-
PDF
- Split View
-
Views
-
Cite
Cite
Zhujun Li, Yarong Chi, Cheng Chen, Lin Jin, Jiuzuo Huang, Xiao Long, Nanze Yu, A Comprehensive Ultrasound Evaluation Approach of Lower Facial Structure Before Masseter Muscle Botulinum Toxin Injection, Aesthetic Surgery Journal, Volume 43, Issue 4, April 2023, Pages NP283–NP292, https://doi.org/10.1093/asj/sjac336
Close - Share Icon Share
Abstract
Masseter reduction by botulinum neurotoxin A (BoNT-A) injection is a popular procedure in East Asia. Inappropriate injection can result in various complications.
The aim of this study was to develop an approach for comprehensively evaluating the lower facial structure based on the shape of the mandible angle, the thickness of the masseter, and the thickness of subcutaneous fat.
Clinical profiles and standard ultrasound images were collected from patients seeking masseter BoNT-A injections. Lower facial structures were evaluated based on 3 aspects: mandible, masseter, and subcutaneous fat and skin. The mandibular angle was classified as extroverted, straight, or introverted. The starting point of the middle part of the masseter was recorded. The thickness of the deep inferior tendon, the superficial and deep belly of the superficial part of the masseter, and their contractility were measured. Overall thickness and the thickness of subcutaneous fat and skin were also measured.
Eighty-four masseters from 42 patients were included. Straight mandibular angles were the most common type of angle (48.81%), followed by introverted (26.19%) and extroverted angles (25.00%). The middle part of the masseter starts from 2.33 [0.36] cm (mean [standard deviation]) above the mandible edge, which is above the usual injection points. The superficial belly was thicker than the deep belly in both static and clenching states (P = .048, P = .001) and had greater contractility. The average overall thickness was 1.87 [0.29] cm.
Comprehensive evaluation of the lower facial contour and structure based on ultrasound examination could be a reliable and replicable assessment approach.

Masseter reduction by botulinum neurotoxin A (BoNT-A) injection is a popular procedure in East Asia. However, not all procedures achieve a satisfactory outcome. Inappropriate BoNT-A injection can result in various complications, such as risorius muscle paralysis, paradoxical muscle bulging, sunken cheeks, and so on.1 It was discovered in clinical practice that the width of the lower face depends mainly on the shape of the mandible angle, the thickness of the masseter, and the thickness of subcutaneous fat. Therefore, the lower facial structure has been comprehensively evaluated based on these 3 variables, and ultrasound examination of the mandible, masseter, and subcutaneous fat has been undertaken to facilitate BoNT-A injection.
METHODS
Patients
Clinical and ultrasound imaging data of patients who sought masseter muscle BoNT-A injection for cosmetic purposes were collected during routine examinations between January 2022 and October 2022 at the Department of Plastic Surgery of Peking Union Medical College Hospital. The inclusion criteria were as follows: (1) healthy females aged between 18 and 50 years old; (2) complaint of a bulky masseter; and (3) intention to receive BoNT-A injection for masseter reduction. The exclusion criteria were as follows: (1) received surgical reduction of the mandible or masseter or operation on lower facial structures; (2) other health conditions unsuitable for BoNT-A injection; and (3) refused or were unable to participate in the study. The study conformed to the Declaration of Helsinki and was approved by the IRB of Peking Union Medical College Hospital. Informed consent was acquired from each patient.
Ultrasound Imaging
Ultrasound imaging was performed as previously described.2 Briefly, patients were examined in a supine position. The anterior and posterior borders of the masseter muscle were palpated during clenching. The zygomatic arch was considered the upper border of the muscle, and the jawline was considered the lower border. Standard ultrasound images were acquired with the probes vertically positioned at the midline to take a coronal section image of the muscle and at the lower third to take a horizontal image of the muscle, as previously described.2,3 The sections were close to the most prominent point of masseter and common injection points, and thus, the results can serve as reference values for clinical practice and ensure comparability. Abundant acoustic couplant was used to ensure that no pressure was applied to the soft tissue, which could compress the tissue and interfere with the thickness data. Ultrasound imaging data were collected with Alpinion E-cube 7 (Seoul, Republic of Korea) and 12H linear probes in both static and clenching states to demonstrate the intensity of muscle contraction.
