-
PDF
- Split View
-
Views
-
Cite
Cite
Gummadi Anjani, Srinivasavardan Govindarajan, Murugan Sudhakar, Himanshi Chaudhary, Amit Rawat, Ankur Kumar Jindal, Catch the thief by its marks: inverse Gottron papules, interstitial lung disease, anti MDA-5 antibody positivity in juvenile dermatomyositis, Rheumatology, Volume 60, Issue 2, February 2021, Pages e56–e58, https://doi.org/10.1093/rheumatology/keaa433
Close - Share Icon Share
Inverse Gottron papules may be associated with ILD and anti MDA-5 antibody positivity in children with JDM.
DearEditor, JDM is an idiopathic inflammatory myopathy that often presents with cutaneous manifestations and muscle weakness. Pulmonary involvement in the form of interstitial lung disease (ILD) is occasionally seen and may worsen the disease prognosis. Inverse Gottron papules have been reported to be associated with ILD and anti-melanoma differentiation associated gene-5 (MDA-5) antibody positivity in adults with dermatomyositis. However, literature on this aspect is scarce in children. Herein, we report one such case.
A 16-year-old girl presented with gradually worsening proximal muscle weakness for the past 3 years. She also had a history of photosensitive rash on face and neck, restriction of movements in multiple joints (wrist, elbow, knee and small joints of hands) and painful ulcers over elbow and ankle region that were discharging whitish material. She also had intermittent chest pain that used to be aggravated by deep inspiration and also developed easy fatiguability. On examination, she had pallor, malar rash involving nasolabial folds, heliotrope rash, Gottron papules and inverse Gottron papules (Fig. 1A), healed calcinosis cutis over left elbow and left ankle (Fig. 1B), proximal muscle weakness with neck flexors involvement, poor gag reflex and loud P2 sound on cardiovascular system examination. Laboratory investigations (Supplementary Table S1, available at Rheumatlogy online) showed elevated muscle enzymes, positive ANA with 4+ with homogeneous pattern (indiret immunofluorescence with 1:60 dilution) and normal serum complements. Contrast-enhanced MRI of biateral thigh muscles showed areas of T2 hyperintensities with post contrast heterogeneous enhancement. X-ray of elbow was suggestive of calcification in subcutaneous tissue (Fig. 1C). High-resolution CT chest revealed reticulation and septal thickening in bilateral lower lobes suggestive of ILD (Fig. 1D) and pulmonary function test showed severe restrictive lung disease (forced vital capacity 50% of predicted). 2D echocardiography revealed mild pulmonary arterial hypertension. A panel of myositis-specific antibodies were tested that showed positivity for MDA-5 antibody. A clincal diagnosis of JDM with ILDs with pulmonary arterial hypertension was considered. She was treated with intravenous methylprednisolone pulses (30 mg/kg/day for 5 days) followed by oral prednisolone (initially 2 mg/kg/day and then tapered) and intravenous cyclophosphamide pulse therapy (500 mg/m2/month for 6 months). She showed gradual recovery of muscle weakness and chest symptoms and forced vital capacity improved to 71%. At 6 months of follow-up, she was initiated on subcutaneous methotrexate (15 mg/m2/week) and mycophenolate mofetil (600 mg/m2/day).
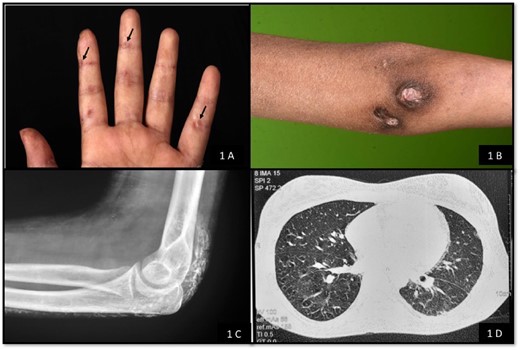
Fig. 1 Clinical and radiological features in the index case with JDM
(A) Inverse Gottron papules on palmar surface; (B) healed calcinosis cutis over left elbow; (C): X-ray of elbow was suggestive of calcification in subcutaneous tissue; (D) high-resolution computed tomography chest ahowing reticulation and septal thickening in bilateral lower lobes suggestive of interstitial lung disease.
Inverse Gottron papules (hyperkeratotic papules that are often noted over palmar aspect of metacarpophalangeal and interphalangeal joints) have been occasionally reported in children with JDM. Quinter et al. reported three patients and Jindal et al. reported four patients [1, 2] with JDM who had inverse Gottron papules. ILD has been reported less frequently in children with JDM as compared with adults. In the year 2003, Kobayashi et al. [3] reported ILD in five patients with JDM.
Anti MDA-5 antibody is a myositis-specific antibody and is associated with a phenotype of dermatomyositis with cutaneous ulcers, palmar papules, arthritis, higher risk of ILD and less severe muscle involvement [4]. The role of anti-MDA-5 as diagnostic and predictive marker of ILD in JDM was highlighted in 2011 by Kobayashi et al. [5] when they reported anti-MDA-5 positivity in five of six children with ILD. In 2014, anti MDA-5 was identified in 21 (7.4%) cases with JDM, of which four had ILD [6]. A correlation between high serum MDA-5 antibodies (>200 units) and rapidly progressive ILD in JDM has also been reported [7]. However, none of these studies on JDM with ILD and MDA-5 antibodies reported inverse Gottron papules.
The triad of inverse Gottron papules, ILD and anti MDA-5 antibody positivity has been reported as anecdotal reports in adults with dermatomyositis [8–10]. However, to the best of our knowledge, this entity has not been described in young children or adolescents with JDM. In two case series on inverse Gottron papules in JDM by Quinter et al. and Jindal et al. [1, 2] ILD was reported in 33% and 75% patients, respectively. However, MDA-5 antibodies were not assessed in either of these two studies. To conclude, ILD is a rare manifestation of JDM and may be associated with presence of inverse Gottron papules anti MDA-5 antibody positivity.
Acknowledgements
G.A., S.G.: patient management, concept and draft of manuscript, critical review of literature; M.S., H.C.: patient management, critical review of literature; A.R.: laboratory support; A.J.: patient management, concept of the manuscript, critical review of manuscript for important intellectual content and final approval of the version to be published
All co-authors take full responsibility for the integrity of the study and the final manuscript.
Funding: No specific funding was received from any funding bodies in the public, commercial or not-for-profit sectors to carry out the work described in this manuscript.
Disclosure statement: The authors have declared no conflicts of interest.
Supplementary data
Supplementary data are available at Rheumatology online.




Comments