-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmed Abdalazim Dafallah Albashir, A case of Falciparum malaria presenting with features of functional bowel obstruction, Oxford Medical Case Reports, Volume 2020, Issue 10, October 2020, omaa098, https://doi.org/10.1093/omcr/omaa098
Close - Share Icon Share
Abstract
Malaria is the most common tropical disease in Sudan, which is caused by an infection with Plasmodium protozoa transmitted by an infective female Anopheles mosquito. Headache, fever, cough, fatigue, malaise, shaking chills, arthralgia and myalgia are the cardinal features of malaria, but occasionally, it has an atypical presentation. Intestinal obstruction as a complication is an extremely rare presentation. Here within, we describe a 28-year-old Sudanese man who has presented with of colicky abdominal pain, absolute constipation for two days and fever. Blood film for malaria was positive for Plasmodium falciparum. Intravenous artesunate injections have resulted in the resolution of symptoms of bowel obstruction. In conclusion, malaria should be suspected in any febrile patient with the features of bowel obstruction especially in an endemic area or if the patient has recently travelled to an endemic area with malaria. Treatment of malaria will result in the resolution of symptoms of functional bowel obstruction.
INTRODUCTION
Malaria is a fatal tropic disease that is considered one of the principal causes of death in many developing countries. The clinical presentation of malaria is variable with only 50–70% of patients presenting with classic paroxysms of fever [1]. The principal symptoms of malaria include fever, rigours, headache, sweats, anorexia, nausea and vomiting [1]. Gastrointestinal complications due to malaria including tropical splenomegaly syndrome, gastrointestinal bleeding, splenic rupture and sub-acute intestinal obstruction have been recorded among children with complicated malaria [2]. Functional bowel obstruction due to malaria has been reported very rarely in medical literature (Table 1). One was reported by the food drug administration in 2003 [3]. It was also reported in a 42-year-old black African man [1] and an 18-month-old Indian girl [4]. Intestinal obstruction secondary to mechanical compression caused by an enlarged spleen due to malaria has also been reported [5].
| . | Age . | Sex . | Symptoms . | Physical examination . | Investigation . | Imaging . | Diagnosis . | Anti-malarial drug . | Response . | Reference number . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | One and half year | Female | fever, vomiting and abdominal distension | Hepatomegaly | ICT | AXR and Abd US: were normal | Functional bowel obstruction due to malaria | - | - | 4 |
| 2 | 42 years | Male | Fever, abdominal pain colicky in character, progressive abdominal distension, inability to pass stool and flatus over 4 days, no vomiting. | Mildly distended abdomen with mild diffuse tenderness. Tympanic abdomen with exaggerated bowel sounds. | ICT | AXR: Increased bowel gas. Abd US: Mild free intra-abdominal fluid in all four quadrants. | Functional bowel obstruction due to malaria | I.V. Quinine infusion | Faeces passed 48 hours after initiation of Quinine. Complete resolution of abdominal pain, distension on the fourth day. | 1 |
| 3 | 32 years | Male | constipation and abdominal pain | Spleen was palpable 3 finger breadth below the coastal margin | - | - | Mechanical bowel obstruction caused by massive splenomegaly due to malaria | Atebrin and plasmoquine, followed by quinine. | - | 5 |
| 4 | 42 years | Male, American | - | - | - | - | Functional bowel obstruction due to malaria | - | - | 1 |
| 5 | 28 years | Male | Abdominal pain, inability to pass stool and flatus. Intermittent fever for 4 days, myalgia and back pain and sometimes vomiting. | The abdomen was moderately distended with mild tenderness. Percussion note: tympanic Auscultation: exaggerated bowel sounds. | Blood film for malaria | AXR: Distended bowel with gas with no significant air-fluid levels. Abd US: Loops of distended bowel with mild free intra-abdominal fluid in all four quadrants. | Functional bowel obstruction due to malaria | I.V. artesunate | He passed flatus about 36 hours after starting the I.V. artesunate and he passed faeces after 48 hours with the resolution of the abdominal pain and distension. |
| . | Age . | Sex . | Symptoms . | Physical examination . | Investigation . | Imaging . | Diagnosis . | Anti-malarial drug . | Response . | Reference number . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | One and half year | Female | fever, vomiting and abdominal distension | Hepatomegaly | ICT | AXR and Abd US: were normal | Functional bowel obstruction due to malaria | - | - | 4 |
| 2 | 42 years | Male | Fever, abdominal pain colicky in character, progressive abdominal distension, inability to pass stool and flatus over 4 days, no vomiting. | Mildly distended abdomen with mild diffuse tenderness. Tympanic abdomen with exaggerated bowel sounds. | ICT | AXR: Increased bowel gas. Abd US: Mild free intra-abdominal fluid in all four quadrants. | Functional bowel obstruction due to malaria | I.V. Quinine infusion | Faeces passed 48 hours after initiation of Quinine. Complete resolution of abdominal pain, distension on the fourth day. | 1 |