The following indices were measured from the ultrasound images. (1) The degree and classification of the mandibular angle were measured in static coronal images. Less than 5° of extroversion or introversion was recorded as straight. (2) The masseter was measured in both static and clenching states. The starting point of the middle part was measured in static coronal images. The thickness of the deep inferior tendon (DIT) and the deep and superficial layers of the superficial part of the masseter were measured in both static and clenching states to calculate the contractility of each layer. The DIT was classified into compartmentalized, transverse, and longitudinal types in horizontal images. (3) The thickness of subcutaneous fat and overall thickness were measured in both static and clenching states as well.
Statistical Analysis
Histograms and the Shapiro-Wilk test were used to test the normality of data. Normally distributed data are reported as the mean [standard deviation]. A paired t-test was used to compare the thickness data. P < .05 was considered statistically significant. Data analysis was performed with Prism 9.
RESULTS
Clinical Profiles
Eighty-four masseters from 42 patients were included in the study. The patients were all young females aged between 18 and 40 years (mean age, 28.1 [5.1] years) who came to the Plastic Surgery Clinic for masseter muscle reduction by BoNT-A injection. The parameters of the mandible, masseter, and subcutaneous fat were measured by ultrasound imaging; the findings are shown in Table 1.
| Parameter of the mandible . | |||
|---|---|---|---|
| Mandible | Introvert | Extrovert | Straight |
| Count | 22 | 21 | 41 |
| Percentage | 26.19% | 25.00% | 48.81% |
| Average degree | −26.04° [6.51°] | 26.57° [14.07°] | NA |
| Thickness (cm) | Static | Clenching | C-S |
| Middle part distance from mandibular angle | 2.33 [0.36] | NA | NA |
| Deep belly | 0.58 [0.20] | 0.59 [0.21] | 0.01 [0.14] |
| Deep inferior tendon | 0.11 [0.06] | 0.12 [0.07] | 0.003 [0.05] |
| Superficial belly | 0.66 [0.19] | 0.72 [0.21] | 0.06 [0.12] |
| Subcutaneous fat and skin | 0.54 [0.15] | 0.54 [0.17] | 0.002 [0.07] |
| Overall thickness | 1.87 [0.29] | 1.96 [0.28] | 0.08 [0.07] |
| DIT classification | Compartmentalized | Transverse | Longitudinal |
| Count | 46 | 17 | 21 |
| Percentage | 54.76% | 20.24% | 25.00% |
| Parameter of the mandible . | |||
|---|---|---|---|
| Mandible | Introvert | Extrovert | Straight |
| Count | 22 | 21 | 41 |
| Percentage | 26.19% | 25.00% | 48.81% |
| Average degree | −26.04° [6.51°] | 26.57° [14.07°] | NA |
| Thickness (cm) | Static | Clenching | C-S |
| Middle part distance from mandibular angle | 2.33 [0.36] | NA | NA |
| Deep belly | 0.58 [0.20] | 0.59 [0.21] | 0.01 [0.14] |
| Deep inferior tendon | 0.11 [0.06] | 0.12 [0.07] | 0.003 [0.05] |
| Superficial belly | 0.66 [0.19] | 0.72 [0.21] | 0.06 [0.12] |
| Subcutaneous fat and skin | 0.54 [0.15] | 0.54 [0.17] | 0.002 [0.07] |
| Overall thickness | 1.87 [0.29] | 1.96 [0.28] | 0.08 [0.07] |
| DIT classification | Compartmentalized | Transverse | Longitudinal |
| Count | 46 | 17 | 21 |
| Percentage | 54.76% | 20.24% | 25.00% |
Values are mean [standard deviation] or percentages. C-S, clenching-static; DIT, deep inferior tendon; NA, not applicable.
