-
PDF
- Split View
-
Views
-
Cite
Cite
Philippe F. Simard, Rachel M. Bolton, Nancy J. Tarbell, Anti-Inflammatory Cream Reduces Skin Damage Induced by Ionizing Radiation, The Oncologist, Volume 14, Issue 2, February 2009, Pages 197–198, https://doi.org/10.1634/theoncologist.2008-0256
Close - Share Icon Share
Abstract
The authors assessed whether the use of a topical anti-inflammatory agent at the radiation entry site would prevent radiation-induced skin damage and found that the use of a topical anti-inflammatory agent, such as one containing 10% trolamine salicylate, may reduce skin damage at the radiation entry site if used prophylactically.
The use of ionizing radiation to treat cancer often results in damage at the skin entry site, especially if the dose exceeds 30–40 Gy fractionated [1]. Ionizing radiation can cause erythema, skin discoloration, muscle soreness, death of hair follicles, tissue swelling, and skin breakdown [2]. Damage may be significant enough to interrupt treatment. Methods currently used to reduce radiation-induced entry site damage include the use of multiple entry sites, free radical scavengers, and creams containing metal oxides to block radiation.
Radiation-induced skin damage can be attributed to either a direct effect of ionizing radiation causing DNA damage or an indirect effect resulting from inflammation-induced secondary injury [3]. Inflammation can be prevented using anti-inflammatory agents [4], but systemic anti-inflammatory agents are generally contraindicated when receiving chemotherapy.
We assessed the hypothesis that the use of a topical anti-inflammatory agent at the radiation entry site would prevent skin damage. A patient undergoing fractionated proton therapy (54 Gy total) plus concurrent chemotherapy (vincristine, doxorubicin, cyclophosphamide, ifosfamide, and etoposide) for mesenchymal chondrosarcoma of the temporal bone received twice-daily application of an anti-inflammatory cream containing 10% trolamine salicylate (Aspercreme®; Chattem, Inc., Chattanooga, Tennessee; over-the-counter; off-label use). Aspercreme® treatment was started 1 week after beginning radiation, and initially involved treating only a limited area with erythema and discomfort. Three weeks after beginning radiation, when a new area of erythema and discomfort emerged, Aspercreme® was applied to the entire radiation entry site. Shortly after initiating treatment in any particular area, erythema and discomfort in the corresponding area were markedly reduced. At its worst, the skin reaction induced by radiation was limited to a region of mild-to-moderate erythema and swelling, and an ∼4 mm fissure at the ear–scalp junction (grade 3–4, see Liang et al. [4]) (Fig.). Overall, the skin damage was noticeably less than expected, radiation treatment never had to be interrupted, and the scalp healed fully (Fig.).
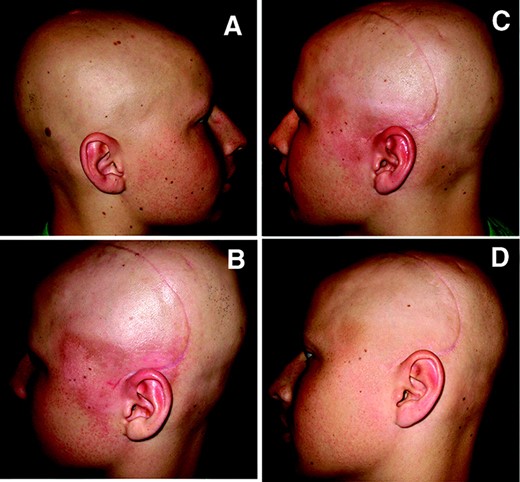
Radiation-induced skin changes. Images of nonirradiated side of head (A) and irradiated side of head (B–D). (B) and (C) were taken 31 and 40 days, respectively, after the start of radiation. (D) was taken 1 month after the end of radiation. (B) represents the worst of the radiation-induced skin changes.
Since this case, prophylactic treatment with Aspercreme® has been used in other pediatric patients receiving proton therapy, and comparably favorable results have been observed.
In summary, we suggest that the use of a topical anti-inflammatory agent, such as Aspercreme®, may reduce skin damage at the radiation entry site if used prophylactically.
References
Author notes
Disclosure: Philippe F. Simard: None; Rachel M. Bolton: None; Nancy J. Tarbell: None
The content of this article has been reviewed by independent peer reviewers to ensure that it is balanced, objective, and free from commercial bias. No financial relationships relevant to the content of this article have been disclosed by the authors, planners, independent peer reviewers, or staff managers.



