-
PDF
- Split View
-
Views
-
Cite
Cite
Han Eol Cho, Won Ah Choi, Sang-Yoep Lee, Seong-Woong Kang, Standardization of Air Stacking as Lung Expansion Therapy for Patients With Restrictive Lung Disease: A Pilot Study, Physical Therapy, Volume 102, Issue 9, September 2022, pzac092, https://doi.org/10.1093/ptj/pzac092
Close - Share Icon Share
Abstract
Although air stacking is a widely used lung expansion therapy essential for restrictive lung diseases, important details such as peak insufflation pressure (PIP) and number of squeezes have not been investigated. The purpose of this study was to standardize a method of air stacking to minimize problems with its application by identifying the optimal pressure and number of squeezes performed by professional physicians and investigating the current status of routine air stacking implementation in patients.
This prospective cross-sectional test–retest study involved individuals who had neuromuscular disorders and had performed air stacking exercise for longer than 1 year. PIP and number of squeezes were measured to identify the differences between caregivers and physicians. Cases of incorrectly performed air stacking were investigated and categorized. The problems associated with air stacking were evaluated.
A total of 45 participants were included. PIP was 41.4 (SD = 4.2; range = 34.8–50.0) cm H2O, and optimal number of squeezes was 3.1 (SD = 0.5; range = 2–4). When the air stacking methods used by caregivers were evaluated, 19 of 45 caregivers (42.2%) used methods inappropriately. Higher PIP and larger number of squeezes were observed with caregiver implementation. Thirty caregivers (66.7%) experienced finger or wrist pain; this problem was observed especially in female caregivers, who tended to incorrectly perform air stacking.
This pilot study showed that the optimal pressure of air stacking was 35 to 50 cm H2O. Caregivers often perform air stacking inappropriately, leading to complications without achieving the purpose of air stacking. The introduction of a new method, such as manometry, can be helpful for achieving optimal air stacking.
Optimal pressure of air stacking can be measured with inexpensive, simple, and commercially available digital manometry. This approach enables air stacking to be performed and taught more accurately and efficiently and reduces complications in both patients and caregivers.
Introduction
Atelectasis is a common and serious complication for individuals who have difficulty taking deep breaths. Lung expansion therapy is the treatment of choice for such individuals. Lung expansion therapy is used for a short period of time when the reason for inability to breathe deeply is temporary, such as postoperative status and heavy sedation. However, individuals with restrictive lung diseases, such as neuromuscular disorders (NMD) and cervical cord injury, lose their ability to maintain deep breathing due to weakened inspiratory and expiratory muscles. Individuals with restrictive lung diseases do not have the strength to fully expand the lungs and chest walls, with intermittent deep breaths or sighs necessary to prevent closure of lung components.1 This results in not only atelectasis but also reduced pulmonary compliance and increased stiffness of the chest wall and lung tissues,2 ultimately reducing pre-cough volume. “Air stacking,” a widely used method of active lung expansion therapy using a manual resuscitation bag for those with restrictive lung diseases, is a way to prevent lungs from losing compliance.3,4 Therefore, individuals with restrictive lung diseases require air stacking for lung and chest wall expansion throughout the lifespan.
However, the endpoint of air stacking is determined by chest fullness experienced by the individual and the resistance felt in the hand of the assistant squeezing the manual resuscitation bag (Fig. 1A). The subjective nature of air stacking has caused anxiety for those who perform it and may have resulted in improper implementation, such as barotrauma, due to excessive pressure.5 This emphasizes the need to quantify air stacking methods. However, important details such as peak target pressure and the number of required squeezes to achieve peak pressure have not been investigated.
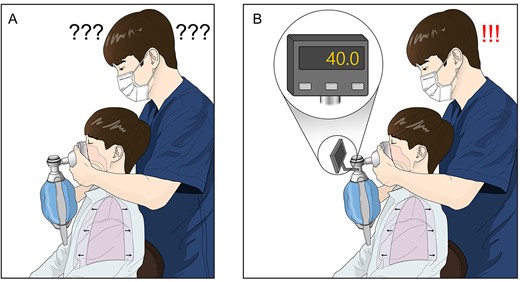
Determining the endpoint of air stacking. (A) There was concern that the peak pressure for the current method of air stacking could be inaccurate because it is dependent on the chest fullness experienced by the patient and the resistance felt in the hand of the assistant. (B) Visual assessment of digitally expressed peak pressure allows the practitioner to perform air stacking accurately and reduces anxiety regarding complications.
We aimed to achieve the following 3 goals in this study: quantify optimal peak insufflation pressure (PIP) during air stacking, investigate common mistakes from the caregivers, and, most importantly, standardize and optimize air stacking procedures.
Methods
Participants
This cross-sectional descriptive study comprised individuals who had NMD and visited the Pulmonary Rehabilitation Center of a tertiary hospital in South Korea between November 2019 and September 2020.