| Parameter of the mandible . | |||
|---|---|---|---|
| Mandible | Introvert | Extrovert | Straight |
| Count | 22 | 21 | 41 |
| Percentage | 26.19% | 25.00% | 48.81% |
| Average degree | −26.04° [6.51°] | 26.57° [14.07°] | NA |
| Thickness (cm) | Static | Clenching | C-S |
| Middle part distance from mandibular angle | 2.33 [0.36] | NA | NA |
| Deep belly | 0.58 [0.20] | 0.59 [0.21] | 0.01 [0.14] |
| Deep inferior tendon | 0.11 [0.06] | 0.12 [0.07] | 0.003 [0.05] |
| Superficial belly | 0.66 [0.19] | 0.72 [0.21] | 0.06 [0.12] |
| Subcutaneous fat and skin | 0.54 [0.15] | 0.54 [0.17] | 0.002 [0.07] |
| Overall thickness | 1.87 [0.29] | 1.96 [0.28] | 0.08 [0.07] |
| DIT classification | Compartmentalized | Transverse | Longitudinal |
| Count | 46 | 17 | 21 |
| Percentage | 54.76% | 20.24% | 25.00% |
| Parameter of the mandible . | |||
|---|---|---|---|
| Mandible | Introvert | Extrovert | Straight |
| Count | 22 | 21 | 41 |
| Percentage | 26.19% | 25.00% | 48.81% |
| Average degree | −26.04° [6.51°] | 26.57° [14.07°] | NA |
| Thickness (cm) | Static | Clenching | C-S |
| Middle part distance from mandibular angle | 2.33 [0.36] | NA | NA |
| Deep belly | 0.58 [0.20] | 0.59 [0.21] | 0.01 [0.14] |
| Deep inferior tendon | 0.11 [0.06] | 0.12 [0.07] | 0.003 [0.05] |
| Superficial belly | 0.66 [0.19] | 0.72 [0.21] | 0.06 [0.12] |
| Subcutaneous fat and skin | 0.54 [0.15] | 0.54 [0.17] | 0.002 [0.07] |
| Overall thickness | 1.87 [0.29] | 1.96 [0.28] | 0.08 [0.07] |
| DIT classification | Compartmentalized | Transverse | Longitudinal |
| Count | 46 | 17 | 21 |
| Percentage | 54.76% | 20.24% | 25.00% |
Values are mean [standard deviation] or percentages. C-S, clenching-static; DIT, deep inferior tendon; NA, not applicable.
Mandibular Bone
The mandibular angles were classified into 3 types under ultrasound observation: introvert, extrovert, and straight. Straight was defined as less than 5° of introversion or extroversion; extrovert was defined as more than 5° of mandibular angle extroversion; and introvert was defined as more than 5° of mandibular angle introversion. The ultrasound and schematic diagrams of the classifications are shown in Figure 1.
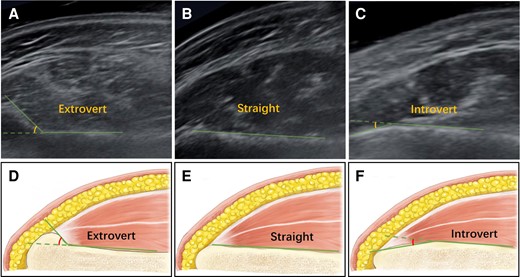
Ultrasound and schematic diagram of the mandibular angle classifications: (A, D) extrovert: more than 5° of mandibular angle extroversion; (B, E) straight: less than 5° of introversion or extroversion; and (C, F) introvert: more than 5° of mandibular angle introversion.
Among the 84 mandible angles observed, straight was the most common type (41 mandibles); 21 mandibles had extroverted angles and 22 mandibles had introverted angles. The proportion of each type of mandibular angle is shown in Table 1. The average degree of introversion was −26.04° [6.51°], and that of extroversion was 26.57° [14.07°].
