-
PDF
- Split View
-
Views
-
Cite
Cite
Christian Erik Preissner, Navin Kaushal, Kathleen Charles, Bärbel Knäuper, A Protection Motivation Theory Approach to Understanding How Fear of Falling Affects Physical Activity Determinants in Older Adults, The Journals of Gerontology: Series B, Volume 78, Issue 1, January 2023, Pages 30–39, https://doi.org/10.1093/geronb/gbac105
Close - Share Icon Share
Abstract
This study applied an extended Protection Motivation Theory to investigate the relative importance of fear of falling (FoF) among motivational and intentional determinants of physical activity (PA) behavior.
Older U.S. adults (N = 667, 65+) were surveyed using online research panels and completed measures of self-efficacy and response efficacy (coping appraisal), perceived vulnerability and perceived severity (threat appraisal), FoF, autonomous motivation, intention, physical health, and past PA level.
Our structural equation model showed that past PA level and health predicted intention via cognitive constructs. PA and health predicted FoF and motivation via threat and coping appraisal. FoF did not directly predict intention.
Results from this sample provide support for the predictive effects of threat appraisal on fear. However, findings suggest that FoF may not be of great importance for the formation of PA intention compared with an established habit of being physically active and a subsequently fostered coping appraisal and motivation.
Older adults are the fastest growing demographic and one of the most vulnerable populations for developing various noncommunicable diseases such as cardiovascular disease, cancer, and osteoarthritis (Barouki et al., 2012). Among other modifiable lifestyle factors associated with psychological aging and well-being (Dogra & Stathokostas, 2012; Mitina et al., 2020), physical activity (PA) has been demonstrated to prevent or reduce the burden of several physical illnesses (Warburton & Brendin 2017). However, older adults are the least active demographic group in the United States: Approximately over 31 million adults aged 50+ are estimated to be inactive (Centers for Disease Control and Prevention, 2019). With older adults gradually representing a larger proportion of society, identifying and targeting modifiable psychological factors that may hinder or promote PA among this demographic is paramount to facilitate healthy aging.
Fear of Falling as a Barrier to PA
Older adults are generally aware of the benefits of maintaining an active lifestyle, as approximately 89% of older adults were aware of health risks associated with living an inactive lifestyle (Goggin & Morrow, 2001). The discrepancy between why older adults are generally aware of the importance of PA and the low participation rates points toward understanding barriers to being or remaining physically active. A specific psychological barrier associated with age and aging is the fear of falling (FoF) that is a pervasive problem in both older adults with and without a history of falling (Hajek et al., 2018; Legters, 2002). FoF refers to a person’s continuous concern about falling that can lead to both protective behavioral adaptations and activity curtailment (Ellmers et al., 2022; Hamed et al., 2021). The latter coping strategy is problematic as regular PA is an effective approach to counteract functional decline and future falls in older adults (Sherrington et al., 2020), and to improve mental, psychological, and social aspects of well-being among this demographic (Langhammer et al., 2018). Therefore, it is key to understand modifiable fear-related and positive coping appraisal processes that may establish intentions to adopt PA as a method to prevent falls and to promote a greater quality of life in older age.
Previous research has identified prominent determinants of FoF (e.g., worse physical health or female gender; Bertera & Bertera, 2008) that may be relevant to what degree an older individual remains or aims to be physically active in the future. However, previous work investigating the relationship between FoF and activity behaviors (a) lacks theoretical underpinnings explaining how preceding psychological and behavioral factors may help mitigate fear, or (b) lacks explicit testing of the applied framework constructs (e.g., Bertera & Bertera, 2008). To effectively guide future interventions, theory-based approaches that are tailored to the behavior and target population are recommended (Davis et al., 2015). Such a theory-based methodology is crucial for keeping findings in scope when considering potentially competing effects of determinants on a behavioral outcome (Davis et al., 2015).
Theoretical Basis of FoF and Activity Behavior
The Protection Motivation Theory (PMT; Rogers, 1983; see Figure 1) proposes a set of constructs that are insightful for understanding the formation of health behavioral intentions, drawing on the premise that an individual will intend to protect themselves from a present health threat (in this case falling). Such intentions are formulated by perceived threat and coping cognitions that can lead to an increased engagement in a preventive behavior (in this case PA) or to avoidance behavior (Ellmers et al., 2022; Rogers, 1983). Whereas threat appraisal consists of evaluations of one’s perceived vulnerability and the perceived severity of the threat, coping appraisal describes (a) the perception that a recommended health behavior effectively prevents the threat (i.e., response efficacy) and (b) confidence in one’s ability to engage in the recommended health behavior (i.e., self-efficacy). The PMT suggests that individuals with high efficacy appraisals are more likely to adopt recommendations to reduce perceived threats when they also judge their own susceptibility and the threat’s severity to be high (Rogers, 1983).
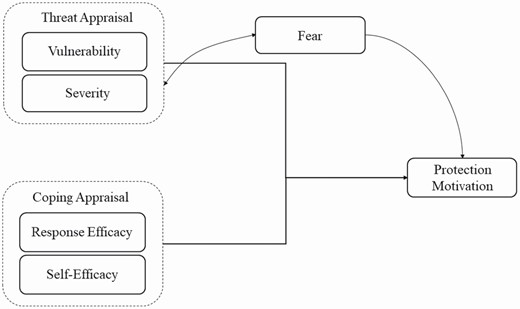
Simplified theoretical backdrop depicting the cognitive processes underlying protection motivation. Adapted from Rogers (1983).