We included only individuals with neuromuscular conditions who had respiratory muscle weakness and whose vital capacity was <2000 mL.6 In addition, to target only those who were familiar with air stacking, we included individuals who previously received training for air stacking at our center and have been conducting air stacking regularly for >1 year.
Individuals with the possibility of ineffective breath holding (individuals with bulbar dysfunction, such as amyotrophic lateral sclerosis or tracheostomy) were not included, because they usually cannot execute correct air stacking. In addition, we identified all types of inconveniences in caregivers.
Clinical and Spirometric Data and Quantification of Pressure During Air Stacking
Before the study began, clinical and spirometric data of the participants were collected, including age, sex, diagnosis, and forced vital capacity (FVC). FVC was measured with a portable spirometer (Micro Medical Ltd, Rochester, Kent, UK) with participants in a sitting position7 and was expressed as a percentage of the predicted normal value.8,9 The maximum insufflation capacity was attained by the participant taking a deep breath and holding it; air stacking then consecutively delivered volumes of air via an oral-nasal interface.
To measure the pressure during air stacking, a digital manometer (Respironics Inc, Murrysville, PA, USA) was installed between the manual resuscitation bag and oronasal mask applied to the participants (Suppl Fig. 1). Theoretically, pressure at the airway opening (mouth) is the same as alveolar pressure (intrapulmonary pressure) at the end of air stacking when respiratory air flow is zero.10 In other words, intrapulmonary pressure can be measured indirectly as the pressure at the mouth in the maximum insufflation capacity state (Suppl Fig. 2).
Assessing the Adequacy of a Caregiver’s Ability to Perform Air Stacking
The evaluation was conducted on the same day or the next day after participants and caregivers agreed to the study. First, air stacking was performed by caregivers as their usual practical method. A physician evaluated whether these procedures were performed well. To determine the suitability of assistance from caregivers, the physician checked to determine whether the following 3 criteria were satisfied: the timing of squeezing by caregivers and inhalation by participants were well synchronized; the participant experienced chest fullness; and the moment when the participant felt chest fullness during air stacking was identical to the moment when resistance was felt in the caregiver’s hand while squeezing the manual resuscitation bag. All criteria were satisfied, then the participant was assigned to the appropriate force group; if any of these were not satisfied, then the participant was assigned to the inappropriate force group.
Based on the mistakes that caregivers made while performing air stacking, the participants in the inappropriate force group were classified into 3 categories. Category 1 (failure to reach the maximum insufflation capacity) was defined as when air stacking was performed but failed to reach the maximum insufflation capacity. Category 2 (asynchronization during air stacking) was defined as cases where the synchronization between the use of a manual resuscitation bag and the participant’s inhalation was not working well. Category 3 (excessive squeezing after the maximum insufflation capacity was reached) defined when caregivers injected excessive amount of air by continuously squeezing the manual resuscitation bag after the participant felt chest fullness and the assistant felt resistance in the hand.
Wrist, Hand, or Finger Pain of Caregivers in Association With Air Stacking
Because of severe limb weakness accompanied by respiratory muscle weakness, caregivers generally perform air stacking exercises by squeezing a manual resuscitation bag. Because the hands are used with the manual resuscitation bag, we checked whether caregivers had any air stacking–related pain or discomfort around the wrists, hands, and fingers.
Measurement of Optimal Peak Pressure and Number of Squeezes When Experts Performed Air Stacking Properly
Air stacking was executed by 2 independent skilled physicians. These skilled physicians have educated more than 200 caregivers on air stacking over the course of 10 years. The skilled physicians stopped the procedure either when resistance was noted while squeezing the manual resuscitation bag or when the participant reported chest fullness. PIP was set as the maximum pressure reached during air stacking. The pressure of each squeeze, PIP, and the number of squeezes preceding PIP were measured. The expiratory volume under PIP status was compared with the maximum insufflation capacity previously measured by other professional medical staff to confirm the suitability of PIP.
Data Analysis
The sample size was therefore determined by using an effect size of 0.5 with an alpha error of .05 and a 1 − beta error of .9. The total sample size was calculated as 45, and the actual power was 0.9000306.
Participant demographics were expressed as numbers or mean (SD). PIP values by caregivers and by skilled, experienced physicians were compared using a paired t test. A chi-square test was used to compare the presence of musculoskeletal pain. The Intraclass correlation coefficient (ICC) was used to evaluate the consistency of the measurements of PIP among physicians. There were no missing values. For visualizing squeezing-pressure relationships, a spaghetti plot technique was used to show the pressure changes in individuals. All statistical analyses were performed using R software version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Role of the Funding Source
The funders played no role in the design, conduct, or reporting of this study.
