-
PDF
- Split View
-
Views
-
Cite
Cite
Megan Crichton, Dana Craven, Hannah Mackay, Wolfgang Marx, Marian de van der Schueren, Skye Marshall, A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: associations with geographical region and sex, Age and Ageing, Volume 48, Issue 1, January 2019, Pages 38–48, https://doi.org/10.1093/ageing/afy144
Close - Share Icon Share
Abstract
protein-energy malnutrition is a major health concern in home-dwelling older adults, particularly in the context of an ageing population. Therefore, a systematic review and meta-analysis was undertaken to determine the prevalence of malnutrition among older adults living independently in the community according to geographical region, sampling frame, rurality and sex.
six electronic databases were searched until September 2016. Original research studies which used the Mini Nutritional Assessment, Patient-Generated Subjective Global Assessment or Subjective Global Assessment to determine nutrition status in community samples with a mean age of ≥65 years were critically appraised and pooled using meta-analysis. Meta-regression was used to explore predictors of malnutrition prevalence in pooled statistics with high heterogeneity.
111 studies from 38 countries (n = 69,702 participants) were included. The pooled prevalence of malnutrition in the older community setting ranged from 0.8% (95% CI: 0.2–1.7%) in Northern Europe to 24.6% (95% CI: 0.0–67.9%) in South-East Asia. Of all sampling frames, participants receiving homecare services had the highest prevalence at 14.6% (95% CI: 9.9–20.0%). Malnutrition prevalence in rural communities (9.9%; 95% CI: 4.5–16.8%) was double that in urban communities (5.7%; 95% CI: 4.2–7.3%) and higher among females than males (odds ratio = 1.45 [95% CI: 1.27–1.66]; P < 0.00001).
the results of this review provide strategic insight to develop public and community health priorities for preventing malnutrition and associated poor health outcomes.
Introduction
From 2010 to 2030, the worldwide population growth of persons ≥65 years is expected to increase by 442 million, making it the fastest growing age group [1]. Governments around the world have committed to promote the independence and wellness of older adults [2, 3], and importantly, these policies align with the desires of the older adult community, who wish to remain in their own homes for as long as possible [2, 4]. However, protein-energy malnutrition (herein referred to as ‘malnutrition’) presents a significant risk factor for nursing home admission and mortality [5, 6]. Malnutrition occurs when energy and protein requirements are not met over time, leading to involuntary muscle mass and visceral wasting, as well as blood and immune cell depletion, with or without fat loss [7]. Due to physical, cognitive and environmental changes that occur in ageing, malnutrition occurs most commonly in older adults; however, the prevalence is also known to vary based on geographical region (representing culture, resource availability and socio-economics), rurality, sex and sampling frame [7–9]. The community setting refers to a person living independently in their own home and not admitted to aged care, acute care or sub-acute care. To date, research of malnutrition in older adults has largely focussed on healthcare settings and less is known about the community living older adult.
In regards to malnutrition, there are three accepted categories of nutritional status: well nourished, at risk of malnutrition and malnourished [10]. Those who are malnourished may be further categorised according to the severity of their malnutrition or the aetiology [11, 12]. A diagnosis of malnutrition is made using a nutrition assessment tool, three of which are validated for use in older adults [13]: the Subjective Global Assessment [14], the Scored Patient-Generated Subjective Global Assessment [15, 16] and the Mini Nutritional Assessment (MNA) [17].
A recent systematic review and meta-analysis reviewed the prevalence of malnutrition reported by studies using the MNA; and found it ranged from 3 to 11% depending on the setting [9]. Settings included community, hospital, nursing home, long-term care, rehabilitation and sub-acute care. Although the review included a high number of studies reporting malnutrition prevalence in the community setting (n = 110 studies), only one database was searched and the analysis did not conduct sub-group analysis examining sex, rurality or geographical regions and countries. Furthermore, assessment by only the MNA may not accurately reflect malnutrition prevalence as the MNA has been found to overestimate the risk of malnutrition, but underdiagnose malnutrition in some settings [8].
Therefore, there is a need to review the prevalence of malnutrition in the older community setting, with studies from other databases included that determine malnutrition using any validated nutrition assessment tool with consideration given to the characteristics of the sample population such as sex, country and rurality. Such data may be used for planning national and international health priorities and services.
Research aim
This systematic review, meta-analysis and meta-regression seeks to determine the prevalence of malnutrition among older adults living independently in the community according to geographical region, sampling frame, rurality and sex.
Methods
A systematic review of the literature was conducted as part of the Malnutrition in the Ageing Community Review (MACRo) Study [13]. This study was reported according to PRISMA guidelines [18] and prospectively registered with PROSPERO (CRD42016051241).
Search strategy
The search strategy has been published previously [13] and is shown in Appendix 1, available in Age and Ageing online. Briefly, published studies in any language were searched for in the electronic databases CENTRAL, CIHAHL (via Ebscohost), EMBASE, Health Source: Nursing/Academic Edition (via Ebscohost), PubMed and Web of Science for publications from database inception to 1 September 2016. The controlled vocabulary of each database was used.
After citations were identified from all databases, duplicates were removed. Two authors scanned the titles and abstracts of studies identified by the search for their potential eligibility (D.C. and S.M.). Full-text articles relating to inclusion criteria were also assessed independently by two authors (D.C. and S.M.); with disagreements managed by consensus between the two authors.
Types of studies
This review considered experimental study designs (including randomised controlled trials, non-randomised controlled trials, quasi-experimental studies, before and after studies), prospective and retrospective cohort studies, case–control studies and cross-sectional studies for inclusion. Excluded study types were abstracts, conference papers, qualitative studies, study protocols, opinions, commentaries, news articles and review papers. Studies in Spanish were translated by S.M., and studies in other languages were translated using Google Translate where possible [19].
If nutrition assessment was measured following a nutrition intervention study, it was excluded as this was not considered to reflect the prevalence of the condition; therefore, intervention studies were only included if baseline data were reported (both intervention and control groups considered) or follow-up data were available in the control group. If data were not reported specifically for the malnourished groups (e.g. reporting MNA category of malnutrition using score <17), studies were excluded as they did not report malnutrition prevalence. If multiple studies reported the prevalence of malnutrition based on the one sample; the study with the most complete data, or otherwise the first published study, was selected and the other studies excluded as ‘data duplicates’.
Types of participants
Studies that included older adult samples with a mean age of ≥65 years living independently in the community, who were assessed for protein-energy malnutrition using the Patient-Generated Subjective Global Assessment, MNA or Subjective Global Assessment were included. Older adults were considered to be community-dwelling if they lived in their own homes at the time of the study, but could be accessed by a range of sampling frames including primary care facilities, homecare agencies, post-hospital discharge, hospital outpatients, community social and/or religious groups, or other methods to access people who live in their own homes. Studies that screened or assessed participants in acute or sub-acute facilities, living in residential aged care (including nursing homes), or were disease-specific samples (e.g. the entire sample had dementia or cancer) were excluded.
Data extraction
Data were extracted from the published papers into a standardised Microsoft Excel (version 1805, 2016 MSO [16.9330.2073]) spreadsheet by one author (M.C. or H.M.). To minimise errors in data extraction, 20% of papers underwent full data checking by a second independent author (M.C., H.M., D.C., S.M. or W.M.) and all data extracted was examined for consistency by S.M.
The selected prevalence statistic extracted varied based on study type. Baseline data were utilised excepting baseline measure taken during an inpatient admission, in which the first measurement taken in the community setting was then selected. To enhance understanding and generalisability, the study populations, who conducted the screening and assessments, and how the sample was accessed were described for each included study. The percentage of malnourished or well-nourished participants was converted to the number of participants in each category using the sample size post-attrition for the relevant time point. The number of participants in each category were reported for the total relevant sample as well as males and females separately, if possible. Participant samples were reported as urban (city/metropolitan) or rural (including remote, regional, villages and towns < 10,000 population size), combined, or nationally representative samples where possible. All age data were summarised to whole numbers. To allow for meta-analysis, where the number of participants of each sex was not reported post-attrition, the values were estimated using the percentage of each sex in the pre-attrition sample.
