-
PDF
- Split View
-
Views
-
Cite
Cite
R E Powers, R M Estrada-Y-Martin, S V Cherian, Urinothorax: an under-reported cause of pleural effusions, QJM: An International Journal of Medicine, Volume 115, Issue 12, December 2022, Pages 862–863, https://doi.org/10.1093/qjmed/hcac194
Close - Share Icon Share
Urinothorax is a rare case of pleural effusion which presents similarly to other types of pleural effusions. The appropriate treatment, however, involves identification and resolution of the underlying obstructive uropathy. We present a case of urinothorax to highlight the importance of early recognition to prevent delay in definitive treatment.
Case description
A 37-year-old female with a history of recurrent nephrolithiasis presented for elective right percutaneous nephrolithotripsy and nephrostomy tract dilation. Post-operative chest X-ray was normal. On post-operative day 1, the percutaneous nephrostomy tube was clamped, then removed in the afternoon. Discharge was delayed due to continuing pain. The following morning, she complained of shortness of breath, chest pain, nausea and vomiting.
She was afebrile, hypertensive at 173/98 mmHg, tachycardic at 105 bpm, breathing 20 breaths per minute and saturating 97% on room air. Physical exam was notable for decreased breath sounds on the right chest area without wheezing and tachycardia without murmurs, rubs or gallops. Abdomen was soft, non-tender and symmetric. Repeat chest X-ray showed a new moderate right-sided pleural effusion (Figure 1a), more obvious on chest computed tomography angiogram (Figure 1b).
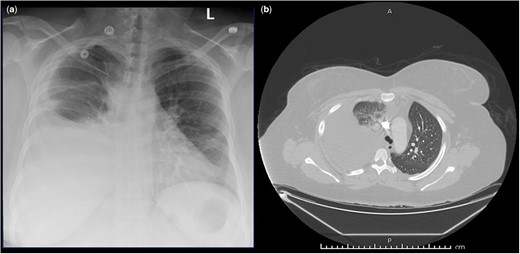
(a) Chest X-ray showing a new moderate right-sided pleural effusion with adjacent opacities likely representing subsegmental atelectasis. (b) Computed tomography angiogram showing a large right-sided pleural effusion with adjacent compressive atelectasis of the right upper, middle and lower lobes; mild subsegmental atelectasis in the left lung base.
Chest tube placement with pleural fluid analysis revealed Lactate Dehydrogenase (LDH) 115 U/l (<2/3 upper limit of normal) and a pleural fluid to serum creatinine ratio of 6.3. Serum creatinine was 0.67 mg/dl. This transudative effusion with an elevated creatinine ratio was consistent with urinothorax.
Foley catheter with stent was placed. Chest X-ray after chest tube placement showed a significant decrease in the effusion. The patient clinically improved, and on post-operative day 6, the chest tube was removed, with repeat chest X-ray showing resolution of the effusion. The patient was discharged home with the indwelling urine catheter.
Discussion
The incidence of urinothorax is likely significantly underreported. A 2016 systematic review yielded only 78 included studies from the 62-year period covered.1,2 Patients typically present with dyspnea, chest pain, abdominal pain and a decrease in urine output. A pleural effusion, usually ipsilateral to the side of uropathy, may be present on chest X-ray with or without atelectasis.3 Treatment of urinothorax involves drainage of the associated pleural effusion and/or treatment of the underlying uropathy. Outcomes for patients that receive both uropathy treatment and chest drainage appear to be superior to treatment with thoracic drainage alone.1 In our patient, both drainage of the pleural fluid and treatment of the underlying urinary obstruction were performed with resolution of the urinothorax.
Conclusion
Urinothorax is a rare transudative pleural effusion arising secondary to obstructive uropathy and high index of suspicion is important to provide timely treatment. Early identification requires measuring pleural fluid creatinine and abdominal imaging to locate the obstruction. The presence of obstructive uropathy or urologic procedure ipsilateral to the pleural effusion should raise the possibility of urinothorax. The treatment in symptomatic patients is relief of the obstruction with drainage of the effusion.
Author contribution
R.E.P.: involved in preparing the letter. S.V.C. and R.M.E.Y.M.: directly involved with the patient’s care and preparing the letter.
Presentation: This case will be presented as a poster presentation at the 2022 ACP Tri-Service Chapters Meeting, 7–10 September 2022.
Conflict of interest: None declared.