Results
Basic Characteristics of Patients
A total of 45 participants were enrolled in this study. The average age was 26.7 (SD = 7.9) years. Forty participants were men. All participants had respiratory muscle weakness; the range of predicted percentages for FVC was 5.2% to 37.5%. The number of participants with each diagnosis is presented in Table 1.
| Characteristic . | Value . |
|---|---|
| Age, y | |
| Mean (SD) | 26.7 (7.9) |
| Range | 14.4–49.4 |
| No. of men/women | 40/5 |
| Diagnosis | 45 |
| Duchenne muscular dystrophy | 31 |
| Spinal muscular atrophy | 5 |
| Limb girdle muscular dystrophy | 3 |
| Congenital myopathy | 3 |
| Charcot–Marie–Tooth disease | 2 |
| Guillain-Barré syndrome | 1 |
| Forced vital capacity, mL | |
| Mean (SD) | 623.4 (323.8) |
| Range | 180–1530 |
| Forced vital capacity, % of predicted normal value | |
| Mean (SD) | 15.0 (8.6) |
| Range | 5.2–37.5 |
| Maximum insufflation capacity, mL | |
| Mean (SD) | 1528.2 (401.3) |
| Range | 600–2550 |
| Characteristic . | Value . |
|---|---|
| Age, y | |
| Mean (SD) | 26.7 (7.9) |
| Range | 14.4–49.4 |
| No. of men/women | 40/5 |
| Diagnosis | 45 |
| Duchenne muscular dystrophy | 31 |
| Spinal muscular atrophy | 5 |
| Limb girdle muscular dystrophy | 3 |
| Congenital myopathy | 3 |
| Charcot–Marie–Tooth disease | 2 |
| Guillain-Barré syndrome | 1 |
| Forced vital capacity, mL | |
| Mean (SD) | 623.4 (323.8) |
| Range | 180–1530 |
| Forced vital capacity, % of predicted normal value | |
| Mean (SD) | 15.0 (8.6) |
| Range | 5.2–37.5 |
| Maximum insufflation capacity, mL | |
| Mean (SD) | 1528.2 (401.3) |
| Range | 600–2550 |
Data are reported as number of patients unless otherwise indicated.
| Characteristic . | Value . |
|---|---|
| Age, y | |
| Mean (SD) | 26.7 (7.9) |
| Range | 14.4–49.4 |
| No. of men/women | 40/5 |
| Diagnosis | 45 |
| Duchenne muscular dystrophy | 31 |
| Spinal muscular atrophy | 5 |
| Limb girdle muscular dystrophy | 3 |
| Congenital myopathy | 3 |
| Charcot–Marie–Tooth disease | 2 |
| Guillain-Barré syndrome | 1 |
| Forced vital capacity, mL | |
| Mean (SD) | 623.4 (323.8) |
| Range | 180–1530 |
| Forced vital capacity, % of predicted normal value | |
| Mean (SD) | 15.0 (8.6) |
| Range | 5.2–37.5 |
| Maximum insufflation capacity, mL | |
| Mean (SD) | 1528.2 (401.3) |
| Range | 600–2550 |
| Characteristic . | Value . |
|---|---|
| Age, y | |
| Mean (SD) | 26.7 (7.9) |
| Range | 14.4–49.4 |
| No. of men/women | 40/5 |
| Diagnosis | 45 |
| Duchenne muscular dystrophy | 31 |
| Spinal muscular atrophy | 5 |
| Limb girdle muscular dystrophy | 3 |
| Congenital myopathy | 3 |
| Charcot–Marie–Tooth disease | 2 |
| Guillain-Barré syndrome | 1 |
| Forced vital capacity, mL | |
| Mean (SD) | 623.4 (323.8) |
| Range | 180–1530 |
| Forced vital capacity, % of predicted normal value | |
| Mean (SD) | 15.0 (8.6) |
| Range | 5.2–37.5 |
| Maximum insufflation capacity, mL | |
| Mean (SD) | 1528.2 (401.3) |
| Range | 600–2550 |
Data are reported as number of patients unless otherwise indicated.
Quantification of Appropriate PIP for Air Stacking
When air stacking was performed by skilled physicians, the mean PIP was 41.4 (SD = 4.2 [range = 34.8–50.0]) cm H2O (Fig. 2). The average number of squeezes required to achieve PIP was 3.1 (SD = 0.5 [range = 2–4]) times. The ICCs between 2 skilled physicians were 0.86 (95% CI = 0.75 to 0.93) for PIP and 1.00 (95% CI = 1.00 to 1.00) for number of squeezes.
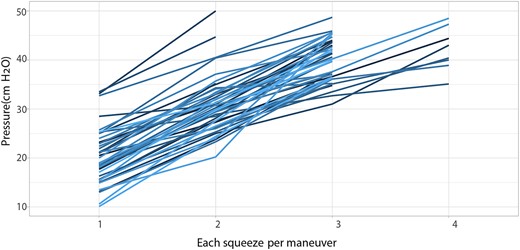
Peak insufflation pressure of each squeeze during air stacking assisted by skilled physicians.