Assessment of methodological quality
Two authors (M.C., H.M., S.M., W.M. or D.C.) critically appraised each study independently using the Academy of Nutrition and Dietetics’ Quality Criteria Checklist: Primary Research [20]. This tool designates studies as having positive (strong quality), neutral (neither strong nor weak quality) or negative (weak quality) assessment [20]. Disagreements between authors for study quality was managed by consensus.
Meta-analysis
The prevalence of malnutrition was reported as a percentage of the whole sample. The number of cases was considered as a binomial variable ‘malnourished’ or ‘well-nourished’. Well-nourished included the ‘normal nutrition status’ and ‘at risk of malnutrition’ categories for the MNA; or the rating ‘A’ for both the Subjective Global Assessment and Patient-Generated Subjective Global Assessment. Malnourished included the ‘malnourished’ category for the MNA; and both the ‘B = moderately (or suspected of being) malnourished’ and ‘C = severely malnourished’ categories for both the Subjective Global Assessment and Patient-Generated Subjective Global Assessment tools. This dichotomisation of nutrition status according to each of the assessment tools is supported by a diagnostic validity study in older adults [16].
To address weighting errors for studies with low malnutrition prevalence, data were transformed using double arcsine transformation [21]. The prevalence of malnutrition, which was assumed to follow a binomial distribution, was pooled using the inverse of the variance of transformed data via MetaXL [Version 5.3, EpiGear International, available from: http://www.epigear.com]. For final presentation, the pooled data were transformed back to a proportion with 95% confidence intervals. A random effects model was chosen due to the recognition of substantial variability in the presentation of malnutrition across individuals and sampling frames. Separate analyses were performed for the sampling frame, country (or groups of countries of similar culture and economics if there were less than three samples in a country) and rurality.
The impact of gender on malnutrition prevalence was calculated as an odds ratio with 95% confidence intervals using the Mantel-Haenszel test random effects model in RevMan [Review Manager 5, Version 5.3, 2014, Cochrane Informatics & Knowledge Management Department].
As meta-analyses of malnutrition prevalence are expected to have high heterogeneity [9], an I2 > 70% was considered substantial. Sensitivity analysis was performed for any pooled data which showed substantial heterogeneity, whereby analysis was repeated by removing studies from the analysis which differed from the majority of included studies based on study quality, the type of nutrition assessment tool, and study sample characteristics. Any criteria used for removing studies during meta-analysis was reported in the results table. However, for the prevalence of malnutrition according to rurality, sensitivity analysis was not performed due to the risk of biasing the pooled prevalence through removal of studies representing all geographical areas (e.g. if neutral study quality studies were removed, approximately half of the included countries would not be represented in the results).
Meta-regression
Where pooled prevalence from ≥10 studies via meta-analysis had substantial heterogeneity (I2 > 70%) remaining after sensitivity analysis, meta-regression was performed using Stata version 14.2 (StataCorp LP, Texas, USA, 2015). Nine meta-regression models were performed using a relevant combination of covariates for each model. Covariates considered were geographical location (either continent, geographical region or country), rurality, study quality, study design, sampling frame, nutrition screening prior to assessment, assessment tool and sex ratio. The covariates included were modified as relevant for each model, for example, rurality was not a covariate for the meta-regression of rural or urban study samples, and assessment tool was not included if all studies used the MNA.
Results
Search results and included studies
There were 111 included studies (Figure 1), which reported data on 114 samples (Appendix 2, available in Age and Ageing online). The majority of prevalence data was reported by cross-sectional studies (n = 89), followed by prospective observational studies (n = 13), baseline data from intervention studies (n = 7) then retrospective studies (n = 2). The method used by included studies to report the age of participants varied greatly between studies, preventing a summary of age ranges (Appendix 2, available in Age and Ageing online). Samples from 38 countries were included, with the majority from Europe (n = 51 samples) and Asia (n = 38 samples). There were 12 samples from North America and seven from Oceania (all from Australia), with only four samples from South America and two from Africa. These studies had a total participant sample size of 69,702, nearly half of which were participants from Spain (n = 30,190 participants). Participants from studies conducted in China comprised the second largest group by country (n = 8,871 participants) followed by Turkey (n = 5,487 participants) (Table 1).
The pooled prevalence of protein-energy malnutrition in community-dwelling older adults by country and/or geographical region, presented from lowest to highest prevalence.
| Geographical region . | Countries included in meta-analysis . | Number of studies . | Sample size . | Qualitya . | Prevalence of malnutritionb (% [95% CI]) . | Heterogeneity (I2, %) . | Prevalence of malnutritionb with sensitivity analysis (% [95% CI]) . | Heterogeneity with sensitivity analysis (I2, %) . | Sensitivity analysis: reason for removed studies . |
|---|---|---|---|---|---|---|---|---|---|
| Northern Europe | Netherlands, Sweden | 17 | 2,267 | 5/3/0 | 2.5 [0.1–7.1] | 95.9 | 0.8 [0.2–1.7] | 50.2 | Age > 80 yearsd |
| East Asia | China | 10 | 8,871 | 2/7/0d | 2.4 [1.5–3.5] | 83.3 | 1.6 [0.8–2.6] | 61.9 | Setting other than ‘community’ |