| 3 | 32 years | Male | constipation and abdominal pain | Spleen was palpable 3 finger breadth below the coastal margin | - | - | Mechanical bowel obstruction caused by massive splenomegaly due to malaria | Atebrin and plasmoquine, followed by quinine. | - | 5 |
| 4 | 42 years | Male, American | - | - | - | - | Functional bowel obstruction due to malaria | - | - | 1 |
| 5 | 28 years | Male | Abdominal pain, inability to pass stool and flatus. Intermittent fever for 4 days, myalgia and back pain and sometimes vomiting. | The abdomen was moderately distended with mild tenderness. Percussion note: tympanic Auscultation: exaggerated bowel sounds. | Blood film for malaria | AXR: Distended bowel with gas with no significant air-fluid levels. Abd US: Loops of distended bowel with mild free intra-abdominal fluid in all four quadrants. | Functional bowel obstruction due to malaria | I.V. artesunate | He passed flatus about 36 hours after starting the I.V. artesunate and he passed faeces after 48 hours with the resolution of the abdominal pain and distension. |
ICT, Immunochromatographic test; AXR, Abdominal X-ray; Abd US, Abdominal Ultrasonography; I.V, Intravenous.
| . | Age . | Sex . | Symptoms . | Physical examination . | Investigation . | Imaging . | Diagnosis . | Anti-malarial drug . | Response . | Reference number . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | One and half year | Female | fever, vomiting and abdominal distension | Hepatomegaly | ICT | AXR and Abd US: were normal | Functional bowel obstruction due to malaria | - | - | 4 |
| 2 | 42 years | Male | Fever, abdominal pain colicky in character, progressive abdominal distension, inability to pass stool and flatus over 4 days, no vomiting. | Mildly distended abdomen with mild diffuse tenderness. Tympanic abdomen with exaggerated bowel sounds. | ICT | AXR: Increased bowel gas. Abd US: Mild free intra-abdominal fluid in all four quadrants. | Functional bowel obstruction due to malaria | I.V. Quinine infusion | Faeces passed 48 hours after initiation of Quinine. Complete resolution of abdominal pain, distension on the fourth day. | 1 |
| 3 | 32 years | Male | constipation and abdominal pain | Spleen was palpable 3 finger breadth below the coastal margin | - | - | Mechanical bowel obstruction caused by massive splenomegaly due to malaria | Atebrin and plasmoquine, followed by quinine. | - | 5 |
| 4 | 42 years | Male, American | - | - | - | - | Functional bowel obstruction due to malaria | - | - | 1 |
| 5 | 28 years | Male | Abdominal pain, inability to pass stool and flatus. Intermittent fever for 4 days, myalgia and back pain and sometimes vomiting. | The abdomen was moderately distended with mild tenderness. Percussion note: tympanic Auscultation: exaggerated bowel sounds. | Blood film for malaria | AXR: Distended bowel with gas with no significant air-fluid levels. Abd US: Loops of distended bowel with mild free intra-abdominal fluid in all four quadrants. | Functional bowel obstruction due to malaria | I.V. artesunate | He passed flatus about 36 hours after starting the I.V. artesunate and he passed faeces after 48 hours with the resolution of the abdominal pain and distension. |
| . | Age . | Sex . | Symptoms . | Physical examination . | Investigation . | Imaging . | Diagnosis . | Anti-malarial drug . | Response . | Reference number . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | One and half year | Female | fever, vomiting and abdominal distension | Hepatomegaly | ICT | AXR and Abd US: were normal | Functional bowel obstruction due to malaria | - | - | 4 |
| 2 | 42 years | Male | Fever, abdominal pain colicky in character, progressive abdominal distension, inability to pass stool and flatus over 4 days, no vomiting. | Mildly distended abdomen with mild diffuse tenderness. Tympanic abdomen with exaggerated bowel sounds. | ICT | AXR: Increased bowel gas. Abd US: Mild free intra-abdominal fluid in all four quadrants. | Functional bowel obstruction due to malaria | I.V. Quinine infusion | Faeces passed 48 hours after initiation of Quinine. Complete resolution of abdominal pain, distension on the fourth day. | 1 |
| 3 | 32 years | Male | constipation and abdominal pain | Spleen was palpable 3 finger breadth below the coastal margin | - | - | Mechanical bowel obstruction caused by massive splenomegaly due to malaria | Atebrin and plasmoquine, followed by quinine. | - | 5 |
| 4 | 42 years | Male, American | - | - | - | - | Functional bowel obstruction due to malaria | - | - | 1 |
| 5 | 28 years | Male | Abdominal pain, inability to pass stool and flatus. Intermittent fever for 4 days, myalgia and back pain and sometimes vomiting. | The abdomen was moderately distended with mild tenderness. Percussion note: tympanic Auscultation: exaggerated bowel sounds. | Blood film for malaria | AXR: Distended bowel with gas with no significant air-fluid levels. Abd US: Loops of distended bowel with mild free intra-abdominal fluid in all four quadrants. | Functional bowel obstruction due to malaria | I.V. artesunate | He passed flatus about 36 hours after starting the I.V. artesunate and he passed faeces after 48 hours with the resolution of the abdominal pain and distension. |
ICT, Immunochromatographic test; AXR, Abdominal X-ray; Abd US, Abdominal Ultrasonography; I.V, Intravenous.