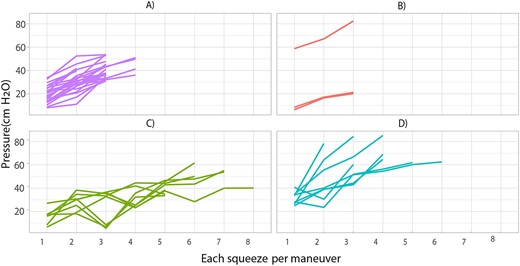
Peak insufflation pressure of each squeeze during air stacking assisted by caregivers for each group. (A) Appropriate force group. (B) Inappropriate force group category 1 (failure to reach maximum insufflation capacity). (C) Inappropriate force group category 2 (asynchronization during air stacking). (D) Inappropriate force group category 3 (excessive squeezing after maximum insufflation capacity was reached).
Differences in PIP and Number of Squeezes When Performed by Caregivers
When air stacking was performed by caregivers, the number of squeezes required to reach PIP was 3.7 (SD = 1.4) (range = 2–8) times and was more widely distributed than that for physicians (P = .003). Twelve participants (26.7%) needed more than 4 squeezes to reach PIP, the average of which was 47.2 (SD = 15.7) (range = 20.1–85.2) cm H2O, higher than with the physicians’ practice (P = .022) (Tab. 2; Fig. 3).
Assessment of the Suitability of Air Stacking
The appropriate force group included 26 participants, and the inappropriate force group comprised 19 participants. The appropriate force group showed no difference in PIP or number of squeezes between caregivers and physicians, whereas a higher PIP and a larger number of squeezes were observed in the inappropriate force group (Tab. 2).
Among 19 participants in the inappropriate force group, 3, 8, and 8 patients were classified as category 1 (failure to reach the maximum insufflation capacity), category 2 (asynchronization during air stacking), and category 3 (excessive squeezing after the maximum insufflation capacity was reached), respectively (Tab. 3).
Comparison of Air Stacking Results According to Assistant and Appropriateness
| Group (No. of Patients) . | Peak Insufflation Pressure, cm H2O . | No. of Squeezes . | ||||
|---|---|---|---|---|---|---|
| By CaregiversMean (SD) . | By Skilled PhysiciansMean (SD) . | P . | By CaregiversMean (SD) . | By Skilled PhysiciansMean (SD) . | P . | |
| Total (45) | 47.2 (15.7) | 41.4 (4.2) | .009a | 3.7 (1.4) | 3.1 (0.5) | .003a |
| Appropriate force (26) | 40.7 (7.0) | 40.6 (4.3) | .948 | 3.0 (0.5) | 3.0 (0.3) | 1.000 |
| Inappropriate force (19) | 56.0 (19.8) | 42.5 (3.8) | .004a | 4.7 (1.7) | 3.3 (0.6) | .001a |
| Group (No. of Patients) . | Peak Insufflation Pressure, cm H2O . | No. of Squeezes . | ||||
|---|---|---|---|---|---|---|
| By CaregiversMean (SD) . | By Skilled PhysiciansMean (SD) . | P . | By CaregiversMean (SD) . | By Skilled PhysiciansMean (SD) . | P . | |
| Total (45) | 47.2 (15.7) | 41.4 (4.2) | .009a | 3.7 (1.4) | 3.1 (0.5) | .003a |
| Appropriate force (26) | 40.7 (7.0) | 40.6 (4.3) | .948 | 3.0 (0.5) | 3.0 (0.3) | 1.000 |
| Inappropriate force (19) | 56.0 (19.8) | 42.5 (3.8) | .004a | 4.7 (1.7) | 3.3 (0.6) | .001a |
Significant at P < .05
Comparison of Air Stacking Results According to Assistant and Appropriateness
| Group (No. of Patients) . | Peak Insufflation Pressure, cm H2O . | No. of Squeezes . | ||||
|---|---|---|---|---|---|---|
| By CaregiversMean (SD) . | By Skilled PhysiciansMean (SD) . | P . | By CaregiversMean (SD) . | By Skilled PhysiciansMean (SD) . | P . | |