This protection motivation is frequently measured through intentions (i.e., a decisional variable that encompasses whether or not to engage in a behavior and the intensity of this decision; Norman et al., 2005; Sheeran, 2002). Meta-analyses suggest self-efficacy to be the strongest predictor of intention, with threat appraisal being least often associated with intention (Floyd et al., 2000; Milne et al., 2000). Past research has also shown the predictive role of coping appraisal and intention for PA behavior (Plotnikoff & Trinh, 2010), and investigated FoF in context with activity avoidance (Bertera & Bertera, 2008).
However, extensive, theory-based investigations are warranted that embed FoF among other contemporary psychological (e.g., motivational, past health behaviors), health, and sociodemographic factors (e.g., gender) to better understand its unique relation with the intention to be or remain active. In the following, we thus propose an augmented PMT that is (a) informed by contemporary recommendations, (b) acknowledges key demographic and behavioral antecedents of threat and coping appraisal pathways, and (c) models consecutive motivational versus fear pathways that may formulate PA intentions.
Extensions of the Theoretical Basis
To study both the unique effects of FoF and enhance the prediction of PA intention, we integrated relevant determinants into our PMT model that have emerged in previous research on PA and cognitive appraisal processes. We first integrated autonomous motivation (i.e., self-endorsed reasons for engaging in a behavior; Deci & Ryan, 1985) into our PMT extension. Previous studies have identified the predictive role of such self-determination regarding self-efficacy and intention (D’Angelo et al., 2007; Sweet et al., 2009). We suggest that autonomous motivation is affected by coping appraisal constructs that positively affect intention. Second, past research has identified various barriers to affect levels of PA such as one’s levels of pain and health problems (Jenkin et al., 2017). Our extension of the PMT will therefore take physical health status into consideration. Considering findings on gender differences in threat appraisals (Ruthig, 2016) and FoF (Bertera & Bertera, 2008; Pohl et al., 2015), we also added gender to the model as a direct predictor of PMT constructs. Previous studies have suggested female gender to be associated with higher perceived vulnerability and severity of a health threat as well as higher FoF. Third, FoF was explicitly linked to threat appraisal to examine the direct effects of the perceived vulnerability to and the severity of falling on a person’s FoF and the subsequent effects of this pathway on PA intention. Lastly, acknowledging the contemporary gap between intention and behavior (Sheeran & Webb, 2016), we included past PA performance in the model as individuals may likely differ in cognitive and motivational variables based on their PA habits; previous research has demonstrated the importance of such habituation for social cognitions as well as the intention and health behavior in older adults (Kaushal et al., 2021; Preissner et al., 2021).
Whereas prior research explored psychosocial, habitual, and planning processes for PA (but omitting fear processes; Preissner et al., 2021) and focused on the impact of a fall history on health perceptions and PA using a dual-process approach (Kaushal et al., 2021), this paper adds novel insight into fear and motivational mechanisms by (a) investigating FoF via PMT, a framework specific to explaining behavior modification from a threat prevention perspective; (b) testing the effects of response efficacy, a distinct PMT construct, in the formation of PA intentions; (c) examining the association of physical health and gender with both appraisal pathways and FoF; and (d) investigating the association between coping appraisal and motivation while considering threat appraisal and FoF.
Objectives
To examine which psychological and behavioral factors may mitigate FoF and promote behavioral intentions, we first examined interactions between PMT components and intention (H1a–b). Second, we investigated the interrelations between the added determinants (i.e., participant characteristics such as gender, health, and past behavior) with fear, motivation, and intention (H2a–d, H3a–b). The hypothesized interactions within the model are presented in Table 1.
| Hypothesis . | Independent variable(s) . | Dependent variable . | Mediator(s) . |
|---|---|---|---|
| H1a | Vulnerability ↑, Severity ↑ | Intention ↓ | |
| H1b | Self-efficacy ↑, Response efficacy ↑ | Intention ↑ | |
| H2a | Fear of falling ↑ | Intention ↓ | |
| H2b | Autonomous motivation ↑ | Intention ↑ | |
| H2c | Vulnerability ↑, Severity ↑ | Fear of falling ↑ | |
| H2d | Self-efficacy ↑, Response efficacy ↑ | Autonomous motivation ↑ | |
| H3a | Physical health ↑, Past behavior ↑, Gender (male) ↑ | Intention ↑ | Self-efficacy ↑, Response efficacy ↑, Autonomous motivation ↑ |
| H3b | Physical health ↑, Past behavior ↓, Gender (female) ↓ | Fear of falling ↑ | Vulnerability ↑, Severity ↑ |
| Hypothesis . | Independent variable(s) . | Dependent variable . | Mediator(s) . |
|---|---|---|---|
| H1a | Vulnerability ↑, Severity ↑ | Intention ↓ | |
| H1b | Self-efficacy ↑, Response efficacy ↑ | Intention ↑ | |
| H2a | Fear of falling ↑ | Intention ↓ | |
| H2b | Autonomous motivation ↑ | Intention ↑ | |
| H2c | Vulnerability ↑, Severity ↑ | Fear of falling ↑ | |
