-
PDF
- Split View
-
Views
-
Cite
Cite
Rohani Omar, Louise Kuo, Sergi G Costafreda, Amanda Hall, Marina Forbes, John T O’Brien, Anne G M Schilder, Managing comorbid cognitive impairment and hearing loss in older adults: a UK survey of audiology and memory services, Age and Ageing, Volume 52, Issue 5, May 2023, afad080, https://doi.org/10.1093/ageing/afad080
Close - Share Icon Share
Abstract
midlife hearing loss is a potentially modifiable risk factor for dementia. Addressing comorbid hearing loss and cognitive impairment in services for older adults may offer opportunities to reduce dementia risk.
to explore current practice and views amongst UK professionals regarding hearing assessment and care in memory clinics and cognitive assessment and care in hearing aid clinics.
national survey study. Between July 2021 and March 2022, we distributed the online survey link via email and via QR codes at conferences to professionals working in National Health Service (NHS) memory services and audiologists working in NHS and private adult audiology services. We present descriptive statistics.
135 professionals working in NHS memory services and 156 audiologists (68% NHS, 32% private sector) responded. Of those working in memory services, 79% estimate that >25% of their patients have significant hearing difficulties; 98% think it useful to ask about hearing difficulties and 91% do so; 56% think it useful to perform a hearing test in clinic but only 4% do so. Of audiologists, 36% estimate that >25% of their older adult patients have significant memory problems; 90% think it useful to perform cognitive assessments, but only 4% do so. Main barriers cited are lack of training, time and resources.
although professionals working in memory and audiology services felt addressing this comorbidity would be useful, current practice varies and does not generally address it. These results inform future research into operational solutions to integrating memory and audiology services.
Key Points
UK memory and audiology service professionals feel addressing comorbid hearing and cognitive impairment would be useful.
Current practice in addressing this comorbidity within UK memory and audiology services is variable.
The main barriers cited are lack of training, time and resources and uncertainty regarding onward referral pathways.
These results inform future research into operational solutions to integrating memory and audiology services.
Introduction
Longitudinal studies have shown a strong association between hearing loss acquired in midlife and dementia [1–4]. The evidence on the nature of this association [5, 6], as well as the impact of early and specialised hearing care on reducing dementia risk, however, is incomplete [7–9]. There is no agreed guidance on whether and how this comorbidity is best addressed in services for older people, or how integrated hearing and dementia pathways could be commissioned. The National Institute for Health and Care Excellence recommends referral of adults with diagnosed or suspected dementia/mild cognitive impairment for hearing assessment [10]. In Wales, an integrated framework of care has been developed prioritising hearing support for older adults with dementia and early identification of cognitive problems in older adults with hearing loss [11].
While further evidence is being gathered about clinical and cost-effectiveness of integrated pathways, it is important to understand perceived barriers and facilitators amongst healthcare professionals that may influence future adoption of innovative hearing and dementia care pathways. We therefore set out to explore current practice and views amongst healthcare professionals working in UK memory and audiology services.
Methods
The objectives of this study are to understand:
Existing practices relating to:
Hearing assessment and care in National Health Service (NHS) memory clinics.
Cognitive assessment and care in older adults attending NHS and private audiology clinics.
Views and expectations of:
Professionals working in NHS memory services regarding hearing assessment and care in their clinics.
Audiologists in the NHS and private sector regarding cognitive assessment in older adults attending their clinics.
We developed two separate surveys for each professional group with descriptive and exploratory questions (Appendix S1); questions were developed through discussion with the author team and experts in the fields of dementia and hearing. We used Google Forms to collect data anonymously, with survey links and QR codes included in emails, newsletters and flyers. The survey was classified as a service evaluation, with no identifiable respondent information collected and responses anonymised, and therefore needed no NHS ethical approval. Dementia professionals (n = 176) were approached between November 2021 and March 2022 via existing email distribution lists of the National Institute of Health Research Clinical Research Network (NIHR CRN) Dementias and Neurodegeneration Specialty, Memory Services National Accreditation Programme and British Geriatric Society.
NHS Audiologists (n = 261) were approached between July 2021 and March 2022 via existing email distribution lists of NHS Audiology heads of service, NIHR CRN Ear, Nose and Throat National (ENT) Specialty, and private audiologists via Boots Hearingcare and Specsavers internal mailing lists. The survey was highlighted in British Society of Audiology newsletters, in flyers distributed at the British Academy of Audiology Annual Conference, November 2021, and British Association of Audiovestibular Physicians National Audit Meeting, November 2021.