Masseter Muscle
The starting point of the middle part of the masseter was positioned at 2.33 [0.36] cm above the mandibular margin, generally higher than the most prominent point of the masseter. The DIT originates from the mandibular angle and can be classified as compartmentalized, transverse, or longitudinal based on the shape in the horizontal section of its ultrasound image, as described by Lee et al.3 In the current population, it was discovered that compartmentalized DIT was the most common type (46/84 masseters), followed by longitudinal DIT (21/84 masseters) and transverse DIT (17/84 masseters). The proportion of each DIT type is shown in Table 1, and ultrasound images are shown in Figure 2.
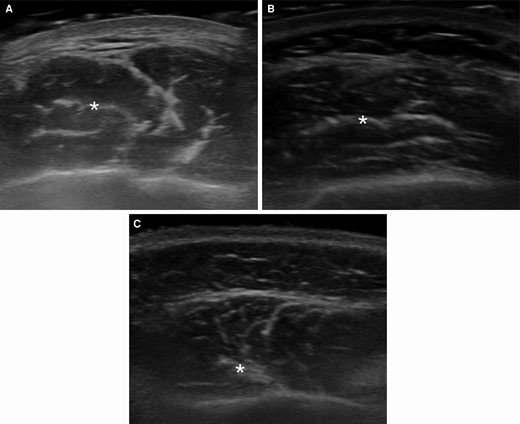
Ultrasound images of the DIT classifications. DIT marked by an asterisk (*) symbol. (A) compartmentalized DIT, (B) transverse DIT, and (C) longitudinal DIT. DIT, deep inferior tendon.
The superficial part of the masseter is divided by the DIT into the superficial belly and deep belly, as shown in Figure 3. The mean thickness measured in the static state was 0.66 [0.19] cm for the superficial belly and 0.58 [0.20] cm for the deep belly; the difference was statistically significant (P = .048). When clenching, the thickness of the superficial belly was 0.72 [0.21] cm, and that of the deep belly was 0.59 [0.21] cm, which was also a significant difference (P = .001). However, a significant change in thickness during clenching was only present in the superficial belly (P < .001), while the thickness of subcutaneous fat, DIT, and deep muscle belly did not significantly change during clenching (P = .753, P = .568, P = .361, respectively).
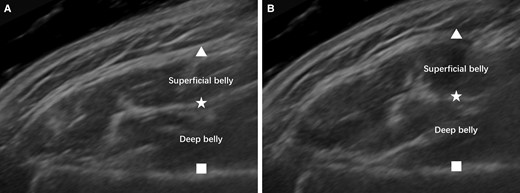
Ultrasound image of the masseter in static (A) and clenching (B) states. Significant bulging of the masseter can be observed from the ultrasound image. Triangle, masseter fascia; star, deep inferior tendon; square, mandible surface.
Subcutaneous Fat and Skin
The mean thickness of subcutaneous fat and skin was 0.54 [0.15] cm in the static state and 0.54 [0.17] cm during clenching; thus, the thickness was not significantly different based on masseter movement (P = .753). The overall thickness of soft tissues above the mandible, including the superficial part of the masseter, subcutaneous fat, and skin, was 1.87 [0.29] cm in the static state and 1.96 [0.28] cm during clenching. Therefore, the soft tissue thickness significantly increased when clenching (P < .001), which is consistent with the bulging appearance and palpation results. The thickness and recommended BoNT-A injection proportion of each layer are shown in Figure 4.
