-
PDF
- Split View
-
Views
-
Cite
Cite
Hasan Satış, Emetullah Cindil, Nuh Ataş, Reyhan Bilici Salman, Abdurrahman Tufan, Successful treatment of coronary artery aneurysm with infliximab in a Behçet’s disease patient, Rheumatology, Volume 60, Issue 1, January 2021, Pages e10–e11, https://doi.org/10.1093/rheumatology/keaa365
Close - Share Icon Share
Infliximab could be an effective treatment option for coronary artery aneurysms observed in Behçet’s disease.
DEAR EDITOR, Behçet’s disease (BD) is a multisystemic vasculitis characterized by recurrent oral and genital ulcers and various systemic manifestations. Coronary arteries are rarely involved but usually associated with fatal outcomes. Due to its rarity and high mortality, optimal management of coronary involvement is largely unknown. Herein, we described a BD patient with huge coronary artery aneurysm which remarkably regressed with infliximab treatment, which has not been reported previously.
A 27-year-old male patient admitted to the emergency department with complaints of palpitation and chest pain radiating to his left neck and shoulder. There was marked ST elevation in V1–V4 derivations of electrocardiogram and >10-fold increase in cardiac-specific troponin levels. He underwent immediate coronary angiography with a diagnosis of acute myocardial infarction, which revealed huge aneurysm in the left main coronary artery and total occlusion of the left anterior descending artery. He gave a history of severe vision loss in his left eye as a result of uveitis, which occurred six months before the admission. In detailed questioning, he described oral aphthous ulcers as frequent as three times in a month and occasional genital ulcers many years before with evidence of two genital scars upon physical examination. Considering his history, he was diagnosed as BD according to International BD Criteria [1]. The patient had no traditional cardiovascular risk factors; thus, the aneurysm was attributed to BD.
Cardiologists recommended emergent coronary bypass grafting (CABG) due to severe ventricular hypokinesia with an ejection fraction of 40% on echocardiography. However, CABG was considered highly risky without antecedent immunosuppression and he was started on 20 mg day prednisone along with infliximab 6 mg/kg, as we were concerned about worsening of myocardial infarction, myocardial wound healing and heart failure with high dose corticosteroids. At the second week of treatment, he was re-evaluated with CT angiography of coronary arteries disclosing left main aneurism of 22 × 11 mm in size and volume of 1.14 cm3. Prednisone was continued 20 mg/day for one month then tapered 5 mg/week until 5 mg/day with maintaining this dose then after. Infliximab was given at weeks 0–2–6 and then every 8 weeks. His repeat CT angiography at four months showed remarkable reduction in aneurysm size, which was 19 × 8 mm in size and a volume of 0.55 cm3 (Fig. 1). Although a remarkable shrinkage of the aneurysm, ventricular function did not improve and he underwent elective CABG without any complication. His treatment was continued with prednisone 5 mg/day and infliximab 6 mg/kg every 8 weeks. In his last visit, three months after the CABG, he was doing well without any complaint but ventricular ejection fraction remained as 40% on echocardiogram in his last visit. Due to frequent radiation exposure, a repeat CT angiogram was planned for one year later.
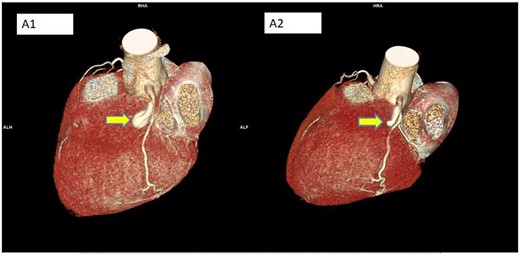
Three-dimensional images of the aneurysm at the start and after 4 months of treatment
(A1) Start; (A2) after 4 months of treatment with infliximab showing regression of aneurysm. Yellow arrows show the aneurysm.
Treatment of BD-related coronary artery aneuysm (CAA) is largely based on high dose corticosteroids and immuno-suppressive agents like cyclophosphamide, an approach inferred from previous rare CAA case reports and treatment of other vascular manifestations [2, 3]. Increased levels of TNF-α has been demonstrated in active BD [4], thus it is not surprising that infliximab and to a lesser extent other anti-TNFs were found effective in various manifestations of BD such as pulmonary artery aneurysm, superior and inferior vena cava syndromes [2, 3]. In clinical practice, coronary artery aneurysm is rarely encountered in vasculitides and usually observed in Kawasaki disease [5]. TNF-α levels were also increased in Kawasaki disease, being highest in those who develop coronary artery aneurysm [6]. Successful treatment of coronary aneurysms has been reported with use of anti-TNF agents in Kawasaki patients [7].
In BD, the risk of recurrence and complications of interventional procedures are very high without antecedent immuno-suppression due to pathergy phenomenon [3]. As yet, there is no consensus for the management of CAA-complicated BD – one of the effective treatments should be started immediately. Infliximab provided shrinkage and prevented dissection of aneurysm in our case; therefore, it might be an effective treatment option for the treatment of coronary artery involvement in patients with BD. However, our observations need to be confirmed in systematic studies to make routine recommendations.
Funding: No specific funding was received from any funding bodies in the public, commercial or not-for profit sectors to carry out the work described in this manuscript.
Disclosure statement: the authors have declared no conflicts of interest.




Comments