| H2d | Self-efficacy ↑, Response efficacy ↑ | Autonomous motivation ↑ | |
| H3a | Physical health ↑, Past behavior ↑, Gender (male) ↑ | Intention ↑ | Self-efficacy ↑, Response efficacy ↑, Autonomous motivation ↑ |
| H3b | Physical health ↑, Past behavior ↓, Gender (female) ↓ | Fear of falling ↑ | Vulnerability ↑, Severity ↑ |
| Hypothesis . | Independent variable(s) . | Dependent variable . | Mediator(s) . |
|---|---|---|---|
| H1a | Vulnerability ↑, Severity ↑ | Intention ↓ | |
| H1b | Self-efficacy ↑, Response efficacy ↑ | Intention ↑ | |
| H2a | Fear of falling ↑ | Intention ↓ | |
| H2b | Autonomous motivation ↑ | Intention ↑ | |
| H2c | Vulnerability ↑, Severity ↑ | Fear of falling ↑ | |
| H2d | Self-efficacy ↑, Response efficacy ↑ | Autonomous motivation ↑ | |
| H3a | Physical health ↑, Past behavior ↑, Gender (male) ↑ | Intention ↑ | Self-efficacy ↑, Response efficacy ↑, Autonomous motivation ↑ |
| H3b | Physical health ↑, Past behavior ↓, Gender (female) ↓ | Fear of falling ↑ | Vulnerability ↑, Severity ↑ |
| Hypothesis . | Independent variable(s) . | Dependent variable . | Mediator(s) . |
|---|---|---|---|
| H1a | Vulnerability ↑, Severity ↑ | Intention ↓ | |
| H1b | Self-efficacy ↑, Response efficacy ↑ | Intention ↑ | |
| H2a | Fear of falling ↑ | Intention ↓ | |
| H2b | Autonomous motivation ↑ | Intention ↑ | |
| H2c | Vulnerability ↑, Severity ↑ | Fear of falling ↑ | |
| H2d | Self-efficacy ↑, Response efficacy ↑ | Autonomous motivation ↑ | |
| H3a | Physical health ↑, Past behavior ↑, Gender (male) ↑ | Intention ↑ | Self-efficacy ↑, Response efficacy ↑, Autonomous motivation ↑ |
| H3b | Physical health ↑, Past behavior ↓, Gender (female) ↓ | Fear of falling ↑ | Vulnerability ↑, Severity ↑ |
Method
The present study received ethical approval by the institutional Research Ethics Board at McGill University (#350-0119) as part of a larger survey study to examine psychosocial determinants of PA in older adults (Kaushal et al., 2021; Preissner et al., 2021). The data to reproduce the present analyses are openly available in Mendeley Data (http://dx.doi.org/10.17632/nvy6hpy5nk.1).
Study Design and Setting
Participants were recruited via Prime Panels, a research platform associated with CloudResearch (formerly TurkPrime). This platform allows researchers to recruit specific populations in various countries and to prescreen participants based on precise eligibility characteristics (Chandler et al., 2019). As 25.9% of U.S. Prime Panels participants are suggested to be older adults above the age of 60 (Recruiting Older Adults Online, 2018), this platform was chosen to recruit a sufficiently large and diverse data set of the specific target group of adults aged 65 and older. Participants were informed about the aims of the study and provided informed consent before being directed to the survey. Respondents were compensated with $5.00 for their participation.
Participants
Respondents were older adults living in the United States in different residential settings (i.e., at home alone, at home with family, in an active senior living complex, and in a senior assisted living complex). Participants were required to have Internet access and adequate computer literacy, in addition to being proficient in the English language, living in the United States, and being over the age of 65. In line with current data cleaning procedures regarding online survey panels (Verma et al., 2021), we first screened for non-U.S. Internet protocol addresses as well as improbable reading and completion speed. Second, we excluded data points with more than 30% missing responses (n = 27), and individuals not meeting the specified age requirement (n = 11). Of the initial pool of 705 individuals who completed the survey, 667 met the inclusion criteria.
Variables and Measurement
Intention
Three items were used to assess PA intention, in line with Arnautovska et al. (2017). Mean scores were calculated from the 7-point Likert-type rating scales (1—strongly agree to 7—strongly disagree) for the items “It is likely that I will be regularly physically active,” “I intend to be regularly physically active,” and “I expect to be regularly physically active” (α = 0.98).
Autonomous motivation
Using the Self-Regulation Questionnaire (Ryan & Connell, 1989), participants’ relative autonomous motivation was assessed. Participants responded to 16 items scored on a 7-point Likert-type rating scale corresponding to the self-regulatory styles of external (α = 0.72), intrinsic (α = 0.88), introjected (α = 0.69), and identified regulation (α = 0.95). Examples following the stem of “I try to engage in physical activity on a regular basis because…” include “Because I enjoy physical activity” or “Because others would be angry at me if I do not.” Results were scored in accordance with the Relative Autonomy Index.
Fear of falling
To investigate FoF in the sample population, the Short Falls Efficacy Scale—International was used (Kempen et al., 2007). Respondents gave answers to seven items on a 4-point Likert-type rating scale how concerned (from 1—not at all concerned to 4—very concerned) they were about the possibility of falling when, for example, “Getting dressed or undressed,” “Going up or down stairs,” or “Going out to a social event” (α = 0.91). Full scores (7–28) were utilized in addition to three distinct FoF groups based on the total number; low (7–8), moderate (9–13), and high (14–28). The cutoff points were based on suggestions by Delbaere et al. (2010).