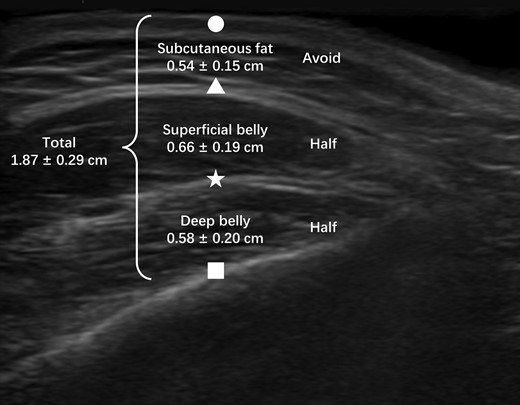
Overall thickness and recommended injection proportion of each layer. Circle, skin; triangle, masseter fascia; star, deep inferior tendon; square, mandible surface.
DISCUSSION
BoNT-A injection is one of the most convenient ways to reduce lower face volume and reshape a smooth contour. However, multiple factors can affect the final aesthetic outcome or even cause unwanted impacts that could compromise quality of life. Therefore, the current study observed and analyzed the factors that could have an influence on BoNT-A injection outcomes, including bone, muscle, subcutaneous fat, and skin, with the aim of comprehensively understanding the factors that affect masseter BoNT-A injection and providing a reference for clinical practice.
The mandible is a factor that is often overlooked in masseter BoNT-A injection. Its influence is weaker than that of the masseter muscle; however, the bone is the foundation of the lower facial contour and should be taken into consideration. According to the findings of this study, approximately 25% of the subjects examined exhibited extrovert mandibular angles, and the mean extroversion angle was 26.57° [14.07°]. For these patients, it is necessary to keep an adequate amount of soft tissue to prevent contour visibility of the mandibular angle, as shown in Figure 5. The jawline is very clear in the patient presented, which is a trait associated with skinny people. However, the rest of her face was fuller, thus creating an unnatural, discordant appearance. Therefore, caution should be emphasized when performing repeated injections, and it is suggested these be carried out by experienced surgeons after ultrasound evaluation of the lower facial structure. A minimum of 1.5 cm of soft tissue should be preserved for patients with an extroverted mandibular angle to avoid such complications.
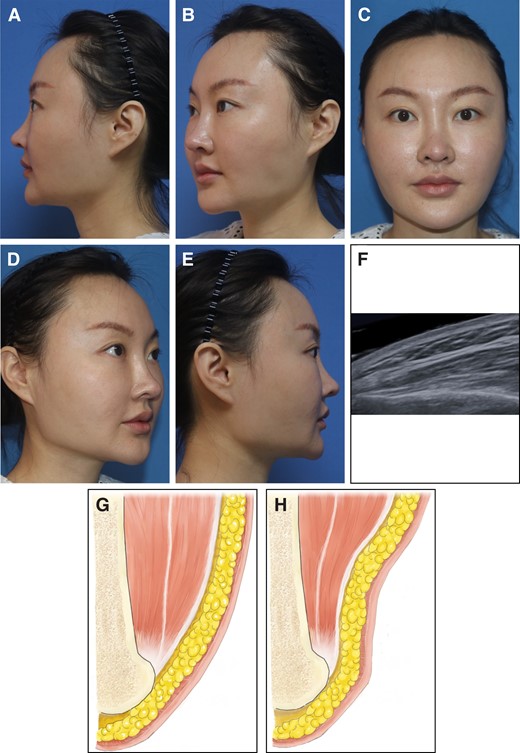
A case of contour visibility of the mandibular angle, and schematic diagrams of the possible cause. (A-E) A representative case of contour visibility of the mandibular angle: (A) left lateral view, (B), left oblique view, (C) frontal view, (D) right oblique view, (E) right lateral view. (F) Ultrasound image of the patient's mandibular angle, which is extrovert in this case. (G) Schematic diagram before injection. The extrovert mandibular angle is covered by masseter, creating a smooth lower facial contour. (H) Schematic diagram after BoNT-A injection. The thickness of masseter is significantly reduced, and the extrovert mandibular angle is now visible. BoNT-A, botulinum neurotoxin A.