We present descriptive statistics of the responses.
Results
Professionals working in NHS memory services
We received 135 responses (77% response rate) from a variety of professionals working in NHS memory services (Table 1). Most worked in community services (78%) and the remainder in hospital services. Most professionals (88%) supported a population with >75% of patients aged over 65.
Demographics of dementia professionals and audiologists responding to surveys
| Demographics . | . | Dementia specialists (n = 135) . | Audiologists . | |
|---|---|---|---|---|
| NHS (n = 104) . | Private sector (n = 51) . | |||
| Type of service | Community-based memory service | 78% | – | – |
| Hospital-based memory service | 22% | – | – | |
| Both community and hospital based | 1% | – | – | |
| Service lead | Yes | – | 67% | 60% |
| Role | Old age psychiatrist | 37% | – | – |
| Dementia nurse | 17% | – | – | |
| Community mental health nurse | 16% | – | - | |
| Geriatrician | 6% | – | – | |
| Occupational therapist | 6% | – | – | |
| Clinical psychologist | 4% | – | – | |
| Neurologist | 3% | – | – | |
| Other | 10% | 4% | 14% | |
| Healthcare science practitioner | – | 41% | 0% | |
| Healthcare clinical scientist | – | 28% | 2% | |
| Hearing aid dispenser | – | 10% | 31% | |
| Audiologist | – | 10% | 51% | |
| Hearing therapist | – | 7% | 2% | |
| Years in service | <1 | 5% | 1% | 2% |
| 1–5 | 26% | 16% | 12% | |
| 6–10 | 21% | 15% | 33% | |
| >10 | 47% | 68% | 53% | |
| Demographics . | . | Dementia specialists (n = 135) . | Audiologists . | |
|---|---|---|---|---|
| NHS (n = 104) . | Private sector (n = 51) . | |||
| Type of service | Community-based memory service | 78% | – | – |
| Hospital-based memory service | 22% | – | – | |
| Both community and hospital based | 1% | – | – | |
| Service lead | Yes | – | 67% | 60% |
| Role | Old age psychiatrist | 37% | – | – |
| Dementia nurse | 17% | – | – | |
| Community mental health nurse | 16% | – | - | |
| Geriatrician | 6% | – | – | |
| Occupational therapist | 6% | – | – | |
| Clinical psychologist | 4% | – | – | |
| Neurologist | 3% | – | – | |
| Other | 10% | 4% | 14% | |
| Healthcare science practitioner | – | 41% | 0% | |
| Healthcare clinical scientist | – | 28% | 2% | |
| Hearing aid dispenser | – | 10% | 31% | |
| Audiologist | – | 10% | 51% | |
| Hearing therapist | – | 7% | 2% | |
| Years in service | <1 | 5% | 1% | 2% |
| 1–5 | 26% | 16% | 12% | |
| 6–10 | 21% | 15% | 33% | |
| >10 | 47% | 68% | 53% | |
Demographics of dementia professionals and audiologists responding to surveys
| Demographics . | . | Dementia specialists (n = 135) . | Audiologists . | |
|---|---|---|---|---|
| NHS (n = 104) . | Private sector (n = 51) . | |||
| Type of service | Community-based memory service | 78% | – | – |
| Hospital-based memory service | 22% | – | – | |
| Both community and hospital based | 1% | – | – | |
| Service lead | Yes | – | 67% | 60% |
| Role | Old age psychiatrist | 37% | – | – |
| Dementia nurse | 17% | – | – | |
| Community mental health nurse | 16% | – | - | |
| Geriatrician | 6% | – | – | |
| Occupational therapist | 6% | – | – | |
| Clinical psychologist | 4% | – | – | |
| Neurologist | 3% | – | – | |
| Other | 10% | 4% | 14% | |
| Healthcare science practitioner | – | 41% | 0% | |
| Healthcare clinical scientist | – | 28% | 2% | |
| Hearing aid dispenser | – | 10% | 31% | |
| Audiologist | – | 10% | 51% | |
| Hearing therapist | – | 7% | 2% | |
| Years in service | <1 | 5% | 1% | 2% |
| 1–5 | 26% | 16% | 12% | |
| 6–10 | 21% | 15% | 33% | |
| >10 | 47% | 68% | 53% | |
| Demographics . | . | Dementia specialists (n = 135) . | Audiologists . | |
|---|---|---|---|---|
| NHS (n = 104) . | Private sector (n = 51) . | |||
| Type of service | Community-based memory service | 78% | – | – |
| Hospital-based memory service | 22% | – | – | |