PMT constructs
The measures presented in the following were used to assess PMT constructs regarding falling and PA.
Perceived severity
The item “Experiencing a fall would be a very bad thing to happen to me” (rated on a 5-point Likert-type rating scale from 1—definitely not to 5—definitely yes), adapted for falling from Plotnikoff and Higginbotham (2002), was used to gain insight into older adults’ perceived severity of falling.
Perceived vulnerability
The item “My chances of falling are small” (rated on a 5-point Likert-type rating scale from 1—definitely not to 5—definitely yes), also adapted for falling from Plotnikoff and Higginbotham (2002), was used to gain insight into older adults’ perceived vulnerability regarding FoF.
Response efficacy
Response efficacy was assessed with three items from Plotnikoff and Higginbotham (2002), which were rated on a 5-point Likert-type rating scale from 1—definitely not to 5—definitely yes: “For me, regular physical activity will keep me healthy,” “For me, regular physical activity will help me either remain fit or get fit,” and “For me, regular physical activity will reduce my chances of getting serious health problems,” in addition to the item “Regular physical activity will reduce my risk of falling” (α = 0.88), adapted for falling from Plotnikoff and Higginbotham (2002).
Perceived self-efficacy
To assess perceived self-efficacy, participants were asked to indicate how confident they were in their ability to regularly engage in PA, despite facing obstacles (e.g., “feeling tired,” “not enjoying it,” or “being bothered by the weather”; α = 0.93). Nine items with an 11-point Likert-type rating scale (from 0—not very confident to 10—very confident) were used, based on Resnick et al. (2000).
Physical health status
The 12-item Short Form Health Survey was used to gain insight into self-reported physical health of respondents (Ware et al., 1996). Participants were asked to respond to items in the domains of general health, vitality, bodily pain, social functioning, role limitations, mental health, and physical functioning, rated on a 5-point Likert-type rating scale from 1—not at all to 5—extremely. The domains were summarized into a Physical Component Summary scale (PCS) and a Mental Component Summary scale. Only the PCS was used in the present analyses (α = 0.81).
Physical activity behavior
The Physical Activity Scale for the Elderly (PASE) was used to assess current PA behavior (Washburn et al., 1993), with higher numbers indicating more PA. Participants were asked to indicate how frequently they engaged in, for example, moderate recreational activities or light and heavy housework. Each of the 10 items is split into weekly frequency (never, 1–2 days, 3–4 days, and 5–7 days) and daily frequency (less than 1 hr, 1 but less than 2 hr, 2–4 hr, and more than 4 hr), with the combinations resulting in a frequency value. The values were multiplied by a corresponding weight for each activity type and added up to form the final score (Washburn et al., 1993).
Analysis Plan
The Statistical Package for the Social Sciences v. 25 (SPSS Inc., Chicago, IL) was used to conduct analyses of demographic data and zero-order bivariate correlations. Analysis of missing data on individual items showed all missing values to be below 1%, apart from two items used for the PCS calculation. We found data to be missing completely at random (MCAR χ 2 (383) = 316.497, p = .994). Missing values were replaced using hierarchical regression imputation prior to testing our hypotheses. However, due to the design of PASE with distinct weights based on the combination of weekly and daily frequency, any missing values on PASE subscales (<1%) were not replaced, and the respective subscales were not included in the total score calculations. Cutoff points by Delbaere et al. (2010) were utilized to gain insight into the prevalence of high FoF in the sample. Maximum likelihood estimation method in AMOS v. 22.0 was employed to test the proposed model (Enders, 2011). We followed estimation criteria by Wolf et al. (2013) to assure that the sample we recruited as part of a larger study was of sufficient size to conduct the present structural equation model. Considering the number of latent factors, number of indicators, an estimated power >80%, and α = 0.05, we estimated that a minimum sample size of 138 participants would be needed to test the proposed model. Cutoff points for the comparative fit index (CFI; equal to or greater than 0.90), the root mean square error of approximation (RMSEA; less than or equal to 0.08 with a confidence interval [CI] of 95%), as well as the Tucker–Lewis index (TLI; greater than or equal to 0.90) were used to assess goodness of fit (Hu & Bentler, 1999). The estimates reported in the following are standardized coefficients.
Results
Descriptives
The sample consisted of 667 individuals (56.7% female, Mage = 70.36 years, SD = 4.70, range = 65–92 years) residing in the United States. Participants predominantly identified as Caucasian (89.4%), followed by African American (6.1%). The majority of respondents was retired (n = 528, 79.2%, Mage = 70.66 years, SD = 4.79), with 45 individuals still employed full-time (Mage = 68.64 years, SD = 4.33) and 57 working part-time (Mage = 68.98 years, SD = 3.38). The participants’ mean body mass index was 28.9 (SD = 6.46). Of the present sample 19.3% (n = 129) indicated high FoF, and 31.6% (n = 211) reported moderate FoF. Further, 27.1% (n = 181) had experienced a fall within the past year. Bivariate correlations found PMT constructs to correlate with each other (see Table 2). Coping appraisal, intention, and PA behavior significantly correlated with autonomous motivation to engage in PA. Perceived FoF was correlated with all PMT constructs, physical health, as well as past PA. As displayed in Table 3, women reported significantly higher scores for FoF. On the other hand, men scored higher on past PA engagement. Therefore, we controlled for gender (i.e., male and female) in the structural equation model (SEM model).