The masseter muscle is the dominant factor in the lower facial contour and is the target of BoNT-A injection. There are 3 parts of the masseter muscle: the superficial, middle, and deep parts. The middle and deep parts originate from higher positions and are often not involved in masseter BoNT-A injections. However, accidental injection into the middle part or high into the superficial part could result in a sunken cheek, as described by Yu et al.4 A case of a sunken cheek is shown in Figure 6. The findings of the current study suggest that injection within 2 cm above the mandibular margin would be safe and efficient because the starting point of the middle part of the masseter was on average 2.33 [0.36] cm above the mandibular edge.

A case of sunken cheek. (A) Before injection and (B) 1 month after injection.
The superficial part of the masseter could be further divided into the superficial belly and deep belly, separated by the DIT. Consistent with the findings of Wang et al, the current study also suggests that the dose of BoNT-A should be proportionally distributed among the superficial belly and deep belly of the masseter muscle to prevent excessive paralysis of the deep belly and compensatory hypertrophy of the superficial belly, resulting in paradoxical muscle bulging or chipmunk deformity, as shown in Figure 7.5 However, in contrast to Wang et al's results, the superficial belly proved to be thicker in both static and clenching states in the current population, possibly due to differences in demographic and ethnic characteristics. Therefore, a possible injection dose distribution derived from this study is 53.23% superficial belly and 46.77% deep belly, which is a ratio of approximately 1:1. The exact proportion for each individual case should be determined by ultrasound examination to achieve optimal results.
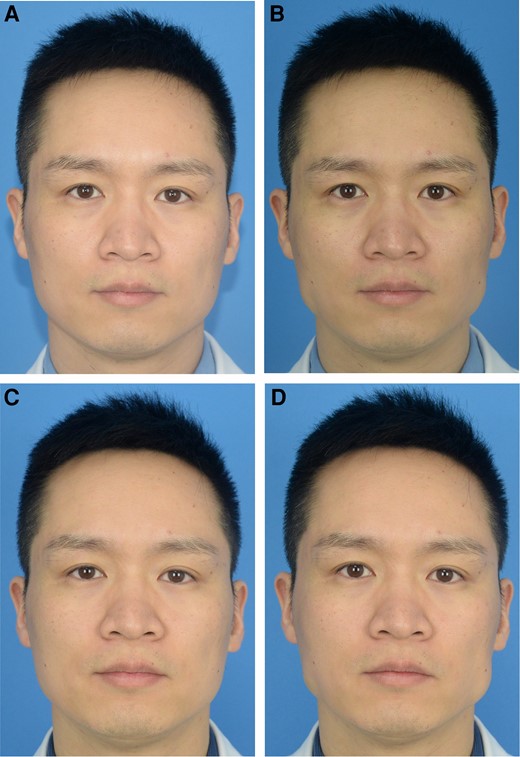
A case of paradoxical muscle bulging. (A) Before injection and (B) 1 week after injection, static. (C) Before injection and (D) 1 week after injection, clenching.
The masseteric fascia beneath the subcutaneous fat is part of the facial muscular aponeurosis system. The average thickness of subcutaneous fat and skin was 0.54 [0.15] cm. BoNT-A injection should be stopped at this layer to prevent paralysis of the risorius muscle, which originates from the anterior part of the fascia, as well as to avoid wasting BoNT-A. In addition, the thickness of subcutaneous fat could be a predictor of BoNT-A injection effectiveness. Patients with relatively thick subcutaneous fat and thin masseters might have less reduction in facial width due to the limited contribution of masseters to the lower facial contour.
Based on the above findings, a comprehensive BoNT-A injection strategy can be devised. First, palpate the masseter borders when the patient is clenching, as well as the most prominent point. Selecting an area within 2 cm of the mandibular margin avoids injection into the middle and deep parts of the masseter. Three-point retrograde injection is one of the most commonly used techniques, but other methods could also be safe and effective as long as the injection points are confined within the safety zones. Most of the syringe needles used are 13-mm, 27- or 30-gauge needles. However, 30-gauge 25-mm needles are recommended for optimal control and adequate depth because the full thickness was 1.87 [0.29] cm based on the study findings, which would be beyond the reach of 13-mm needles.