| Both community and hospital based | 1% | – | – | |
| Service lead | Yes | – | 67% | 60% |
| Role | Old age psychiatrist | 37% | – | – |
| Dementia nurse | 17% | – | – | |
| Community mental health nurse | 16% | – | - | |
| Geriatrician | 6% | – | – | |
| Occupational therapist | 6% | – | – | |
| Clinical psychologist | 4% | – | – | |
| Neurologist | 3% | – | – | |
| Other | 10% | 4% | 14% | |
| Healthcare science practitioner | – | 41% | 0% | |
| Healthcare clinical scientist | – | 28% | 2% | |
| Hearing aid dispenser | – | 10% | 31% | |
| Audiologist | – | 10% | 51% | |
| Hearing therapist | – | 7% | 2% | |
| Years in service | <1 | 5% | 1% | 2% |
| 1–5 | 26% | 16% | 12% | |
| 6–10 | 21% | 15% | 33% | |
| >10 | 47% | 68% | 53% | |
Seventy-nine percent estimated >25% of their patients have significant hearing difficulties (significant indicating a problem that disrupts/limits a person’s day-to-day function). Ninety-one percent ask their patients or accompanying person about hearing difficulties; 4% perform hearing assessment within their clinic setting. Actions taken by dementia professionals when hearing difficulties are identified are summarised in Figure 1a. Most commonly (86%) this involves advising patients to see their GP or have their hearing tested at a high street audiology service. Most allocate <5 min to hearing assessment including discussing results (88%). Reasons for not addressing hearing are summarised in Figure 1c.
Almost all respondents felt it is/would be useful to ask about hearing difficulties and to have direct links to an audiology service, with more variable responses to usefulness of performing hearing assessment in memory clinics or having an audiologist in their team (Figure 1e and f). Only 8% responded that their service has a direct referral pathway to an audiology service.
Audiologists
We received responses from 156 audiologists, 106 (68%) working in NHS audiology services and 50 (32%) in the private sector; demographics are summarised in Table 1. Thirty-three percent of NHS and 39% of private sector respondents estimated >25% of their older adult patients have significant memory problems. Only 7 (4.5%) ask their older patients about memory problems or diagnosis of dementia and 4 (2.6%; 3 NHS, 1 private) perform a cognitive assessment (e.g. MMSE, 6cit, Cambridge Cognition tool, Mini-Cog). Actions taken when cognitive impairment is identified are summarised in Figure 1b. These involve advising patients to see their GP, and using adapted hearing tests and hearing aid fitting methods. Over half (n = 4) allocate <5 min to cognitive assessment including discussing results. Reasons for not performing cognitive assessments in audiology clinics are summarised in Figure 1d. Ninety-two percent of NHS and 84% of private sector respondents felt it is/would be useful to ask about memory or perform a cognitive assessment in audiology clinics (Figure 1g).
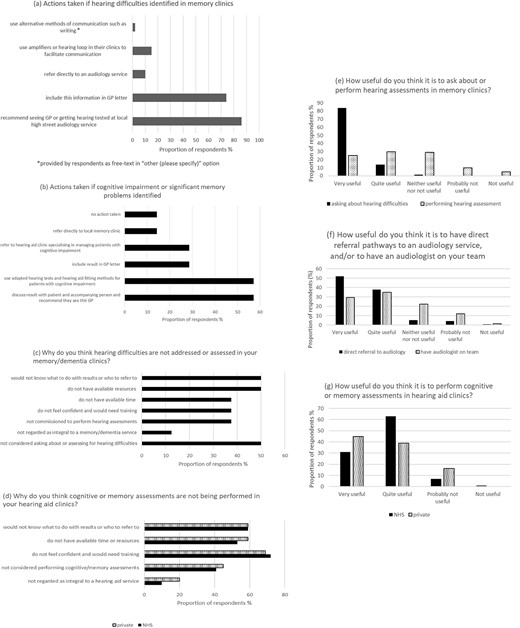
(a) Actions taken by dementia professionals (91% of total respondents) if hearing difficulties are identified from asking and/or hearing assessment in memory clinics, (b) actions taken by audiologists (4% of total respondents) if cognitive impairment or significant memory problems are identified in hearing aid clinics, (c) reasons provided by dementia professionals for not addressing hearing in memory clinics, (d) reasons provided by audiologists for not addressing memory in hearing aid clinics, (e) perceived usefulness of asking about hearing difficulties or assessing hearing in memory clinics, (f) perceived usefulness of memory services having direct referral pathways to an audiology service and/or having an audiologist on the memory service team, (g) perceived usefulness of performing cognitive or memory assessments in hearing aid clinics.