| South America | Brazil, Chile | 31 | 2,005 | 2/2/0 | 1.7 [0.9–2.8] | 52.0 | – | – | – |
| European Russia | Russia | 1 (not pooled)c | 611 | 1/0/0 | 1.8 | – | – | – | – |
| Northern Europe | Denmark, Finland | 13 | 691 | 0/4/0 | 1.9 [0.6–3.8] | 37.6 | – | – | – |
| Central Europe | Poland | 4 | 2,098 | 2/2/0 | 2.7 [0.1–7.9] | 95.5 | – | – | – |
| Western Europe | Ireland, United Kingdom | 31 | 847 | 1/3/0 | 2.8 [0.0–7.3] | 86.5 | – | – | – |
| Middle East | Turkey | 6 | 5,487 | 4/2/0 | 5.1 [1.6–10.1] | 97.6 | 3.0 [2.2–3.9] | 0.0 | Setting other than ‘community’ |
| Central Europe | Germany | 4 | 705 | 1/3/0 | 4.3 [0.0–14.1] | 95.8 | – | – | – |
| Southwestern Europe | Spain | 19 | 30,190 | 7/12/0 | 4.8 [3.2–6.7] | 95.0 | – | – | – |
| Australia/New Zealand | Australia | 7 | 871 | 3/4/0 | 18.1 [4.3–37.5] | 97.1 | 6.0 [4.4–8.2] | 14.7 | Assessment tools SGA and PG-SGA |
| Middle East | Israel, Lebanon | 13 | 2,762 | 2/2/0 | 6.1 [3.3–9.7] | 90.8 | – | – | – |
| East Asia | Japan, South Korea | 41 | 905 | 2/2/0 | 6.4 [0.7–16.1] | 95.0 | – | – | – |
| North America | Canada, United States of America | 15 | 683 | 3/3/0 | 6 [1.4–17.5] | 92.3 | – | – | – |
| South Asia | India, Bangladesh | 31 | 1,126 | 2/2/0 | 7.8 [0.1–17.7] | 92.1 | – | – | – |
| Middle East | Iran | 6 | 4,507 | 2/4/0 | 7.3 [4.7–10.5] | 90.9 | – | – | – |
| Southern Europe | Italy, France | 22 | 1,061 | 1/3/0 | 11.0 [0.0–50.2] | 99.5 | – | – | – |
| Central America/Caribbean | Cuba, Mexico | 15 | 1,317 | 3/3/0 | 12.6 [2.5–27.6] | 96.8 | – | – | – |
| Central and West Africa | Democratic Republic of the Congo, Nigeria | 11 | 870 | 1/1/0 | 14.5 [0.0–40.4] | 98.5 | – | – | – |
| Central Europe | Czech Republic, Austria | 21 | 673 | 1/2/0 | 16.5 [4.1–33.8] | 94.5 | – | – | – |
| Southeast Asia | Laos Singapore, Thailand | 111 | 1,155 | 2/1/0 | 24.6 [0.0–67.9] | 99.5 | – | – | – |
| Geographical region . | Countries included in meta-analysis . | Number of studies . | Sample size . | Qualitya . | Prevalence of malnutritionb (% [95% CI]) . | Heterogeneity (I2, %) . | Prevalence of malnutritionb with sensitivity analysis (% [95% CI]) . | Heterogeneity with sensitivity analysis (I2, %) . | Sensitivity analysis: reason for removed studies . |
|---|---|---|---|---|---|---|---|---|---|
| Northern Europe | Netherlands, Sweden | 17 | 2,267 | 5/3/0 | 2.5 [0.1–7.1] | 95.9 | 0.8 [0.2–1.7] | 50.2 | Age > 80 yearsd |
| East Asia | China | 10 | 8,871 | 2/7/0d | 2.4 [1.5–3.5] | 83.3 | 1.6 [0.8–2.6] | 61.9 | Setting other than ‘community’ |
| South America | Brazil, Chile | 31 | 2,005 | 2/2/0 | 1.7 [0.9–2.8] | 52.0 | – | – | – |
| European Russia | Russia | 1 (not pooled)c | 611 | 1/0/0 | 1.8 | – | – | – | – |
| Northern Europe | Denmark, Finland | 13 | 691 | 0/4/0 | 1.9 [0.6–3.8] | 37.6 | – | – | – |
| Central Europe | Poland | 4 | 2,098 | 2/2/0 | 2.7 [0.1–7.9] | 95.5 | – | – | – |
| Western Europe | Ireland, United Kingdom | 31 | 847 | 1/3/0 | 2.8 [0.0–7.3] | 86.5 | – | – | – |
| Middle East | Turkey | 6 | 5,487 | 4/2/0 | 5.1 [1.6–10.1] | 97.6 | 3.0 [2.2–3.9] | 0.0 | Setting other than ‘community’ |
| Central Europe | Germany | 4 | 705 | 1/3/0 | 4.3 [0.0–14.1] | 95.8 | – | – | – |
| Southwestern Europe | Spain | 19 | 30,190 | 7/12/0 | 4.8 [3.2–6.7] | 95.0 | – | – | – |
| Australia/New Zealand | Australia | 7 | 871 | 3/4/0 | 18.1 [4.3–37.5] | 97.1 | 6.0 [4.4–8.2] | 14.7 | Assessment tools SGA and PG-SGA |
| Middle East | Israel, Lebanon | 13 | 2,762 | 2/2/0 | 6.1 [3.3–9.7] | 90.8 | – | – | – |
| East Asia | Japan, South Korea | 41 | 905 | 2/2/0 | 6.4 [0.7–16.1] | 95.0 | – | – | – |
| North America | Canada, United States of America | 15 | 683 | 3/3/0 | 6 [1.4–17.5] | 92.3 | – | – | – |
| South Asia | India, Bangladesh | 31 | 1,126 | 2/2/0 | 7.8 [0.1–17.7] | 92.1 | – | – | – |
| Middle East | Iran | 6 | 4,507 | 2/4/0 | 7.3 [4.7–10.5] | 90.9 | – | – | – |
| Southern Europe | Italy, France | 22 | 1,061 | 1/3/0 | 11.0 [0.0–50.2] | 99.5 | – | – | – |
| Central America/Caribbean | Cuba, Mexico | 15 | 1,317 | 3/3/0 | 12.6 [2.5–27.6] | 96.8 | – | – | – |
| Central and West Africa | Democratic Republic of the Congo, Nigeria | 11 | 870 | 1/1/0 | 14.5 [0.0–40.4] | 98.5 | – | – | – |
| Central Europe | Czech Republic, Austria | 21 | 673 | 1/2/0 | 16.5 [4.1–33.8] | 94.5 | – | – | – |
| Southeast Asia | Laos Singapore, Thailand | 111 | 1,155 | 2/1/0 | 24.6 [0.0–67.9] | 99.5 | – | – | – |
aAcademy of Nutrition and Dietetics Quality Criteria Checklist rating (number of positive/neutral/negative).
bDetermined by MNA score < 17 or Patient-Generated Subjective Global Assessment or Subjective Global Assessment rating of B and C.
cData not pooled as there were no other samples with reasonable geographical and economical similarities.
dMajority of studies included in this meta-analysis had a younger cohort (65–75 years), therefore the few studies with older cohorts were excluded age was found to be a source of heterogeneity.
eChan et al. [22], which was conducted in China, could not be sufficiently translated to allow for assessment of study quality.
The pooled prevalence of protein-energy malnutrition in community-dwelling older adults by country and/or geographical region, presented from lowest to highest prevalence.
| Geographical region . | Countries included in meta-analysis . | Number of studies . | Sample size . | Qualitya . | Prevalence of malnutritionb (% [95% CI]) . | Heterogeneity (I2, %) . | Prevalence of malnutritionb with sensitivity analysis (% [95% CI]) . | Heterogeneity with sensitivity analysis (I2, %) . | Sensitivity analysis: reason for removed studies . |
|---|---|---|---|---|---|---|---|---|---|
| Northern Europe | Netherlands, Sweden | 17 | 2,267 | 5/3/0 | 2.5 [0.1–7.1] | 95.9 | 0.8 [0.2–1.7] | 50.2 | Age > 80 yearsd |
| East Asia | China | 10 | 8,871 | 2/7/0d | 2.4 [1.5–3.5] | 83.3 | 1.6 [0.8–2.6] | 61.9 | Setting other than ‘community’ |
| South America | Brazil, Chile | 31 | 2,005 | 2/2/0 | 1.7 [0.9–2.8] | 52.0 | – | – | – |