| Total (45) | 47.2 (15.7) | 41.4 (4.2) | .009a | 3.7 (1.4) | 3.1 (0.5) | .003a |
| Appropriate force (26) | 40.7 (7.0) | 40.6 (4.3) | .948 | 3.0 (0.5) | 3.0 (0.3) | 1.000 |
| Inappropriate force (19) | 56.0 (19.8) | 42.5 (3.8) | .004a | 4.7 (1.7) | 3.3 (0.6) | .001a |
| Group (No. of Patients) . | Peak Insufflation Pressure, cm H2O . | No. of Squeezes . | ||||
|---|---|---|---|---|---|---|
| By CaregiversMean (SD) . | By Skilled PhysiciansMean (SD) . | P . | By CaregiversMean (SD) . | By Skilled PhysiciansMean (SD) . | P . | |
| Total (45) | 47.2 (15.7) | 41.4 (4.2) | .009a | 3.7 (1.4) | 3.1 (0.5) | .003a |
| Appropriate force (26) | 40.7 (7.0) | 40.6 (4.3) | .948 | 3.0 (0.5) | 3.0 (0.3) | 1.000 |
| Inappropriate force (19) | 56.0 (19.8) | 42.5 (3.8) | .004a | 4.7 (1.7) | 3.3 (0.6) | .001a |
Significant at P < .05
| Category . | Patient Age, yb . | Diagnosis . | Peak Insufflation Pressure by Caregivers . | No. of Squeezes by Caregivers . | Peak Insufflation Pressure by Physicians . | No. of Squeezes by Physicians . |
|---|---|---|---|---|---|---|
| 1 (failure to reach maximum insufflation capacity) | 19 | DMD | 21.2 | 3 | 37.6 | 3 |
| 22 | DMD | 20.1 | 3 | 37.1 | 3 | |
| 30 | DMD | 82.4c | 3 | 42.1 | 3 | |
| 2 (asynchronization during air stacking) | 26 | DMD | 53.9 | 7 | 35.1 | 4 |
| 19 | DMD | 40.1 | 8 | 40.6 | 3 | |
| 25 | SMA | 61.6 | 6 | 44.7 | 3 | |
| 24 | DMD | 55.1 | 7 | 47.3 | 4 | |
| 24 | DMD | 33.6 | 5 | 42.3 | 3 | |
| 22 | SMA | 50.1 | 6 | 40.0 | 4 | |
| 26 | DMD | 41.9 | 5 | 41.8 | 3 | |
| 35 | DMD | 38.4 | 5 | 39.9 | 3 | |
| 3 (excessive squeezing after maximum insufflation capacity was reached) | 21 | DMD | 85.2 | 4 | 44.4 | 4 |
| 34 | DMD | 84.3 | 3 | 45.7 | 3 | |
| 30 | CMT | 60.3 | 3 | 48.5 | 4 | |
| 23 | DMD | 61.9 | 5 | 44.7 | 3 | |
| 37 | DMD | 69.0 | 4 | 43.0 | 3 | |
| 37 | DMD | 64.7 | 4 | 41.3 | 3 | |
| 14 | Congenital myopathy | 78.3 | 2 | 50.0 | 2 | |
| 46 | DMD | 62.5 | 6 | 40.4 | 4 |
| Category . | Patient Age, yb . | Diagnosis . | Peak Insufflation Pressure by Caregivers . | No. of Squeezes by Caregivers . | Peak Insufflation Pressure by Physicians . | No. of Squeezes by Physicians . |
|---|---|---|---|---|---|---|
| 1 (failure to reach maximum insufflation capacity) | 19 | DMD | 21.2 | 3 | 37.6 | 3 |
| 22 | DMD | 20.1 | 3 | 37.1 | 3 | |
| 30 | DMD | 82.4c | 3 | 42.1 | 3 | |
| 2 (asynchronization during air stacking) | 26 | DMD | 53.9 | 7 | 35.1 | 4 |
| 19 | DMD | 40.1 | 8 | 40.6 | 3 | |
| 25 | SMA | 61.6 | 6 | 44.7 | 3 | |
| 24 | DMD | 55.1 | 7 | 47.3 | 4 | |
| 24 | DMD | 33.6 | 5 | 42.3 | 3 | |
| 22 | SMA | 50.1 | 6 | 40.0 | 4 | |
| 26 | DMD | 41.9 | 5 | 41.8 | 3 | |
| 35 | DMD | 38.4 | 5 | 39.9 | 3 | |
| 3 (excessive squeezing after maximum insufflation capacity was reached) | 21 | DMD | 85.2 | 4 | 44.4 | 4 |
| 34 | DMD | 84.3 | 3 | 45.7 | 3 | |
| 30 | CMT | 60.3 | 3 | 48.5 | 4 | |
| 23 | DMD | 61.9 | 5 | 44.7 | 3 | |
| 37 | DMD | 69.0 | 4 | 43.0 | 3 | |
| 37 | DMD | 64.7 | 4 | 41.3 | 3 | |
| 14 | Congenital myopathy | 78.3 | 2 | 50.0 | 2 | |
| 46 | DMD | 62.5 | 6 | 40.4 | 4 |
CMT = Charcot–Marie–Tooth disease; DMD = Duchenne muscular dystrophy; SMA = spinal muscular atrophy.
All patients were male.