We can take 3-point retrograde injection, 24 to 32 units on each side, as an example. The schematic diagram is shown in Figure 8. The first step would be to find the most prominent point of the masseter by palpation. Half of the total BoNT-A dose should be injected into this point; the other half should be injected into the 2 lower points of the isosceles triangle. Enter the skin vertically until the needle tip reaches the periosteum, which is 1.87 [0.29] cm beneath the skin. The resistance increases when meeting the masseteric fascia and DIT and resolves after penetrating these layers. The surface of the mandible is hard and impenetrable, which can help in judging the position of the needle tip. After retracting approximately 0.25 cm, the needle tip should be in the center of the deep belly of the superficial part of masseter. According to the ratio recommended above, the deep belly should be injected with half of the total dose. When the needle is retracted approximately 0.65 cm, the needle tip reaches approximately the center of the superficial muscle belly, and half of the total BoNT-A dose is injected into this layer. A more experienced doctor could also perform continuous layer-by-layer retrograde injections to ensure more even distribution of the drug. Now, the needle tip would be approximately 1 cm deep into the skin, which is well beneath the subcutaneous fat. The needle is extracted without making any injections so that the subcutaneous fat and origin of the risorius muscle are left untouched. The injection process is repeated at the other 2 points of the isosceles triangle, following a ratio of 1:1 in the deep and superficial belly, or the proportion is calculated according to the patient's ultrasound image during consultation. A well-performed treatment case is shown in Figure 9.
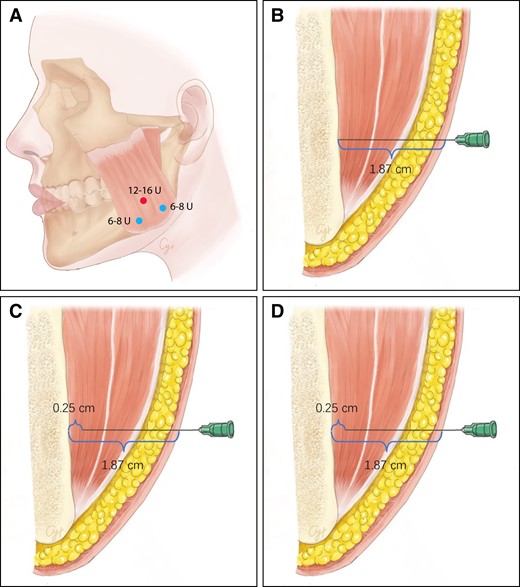
Schematic diagram of the recommended botulinum toxin injection strategy. (A) An example of botulinum toxin injection dose and sites. The red dot represents the most prominent point of masseter, determined by palpation during clenching; 12 to 16 units of botulinum toxin should be injected into this point in total. The blue dots represent the lower injection points, which should form an isosceles triangle with the red dot; 6 to 8 units of botulinum toxin should be injected into these points, respectively. (B) Enter the skin vertically until the needle tip reaches the periosteum. (C) Retract for approximately 0.25 cm; the needle tip should be in the center of the deep belly of the superficial part of masseter. Half of the dose should be injected into this layer. (D) Further retract for approximately 0.65 cm; the needle tip should reach the center of the superficial muscle belly, the other half of the due dose of a point should be injected into this layer.

A case of well-performed masseter reduction by botulinum toxin injection. (A) Before injection and (B) 6 months after injection.