| European Russia | Russia | 1 (not pooled)c | 611 | 1/0/0 | 1.8 | – | – | – | – |
| Northern Europe | Denmark, Finland | 13 | 691 | 0/4/0 | 1.9 [0.6–3.8] | 37.6 | – | – | – |
| Central Europe | Poland | 4 | 2,098 | 2/2/0 | 2.7 [0.1–7.9] | 95.5 | – | – | – |
| Western Europe | Ireland, United Kingdom | 31 | 847 | 1/3/0 | 2.8 [0.0–7.3] | 86.5 | – | – | – |
| Middle East | Turkey | 6 | 5,487 | 4/2/0 | 5.1 [1.6–10.1] | 97.6 | 3.0 [2.2–3.9] | 0.0 | Setting other than ‘community’ |
| Central Europe | Germany | 4 | 705 | 1/3/0 | 4.3 [0.0–14.1] | 95.8 | – | – | – |
| Southwestern Europe | Spain | 19 | 30,190 | 7/12/0 | 4.8 [3.2–6.7] | 95.0 | – | – | – |
| Australia/New Zealand | Australia | 7 | 871 | 3/4/0 | 18.1 [4.3–37.5] | 97.1 | 6.0 [4.4–8.2] | 14.7 | Assessment tools SGA and PG-SGA |
| Middle East | Israel, Lebanon | 13 | 2,762 | 2/2/0 | 6.1 [3.3–9.7] | 90.8 | – | – | – |
| East Asia | Japan, South Korea | 41 | 905 | 2/2/0 | 6.4 [0.7–16.1] | 95.0 | – | – | – |
| North America | Canada, United States of America | 15 | 683 | 3/3/0 | 6 [1.4–17.5] | 92.3 | – | – | – |
| South Asia | India, Bangladesh | 31 | 1,126 | 2/2/0 | 7.8 [0.1–17.7] | 92.1 | – | – | – |
| Middle East | Iran | 6 | 4,507 | 2/4/0 | 7.3 [4.7–10.5] | 90.9 | – | – | – |
| Southern Europe | Italy, France | 22 | 1,061 | 1/3/0 | 11.0 [0.0–50.2] | 99.5 | – | – | – |
| Central America/Caribbean | Cuba, Mexico | 15 | 1,317 | 3/3/0 | 12.6 [2.5–27.6] | 96.8 | – | – | – |
| Central and West Africa | Democratic Republic of the Congo, Nigeria | 11 | 870 | 1/1/0 | 14.5 [0.0–40.4] | 98.5 | – | – | – |
| Central Europe | Czech Republic, Austria | 21 | 673 | 1/2/0 | 16.5 [4.1–33.8] | 94.5 | – | – | – |
| Southeast Asia | Laos Singapore, Thailand | 111 | 1,155 | 2/1/0 | 24.6 [0.0–67.9] | 99.5 | – | – | – |
| Geographical region . | Countries included in meta-analysis . | Number of studies . | Sample size . | Qualitya . | Prevalence of malnutritionb (% [95% CI]) . | Heterogeneity (I2, %) . | Prevalence of malnutritionb with sensitivity analysis (% [95% CI]) . | Heterogeneity with sensitivity analysis (I2, %) . | Sensitivity analysis: reason for removed studies . |
|---|---|---|---|---|---|---|---|---|---|
| Northern Europe | Netherlands, Sweden | 17 | 2,267 | 5/3/0 | 2.5 [0.1–7.1] | 95.9 | 0.8 [0.2–1.7] | 50.2 | Age > 80 yearsd |
| East Asia | China | 10 | 8,871 | 2/7/0d | 2.4 [1.5–3.5] | 83.3 | 1.6 [0.8–2.6] | 61.9 | Setting other than ‘community’ |
| South America | Brazil, Chile | 31 | 2,005 | 2/2/0 | 1.7 [0.9–2.8] | 52.0 | – | – | – |
| European Russia | Russia | 1 (not pooled)c | 611 | 1/0/0 | 1.8 | – | – | – | – |
| Northern Europe | Denmark, Finland | 13 | 691 | 0/4/0 | 1.9 [0.6–3.8] | 37.6 | – | – | – |
| Central Europe | Poland | 4 | 2,098 | 2/2/0 | 2.7 [0.1–7.9] | 95.5 | – | – | – |
| Western Europe | Ireland, United Kingdom | 31 | 847 | 1/3/0 | 2.8 [0.0–7.3] | 86.5 | – | – | – |
| Middle East | Turkey | 6 | 5,487 | 4/2/0 | 5.1 [1.6–10.1] | 97.6 | 3.0 [2.2–3.9] | 0.0 | Setting other than ‘community’ |
| Central Europe | Germany | 4 | 705 | 1/3/0 | 4.3 [0.0–14.1] | 95.8 | – | – | – |
| Southwestern Europe | Spain | 19 | 30,190 | 7/12/0 | 4.8 [3.2–6.7] | 95.0 | – | – | – |
| Australia/New Zealand | Australia | 7 | 871 | 3/4/0 | 18.1 [4.3–37.5] | 97.1 | 6.0 [4.4–8.2] | 14.7 | Assessment tools SGA and PG-SGA |
| Middle East | Israel, Lebanon | 13 | 2,762 | 2/2/0 | 6.1 [3.3–9.7] | 90.8 | – | – | – |
| East Asia | Japan, South Korea | 41 | 905 | 2/2/0 | 6.4 [0.7–16.1] | 95.0 | – | – | – |
| North America | Canada, United States of America | 15 | 683 | 3/3/0 | 6 [1.4–17.5] | 92.3 | – | – | – |
| South Asia | India, Bangladesh | 31 | 1,126 | 2/2/0 | 7.8 [0.1–17.7] | 92.1 | – | – | – |
| Middle East | Iran | 6 | 4,507 | 2/4/0 | 7.3 [4.7–10.5] | 90.9 | – | – | – |
| Southern Europe | Italy, France | 22 | 1,061 | 1/3/0 | 11.0 [0.0–50.2] | 99.5 | – | – | – |
| Central America/Caribbean | Cuba, Mexico | 15 | 1,317 | 3/3/0 | 12.6 [2.5–27.6] | 96.8 | – | – | – |
| Central and West Africa | Democratic Republic of the Congo, Nigeria | 11 | 870 | 1/1/0 | 14.5 [0.0–40.4] | 98.5 | – | – | – |
| Central Europe | Czech Republic, Austria | 21 | 673 | 1/2/0 | 16.5 [4.1–33.8] | 94.5 | – | – | – |
| Southeast Asia | Laos Singapore, Thailand | 111 | 1,155 | 2/1/0 | 24.6 [0.0–67.9] | 99.5 | – | – | – |
aAcademy of Nutrition and Dietetics Quality Criteria Checklist rating (number of positive/neutral/negative).
bDetermined by MNA score < 17 or Patient-Generated Subjective Global Assessment or Subjective Global Assessment rating of B and C.
cData not pooled as there were no other samples with reasonable geographical and economical similarities.
dMajority of studies included in this meta-analysis had a younger cohort (65–75 years), therefore the few studies with older cohorts were excluded age was found to be a source of heterogeneity.
eChan et al. [22], which was conducted in China, could not be sufficiently translated to allow for assessment of study quality.
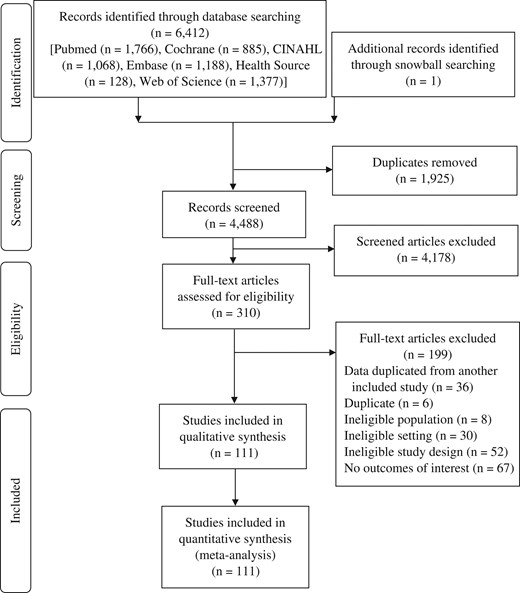
PRISMA flow-chart of studies screened and reviewed for inclusion in the Malnutrition in the Ageing Community Review Study of malnutrition prevalence in community-dwelling older adults.
The most frequent nutrition assessment tool was the MNA (n = 112 samples), with the Subjective Global Assessment used in three samples and the Patient-Generated Subjective Global Assessment used in one. Nutrition assessment was most frequently performed by nurses (n = 22 studies); however, 40 studies did not report who completed the nutrition assessment.
Study quality
In total, 65 (59%) studies were rated as having neutral quality, and 46 (41%) were rated as having positive quality. There was one study, with an English abstract, in which the methods of the paper could not be translated, and therefore the quality assessment could not be applied [22]. There were three studies published in Spanish in which the document could not be translated by Google Translate, and therefore the quality rating was reviewed by one author only (S.M.) who had familiarity with the language.