Air did not transfer to the lungs and remained in the mouth.
| Category . | Patient Age, yb . | Diagnosis . | Peak Insufflation Pressure by Caregivers . | No. of Squeezes by Caregivers . | Peak Insufflation Pressure by Physicians . | No. of Squeezes by Physicians . |
|---|---|---|---|---|---|---|
| 1 (failure to reach maximum insufflation capacity) | 19 | DMD | 21.2 | 3 | 37.6 | 3 |
| 22 | DMD | 20.1 | 3 | 37.1 | 3 | |
| 30 | DMD | 82.4c | 3 | 42.1 | 3 | |
| 2 (asynchronization during air stacking) | 26 | DMD | 53.9 | 7 | 35.1 | 4 |
| 19 | DMD | 40.1 | 8 | 40.6 | 3 | |
| 25 | SMA | 61.6 | 6 | 44.7 | 3 | |
| 24 | DMD | 55.1 | 7 | 47.3 | 4 | |
| 24 | DMD | 33.6 | 5 | 42.3 | 3 | |
| 22 | SMA | 50.1 | 6 | 40.0 | 4 | |
| 26 | DMD | 41.9 | 5 | 41.8 | 3 | |
| 35 | DMD | 38.4 | 5 | 39.9 | 3 | |
| 3 (excessive squeezing after maximum insufflation capacity was reached) | 21 | DMD | 85.2 | 4 | 44.4 | 4 |
| 34 | DMD | 84.3 | 3 | 45.7 | 3 | |
| 30 | CMT | 60.3 | 3 | 48.5 | 4 | |
| 23 | DMD | 61.9 | 5 | 44.7 | 3 | |
| 37 | DMD | 69.0 | 4 | 43.0 | 3 | |
| 37 | DMD | 64.7 | 4 | 41.3 | 3 | |
| 14 | Congenital myopathy | 78.3 | 2 | 50.0 | 2 | |
| 46 | DMD | 62.5 | 6 | 40.4 | 4 |
| Category . | Patient Age, yb . | Diagnosis . | Peak Insufflation Pressure by Caregivers . | No. of Squeezes by Caregivers . | Peak Insufflation Pressure by Physicians . | No. of Squeezes by Physicians . |
|---|---|---|---|---|---|---|
| 1 (failure to reach maximum insufflation capacity) | 19 | DMD | 21.2 | 3 | 37.6 | 3 |
| 22 | DMD | 20.1 | 3 | 37.1 | 3 | |
| 30 | DMD | 82.4c | 3 | 42.1 | 3 | |
| 2 (asynchronization during air stacking) | 26 | DMD | 53.9 | 7 | 35.1 | 4 |
| 19 | DMD | 40.1 | 8 | 40.6 | 3 | |
| 25 | SMA | 61.6 | 6 | 44.7 | 3 | |
| 24 | DMD | 55.1 | 7 | 47.3 | 4 | |
| 24 | DMD | 33.6 | 5 | 42.3 | 3 | |
| 22 | SMA | 50.1 | 6 | 40.0 | 4 | |
| 26 | DMD | 41.9 | 5 | 41.8 | 3 | |
| 35 | DMD | 38.4 | 5 | 39.9 | 3 | |
| 3 (excessive squeezing after maximum insufflation capacity was reached) | 21 | DMD | 85.2 | 4 | 44.4 | 4 |
| 34 | DMD | 84.3 | 3 | 45.7 | 3 | |
| 30 | CMT | 60.3 | 3 | 48.5 | 4 | |
| 23 | DMD | 61.9 | 5 | 44.7 | 3 | |
| 37 | DMD | 69.0 | 4 | 43.0 | 3 | |
| 37 | DMD | 64.7 | 4 | 41.3 | 3 | |
| 14 | Congenital myopathy | 78.3 | 2 | 50.0 | 2 | |
| 46 | DMD | 62.5 | 6 | 40.4 | 4 |
CMT = Charcot–Marie–Tooth disease; DMD = Duchenne muscular dystrophy; SMA = spinal muscular atrophy.
All patients were male.
Air did not transfer to the lungs and remained in the mouth.
Category 1 (Failure to Reach Maximum Insufflation Capacity)
Two participants finished their air stacking near a PIP of 20 cm H2O. When skilled physicians performed air stacking for these participants, the pressure was measured at approximately 37 cm H2O, and participants reported chest fullness that they had not experienced during routine practice. When air stacking was performed for the other participant, air did not transfer to the lungs and remained in the mouth. The pressure was >80 cm H2O, but the participant did not feel chest fullness. After reeducation and with air stacking performed by skilled physicians, the participant reported tightness of the chest even at a pressure of 42.1 cm H2O (Fig. 3B).
Category 2 (Asynchronization During Air Stacking)
In 8 participants, inspiration was out of sync with the squeeze timing of the manual resuscitation bag. This category showed the volatility of pressure for each squeeze during air stacking. Fluctuation of pressure was due to flawed practice of air stacking. When a manual resuscitation bag is used incorrectly, the air flow can be obstructed by the glottis, resulting in a relatively high pressure. However, when a manual resuscitation bag is used properly, the pressure decreases as air flow is no longer blocked by the glottis. In most cases, asynchronicity during air stacking prevented sufficient air delivery to the lungs, resulting in caregivers squeezing more than 5 times to achieve proper PIP. However, when a skilled physician performed air stacking, only 3 or 4 squeezes were required (Fig. 3C).