In fact, the clinical classification of masseter and DIT has been proposed by many researchers due to their important influence on BoNT-A injection. For example, Xie et al identified 5 bulging types of masseters based on appearance, palpation, B-mode ultrasound examination, and anatomic dissection.6 Following a tailored injection protocol, good injection outcomes were achieved. Lee et al proposed in 2016 that the existence of the DIT could be the cause of paradoxical masseteric bulging.7 Three types of DIT were identified according to the area covered in their cadaveric study. Further in vivo observation by ultrasound examination revealed the internal structure of the DIT, and a new classification was proposed based on the pattern in horizontal section: compartmentalized, transverse, or longitudinal.3 Ultrasound examination can provide many clues about the internal structure of the masseter as well as about bone, subcutaneous fat, and skin. Evidence from a clinical trial has proven that ultrasound-guided BoNT-A injection is more effective than traditional blind injection.8 Therefore, the importance of ultrasound imaging should be considered in preoperative design, during injection, and at postoperative follow-ups. Only by observing the internal structure can we devise personalized injection strategies. Patient-doctor communication efficiency could also benefit from ultrasound images, from which patients can obtain a visualized reference of their own condition.
The current study is a cross-sectional study, which aimed to devise a comprehensive evaluation approach based on ultrasound imaging to analyze the lower facial structure, in order to assist and evaluate masseter botulinum toxin injection as well as other potential cosmetic procedures. Previous literature has revealed that masseter botulinum toxin injection without a proper understanding of the underlying anatomic structures can result in unsatisfactory outcomes. For example, Yu et al found that accidental injection into the middle part of masseter or high into the superficial part could result in a sunken cheek;4 Lee et al proposed that the existence of the DIT could be the cause of paradoxical masseteric bulging.7 This study was based on knowledge obtained from these valuable works, and proposed an effective evaluation approach, linking anatomic knowledge to clinical application. Determining whether the usage of ultrasound can greatly improve clinical outcomes and patient satisfaction requires further clinical trials.
The current study has some limitations. First, previous animal studies have suggested the possibility of mandible changes after masseter botulinum toxin injection.9,10 However, a previous retrospective cohort study revealed that slight changes in the masseter would not induce significant changes in the mandibular bone in the relatively short term,11 consistent with our clinical observations and experience. Therefore, long-term prospective clinical trials are required to reach a definite conclusion as to whether masseter reduction by BoNT-A injection would cause changes in the mandibular bone. Second, only Asian females were included, and the sample size was relatively small. However, these patients are the major recipients of masseter BoNT-A injection. The data acquired were of good quality, and statistically significant results were achieved with adequate statistical power. Therefore, it is believed that the results from this study are valid and could be used for clinical guidance. Third, the current study is a cross-sectional study based on known anatomic knowledge and aimed to construct a comprehensive evaluation approach based on ultrasound imaging to analyze the lower facial structure to assist and evaluate masseter botulinum toxin injection and other potential cosmetic procedures. Additional clinical trials are needed to determine whether the use of ultrasound could significantly improve clinical outcomes and patient satisfaction.
CONCLUSIONS
Comprehensive evaluation of the lower facial contour and structure based on ultrasound examination provides a reliable and repeatable assessment approach. This approach can be applied for the evaluation of masseter BoNT-A injection outcomes, the development of individualized treatment strategies before injection, and the prediction of posttreatment results.
Acknowledgments
Drs Li and Chi contributed equally to this work as co-first authors.
Disclosures
Drs Yu, Huang, and Long received funding from the National High Level Hospital Clinical Research for this study. The authors declared no other potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The work was supported by National High Level Hospital Clinical Research Funding, grant numbers: 2022-PUMCH-B-041, 2022-PUMCH-C-025, and 2022-PUMCH-A-210.
REFERENCES
Author notes
Dr Li is a medical student, Department of Plastic Surgery, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China.
Dr Chi is a medical student, Department of Plastic Surgery, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China.
Dr Chen is an ultrasound doctor, Department of Ultrasound, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China.
Ms Jin is a research assistant, Department of Plastic Surgery, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China.
Dr Huang is a plastic surgeon, Department of Plastic Surgery, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China.
Dr Long is a plastic surgeon, Department of Plastic Surgery, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China.
Dr Yu is a plastic surgeon, Department of Plastic Surgery, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China.



