-
PDF
- Split View
-
Views
-
Cite
Cite
S-Z Liu, X Zhou, Y-P Wang, Y Liu, Osteosclerosis in Castleman’s disease, QJM: An International Journal of Medicine, Volume 115, Issue 3, March 2022, Pages 171–172, https://doi.org/10.1093/qjmed/hcac013
Close - Share Icon Share
A 32-year-old man presented to the orthopedic clinic with a 1-year history of systemic multiple sclerosis, especially in the spine. A year previously, the patient was also diagnosed with unicentric mixed type Castleman’s disease (CD) and underwent complete excision of a left axillary mass. Following this, the patient was found to have adenocarcinoma of the left lung and underwent thoracoscopic left lower lobectomy with systematic lymph node dissection. The patient then complained of waist soreness but denied experiencing any other constitutional symptoms or any history of trauma during the past years. Two months previously, his mother was also diagnosed with unicentric mixed type CD. Physical examination and laboratory investigations were performed which did not reveal any abnormality, except that the neuron-specific enolase was mildly elevated at 19.1 U/ml (normal range ≤16.3 U/ml). Computed tomography of the spine showed significant sclerosis of the partial T2, T3, T7, L1 vertebral body and the appendix (Figure 1A and B). Magnetic resonance imaging of the spine demonstrated multiple round-like abnormal signals in the thoracic, lumbar and sacral vertebral bodies and appendages. Subsequent positron emission tomography/computed tomography scan identified multiple cystic lesions in the vertebral bodies with no increased uptake of 18F-FDG, indicating bone changes in CD (Figure 1C). After careful evaluation and consideration to exclude spinal metastases, percutaneous vertebroplasty was performed, with the histopathological examination later confirmed the diagnosis of diffuse osteosclerosis in CD. Therefore, the patient was referred to the department of hematology and thoracic surgery for further management.
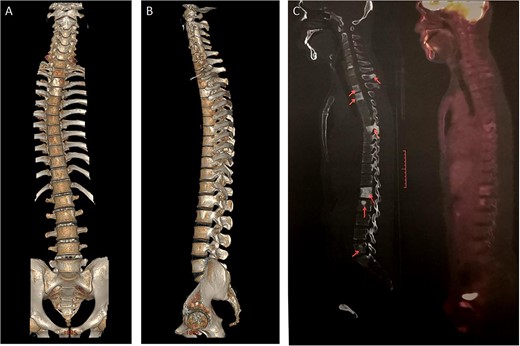
Osteosclerosis in Castleman's disease (A,B) Three dimensional reconstruction of whole spine CT showed multiple abnormal high-density shadows in spine, thorax and pelvis. (C) 18F-FDG P ET / CT showed multiple osteogenic changes in multiple vertebral bodies and accessories of the spine, and there was no increase in metabolism.
CD is a rare, undetermined chronic lymphoproliferative disorder with an incidence rate of 1/50 000.1 CD is highly heterogeneous and can be categorized as unicentric CD (UCD) and multicentric CD based on the different areas of lymph node involvement. One of the characteristics of the present case is that CD was complicated by lung cancer. In addition, the patient’s mother was diagnosed with UCD and the father with lung cancer. The incidence of CD in this patient thus indicated a certain family tendency, which is clinically rare and also rarely reported in the literature.2 Clinicians should pay complete attention to the clinical phenomenon of osteosclerosis in patients with CD, especially when the patients show complications with malignant tumors, and their condition should be fully differentiated from bone metastases.3 Therefore, under circumstances similar to those in the present case, tissue biopsy of the affected bone for pathological diagnosis is imperative.
Conflict of interest. None declared.



