-
PDF
- Split View
-
Views
-
Cite
Cite
Junta Ishikawa, Nobuhiro Sato, Naho Ishigame, Ayaka Ono, Ikumi Yamagishi, Atsushi Sakagami, Yoshinori Sakai, Yasuo Hirose, Masahiro Yabe, Fat embolism syndrome in a patient with a right undisplaced femoral neck fracture, Age and Ageing, Volume 51, Issue 3, March 2022, afac046, https://doi.org/10.1093/ageing/afac046
Close - Share Icon Share
Abstract
Fat embolism syndrome (FES) is a rare condition characterised by the classic triad of respiratory distress, neurologic symptoms and petechial rash. Here, we encountered a case of FES in a patient with an asymptomatic right undisplaced femoral neck fracture (Garden Stage II). FES was diagnosed based on the Gurd and Willson’s diagnostic criteria and brain magnetic resonance imaging features. To the best of our knowledge, this is the first case of FES in a patient with an undisplaced femoral neck fracture. This study highlights the importance of considering the possibility of FES even in patients with undisplaced femoral neck fractures.
Key Points
We encountered a case of fat embolism syndrome (FES) in a patient with an asymptomatic undisplaced femoral neck fracture.
The patient was diagnosed with fat embolism syndrome (FES) based on the presence of respiratory failure, transient disorientation, and a right undisplaced femoral neck fracture.
To the best of our knowledge, this is the first case of fat embolism syndrome (FES) in a patient with an undisplaced femoral neck fracture.
Case report
A 91-year-old woman presented to the emergency department for chest pain and dyspnoea following a fall injury in a long-term care facility. Her symptoms had disappeared when she came to the hospital. The vital sign included blood pressure, 89/52 mm Hg; heart rate, 100 bpm; respiratory rate, 24/min; pulse oximetry, 90% on room air; and body temperature, 36.8°C. Laboratory findings showed non-specific findings. Electrocardiography found incomplete right bundle branch block but no other significant findings. Chest computed tomography (CT) demonstrated broad interstitial thickening, including the interlobular septal wall and bronchovascular bundles, which were non-specific. Due to the hypoxemia, the patient was admitted for monitoring. After 1 day, she complained of right hip joint pain. Hip radiography and CT revealed a right undisplaced femoral neck fracture (Garden Stage II) (Figure 1a). Femoral neck fracture and hypoxemia were suggestive of fat embolism syndrome (FES). Cytology revealed a small amount of fat droplets in the blood (Figure 1b).
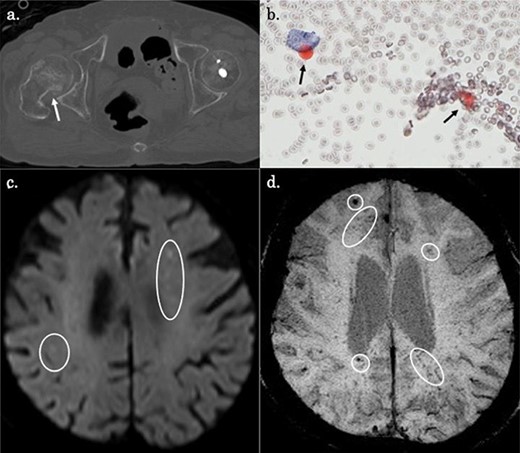
(a) CT showing a right undisplaced femoral neck fracture (Garden Stage II) (white arrowhead). (b) Blood cytology with oil red staining showing a small number of fat droplets in the background and a small number of cells that appeared to be histiocytes with fat in their cytoplasm (black arrowheads). (c) Diffusion-weighted MRI showing scattered punctate hyperintense signals in the watershed regions of the bilateral cerebrum (white circles). (d) Susceptibility-weighted imaging (SWI) showing diffuse hypointense lesions in the cerebrum (white circles).
After 2 days, the patient presented with transient disorientation, which prompted further evaluation with brain magnetic resonance imaging (MRI). Diffusion-weighted MRI showed scattered punctate hyperintense signals in the watershed regions of the bilateral cerebrum (Figure 1c). T2*-weighted imaging and susceptibility-weighted imaging (SWI) demonstrated multiple granular hypointense signals in the bilateral cerebral cortex and subcortical white matter (Figure 1d). These findings were consistent with a diagnosis of FES based on the Gurd and Willson’s diagnostic criteria [1].
The patient recovered with supportive care, and she underwent surgical correction of her femoral neck fracture. Follow-up examination revealed no recurrence of FES. Currently, she was transferred to another hospital for rehabilitation. At the time of transfer to the hospital, her poor renal function and low platelet count improved.
Discussion
FES is a rare condition characterised by the presence of fat emboli in the pulmonary or peripheral circulation, commonly associated with orthopaedic trauma (e.g. bone fracture) [2]. The incidence of FES is approximately 1.29% in patients with multiple femoral fractures excluding the neck, 0.54% in patients with single femoral fracture, and 0.06% in patients with single femoral neck fracture [3].
Although FES is characterised by a triad of respiratory distress, neurologic symptoms and petechial rash, patients rarely present with all of those. The diagnosis of FES is mainly established through clinical symptoms, laboratory tests and imaging studies [2]. Radiologically, FES presents with scattered hyperintense lesions on diffusion-weighted brain MRI [4]. On SWI, FES may be characterised by the presence of hypointense areas, depicting the minute petechial haemorrhages around the blood vessels [5]. These were consistent with our MRI findings. Diffusion-weighted images of head MRI are useful in the diagnosis of FES, and such imaging findings and the presence of symptoms in other organs systems, such as in the respiratory system, may help to differentiate FES from cerebrovascular disease [1, 2, 5]. In terms of chest CT, patients with FES present with diverse and nonspecific findings (i.e. infiltrative and frosted shadows, nodular shadows and occasional crazy paving) [1, 4].
We encountered a case of FES presenting with respiratory failure and transient disorientation in a patient with a right undisplaced femoral neck fracture. To the best of our knowledge, there have been no reports of FES in patients with undisplaced femoral neck fractures. Although the frequency of FES related to a single femoral neck fracture was low, this study highlights the importance of considering the possibility of FES even in patients with undisplaced femoral neck fractures.
Statement of ethics
Written informed consent for the publication of the clinical details and clinical images was obtained from the patient.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
None.




Comments