The international prevalence of malnutrition
Appendix 2, available in Age and Ageing online reports the prevalence of malnutrition reported by each study (not-pooled). The pooled prevalence of malnutrition in the community setting in various countries and/or geographical regions is shown in Table 1 and graphically represented on a world map in Appendix 3, available in Age and Ageing online.
All countries and/or geographical regions could be pooled excepting European Russia, which included only one study sample and was not similar to other included studies in terms of geography, culture and economy. Europe had the largest number of areas analysed for pooled prevalence with nine regions (14 countries) analysed, where prevalence ranged from 0.8% (in the Netherlands and Sweden) to 11.0% (Italy and France). Data from 12 countries in Asia were analysed in seven pooled geographical regions, with prevalence ranging from 1.6% (in China) to 24.6% (in Laos, Singapore and Thailand). North America (USA and Canada) had 7.6% of community-dwelling older adults with malnutrition, whereas Central America (Mexico and Cuba) had 12.6%. Australia (6.0% prevalence), Africa (14.5% prevalence) and South America (1.7% prevalence) had one area of pooled prevalence each respectively. After sensitivity analysis was conducted, heterogeneity remained substantial (I2 > 70%) in 14 of the 21 analyses for malnutrition prevalence by geographical region.
Of all geographical regions, only Spain (n = 17 studies) met the criteria for meta-regression. The covariates of sampling frame, percent female sex and study quality were included in the model which was found to explain 75.53% of the variation in malnutrition prevalence (adjusted R2 = 75.53); however, the model had substantial heterogeneity (I2 residual = 92.10%) remaining after adjusting for the covariates. One percent increase in the proportion of females in the sample was found to predict an increase in the prevalence of malnutrition by 0.4% (coefficient: 0.0038 [95% CI: 0.001–0.007]; P = 0.016). Each sampling frame was found to cause 3% variance in malnutrition prevalence in Spain (coefficient: 0.0290 [95% CI: 0.02–0.042]; P < 0.001). Study quality was not a significant covariate in the model.
The prevalence of malnutrition in the community according to the sampling frame
Table 2 outlines the pooled prevalence of protein-energy malnutrition in community-dwelling older adults according to the sampling frame in which the participants were recruited. The two nationally representative older samples had the lowest pooled prevalence of malnutrition at 3.2% (representing Taiwan and Spain). The next lowest prevalence was in the general community at 4.7%, representing those living at home and not accessed through any form of health or social service. South America had the lowest pooled prevalence of malnutrition in the general community at 2.1%, and North America had the highest at 6.1%. However, in the general community Africa had the highest prevalence at 28% which came from one sample in the Democratic Republic of the Congo. Of all community sampling frames, participants sampled through homecare services had the highest prevalence of malnutrition at 14.6%, where Australia had the lowest pooled prevalence of 6.3% and Asia had the highest at 14.6%.
The pooled prevalence of protein energy malnutrition in community-dwelling older adults by type of community setting overall and per continent.
| Community setting . | Number of studies . | Sample size . | Qualitya . | Prevalence of malnutritionb (% [95% CI]) . | Heterogeneity (I2, %) . | Prevalence of malnutritionb with sensitivity analysis (% [95% CI]) . | Heterogeneity with sensitivity analysis (I2, %) . | Sensitivity analysis: reason for removed studies . |
|---|---|---|---|---|---|---|---|---|
| Community | 63 | 50,905 | 28/35/0 | 4.7 [3.6–6.1] | 97.1 | – | – | – |
| Asia | 27 | 16,476 | 13/14/0 | 5.7 [3.3–8.6] | 98.0 | – | – | – |
| Europe | 27 | 31,001 | 11/16/0 | 2.8 [1.7–4.2] | 94.9 | – | – | – |
| North America | 4 | 1,112 | 2/2/0 | 11.5 [3.5–22.7] | 93.2 | 6.1 [3.5–9.2] | 0.0 | Neutral/negative quality |
| South America | 3 | 1,908 | 2/1/0 | 2.1 [1.4–3.0] | 25.9 | – | – | – |
| Australia (not pooled)c | 1 | 38 | 0/1/0 | 5.3 | – | – | – | – |
| Africa (not pooled)c | 1 | 370 | 0/1/0 | 28.4 | – | – | – | – |
| Homecare | 19 | 3,283 | 7/12/0 | 14.6 [9.9–20.0] | 93.9 | – | – | – |
| Asia | 2 | 462 | 1/1/0 | 14.6 [2.1–33.7] | 95.2 | – | – | – |
| Australia | 4 | 598 | 2/2/0 | 26.4 [1.2–63.1] | 98.4 | 6.3 [3.5–9.9] | 53.5 | Neutral/negative quality |
| Europe | 12 | 2,025 | 3/9/0 | 11.2 [7.4–15.5] | 86.9 | – | – | – |
| North America (not pooled)c | 1 | 198 | 1/0/0 | 12.1 | – | – | – | – |
| Hospital outpatient | 4 | 1,901 | 2/2/0 | 5.1 [0.1–14.6] | 97.3 | – | – | – |
| Asia | 2 | 1,304 | 1/1/0 | 10.2 [0.0–28.3] | 98.2 | – | – | – |
| Africa (not pooled)c | 1 | 500 | 1/0/0 | 7.8 | – | – | – | – |
| South America (not pooled)c | 1 | 97 | 0/1/0 | 0.0 | – | – | – | – |
| Nationally representative | 2 | 5,745 | 1/1/0 | 3.2 [2.4–3.7] | 53.9 | – | – | – |
| Asia (not pooled)c | 1 | 2,674 | 0/1/0 | 2.7 | – | – | – | – |
| Europe (not pooled)c | 1 | 3,071 | 1/0/0 | 3.3 | – | – | – | – |
| Post-hospital discharge | 2 | 305 | 1/1/0 | 5.1 [2.9–7.8] | 0.0 N/A | – | – | – |
| Australia (not pooled)c | 1 | 223 | 1/0/0 | 4.9 | N/A | |||
| Germany (not pooled)c | 1 | 82 | 0/1/0 | 4.9 | ||||
| Primary healthcare centre | 19 | 6,639 | 9/10/0 | 7.3 [2.4–14.2] | 98.6 | – | – | – |
| Asia | 4 | 3,151 | 2/2/0 | 7.7 [5.4–10.4] | 63.8 | – | – | – |
| Europe | 9 | 2,867 | 4/5/0 | 5.7 [0.0–17.4] | 99.1 | – | – | – |
| North America | 6 | 621 | 3/3/0 | 9.5 [0.0–26.9] | 95.8 | – | – | – |
| Other | 5 | 924 | 0/4/0d | 3.3 [1.9–5.0] | 23.8 | – | – | – |
| Asia | 2 | 746 | 0/1/0d | 3.6 [2.3–5.0] | 0.0 | – | – | – |
