-
PDF
- Split View
-
Views
-
Cite
Cite
Maya Yamato, Tsuyoshi Shirai, Hiroko Sato, Tomonori Ishii, Hiroshi Fujii, First reported case of pulmonary arteritis in patients with relapsing polychondritis, Rheumatology, Volume 63, Issue 1, January 2024, Pages e9–e11, https://doi.org/10.1093/rheumatology/kead300
Close - Share Icon Share
Relapsing polychondritis manifests pulmonary arteritis detectable by MRI and FDG-PET, and infliximab is effective.
Dear Editor, Relapsing polychondritis (RP) primarily affects the auricular, laryngotracheal and nasal cartilages; however, it may occasionally involve the inner ears, eyes and joints. RP comprises a distinct subpopulation represented by the VEXAS syndrome [1]. Moreover, involvement of the cardiovascular system, including large vessel lesions, has also been reported. A recent systematic review estimated the prevalence of aortic involvement in RP to range from 4.4% to 18.6%, encompassing the aorta, aortic valve and coronary arteries. However, the involvement of the pulmonary artery has not been reported [2]. Herein, we present a case of RP with pulmonary arteritis that was treated successfully with prednisolone (PSL), MTX and infliximab.
The patient evaluated in the study was a 32-year-old Japanese woman with a history of fever exceeding 38°C and a sputum-producing cough persistent for 2 months before presentation. She was referred to our hospital after the initial PSL treatment for her acute subglottic laryngitis failed in another facility. The patient also complained of pain in her nose, and the physical examination revealed tenderness in the nasal root area. Several pustules and ulcerative lesions were observed at the injection site on the forearm (Fig. 1a), but no other abnormalities were identified. Laboratory findings included elevated levels of white cells (16 600 per µL) and CRP (7.42 mg/dl). The patient tested negative for autoantibodies, including antineutrophil and cytoplasmic antibodies. Human leucocyte antigen types were identified as A2, A24, B35 and B62. Fluorodeoxyglucose (FDG)-PET revealed increased FDG uptake by the nasal septal, alar, tracheal and costal cartilages and the right and left pulmonary arteries (Fig. 1b). The inflammatory findings in the pulmonary artery, difficult to detect using enhanced CT, were confirmed using T2-weighted MRI (Fig. 1c). The patient’s symptoms aligned with the Michet’s classification criteria for RP [3] as inflammatory lesions were observed in the nasal and laryngotracheal cartilages. Treatment with PSL (50 mg/day) and MTX (6 mg/week) was initiated. Infliximab was administered at 500 mg during the first and third weeks of admission. During the 4 weeks of hospitalization, the MTX dose was increased to 10 mg/week, while the PSL dose was reduced to 35 mg/day. Moreover, during the outpatient follow-up visits, the patient continued to receive infliximab and MTX at a dose of 12 mg/week, while the PSL dosage was tapered to 10 mg/day. CRP was monitored as a marker of systemic inflammation, and it responded favourably to the first dose of infliximab. A follow-up MRI of the pulmonary artery, 2 months after the discharge, revealed a resolution of inflammation (Fig. 1c, right). The patient has since been closely monitored with no evidence of recurrent inflammation or nasal root pain.
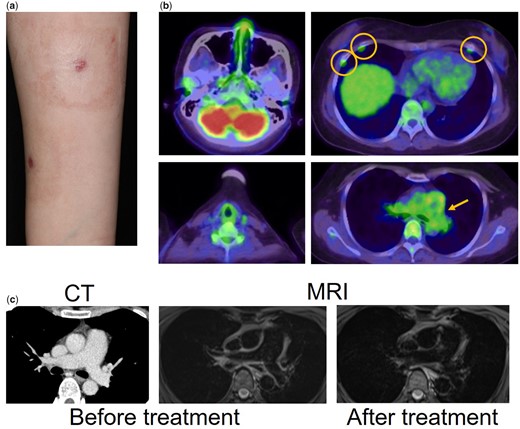
Clinical imaging of this patient. (a), Multiple pustular skin lesions at the injection site on her forearm. (b) Fluorodeoxyglucose (FDG)-PET scan. (c) The imaging of the pulmonary artery by CT, left and MRI, middle (T2WI). The imaging of the pulmonary artery using MRI obtained 2 months after discharge (right)
RP sometimes overlaps with the Behçet’s disease (BD), also known as the mouth and genital ulcers with inflamed cartilage (MAGIC) syndrome. The patient developed pustules known as pathergy at the injection site indicating neutrophilic inflammation. Pathergy is commonly observed in BD and MAGIC syndromes but very rarely in RP [4]. Although the case did not meet the international classification criteria owing to the absence of ocular symptoms and oral aphthous or genital ulcers, we suspected the involvement of neutrophilic vasculitis in the development of pulmonary arteritis. Similarly, Takayasu arteritis is also known for neutrophilic vasculitis involving pulmonary arteritis [5]; however, the current case did not meet the criteria. We previously reported a case of large-vessel vasculitis (LVV) with concomitant features related to RP, Takayasu arteritis, and BD [6], indicating the possibility of a mixed-state presentation, including the three diseases.
Moreover, as no tissue sample was obtained from the patient, pathological images were not available. However, RP can be diagnosed based only on clinical criteria, with or without histopathological evidence. Furthermore, FDG-PET demonstrates high sensitivity and specificity in LVV imaging [7], which in this case enabled the detection of pulmonary artery inflammation. The case was successfully treated with infliximab; the first dose alone lowered the CRP levels, and the administration of three doses substantially ameliorated the inflammation in the pulmonary artery. For RP associated with LVV, high-dose corticosteroids and biological agents, including infliximab, tocilizumab, adalimumab and rituximab have demonstrated effectiveness [8].
To the best of our knowledge, this is the first documented example of pulmonary arteritis in a patient with RP, involving neutrophilic vasculitis. The lesion was difficult to detect using conventional CT imaging, and FDG-PET was required. Based on our experience, a combination of PSL, MTX and anti-tumour necrosis factor α therapy is recommended for the remission of pulmonary arteritis.
Informed consent has been received for the publication of this case report.
Data availability
Data available on request to the corresponding author.
Funding
This work was partly supported by JSPS KAKENHI Grant Number 21K08469T and the JCR Grant for Promoting Research for D2T RA.
Disclosure statement: The authors have declared no conflicts of interest.




Comments