Category 3 (Excessive Squeezing After the Maximum Insufflation Capacity Was Reached)
In these cases, PIP was too high, surpassing 60 cm H2O when performed by caregivers. In comparison, the range was 40 to 50 cm H2O when performed by skilled physicians. This was caused by forceful squeezing after the lungs were filled with air (Fig. 3D).
Wrist, Hand, or Finger Pain of Caregivers
Of the 45 caregivers who participated in the study, 30 (66.7%) experienced finger or wrist pain that lasted >3 months. None of the 5 male caregivers reported discomfort, whereas 75.0% (30/40) of the female caregivers reported pain. Two female caregivers squeezed the manual resuscitation bag in a modified way; 1 caregiver placed the resuscitator bag on the floor and used both of her knees to compress the resuscitator bag, and the other used the left forearm to hold the bag and compressed the bag with the right fist. In the appropriate group, 17 of 26 caregivers (65.4%) experienced pain. Similarly, 13 of 19 caregivers (68.4%) in the inappropriate group (P = .831) reported pain.
To identify differences by group among female caregivers, we created subgroups of excessive force used during air stacking (categories 2 and 3) and appropriate force (appropriate force group and category 1). All caregivers in the excessive force group reported pain (100%; 12 out of 12), whereas the percentage of caregivers in the appropriate force group who reported pain was only 67.9% (19 out of 28 [P = .037]).
Discussion
Our data gathered from skilled physicians suggest a proper range of PIP during air stacking of 35 to 50 cm H2O, which can be achieved by 2 to 4 compressions of the manual resuscitation bag. Also, many caregivers inappropriately performed air stacking, which might be modified with digitally expressed manometry.
The maximum insufflation capacity is the maximum volume of air that can be held in the lungs with a closed glottis after insufflation and is one of the most important variables in participants with restrictive lung diseases. Just as weakness of limbs does not cause immediate contracture, decreased FVC and total lung capacity do not indicate an immediate loss of maximum space in which the lung can be passively stretched. FVC and total lung capacity reflect active range of motion, and decrease as soon as the respiratory muscle weakens. On the other hand, the maximum insufflation capacity, which reflects compliance of the chest cavity, may not decrease even after muscle weakness (Suppl. Fig. 3). A previous study showed that the maximum insufflation capacity can be maintained or even increased with air stacking, regardless of the decrease in FVC.2 Because the maximum insufflation capacity is related to the assisted cough capacity,11 air stacking can prevent lung morbidities, including pneumonia. In addition, because air stacking can slow deterioration of cough flows12 and preserve FVC,4 it is recommended in individuals with NMD and respiratory muscle weakness.13
However, there are always concerns about barotrauma because such air stacking passively stretches lungs.14,15 Previous papers reported barotrauma with excessive pressure to the lung, although there was no direct mention of air stacking. One clinical study reported that a PIP of >50 cm H2O in individuals using mechanical ventilators increased the risk of barotrauma.16 An animal study showed alveolar edema microvascular injury in rats exposed to a peak airway pressure of 45 cm H2O over 20 minutes.15 Loewen et al suggested that regional variability in the lung during air stacking could cause areas of overdistension leading to pneumothorax,17 which has been supported by other studies.5,18 However, Bach revealed the safety of air stacking based on extensive clinical experience; he reported no cases of pneumothorax over 28 years in more than 1000 individuals with NMD who had undergone air stacking, even when the airway pressure exceeded 60 cm H2O.12,19 In agreement, we have educated and encouraged all patients without major risk factors to undergo air stacking over 20 years at our center, including more than 1000 individuals with NMD or cervical cord syndrome with respiratory weakness. Among these individuals, there was no experience of pneumothorax directly caused by air stacking. The reason that air stacking is safe in practice might be that the actual duration of excessive pressure during 1 cycle of air stacking is only a few seconds (Suppl. Fig. 4). Though we could not find studies to directly support this, early studies using mechanical insufflation-exsufflation showed indirect supportive evidence. Early studies of mechanical insufflation-exsufflation revealed that a positive pressure of 40 mm Hg (approximately 55 cm H2O) did not damage the lung,20,21 indirectly indicating that a short duration of high pressure does not have a harmful effect in clinical settings. Despite the evidence, however, the issue of barotrauma caused by air stacking cannot be completely eliminated because the pressure is directly applied to the lung.