| Australia (not pooled)c | 1 | 12 | 0/1/0 | 16.7 | – | – | – | – |
| Europe (not pooled)c | 1 | 97 | 0/1/0 | 1.0 | – | – | – | – |
| North America (not pooled)c | 1 | 69 | 0/1/0 | 2.9 | – | – | – | – |
| Community setting . | Number of studies . | Sample size . | Qualitya . | Prevalence of malnutritionb (% [95% CI]) . | Heterogeneity (I2, %) . | Prevalence of malnutritionb with sensitivity analysis (% [95% CI]) . | Heterogeneity with sensitivity analysis (I2, %) . | Sensitivity analysis: reason for removed studies . |
|---|---|---|---|---|---|---|---|---|
| Community | 63 | 50,905 | 28/35/0 | 4.7 [3.6–6.1] | 97.1 | – | – | – |
| Asia | 27 | 16,476 | 13/14/0 | 5.7 [3.3–8.6] | 98.0 | – | – | – |
| Europe | 27 | 31,001 | 11/16/0 | 2.8 [1.7–4.2] | 94.9 | – | – | – |
| North America | 4 | 1,112 | 2/2/0 | 11.5 [3.5–22.7] | 93.2 | 6.1 [3.5–9.2] | 0.0 | Neutral/negative quality |
| South America | 3 | 1,908 | 2/1/0 | 2.1 [1.4–3.0] | 25.9 | – | – | – |
| Australia (not pooled)c | 1 | 38 | 0/1/0 | 5.3 | – | – | – | – |
| Africa (not pooled)c | 1 | 370 | 0/1/0 | 28.4 | – | – | – | – |
| Homecare | 19 | 3,283 | 7/12/0 | 14.6 [9.9–20.0] | 93.9 | – | – | – |
| Asia | 2 | 462 | 1/1/0 | 14.6 [2.1–33.7] | 95.2 | – | – | – |
| Australia | 4 | 598 | 2/2/0 | 26.4 [1.2–63.1] | 98.4 | 6.3 [3.5–9.9] | 53.5 | Neutral/negative quality |
| Europe | 12 | 2,025 | 3/9/0 | 11.2 [7.4–15.5] | 86.9 | – | – | – |
| North America (not pooled)c | 1 | 198 | 1/0/0 | 12.1 | – | – | – | – |
| Hospital outpatient | 4 | 1,901 | 2/2/0 | 5.1 [0.1–14.6] | 97.3 | – | – | – |
| Asia | 2 | 1,304 | 1/1/0 | 10.2 [0.0–28.3] | 98.2 | – | – | – |
| Africa (not pooled)c | 1 | 500 | 1/0/0 | 7.8 | – | – | – | – |
| South America (not pooled)c | 1 | 97 | 0/1/0 | 0.0 | – | – | – | – |
| Nationally representative | 2 | 5,745 | 1/1/0 | 3.2 [2.4–3.7] | 53.9 | – | – | – |
| Asia (not pooled)c | 1 | 2,674 | 0/1/0 | 2.7 | – | – | – | – |
| Europe (not pooled)c | 1 | 3,071 | 1/0/0 | 3.3 | – | – | – | – |
| Post-hospital discharge | 2 | 305 | 1/1/0 | 5.1 [2.9–7.8] | 0.0 N/A | – | – | – |
| Australia (not pooled)c | 1 | 223 | 1/0/0 | 4.9 | N/A | |||
| Germany (not pooled)c | 1 | 82 | 0/1/0 | 4.9 | ||||
| Primary healthcare centre | 19 | 6,639 | 9/10/0 | 7.3 [2.4–14.2] | 98.6 | – | – | – |
| Asia | 4 | 3,151 | 2/2/0 | 7.7 [5.4–10.4] | 63.8 | – | – | – |
| Europe | 9 | 2,867 | 4/5/0 | 5.7 [0.0–17.4] | 99.1 | – | – | – |
| North America | 6 | 621 | 3/3/0 | 9.5 [0.0–26.9] | 95.8 | – | – | – |
| Other | 5 | 924 | 0/4/0d | 3.3 [1.9–5.0] | 23.8 | – | – | – |
| Asia | 2 | 746 | 0/1/0d | 3.6 [2.3–5.0] | 0.0 | – | – | – |
| Australia (not pooled)c | 1 | 12 | 0/1/0 | 16.7 | – | – | – | – |
| Europe (not pooled)c | 1 | 97 | 0/1/0 | 1.0 | – | – | – | – |
| North America (not pooled)c | 1 | 69 | 0/1/0 | 2.9 | – | – | – | – |
aAcademy of Nutrition and Dietetics Quality Criteria Checklist rating (number of positive/neutral/negative).
bDetermined by MNA score < 17 or Patient-Generated Subjective Global Assessment or Subjective Global Assessment rating of B and C.
cData not pooled as there were no other samples in the same continent.
dChan et al. [22], which was conducted in an undescribed community setting in China, could not be sufficiently translated to allow for assessment of study quality.
The pooled prevalence of protein energy malnutrition in community-dwelling older adults by type of community setting overall and per continent.
| Community setting . | Number of studies . | Sample size . | Qualitya . | Prevalence of malnutritionb (% [95% CI]) . | Heterogeneity (I2, %) . | Prevalence of malnutritionb with sensitivity analysis (% [95% CI]) . | Heterogeneity with sensitivity analysis (I2, %) . | Sensitivity analysis: reason for removed studies . |
|---|---|---|---|---|---|---|---|---|
| Community | 63 | 50,905 | 28/35/0 | 4.7 [3.6–6.1] | 97.1 | – | – | – |
| Asia | 27 | 16,476 | 13/14/0 | 5.7 [3.3–8.6] | 98.0 | – | – | – |
| Europe | 27 | 31,001 | 11/16/0 | 2.8 [1.7–4.2] | 94.9 | – | – | – |
| North America | 4 | 1,112 | 2/2/0 | 11.5 [3.5–22.7] | 93.2 | 6.1 [3.5–9.2] | 0.0 | Neutral/negative quality |
| South America | 3 | 1,908 | 2/1/0 | 2.1 [1.4–3.0] | 25.9 | – | – | – |
| Australia (not pooled)c | 1 | 38 | 0/1/0 | 5.3 | – | – | – | – |
| Africa (not pooled)c | 1 | 370 | 0/1/0 | 28.4 | – | – | – | – |
| Homecare | 19 | 3,283 | 7/12/0 | 14.6 [9.9–20.0] | 93.9 | – | – | – |
| Asia | 2 | 462 | 1/1/0 | 14.6 [2.1–33.7] | 95.2 | – | – | – |
| Australia | 4 | 598 | 2/2/0 | 26.4 [1.2–63.1] | 98.4 | 6.3 [3.5–9.9] | 53.5 | Neutral/negative quality |
| Europe | 12 | 2,025 | 3/9/0 | 11.2 [7.4–15.5] | 86.9 | – | – | – |
| North America (not pooled)c | 1 | 198 | 1/0/0 | 12.1 | – | – | – | – |
| Hospital outpatient | 4 | 1,901 | 2/2/0 | 5.1 [0.1–14.6] | 97.3 | – | – | – |
| Asia | 2 | 1,304 | 1/1/0 | 10.2 [0.0–28.3] | 98.2 | – | – | – |
| Africa (not pooled)c | 1 | 500 | 1/0/0 | 7.8 | – | – | – | – |
| South America (not pooled)c | 1 | 97 | 0/1/0 | 0.0 | – | – | – | – |
| Nationally representative | 2 | 5,745 | 1/1/0 | 3.2 [2.4–3.7] | 53.9 | – | – | – |
| Asia (not pooled)c | 1 | 2,674 | 0/1/0 | 2.7 | – | – | – | – |
| Europe (not pooled)c | 1 | 3,071 | 1/0/0 | 3.3 | – | – | – | – |
| Post-hospital discharge | 2 | 305 | 1/1/0 | 5.1 [2.9–7.8] | 0.0 N/A | – | – | – |
| Australia (not pooled)c | 1 | 223 | 1/0/0 | 4.9 | N/A | |||
| Germany (not pooled)c | 1 | 82 | 0/1/0 | 4.9 | ||||
| Primary healthcare centre | 19 | 6,639 | 9/10/0 | 7.3 [2.4–14.2] | 98.6 | – | – | – |
| Asia | 4 | 3,151 | 2/2/0 | 7.7 [5.4–10.4] | 63.8 | – | – | – |
| Europe | 9 | 2,867 | 4/5/0 | 5.7 [0.0–17.4] | 99.1 | – | – | – |
| North America | 6 | 621 | 3/3/0 | 9.5 [0.0–26.9] | 95.8 | – | – | – |
| Other | 5 | 924 | 0/4/0d | 3.3 [1.9–5.0] | 23.8 | – | – | – |
| Asia | 2 | 746 | 0/1/0d | 3.6 [2.3–5.0] | 0.0 | – | – | – |
