the use of curved osteotomy to treat mandibular angle hypertrophy.7 Gui et al improved this technique and proposed a single curved mandibular angle osteotomy with an intraoral approach. This avoided multiple osteotomy surgeries and the formation of 2 or more mandibular angles, and resulted in a more natural lateral contour and a smoother cutting curve, which was consistent with the aesthetic views of East Asians. This has now become the mainstream technique.8,9 Chao et al further improved and reported on the long arc osteotomy technique and discussed the mandibular anterior section osteotomy approach, which achieved good postoperative results for the wide and deformed mandibular body. However, specific details regarding the quantitative design of the osteotomy lines for the mandibular body, and the junction between the angle and body osteotomy lines, were not provided.10
In this study, we based our design and procedure for mandibular osteotomy on the common aesthetic standards for East Asian individuals, with fixed anatomical markers on the mandible. Compared to previous investigations, this osteotomy approach encompassed both prominent design of the mandibular angle osteotomy and a continuation of osteotomy design into the wide mandibular body region. Furthermore, the osteotomy designs for these 2 anatomical areas were integrated into a cohesive scheme, facilitating improved alignment between the angle osteotomy line and the body osteotomy line. As a result, the postoperative contour of the mandibular lower border exhibited a smoother configuration. Furthermore, great care was taken to avoid damage to the mandibular nerve canal. In addition to the standard mandibular angle shape (120°-140°), a straight-line shape of the mandibular body from a lateral view was considered an important feature of perfect mandibular morphology. Therefore, a straight-line osteotomy was performed on the mandibular body, while an osteotomy with varying degrees of curvature was performed on the mandibular angle, depending on the patient's needs. Improvements in lateral contouring also improved facial appearance from both the front and the side. This was the goal of mandibular angle osteotomy surgery. The main postoperative complication of this osteotomy plan was numbness of the lower lip, which was generally caused by traction injury to the mental nerve during surgery and gradually recovered within 6 to 12 months after surgery, requiring no special treatment. The incidence of severe complications was only 1.12% (Clavien-Dindo grade IIIa or higher), which was no higher than that reported in other relevant literature. The osteotomy plan had a reliable design effect, and the satisfaction rate of patients after surgery was high. CT measurements after surgery showed that the actual osteotomy angle was basically the same among different gender groups, indicating that this osteotomy plan had gender universality.
Mandibular angle hypertrophy can be classified based on the different shapes of the mandibular angle. There are currently 2 commonly used classification methods for mandibular angle hypertrophy: (1) According to the shape of the mandibular angle bone, it can be classified as posterior protrusion type, outward rotation type, or posterior protrusion combined with outward rotation type. The posterior protrusion type is characterized by a backward and downward protrusion of the mandibular angle, with an angle of less than 110°; the outward rotation type is characterized by a significant outward rotation of the mandibular angle, resulting in a mandibular angle distance greater than the zygomatic distance; and the posterior protrusion combined with outward rotation type combines the characteristics of the 2 types. (2) Based on the shape of the mandibular angle bone and the characteristics of the lower facial contour, it can be classified as mild type, moderate type, severe type, or complex type. The mild type has a soft facial contour, but the angle of the mandibular angle decreases from the lateral view; the moderate type has a protruding mandibular angle with outward rotation; the severe type has a significant outward protrusion of the mandibular angle and hypertrophy of the masseter muscle; and the complex type has a mandibular angle that is significantly outwardly protruding and associated with a small chin deformity.
However, the above 2 common classification methods focus on the classification of the mandibular angle, without considering the impact of the wide shape of the mandibular body on appearance. Therefore, based on the clinical demand for long arch osteotomy and the location of the osteotomy, we have included the mandibular body as part of the classification criteria. Accordingly, the mandible is categorized by 3 types. Type I only requires osteotomy of the mandibular body, without osteotomy of the mandibular angle. Type II only requires osteotomy of the mandibular angle, without osteotomy of the mandibular body. Type III requires osteotomy of both the mandibular body and mandibular angle. Statistical analysis showed that type III was the most common, while type I and type II were less frequent. It is suggested that most cases of a prominent mandibular angle involve both the mandibular angle and mandibular body, and therefore simultaneous osteotomy is recommended. In this study, a case of a type I patient who underwent maxillofacial surgery with a LeFort 1 osteotomy, sagittal split ramus osteotomy, chin osteotomy, and mandibular angle osteotomy is shown (Figure 2A, B). This case indicates that traditional mandibular angle osteotomy surgery can only solve problems in the angle area, and patients may remain dissatisfied with the wide appearance of the mandibular body after surgery, with further mandibular body osteotomy surgery needed for treatment.
The potential limitation of this study is that it only included patients who underwent mandibular angle osteotomy without simultaneous chin osteotomy. For patients who were designated type I before surgery, the original mandibular lower edge extension line and mandibular posterior edge extension line were usually performed at a large angle, resulting in a long face appearance and an unsatisfactory chin position. If the osteotomy plan described in this study is used, a U-shaped osteotomy is performed, with limited chin position adjustment. Some patients may choose to undergo simultaneous chin osteotomy to achieve the desired surgical appearance. Combination of mandibular osteotomy surgery and chin osteotomy surgery and how to design the chin osteotomy plan will be further elaborated and reported in future studies.
CONCLUSIONS
In conclusion, we measured and analyzed the morphology of the mandibular region in patients’ craniofacial CT with Mimics software, based on the aesthetic standards of East Asians, and developed an integrated mandibular angle and body osteotomy design and process based on fixed anatomical markers of the mandible. This design is concise and clear, can fully guide the design of osteotomy lines for the mandibular angle and body, and can solve the problems of a prominent mandibular angle and mandibular body widening, achieving good surgical and aesthetic effects and high patient satisfaction after surgery. Based on this osteotomy design, we designated 3 types of mandible and conducted a preliminary study of their distribution across demographic groups. This study has significant implications for the guidance of mandibular angle surgery and morphological studies in East Asians.
Supplemental Material
This article contains supplemental material located online at www.aestheticsurgeryjournal.com.
Acknowledgments
Drs Zhang and Shi contributed equally to this work as co-first authors.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
This study was funded by the Chinese Association of Plastics and Aesthetics (A68491-08).
REFERENCES
Author notes
From the Department of Plastic Surgery, Peking University Third Hospital, Beijing 100191, China.



