-
PDF
- Split View
-
Views
-
Cite
Cite
Jennifer A Furze, Lisa Black, Amy W McDevitt, Kara L Kobal, Steven J Durning, Gail M Jensen, Clinical Reasoning: The Missing Core Competency in Physical Therapist Education and Practice, Physical Therapy, Volume 102, Issue 9, September 2022, pzac093, https://doi.org/10.1093/ptj/pzac093
Close - Share Icon Share
Clinical Reasoning (CR): Taking a Deeper Dive
CR is a defining characteristic essential to all health professionals. It is the holy grail, so to speak, yet confusion and miscommunication regarding key constructs and terminology exist.1,2 CR is a complex cycle of cognitive and metacognitive processes requiring the integration of knowledge, psychomotor skills, and reflection within the situational context of clinical practice.2,3 Effective CR in the health professions also embraces the patient and family perspective in the course of decision-making to provide optimal patient management.2–4 Physical therapy, like many other health professions, struggles with differing perceptions and descriptions of CR. Christensen and colleagues report great variability in how programs define, teach, and assess CR, thus contributing to the uncertainty surrounding CR and compounding the quandary of establishing best practice.4 This struggle creates challenges in “speaking the same language,” which in turn leads to confusion in how to best improve the teaching, learning, and assessment of CR in learners across the educational continuum.4–6
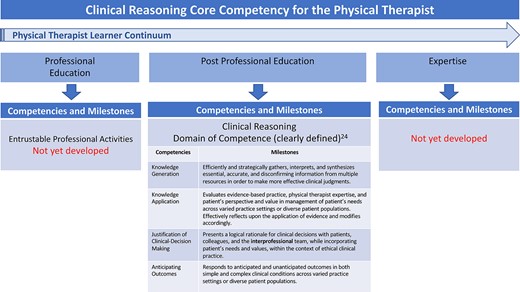
Components of competency-based education (CBE) for clinical reasoning (CR) spanning the educational continuum.24
We believe the profession should shift to a theory-informed teaching, learning, and assessment model to provide clarity and highlight CR as a foundation of learner development, beginning in professional physical therapist education and continuing through clinical and postprofessional education. A curricular paradigm that firmly establishes proficiency in CR as a required outcome with a focus on learner development and progression in meeting patient needs would be a step in the right direction. Competency-based education (CBE) is a sound educational structure consisting of competencies, learning objectives for the competencies, and assessment of learner performance that can drive educational change for the profession.7
Postprofessional residency education has clearly emphasized the importance of CR8,9 through the adoption of an explicit CR domain of competence (DOC) in the newly published residency assessment instrument implemented in Fall of 2022.10,11 Although educators may argue CR is identified, facilitated, and assessed in professional education, this occurs with less consistency, more variability, and little linkage to postprofessional education.4 This concentration on CR so late in the learner’s training results in a potential reduction of learners’ CR development and missed opportunities using a learner continuum view, and we argue that a fundamental and separate DOC beginning in professional education would facilitate the development of CR in all physical therapists, not just those pursuing residency.
As the profession makes an argument to move toward CBE as a transformative strategy that emphasizes the learner continuum, there is an opportunity to integrate explicit and theory-informed frameworks for more consistent development of CR.7,12 Since the publication of the CBE and Entrustable Professional Activities point of view in 2017,12 the Education Leadership Partnership created panels and workgroups to develop DOCs as an initial step forward in CBE.13 Although the specific DOCs have yet to be shared publicly, preliminary drafts neglect to include CR as a separate DOC but rather embed it across multiple DOCs where its importance becomes diluted. This resembles medicine’s approach where, again, CR is assumed to be part of several DOCs. Connor et al argue that CR in medicine should be recognized as a separate DOC because it is foundational for practice.14 Clinical reasoning is critical to physical therapist practice and a foundational component of expertise15 and, as such, should be identified as an individual DOC in the overall CBE framework.
The purpose of this Point of View is to demonstrate an urgent need for CR to be identified as a fundamental and separate DOC across physical therapist education and practice. The authors of this paper believe that a CR DOC would drive much needed progress toward educational innovation and contemporary physical therapist practice that emphasizes and prioritizes patient and learner outcomes that address patient needs.
CR Is Everywhere Yet Nowhere
Despite the abundance of CR literature in the health professions and the identification of the critical role CR plays in these respective professions including a core construct of expertise, achieving shared consensus on terminology and how we teach and assess CR remains a challenge.1,15 Although it may be partially interwoven or implied in other concepts, CR lacks an explicit placeholder in many health profession’s core competencies and entrustable professional activities. Medicine, physician assistant, pharmacy, and nursing have demonstrated ongoing work with development of competencies and entrustable professional activities.16 The physician assistant and physician professions have included use of the terms “clinical problem solving,” “clinical judgement,” and “critical thinking” within their DOCs, but we argue that this is not sufficiently inclusive.17 The authors’ focus is on CBE in the United States, yet internationally, CBE frameworks are being developed and adopted by many countries as a mechanism to describe expected entry-level physical therapist practice.18 However, a single competency framework in physical therapist education has not been acknowledged on an international level.