| Australia (not pooled)c | 1 | 12 | 0/1/0 | 16.7 | – | – | – | – |
| Europe (not pooled)c | 1 | 97 | 0/1/0 | 1.0 | – | – | – | – |
| North America (not pooled)c | 1 | 69 | 0/1/0 | 2.9 | – | – | – | – |
| Community setting . | Number of studies . | Sample size . | Qualitya . | Prevalence of malnutritionb (% [95% CI]) . | Heterogeneity (I2, %) . | Prevalence of malnutritionb with sensitivity analysis (% [95% CI]) . | Heterogeneity with sensitivity analysis (I2, %) . | Sensitivity analysis: reason for removed studies . |
|---|---|---|---|---|---|---|---|---|
| Community | 63 | 50,905 | 28/35/0 | 4.7 [3.6–6.1] | 97.1 | – | – | – |
| Asia | 27 | 16,476 | 13/14/0 | 5.7 [3.3–8.6] | 98.0 | – | – | – |
| Europe | 27 | 31,001 | 11/16/0 | 2.8 [1.7–4.2] | 94.9 | – | – | – |
| North America | 4 | 1,112 | 2/2/0 | 11.5 [3.5–22.7] | 93.2 | 6.1 [3.5–9.2] | 0.0 | Neutral/negative quality |
| South America | 3 | 1,908 | 2/1/0 | 2.1 [1.4–3.0] | 25.9 | – | – | – |
| Australia (not pooled)c | 1 | 38 | 0/1/0 | 5.3 | – | – | – | – |
| Africa (not pooled)c | 1 | 370 | 0/1/0 | 28.4 | – | – | – | – |
| Homecare | 19 | 3,283 | 7/12/0 | 14.6 [9.9–20.0] | 93.9 | – | – | – |
| Asia | 2 | 462 | 1/1/0 | 14.6 [2.1–33.7] | 95.2 | – | – | – |
| Australia | 4 | 598 | 2/2/0 | 26.4 [1.2–63.1] | 98.4 | 6.3 [3.5–9.9] | 53.5 | Neutral/negative quality |
| Europe | 12 | 2,025 | 3/9/0 | 11.2 [7.4–15.5] | 86.9 | – | – | – |
| North America (not pooled)c | 1 | 198 | 1/0/0 | 12.1 | – | – | – | – |
| Hospital outpatient | 4 | 1,901 | 2/2/0 | 5.1 [0.1–14.6] | 97.3 | – | – | – |
| Asia | 2 | 1,304 | 1/1/0 | 10.2 [0.0–28.3] | 98.2 | – | – | – |
| Africa (not pooled)c | 1 | 500 | 1/0/0 | 7.8 | – | – | – | – |
| South America (not pooled)c | 1 | 97 | 0/1/0 | 0.0 | – | – | – | – |
| Nationally representative | 2 | 5,745 | 1/1/0 | 3.2 [2.4–3.7] | 53.9 | – | – | – |
| Asia (not pooled)c | 1 | 2,674 | 0/1/0 | 2.7 | – | – | – | – |
| Europe (not pooled)c | 1 | 3,071 | 1/0/0 | 3.3 | – | – | – | – |
| Post-hospital discharge | 2 | 305 | 1/1/0 | 5.1 [2.9–7.8] | 0.0 N/A | – | – | – |
| Australia (not pooled)c | 1 | 223 | 1/0/0 | 4.9 | N/A | |||
| Germany (not pooled)c | 1 | 82 | 0/1/0 | 4.9 | ||||
| Primary healthcare centre | 19 | 6,639 | 9/10/0 | 7.3 [2.4–14.2] | 98.6 | – | – | – |
| Asia | 4 | 3,151 | 2/2/0 | 7.7 [5.4–10.4] | 63.8 | – | – | – |
| Europe | 9 | 2,867 | 4/5/0 | 5.7 [0.0–17.4] | 99.1 | – | – | – |
| North America | 6 | 621 | 3/3/0 | 9.5 [0.0–26.9] | 95.8 | – | – | – |
| Other | 5 | 924 | 0/4/0d | 3.3 [1.9–5.0] | 23.8 | – | – | – |
| Asia | 2 | 746 | 0/1/0d | 3.6 [2.3–5.0] | 0.0 | – | – | – |
| Australia (not pooled)c | 1 | 12 | 0/1/0 | 16.7 | – | – | – | – |
| Europe (not pooled)c | 1 | 97 | 0/1/0 | 1.0 | – | – | – | – |
| North America (not pooled)c | 1 | 69 | 0/1/0 | 2.9 | – | – | – | – |
aAcademy of Nutrition and Dietetics Quality Criteria Checklist rating (number of positive/neutral/negative).
bDetermined by MNA score < 17 or Patient-Generated Subjective Global Assessment or Subjective Global Assessment rating of B and C.
cData not pooled as there were no other samples in the same continent.
dChan et al. [22], which was conducted in an undescribed community setting in China, could not be sufficiently translated to allow for assessment of study quality.
Heterogeneity was substantial in all sampling frames excepting the nationally representative pooled prevalence. Removal of negative and/or neutral quality studies improved heterogeneity for the North American general community sampling frame and the Australian homecare sampling frame only.
There were five meta-regression models applied to examine the influence of covariates on sampling frames with high heterogeneity which were unresolved by sensitivity analysis. No covariates were found to be significant predictors of the malnutrition proportion for the general community sampling frame for all countries (n = 70 studies), the general community sampling frame in Asia (n = 27 studies), the general sampling frame in Europe (n = 27 studies), the homecare sampling frame in Europe (n = 12 studies), nor the primary healthcare sampling frame for all countries (n = 19 studies). In the homecare sampling frame for all countries, the type of assessment tool ([Subjective Global Assessment or Patient-Generated Subjective Global Assessment] versus the MNA) and country were included as covariates in the model. Assessment tool was the only significant covariate, indicating the MNA predicted a 51% lower malnutrition prevalence than Patient-Generated Subjective Global Assessment or the Subjective Global Assessment (coefficient: −0.51 [95% CI: −0.69 to −0.32]; P < 0.001; Adj. R2: 76.47%). However, there remained 89% residual variation due to heterogeneity (I2 residual: 89.35%).
The influence of rurality on the prevalence of protein-energy malnutrition in the international community setting
There were 17 studies (n = 5,822 total participants) which reported the prevalence of malnutrition in rural community-dwelling older adults, and 69 studies (n = 21,834 total participants) which reported malnutrition prevalence in urban communities. The pooled prevalence in rural communities (9.9% [95% CI: 4.5–16.8%], I2 = 98.2%) was nearly double the prevalence in urban communities (5.7% [95% CI: 4.2–7.3%], I2 = 95.9%). Sensitivity analysis based on study quality and sampling frame did not improve heterogeneity. Meta-regression did not identify any covariate which significantly predicted the pooled prevalence of malnutrition in rural nor urban communities.
The influence of gender on the risk of protein-energy malnutrition in the international community setting
Overall, 27 studies (n = 38,703 participants) were included which reported malnutrition rates for each sex. Globally, women were 45% more likely to be malnourished than men (OR 1.45 [95% CI: 1.27–1.66], P < 0.00001, I2 = 24%) (Figure 2).