Bivariate Correlations of Variables Included in the Structural Equation Model (n = 659)
| Construct . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . |
|---|---|---|---|---|---|---|---|---|---|---|
| Health status (PCS) | — | |||||||||
| Gender | −0.05 | — | ||||||||
| Vulnerability | −0.28** | 0.18** | — | |||||||
| Severity | −0.22** | 0.26** | 0.24** | — | ||||||
| Self-efficacy | 0.32** | −0.04 | −0.23** | −0.18** | — | |||||
| Response efficacy | 0.19** | 0.03 | −0.23** | −0.08* | 0.38** | — | ||||
| Fear of falling | −0.44** | 0.12** | 0.49** | 0.32** | −0.32** | −0.24** | — | |||
| RAI | 0.17** | 0.06 | −0.18** | −0.10* | 0.33** | 0.41** | −0.23** | — | ||
| Intention | 0.34** | −0.01 | −0.20** | −0.11** | 0.55** | 0.56** | −0.30** | 0.49** | — | |
| PASE | 0.25** | −0.14** | −0.19** | −0.21** | 0.21** | 0.24** | −0.26* | 0.22** | 0.38** | — |
| Construct . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . |
|---|---|---|---|---|---|---|---|---|---|---|
| Health status (PCS) | — | |||||||||
| Gender | −0.05 | — | ||||||||
| Vulnerability | −0.28** | 0.18** | — | |||||||
| Severity | −0.22** | 0.26** | 0.24** | — | ||||||
| Self-efficacy | 0.32** | −0.04 | −0.23** | −0.18** | — | |||||
| Response efficacy | 0.19** | 0.03 | −0.23** | −0.08* | 0.38** | — | ||||
| Fear of falling | −0.44** | 0.12** | 0.49** | 0.32** | −0.32** | −0.24** | — | |||
| RAI | 0.17** | 0.06 | −0.18** | −0.10* | 0.33** | 0.41** | −0.23** | — | ||
| Intention | 0.34** | −0.01 | −0.20** | −0.11** | 0.55** | 0.56** | −0.30** | 0.49** | — | |
| PASE | 0.25** | −0.14** | −0.19** | −0.21** | 0.21** | 0.24** | −0.26* | 0.22** | 0.38** | — |
Notes: PASE = Physical Activity Scale for the Elderly (physical activity behavior); PCS = Physical Component Summary score (health status); RAI = Relative Autonomy Index (autonomous motivation). Eight individuals were excluded from the present analyses as they did not indicate their gender (n = 4) or identified as outside of the binary gender options (n = 4), which did not allow for the predetermined statistical comparison of mean scores with those of men and women.
*p < .05. **p < .01.
Bivariate Correlations of Variables Included in the Structural Equation Model (n = 659)
| Construct . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . |
|---|---|---|---|---|---|---|---|---|---|---|
| Health status (PCS) | — | |||||||||
| Gender | −0.05 | — | ||||||||
| Vulnerability | −0.28** | 0.18** | — | |||||||
| Severity | −0.22** | 0.26** | 0.24** | — | ||||||
| Self-efficacy | 0.32** | −0.04 | −0.23** | −0.18** | — | |||||
| Response efficacy | 0.19** | 0.03 | −0.23** | −0.08* | 0.38** | — | ||||
| Fear of falling | −0.44** | 0.12** | 0.49** | 0.32** | −0.32** | −0.24** | — | |||
| RAI | 0.17** | 0.06 | −0.18** | −0.10* | 0.33** | 0.41** | −0.23** | — | ||
| Intention | 0.34** | −0.01 | −0.20** | −0.11** | 0.55** | 0.56** | −0.30** | 0.49** | — | |
| PASE | 0.25** | −0.14** | −0.19** | −0.21** | 0.21** | 0.24** | −0.26* | 0.22** | 0.38** | — |
| Construct . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . |
|---|---|---|---|---|---|---|---|---|---|---|
| Health status (PCS) | — | |||||||||
| Gender | −0.05 | — | ||||||||
| Vulnerability | −0.28** | 0.18** | — | |||||||
| Severity | −0.22** | 0.26** | 0.24** | — | ||||||
| Self-efficacy | 0.32** | −0.04 | −0.23** | −0.18** | — | |||||
| Response efficacy | 0.19** | 0.03 | −0.23** | −0.08* | 0.38** | — | ||||
| Fear of falling | −0.44** | 0.12** | 0.49** | 0.32** | −0.32** | −0.24** | — | |||
| RAI | 0.17** | 0.06 | −0.18** | −0.10* | 0.33** | 0.41** | −0.23** | — | ||
| Intention | 0.34** | −0.01 | −0.20** | −0.11** | 0.55** | 0.56** | −0.30** | 0.49** | — | |
| PASE | 0.25** | −0.14** | −0.19** | −0.21** | 0.21** | 0.24** | −0.26* | 0.22** | 0.38** | — |
Notes: PASE = Physical Activity Scale for the Elderly (physical activity behavior); PCS = Physical Component Summary score (health status); RAI = Relative Autonomy Index (autonomous motivation). Eight individuals were excluded from the present analyses as they did not indicate their gender (n = 4) or identified as outside of the binary gender options (n = 4), which did not allow for the predetermined statistical comparison of mean scores with those of men and women.
*p < .05. **p < .01.