Discussion
Our survey highlights a high level of awareness amongst professionals working in NHS memory services and NHS and private sector audiologists of the association between hearing loss and dementia. Most respondents feel it would be useful to address hearing in dementia clinics and cognition in audiology clinics. Whereas hearing loss is addressed in most memory services in the sense that hearing difficulties are identified and referred onwards to GP, this is less so for cognitive problems in adult audiology services. Barriers cited by audiologists include the need for training on dementia in relation to hearing loss, not knowing what to do with test results or the onward referral pathway, and lack of time and resources to address memory in hearing clinics. Free-text responses mentioned the ‘stigma attached to a diagnosis of dementia’ and concerns regarding ‘the potential for fall out and inability to counsel or provide support if cognitive problems are identified by audiologists’. Others commented that addressing cognition might not be something patients want to engage with at a hearing aid appointment: ‘they might just want to have their hearing checked and care provided for their hearing difficulties’. Some commented that cognitive screening would enhance quality of care provided by the audiologists by allowing for modifications such as time allocated for appointments, method of communication and choice of tests. Professionals working in memory services commented on the issue of poor hearing aid adherence amongst their patients and the role they could play in encouraging hearing aid use. They also commented on a need for closer working with GPs so that hearing loss is managed prior to memory clinic visits. Recognising pressures on primary care, they suggested direct links between memory and audiology services. Others suggested ‘one stop’ dementia services incorporating hearing, vision and dental care.
Our survey asked audiologists if they performed cognitive/memory assessments, without specifying that this includes both asking about memory problems or performing cognitive assessment. This may have caused an underestimation of audiologists who ask about memory problems, but do not perform a test. Our survey asked dementia professionals about actions taken if hearing difficulties are identified, but did not separate the options advising patients to see their GP or have their hearing tested at a high street audiology service. We will be exploring these and other survey topics in more depth in our upcoming qualitative research.
Our previous pilot in patients with mild cognitive impairment (MCI) identified with hearing loss in a community memory clinic showed that onward referral through standard NHS audiological pathways resulted in low hearing aid uptake and poor long-term adherence [9]. Our respondents’ views are consistent with our recent qualitative study in older people with MCI or Alzheimer’s disease, highlighting the importance of specialised hearing care in addressing additional challenges brought about by cognitive problems relating to hearing aid use [12].
Professionals working in memory services commented on the potential impact of hearing loss on their patients’ performance on cognitive testing: ‘…patients I’ve seen are regarded as having a memory problem when it is their hearing that is affected’. This is evidenced by our recent work on adapted cognitive screening tests for people with hearing loss [13–15]. Reciprocally, older people with combined cognitive and hearing impairment may require adapted hearing tests since standard pure tone audiometry may be a poor predictor of their hearing abilities [16].
Perspectives of clinicians practising in UK memory and audiology services expressed in our study support those of a recent European expert group highlighting the complexity of addressing the comorbidities of hearing loss and cognitive impairment [17].
Conclusions
Professionals working with older adults in UK memory and audiology services recognise a potential unmet need of addressing this common comorbidity. This highlights the urgency of generating evidence on the effectiveness of early identification and specialised hearing care in reducing dementia risk [8, 9, 18]. Further research is required to develop operational solutions for integrated memory and hearing care. This should build on the barriers and facilitators identified in our surveys, and involve the stakeholders who guide, commission, deliver and use hearing and memory services.
Acknowledgements
This study was supported by the National Institute for Health and Social Care Research (NIHR) Clinical Research Network, the NIHR University College London Hospitals Biomedical Research Centre Hearing Health Theme and the ENT UK Foundation. We thank Doris-Eva Bamiou, Jason Warren, Catherine Mummery, Dawn Clare and Jack Constable for advising on the surveys and Yu Hsuen Yang for support in data presentation.
Declaration of Conflicts of Interest
A.S. advises on development and delivery of clinical trials of novel hearing therapeutics to hearing industry. J.O’B. has acted as a consultant for TauRx, Novo Nordisk, Biogen, Roche, Lilly and GE Healthcare and received grant support from Avid/Lilly, Merck and Alliance Medical.
Declaration of Sources of Funding
None.
Data Availability
The data will be made available from the corresponding author on reasonable request.




Comments