![Protein-energy malnutrition prevalence was higher among females than males (OR 1.45 [95% CI: 1.27–1.66]; P < 0.00001; n = 24 studies; n = 38,703 participants; I2 = 24%).](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/ageing/48/1/10.1093_ageing_afy144/1/m_afy144f02.jpeg?Expires=1750223533&Signature=FEtOGY0urTqVEv3XllTZXpCT9NMXO3kehr~49VvbydvZPjoLhSglutuqIGW-MRNH6ZOpNTDErkBPLIbyyxmGzCNjAe6iYpoy2PxVJJcV2BkC3KCPnoBChJckn6nWB6Jf0xxMl7nl5-jwDZtYbHD5OdHqQw8xHChFR~fwhW7aQ-9V8GXm1uUWVxC3rYluvVExrYlW82UknILimEjiHZkrEAB~fKC1tDIK~kN2egpj-ZJQU4TVw5Fo7WGJtHKqjZI-tcJEcgiXz1eKTCFI6tTuL3k-H2ZMtCZmiAd~aukcFRNz5nMuvV-qYGHT5bov7~tBnVXT265v~ZIJF4chBbnG9w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Protein-energy malnutrition prevalence was higher among females than males (OR 1.45 [95% CI: 1.27–1.66]; P < 0.00001; n = 24 studies; n = 38,703 participants; I2 = 24%).
Discussion
This systematic review, meta-analysis and meta-regression is the most comprehensive assessment of the prevalence of malnutrition in home-dwelling older adults worldwide, and is also the first to pool the international prevalence of malnutrition examining geographical region, rurality, sampling frame and sex. However, it should be acknowledged that while there were a large number of diverse studies which contributed to this review, that there are populations which are under-represented, especially in Africa, South America and non-Australian Oceania. Within Asia and Europe, which had a large number of studies, there are still regions and countries which are not well represented, such as South-East Asia and Eastern Europe. Despite being limited in terms of international representation, the results of this review provide the best available strategic insight for global and national public health priorities, such as addressing the higher prevalence in homecare recipients and in women.
Although the prevalence, which ranged from <1 to 24.6%, is substantially lower than in other settings, where the prevalence may exceed 50% in rehabilitation and aged care [6, 8], the large majority of the 603 million older adults worldwide are community-dwelling [1]. It therefore represents a much larger number of individuals with malnutrition who require nutrition support.
Northern Europe had the lowest prevalence of malnutrition at <1% and South-East Asia had the highest at 25%. While this may initially suggest a negative influence of the social and economic disadvantage in developing countries, this trend was not consistent, where East Asia and South America both had a very low prevalence of malnutrition (<2%), and some well-developed countries in Europe had higher prevalence of up to 17%. This inconsistent finding may be due to limitations introduced by sampling bias, where the most at risk older adults in developing countries may not have been included in the sample. Alternatively, it may be due to a prevailing high risk of malnutrition for older adults living at home despite a more advanced economy and built environment [7].
Older adults receiving homecare services had the highest prevalence of malnutrition compared with other community sampling frames. This may reflect greater physical and/or health limitations in this population, such as increased frailty, compared to those not requiring such services. This highlights the greater need for nutrition to be addressed by homecare services as part of standard care. There is preliminary research suggesting homecare assistants may be effective in implementing both malnutrition screening and treatment interventions as part of a multidisciplinary malnutrition care team [4, 23].
The higher malnutrition prevalence in rural compared with urban communities aligns with previous research showing that older adults in rural, regional and remote areas have poorer health and less access to family support [2, 24, 25]. Of further concern, rural communities have less access to health services including both medical and allied health [2, 24]. Research evaluating and developing sustainable and feasible malnutrition interventions for rural communities is needed. Telehealth delivered via telephone conversations with dietitians has been found to be an effective method for treating malnutrition in older adults living at home, and is a feasible option for rural and remote areas [26].
Confirming previous research which has suggested females are at a greater risk of malnutrition [27, 28], this review found that globally, females have 45% greater odds of being malnourished compared to males. The meta-regression of Spanish studies found that as the percent of females in the sample increased, so did the malnutrition prevalence. Whilst it is acknowledged higher numbers of females than males were recruited in most studies; meta-analysis and meta-regression accounted for this difference. It is unclear if reasons for the greater risk in females is due to social and economic circumstance, greater age, more likely to be widowed, gender inequality and/or underlying differences in physiology. This highlights a need for future research investigating possible explanations so that more relevant interventions may be developed for female older adults.
Limitations
The number of included studies was substantially decreased due to many studies failing to report the prevalence of malnutrition despite using the Patient-Generated Subjective Global Assessment, MNA or Subjective Global Assessment; or due to combining community samples with participants from other settings such as aged care. Although this review included studies reporting the prevalence of malnutrition according to any of the three validated tools for this setting, only four studies were identified which used the Patient-Generated Subjective Global Assessment or Subjective Global Assessment. Therefore, this review is subject to the same limitation as Cereda et al. [9], in that the pooled prevalence of malnutrition may be underestimated due to the limitations of the MNA [8]. The meta-regression in the homecare setting further supported this, indicating that using the MNA predicted a 51% lower malnutrition prevalence than studies which used the Patient-Generated Subjective Global Assessment or the Subjective Global Assessment.
The quality of individual studies was examined by focussing on the risk of bias relevant to the prevalence statistic. Although none of the included studies were found to be of a negative quality, as 59% were neutral quality, there is a substantial risk of bias in many of the reported prevalence data, limiting confidence in the pooled results. Although data were included from both randomised and non-randomised studies, only baseline data of both intervention and control groups was used.
Most pooled prevalence statistics in this review had substantial heterogeneity which was not improved by sensitivity analysis, aligning with the finding by Cereda et al. [9]. Meta-regression using the covariates considered explained variation in only two of the nine models. Pooled results with substantial heterogeneity should be interpreted with some caution and the individual studies contributing to pooled prevalence data should also be considered (available in Appendix 2, available in Age and Ageing online) to help understand the available data. As a reflection of the highly complex physiological, social and temporal nature of malnutrition which varies from individual to individual [7], as well as bias introduced by study design, it is unlikely that any review examining the pooled prevalence of malnutrition will be able to account for all sources of heterogeneity. This also explains why meta-regression considering the extracted covariates did not explain sources of heterogeneity in most models, as medical, pharmaceutical and physical characteristics could not be analysed.
Conclusion
Malnutrition prevalence varies across geographical regions, but was not predicted by the social and economic development of countries. Home-dwelling older adults at greater risk of malnutrition may be those accessing homecare services and those living in rural communities. Females are at a much greater risk of malnutrition compared to males. Further research is required to determine the prevalence of malnutrition in specific areas, particularly in South America, Africa and non-Australian Oceania.
The prevalence of malnutrition ranged widely from 0.8 to 24.6% depending on region.
Homecare recipients have the highest prevalence of all sampling frames (14.6%).
Prevalence of malnutrition in rural communities (9.9%) is twice that in urban (5.7%).
Females have 45% higher odds of being malnourished than males (OR: 1.45, [95% CI: 1.27–1.66]).
Acknowledgements
The authors gratefully acknowledge the assistance of D. Honeyman, Librarian at Bond University, for contributing to the search strategy; and A/Prof Elaine Beller, Statistician at Bond University for her assistance in the implementation and interpretation of meta-regression.
Conflicts of interest
None.
Funding
None.
References
World Population Prospects: 2012 Revision. 2013: Department of Economic and Social Affairs, United Nations.
Policy Paper: 2010 to 2015 Government Policy: Older People. 2015, UK Government: Department for Work & Pensions and The Rt Hon Steve Webb.
Australian Coding Standards for ICD-10-AM.
Evidence analysis manual: steps in the Academy Evidence Analysis Process. In: Reserach and Strategic Business developmentm, Academy of Nutrition and Dietetics.




Comments