-
PDF
- Split View
-
Views
-
Cite
Cite
Casey Rimland, Kaitlin Quinn, Joel Rosenblum, Mollie Schwartz, Katherine Gribbons, Elaine Novakovich, Antoine Sreih, Peter Merkel, Mark Ahlman, Peter Grayson, 266. OUTCOME MEASURES IN LARGE-VESSEL VASCULITIS: RELATIONSHIPS BETWEEN PATIENT, PHYSICIAN, IMAGING, AND LABORATORY-BASED DOMAINS, Rheumatology, Volume 58, Issue Supplement_2, March 2019, kez062.040, https://doi.org/10.1093/rheumatology/kez062.040
Close - Share Icon Share
Background: Various outcome measure domains have been proposed to evaluate treatment response in patients with large-vessel vasculitis (LVV), including patient-reported outcomes (PROs), physician assessment of disease activity, vascular imaging, and laboratory assessment. Data examining the complex relationships between outcome domains in LVV is limited.
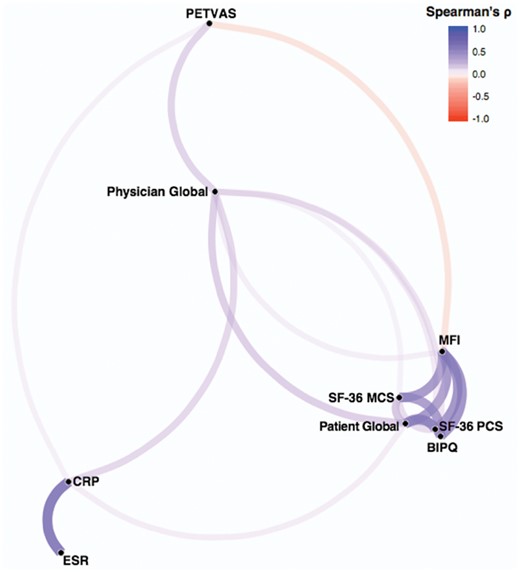
Methods: Patients with giant cell arteritis (GCA) or Takayasu’s arteritis (TAK) were recruited into a prospective, observational cohort. Assessments within the following domains were independently recorded: patient-reported outcomes [multi-dimensional fatigue inventory (MFI); patient global assessment (PtGlobal); 36-item short form health survey (SF-36); brief-illness perception questionnaire (BIPQ)], physician global assessment (PhGlobal), acute-phase reactants (CRP, ESR), and imaging assessment (PETVAS, a qualitative score of vascular FDG-PET activity). To visualize the relationship between domains, Spearman’s correlation network analysis was performed. This analysis enables visualization of the strength and directionality of correlations and clusters variables most correlated to one another. Change over time in outcome measures was compared using the Wilcoxon signed rank test in patients with a change in clinical status from active disease (PhGlobal >0) to remission (PhGlobal=0) or from remission to active disease.
Results: Analyses were performed on 112 patients (GCA=56, TAK=56), over 296 visits, with an average follow-up interval of 8 months (range 2-20). Network analysis revealed that the outcome measures clustered independently and by specific domain (Figure). The strongest correlations were within domains: all four of the PROs strongly correlated with each other (ρ = 0.35-0.60, p < 0.0001); and ESR and CRP were strongly correlated (ρ = 0.71, p < 0.0001). Interestingly, PROs were not positively correlated with PETVAS and only PtGlobal weakly correlated with CRP (ρ = 0.16, p < 0.01). PhGlobal was centrally linked to all other domains, but correlations were modest (ρ = 0.12 – 0.31, p < 0.05). Patients whose disease activity changed from active to remission (n = 19) had significantly decreased ESR, CRP, PETVAS, and PtGlobal at remission visit, without change in MFI, SF-36, or the BIPQ. Patients whose disease activity changed from remission to active (n = 12) only had significantly increased CRP and PtGlobal at active visit.
Conclusion: These results demonstrate that outcome measures in LVV consist of independent, yet complementary domains, supporting the need for the development of either multidimensional outcome measures or a standard set of measures covering all domains.
Disclosures: This research was supported by the Division of Intramural Research of the National Institute of Arthritis and Musculoskeletal and Skin Diseases.




Comments