This study aimed to eliminate such concerns by providing an optimal PIP range of air stacking. The study showed proper range of PIP during air stacking of 35 to 50 cm H2O. To our knowledge, there has been no previous direct research on the appropriate pressure for air stacking. However, 1 study revealed that the normal lung is inflated fully (total lung capacity) at a minimum transalveolar pressure of 35 cm H2O.22 Considering that the purpose of air stacking is to maximally expand the chest cavity, a pressure >35 cm H2O should be considered a theoretical target. In addition, we suggest that digitally expressed manometry can be helpful for achieving proper pressure during air stacking. Digitally expressed manometry can also help facilitate patient education. In our center, professional medical personnel have been repetitively educating patients and caregivers about air stacking according to the consensus of pulmonary rehabilitation.13 The patients and caregivers who performed air stacking exercises proficiently did not show significant differences from skilled physicians. However, some patients and caregivers who performed the exercises improperly showed significant variations from our standards. This demonstrates the need to make it easier for patients and caregivers to understand the method of air stacking. At the end of our study, we reeducated participants and caregivers on proper air stacking with digital manometry to give them visual assessment of pressure (Fig. 1B). The result was successful. It was much easier to make people understand the method of air stacking with visual feedback than by simply explaining the concept and method of air stacking abstractly. Caregivers were satisfied with the education using manometry, and the majority of them even asked if they could use manometry at home. There are several inexpensive, small, and lightweight portable manometers on the market. Connecting them to manual resuscitation bags will not only support proper air stacking education but will also enable patients and caregivers to conduct air stacking much more accurately based on visual feedback.
Wrist or finger pain was common for female caregivers due to long durations of practice. Notably caregivers who inefficiently performed air stacking showed relatively high rate of wrist or finger pain. Air stacking is a kind of passive stretching and should be performed every day.12,23 However, the problem is that repeated squeezing of the manual resuscitation bag can strain people’s hands and wrists. As the life expectancy of individuals with NMD has increased (eg, the average lifespan of individuals with Duchenne muscular dystrophy was approximately 20 years when there was no specific treatment in the past. Many individuals with Duchenne muscular dystrophy can now expect to live into their fourth decade with standards of care),24 the period of air stacking has also changed from a few years to decades. It means the additional burden on the caregiver’s wrist increases dramatically if they squeeze the manual resuscitation bag only a few times per maneuver due to inefficient air stacking. The methods for reducing these musculoskeletal complications are as follows. First, reduce the number of squeezes by assisting caregivers in efficient air stacking through accurate and repetitive education. According to our results, a properly performed case squeezed the manual resuscitation bag no more than 5 times. The maximum value of in our study was 1590 mL, which was similar to those in past studies.11,25 Because a manual resuscitation bag delivers approximately 500 mL of air per squeeze, it can theoretically reach the maximum insufflation capacity with 3 or 4 squeezes. If a caregiver squeezes the manual resuscitation bag more than 5 times during 1 session of air stacking, the physician should assess the accuracy of the performance. Second, the force applied to the hand should be reduced through slow and gentle squeezing during air stacking. The accurate pressure target with manometry could prevent unnecessary squeezing. Other methods of passive lung expansion therapy, such as using a positive pressure ventilator, mechanical insufflation-exsufflation, or by glossopharyngeal breathing, should also be considered.
Limitations
This study had inherent limitations. We did not include individuals with tracheostomy who need air stacking. Because these individuals often use a volume-targeted ventilator or mechanical insufflation-exsufflation for lung expansion, future study is needed to investigate the accurate volume–pressure relationship during such lung expansion therapy for those individuals. Another limitation was the cross-sectional design of this study. Further study is needed to examine the difference in long-term effects on lung expansion and complications between standardized air stacking under proper pressure and air stacking without standardized education. Lastly, there was a difference in the ratio between sexes. However, this is because we included many individuals with Duchenne muscular dystrophy, which is one of the most common NMD with respiratory problems.
Our data suggest a proper range of PIP during air stacking of 35 to 50 cm H2O, which can be achieved by 2 to 4 compressions of the manual resuscitation bag. It is necessary to measure the pressure digitally to execute proper air stacking. Such pressure can be easily measured using commercially available, lightweight, and small manometry, which allows accurate and efficient teaching and performance of air stacking. This increase in performance is expected to help maintain lung compliance of patients while reducing complications in patients and caregivers.
Author Contributions
Concept/idea/research design: H.E. Cho, W.A. Choi, S.-W. Kang
Writing: H.E. Cho
Data collection: H.E. Cho, S.-Y. Lee
Data analysis: H.E. Cho, S.-Y. Lee, S.-W. Kang
Project management: H.E. Cho, S.-W. Kang
Fund procurement: S.-W. Kang
Providing participants: S.-W. Kang
Providing facilities/equipment: S.-W. Kang
Consultation (including review of manuscript before submitting): H.E. Cho, W.A. Choi, S.-W. Kang
Acknowledgments
The authors thank Medical Illustration & Design, part of the Medical Research Support Services of Yonsei University College of Medicine, for all the artistic support related to this work.
Funding
This work was supported by the Rehabilitation Institute of Neuromuscular Disease, Yonsei University College of Medicine (grant no. 3–2019-0316).
Ethics Approval
This study was approved by the Institutional Review Board of Gangnam Severance Hospital, Seoul, Republic of Korea (IRB no. 3–2019-0316). The study protocol was in accordance with the Declaration of Helsinki.
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.




Comments