Gender Differences in Means and Standard Deviations of Variables Included in the Structural Equation Model (n = 659)
| . | . | Men (n = 281) . | Women (n = 378) . | . | ||
|---|---|---|---|---|---|---|
| Variable . | Min. to max. . | M . | SD . | M . | SD . | t . |
| Health status (PCS) | 26.73 to 62.05 | 39.82 | 7.92 | 40.26 | 8.02 | −0.66 |
| Physical activity | 0.00 to 510.76 | 139.40 | 76.21 | 117.89 | 71.36 | 3.72** |
| Fear of falling | 7 to 28 | 9.80 | 4.31 | 10.97 | 4.80 | −3.27* |
| Severity | 1 to 5 | 3.76 | 1.09 | 4.34 | .97 | −7.09** |
| Vulnerability | 1 to 5 | 2.25 | 1.14 | 2.70 | 1.19 | −4.87** |
| Self-efficacy | 0 to 90 | 51.09 | 24.56 | 48.96 | 24.31 | 1.11 |
| Response efficacy | 4 to 20 | 16.51 | 3.23 | 16.67 | 3.34 | −0.62 |
| Autonomous motivation (RAI) | −4.25 to 18.00 | 5.56 | 4.48 | 6.07 | 4.38 | −1.46 |
| Intention | 3 to 21 | 15.23 | 5.42 | 15.26 | 5.34 | −0.08 |
| . | . | Men (n = 281) . | Women (n = 378) . | . | ||
|---|---|---|---|---|---|---|
| Variable . | Min. to max. . | M . | SD . | M . | SD . | t . |
| Health status (PCS) | 26.73 to 62.05 | 39.82 | 7.92 | 40.26 | 8.02 | −0.66 |
| Physical activity | 0.00 to 510.76 | 139.40 | 76.21 | 117.89 | 71.36 | 3.72** |
| Fear of falling | 7 to 28 | 9.80 | 4.31 | 10.97 | 4.80 | −3.27* |
| Severity | 1 to 5 | 3.76 | 1.09 | 4.34 | .97 | −7.09** |
| Vulnerability | 1 to 5 | 2.25 | 1.14 | 2.70 | 1.19 | −4.87** |
| Self-efficacy | 0 to 90 | 51.09 | 24.56 | 48.96 | 24.31 | 1.11 |
| Response efficacy | 4 to 20 | 16.51 | 3.23 | 16.67 | 3.34 | −0.62 |
| Autonomous motivation (RAI) | −4.25 to 18.00 | 5.56 | 4.48 | 6.07 | 4.38 | −1.46 |
| Intention | 3 to 21 | 15.23 | 5.42 | 15.26 | 5.34 | −0.08 |
Notes: PCS = Physical Component Summary score; RAI = Relative Autonomy Index (autonomous motivation); SD = standard deviation. Means for the groups of men and women correspond to the sum scores for the respective constructs; eight individuals were excluded from the present analyses as they did not indicate their gender (n = 4) or identified as outside of the binary gender options (n = 4), which did not allow for the predetermined statistical comparison of mean scores with those of men and women.
*p < .01. **p < .001.
Gender Differences in Means and Standard Deviations of Variables Included in the Structural Equation Model (n = 659)
| . | . | Men (n = 281) . | Women (n = 378) . | . | ||
|---|---|---|---|---|---|---|
| Variable . | Min. to max. . | M . | SD . | M . | SD . | t . |
| Health status (PCS) | 26.73 to 62.05 | 39.82 | 7.92 | 40.26 | 8.02 | −0.66 |
| Physical activity | 0.00 to 510.76 | 139.40 | 76.21 | 117.89 | 71.36 | 3.72** |
| Fear of falling | 7 to 28 | 9.80 | 4.31 | 10.97 | 4.80 | −3.27* |
| Severity | 1 to 5 | 3.76 | 1.09 | 4.34 | .97 | −7.09** |
| Vulnerability | 1 to 5 | 2.25 | 1.14 | 2.70 | 1.19 | −4.87** |
| Self-efficacy | 0 to 90 | 51.09 | 24.56 | 48.96 | 24.31 | 1.11 |
| Response efficacy | 4 to 20 | 16.51 | 3.23 | 16.67 | 3.34 | −0.62 |
| Autonomous motivation (RAI) | −4.25 to 18.00 | 5.56 | 4.48 | 6.07 | 4.38 | −1.46 |
| Intention | 3 to 21 | 15.23 | 5.42 | 15.26 | 5.34 | −0.08 |
| . | . | Men (n = 281) . | Women (n = 378) . | . | ||
|---|---|---|---|---|---|---|
| Variable . | Min. to max. . | M . | SD . | M . | SD . | t . |
| Health status (PCS) | 26.73 to 62.05 | 39.82 | 7.92 | 40.26 | 8.02 | −0.66 |
| Physical activity | 0.00 to 510.76 | 139.40 | 76.21 | 117.89 | 71.36 | 3.72** |
| Fear of falling | 7 to 28 | 9.80 | 4.31 | 10.97 | 4.80 | −3.27* |
| Severity | 1 to 5 | 3.76 | 1.09 | 4.34 | .97 | −7.09** |
| Vulnerability | 1 to 5 | 2.25 | 1.14 | 2.70 | 1.19 | −4.87** |
| Self-efficacy | 0 to 90 | 51.09 | 24.56 | 48.96 | 24.31 | 1.11 |
| Response efficacy | 4 to 20 | 16.51 | 3.23 | 16.67 | 3.34 | −0.62 |
| Autonomous motivation (RAI) | −4.25 to 18.00 | 5.56 | 4.48 | 6.07 | 4.38 | −1.46 |
| Intention | 3 to 21 | 15.23 | 5.42 | 15.26 | 5.34 | −0.08 |
Notes: PCS = Physical Component Summary score; RAI = Relative Autonomy Index (autonomous motivation); SD = standard deviation. Means for the groups of men and women correspond to the sum scores for the respective constructs; eight individuals were excluded from the present analyses as they did not indicate their gender (n = 4) or identified as outside of the binary gender options (n = 4), which did not allow for the predetermined statistical comparison of mean scores with those of men and women.