“Knowledge for practice” is a DOC seen across many of the health professions’ competency frameworks; however, dissecting clinical knowledge from the organization and thinking of knowledge is a slippery slope. CR is not a skill but is multi-faceted and evolving as it draws from both cognitive and noncognitive processes.14,19 A clinician’s reasoning ability cannot be separated from how well they build and organize their knowledge.20 If the professions value CR and consider CR essential to excellent clinical practice, then it must be defined as a separate and explicit DOC.
The Value of CR
The current variability in physical therapist education focused on CR, including differing curricular emphases and content focus and varying clinical education time frames, poses challenges for the profession.21 In addition to these inconsistencies, complexities of determining and evaluating learner outcomes using sound and credible measures exist across education and CR in particular.22 The most recent and comprehensive study of physical therapist education, The National Study of Excellence and Innovation in Physical Therapist Education, highlights the need for our profession to establish a longitudinal approach for standardizing learner outcomes across the educational continuum grounded in DOCs.23
Findings from The National Study of Excellence and Innovation in Physical Therapist Education call for a comprehensive and longitudinal approach to teaching and assessing CR given the importance of this construct to the profession.23 This recommendation was based on evidence that academic and clinical educators valued CR as foundational to practice; however, they were facilitating and assessing CR without a deep understanding of the theoretical learning concepts that underpin effective CR teaching and learning strategies.22
Connecting the Pieces: Faculty Development—A Missing Piece of the Puzzle
Evidence suggests that academic and clinical faculty inconsistently describe CR1,4,20 and may not be equipped with strategies and tools to effectively teach and facilitate the development of CR abilities necessary for patient care.24 Faculty development in the realm of CR is an essential component to fostering increased homogeneity and consistency in the teaching, learning, and assessment of CR. Therefore, development of a CR DOC in professional physical therapist education will likely drive the much needed educational innovation and collaboration across institutions and scholarly agendas, ultimately optimizing patient-centered care while reducing errors.14 Identifying CR as a separate DOC, similar to medicine’s call for change, explicitly emphasizes the foundational nature of this construct in practice and education to optimize patient care.14
Residency Education: Leading the Way
Compared with professional physical therapist education, postprofessional residency education is still in the infancy stage of development. Yet, residency education has already adopted a CBE framework and developed a learner assessment tool based on DOCs, competencies, and milestones.7,10 In 2014, the American Board of Physical Therapy Residency and Fellowship Education appointed a task force to develop competencies and create an assessment tool to evaluate resident abilities across points in time, all aimed at assuring the public that residency graduates have the knowledge, skills, and abilities to safely provide effective care.10 Seven domains of competence have been established in residency education and include CR, knowledge for specialty practice, professionalism, communication, education, systems-based practice, and patient management.11 Advancing CR is considered a priority and a cornerstone of residency education.25 The desire to improve CR is one of the major reasons physical therapists pursue residency education.25 The Figure identifies components of CBE related to CR that currently exist in physical therapist education as well as gaps that span the educational continuum. This visual illustrates the need to link existing DOCs in residency to DOCs that should be developed in professional education and expert practice.11
Making CR a Core Competency: A Call to Action
As described above, CR is complex, contextual, and multifactorial yet crucial to optimal patient care. The time has arrived for us to more intentionally focus on CR as an explicit and separate DOC in professional physical therapist education, a domain that is currently lacking in the forthcoming Education Leadership Partnership recommendations. The development of effective CR abilities in professional physical therapist students has been an ongoing recommendation given the critical nature of CR to physical therapist practice, yet best practice, including curricular guidelines in teaching, learning, and assessment of CR, has yet to be formally established.3 Efforts to explicitly include CR and guide best practice in teaching, learning, and assessment of CR as a foundational component of practice are long overdue.
Author Contributions
Concept/idea/research design: J.A. Furze, L. Black, A.W. McDevitt, K.L. Kobal, S.J. Durning, G.M. Jensen
Writing: J.A. Furze, L. Black, A.W. McDevitt, K.L. Kobal, S.J. Durning, G.M. Jensen
Consultation (including review of manuscript before submitting): J.A. Furze, A.W. McDevitt, S.J. Durning, G.M. Jensen
Funding
There are no funders to report for this work.
Disclosures and Presentations
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
The views expressed herein are those of the authors and not necessarily those of the Department of Defense, the Uniformed Services University, or other federal agencies.




Comments