*p < .01. **p < .001.
Model Effects
All items for each latent variable demonstrated reliable factor loadings with the exception of self-efficacy, where the first item (“being bothered by the weather”) was removed to improve latent stability. Model fit greatly improved by not connecting coping appraisal components with FoF. Thus, these pathways were omitted in the final model. The model produced adequate fit (χ 2 = 1,295.726, df = 327, p < .001, RMSEA = 0.067, 90% CI [0.063, 0.071], CFI = 0.927, TLI = 0.916). The model is illustrated in Figure 2 and corresponding factor loadings of the included constructs can be found in Supplementary Table 1.

Structural equation model predicting older adults’ (n = 659) intention to engage in physical activity (PA) using Protection Motivation Theory constructs and the added variables of gender, health status, past behavior, fear of falling, and autonomous motivation. Notes: Only significant paths are shown. *p < .05, **p < .001.
Prediction of Intention Using the PMT
Predictors of intention
In line with H1b, response efficacy (β = 0.36, p < .001) and self-efficacy (β = 0.30, p < .001) predicted intention. However, vulnerability (β = 0.04, p = .192) and severity (β = 0.05, p = .087) were not directly associated with intention (H1a). Corresponding to H2b, autonomous motivation predicted intention (β = 0.21, p < .001). In line with H3a, physical health was indirectly associated with intention (β = 0.11, p < .001, CI −0.088 to 0.26). Past behavior predicted intention directly (β = 0.17, p < .001) and indirectly through cognitive constructs (β = 0.23, p = .006, 95% CI 0.19 to 0.27). Gender did not indirectly predict intention (β = 0.006, p = .468, 95% CI −0.047 to 0.054).
Coping appraisal pathways
Predictors of autonomous motivation
The model supported H2d as both response efficacy and self-efficacy directly predicted autonomous motivation with coefficients of β = 0.37 (p < .001) and β = 0.16 (p < .001), respectively. Health status (β = 0.10, p = .021, 95% CI 0.063 to 0.13) and past behavior (β = 0.14, p = .007, 95% CI 0.11 to 0.18) were found to predict autonomous motivation when accounting for indirect effects (H3a). Gender (β = −0.004, p = .873, 95% CI −0.039 to 0.032) did not predict autonomous motivation.
Predictors of coping appraisal
In line with H3a, response efficacy was predicted by physical health (β = 0.16, p < .001) and past PA (β = 0.23, p < .001). Better physical health (β = 0.28, p < .001) and past PA (β = 0.13, p = .002) predicted increased self-efficacy. Gender only predicted response efficacy (β = 0.079, p = .044) but not self-efficacy (β = 0.003, p = .946).
Threat appraisal pathways
Predictors of intention
Contrary to H2a, perceived FoF did not directly predict PA intention (β = −0.019, p = .539).
Predictors of FoF
As hypothesized (H2c), perceived vulnerability (β = 0.43, p < .001) and perceived severity predicted FoF (β = 0.20, p < .001). Analyses for indirect effects found that physical health (β = −0.14, p = .014, 95% CI −0.19 to −0.11), past behavior (β = −0.11, p = .012, 95% CI −0.14 to −0.07), and gender were associated with FoF (β = 0.15, p = .019, 95% CI 0.11 to 0.19), adding support to H3b.
Predictors of threat appraisal
Physical health status predicted both perceived vulnerability (β = −0.25, p < .001) and perceived severity (β = −0.18, p < .001). Female gender predicted both higher perceived vulnerability (β = 0.16, p < .001) and perceived severity (β = 0.24, p < .001). Lastly, past PA behavior predicted both vulnerability (β = −0.10, p = .008) and severity (β = −0.13, p < .001).
Discussion
The purpose of this study was to examine the relationship between FoF and older adults’ intention to be or remain physically active. We embedded FoF as a construct within a modified PMT framework including further key determinants of PA intentions (e.g., autonomous motivation, health status, past behavior). The model presented adequate fit with the data as indicated by the corresponding goodness-of-fit indices. Results indicated two main findings: First, as one would expect, coping appraisal components of PMT (i.e., self-efficacy and response efficacy) positively affected PA intention (H1), independently of the autonomous motivation to engage in PA. Previous studies demonstrated the importance of self-efficacy and response efficacy regarding health behaviors (Floyd et al., 2000; Milne et al., 2000). Through both, more trust in one’s abilities to avert health threats such as falling, and frequent PA being the key to that, PA may be perceived as more beneficial to maintaining one’s health. This process in turn may affect autonomous motivation and shape the future intention to remain or get active.
Second, we also expected that a higher perception of falling as a threat would lower an individual’s intention to engage in PA. However, neither threat appraisal nor FoF was directly associated with the intention to be physically active when embedded in the final model. Although this finding may suggest a stronger impact of the benefits rather than the perceived barriers on older adults’ intention to engage in PA as a preventative health behavior, past research indicated FoF to be a significant barrier to PA (e.g., Kendrick et al., 2012) and be related to activity avoidance (Bertera & Bertera, 2008). A potential reason for this discrepancy may be the effect of having included past behavior in the prediction of intention: Meta-analytic findings indicate previous behavior to be a significant predictor of future intention and behavior (McEachan et al., 2011). Our results suggest that older adults’ perceived FoF may not be of great importance for the formation of PA intentions compared with the effects of frequent engagement in PA and having subsequently fostered coping appraisal and autonomous motivation. Findings from this study show that older adults with more engagement in PA and better physical health perceived themselves as less vulnerable to the threat of falling, which in turn accounted for a lower perceived FoF. Those participants also showed increased self-efficacy and response efficacy regarding PA being a measure to remain fit and prevent future falls. More response efficacy also accounted for increased autonomous motivation regarding future PA behavior, resulting in a greater intention to engage in PA.
As past behavior significantly predicted all PMT components as well as intention via the included cognitive constructs, it may be that older adults with better physical health and more PA engagement deal differently with FoF and corresponding preventative behavior than those with greater health problems. This might be due to a difference in their perception of FoF as a threat to their health, in addition to the enhanced coping appraisal. Conversely, the greater perceived vulnerability and lower efficacy appraisals of respondents with lower physical health and less engagement in PA correspond to previous research, suggesting that risk awareness may not directly influence the intention to engage in preventive behaviors (Gustavsson et al., 2018). This finding might also point in the direction of those individuals potentially not knowing how to take recommended actions regarding their physical health, to ultimately lower the perceived threat that falling poses in their lives; an aspect, which has been suggested by stage models.
Strengths and Limitations
The adaptation of PMT in the current model should be interpreted considering present limitations. Regarding the questionnaire constructs, neither the PMT variable of response costs nor maladaptive response rewards was assessed, which may have helped to gain more insight into the range of perceived benefits and costs associated with participants’ health status and PA behavior. Similarly, no objective measure of PA (e.g., accelerometry) was employed to verify the self-reported PA engagement, making it subject to potential reporting biases. Regarding the method of data collection, current findings are limited to the population of predominantly Caucasian, educated, and cognitively healthier seniors (as implied through the computer literacy required to answer the survey) with relatively low mean FoF (see Table 3). This may have affected the finding that FoF was not directly linked to PA intention. Therefore, we recommend that future research explores FoF among other cognitive determinants of PA and intention in different older adult subpopulations, and also by means of direct community recruitment methods. Lastly, the cross-sectional design of the study does not allow for prospective conclusion about the observed relationships and for predicting future PA.
Nonetheless, this study has notable strengths. To date there is limited evidence about the use of PMT to explain the relationship between FoF and psychological predictors of PA engagement, especially when embedded in more elaborate predictive models with key determinants such as motivation, intention, and behavior. To our knowledge, this investigation is the first to study the interrelation of these predictive factors and participant characteristics within the PMT using suitable, reliable measures. The expanded predictive model provides detailed insight into the effects of physical health, past behavior, and gender on older adults’ intention via autonomous motivation and fall-related PMT constructs. The presented regression coefficients and correlations are resourceful for researchers conducting meta-analyses.
Implications and Further Research
In sum, although our results support previous findings regarding the predictive effects of threat appraisal cognitions on fear in older adults (Ruthig, 2016), we found coping appraisal cognitions to be more important for older adults’ intention to continue to engage in PA than their FoF itself. Our results suggest that individuals may not need to be excluded from or treated significantly differently solely based on their FoF in randomized controlled trials that focus on increasing older adults’ intention to engage in PA.
Nonetheless, our results show that individuals’ perceptions of their vulnerability to and perceived severity of falling must be taken into consideration when tailoring interventions to the individual to address fear; especially among women and those with currently low engagement in PA and a worse physical health status. To increase the intention to remain active in older adulthood via coping and threat appraisal mechanisms, health professionals should consider applying motivationally adaptive strategies (see Hancox et al., 2018) that encourage meaningful discourse about individuals’ needs, preferences, goals, and their perceived concerns. This allows for both tailored feedback and activity recommendations that are safe, achievable, and enjoyable for individuals. Further, it may be worthwhile to focus on positive goals (e.g., remaining independent), instead of highlighting the negative health effects of inactivity (Marcus-Varwijk et al., 2016). These strategies in both individual and group settings may help to mitigate perceived barriers and foster self-efficacy and the perceived benefits of being active. In turn, this may assist older adults in navigating age-related physiological changes and promote physical, psychological, and social well-being. Though, more longitudinal investigations using appropriate theory-based strategies are needed to assess the impact of FoF as a significant barrier to PA later in the adult life span.
Funding
This study was supported by funds from James McGill Professorship awarded to B. Knäuper.
Conflict of Interest
None declared.
Acknowledgments
The present survey study was not preregistered.
Ethical Approval
Ethical approval was granted by the Research Ethics Board at McGill University (#350-0119).
Data Availability
The data supporting the findings of this study are openly available in Mendeley Data at http://dx.doi.org/10.17632/nvy6hpy5nk.1. Further information on study materials and methods can be obtained from the corresponding author upon reasonable request.