CASE REPORT
A 28-year-old Sudanese man, with no relevant past medical history, presented to a university hospital, Sudan with a 3-day history of abdominal pain and inability to pass stool and flatus. The pain was colicky in nature and has a severity of 6/10 on a visual analogue scale. On inquiry, the patient documented intermittent fever for 4 days for which he had taken paracetamol tablets (500 mg tab/8 hourly). The fever had irregular spikes without a noticeable rhythm. Besides, he has reported mild myalgia and back pain and sometimes vomiting. The patient has no history of major surgery and not admitted in the previous months to any hospital.
On examination, pulse 76 bpm, blood pressure 130/80 mmHg and temp 36.8°C. His abdomen was moderately distended with mild diffuse tenderness with exaggerated bowel sounds. Neither guarding nor rebound tenderness has been documented with tympanic percussion note. Digital rectal examination revealed empty rectum. The rest of the physical examination was unremarkable.
Blood film for malaria was positive for Plasmodium falciparum (Fig. 1). Complete blood counts revealed a hemoglobin of 13.7 g/dL (11–17 g/dL), white blood cells count of 8400 cells/uL (4.0–11.0 cells/uL) and platelet count of 240 000 cells/uL (150–450 cells/uL). Random blood glucose was normal. Renal function tests were normal with a blood Urea of 42 mg/dL (15–45 mg/dL) and serum creatinine of 1.1 mg/dL (0.6–1.3 mg/dL). Important serum electrolytes were within normal range: sodium (Na+) was 138 mEql/L (135–145 mEql/L), potassium (K+) was 4.2 mEql/L (3.5–5.5 mEql/L), calcium was 10 mg/dl (8.6–10.3 mg/dl) and chloride (Cl−) was 103 mEql/L (96–109 mEql/L). Vidal test for typhoid fever and rapid antibody test was normal. ICT for Hepatitis B, Hepatitis C and HIV was negative. Abdominal X-ray showed distended bowel with gas with no significant air–fluid levels. Abdominal ultrasound revealed loops of distended bowel with mild free intra-abdominal fluid in all four quadrants.
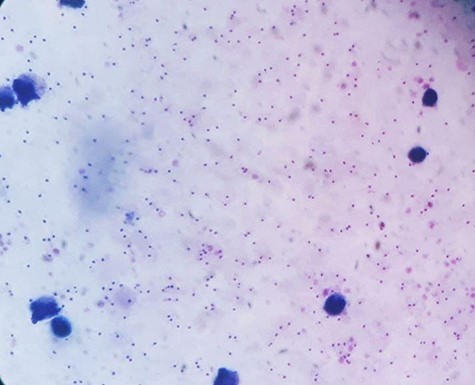
Blood film took on the first day showing a very high density of P. falciparum malaria.
The patients were diagnosed with functional bowel obstruction secondary to malaria. The patient was admitted and received nothing per mouth and nasogastric tube for suction of air. He received intravenous Artesunate according to the world health organization (WHO) prescription (2.4 mg/kg at 0, 12 hours, 24 hours then qday). The I.V. artesunate was continued for a total of 3 days from the first dose. The patient administered I.V. fluids in terms of 0.9% normal saline at a rate of 1 litre/8 hourly for 48 hours. He passed flatus about 36 hours after starting the intravenous artesunate and he passed faeces around 48 hours with the resolution of the abdominal pain and distension. A stool examination was performed with no organisms identified. On the fourth day of hospitalization, auscultation showed normal bowel sounds and the patient discharged in good condition on oral artesunate tablets. A blood film has been taken to ensure the clearance of parasites (Fig. 2). The follow-up 1 week later was unremarkable.
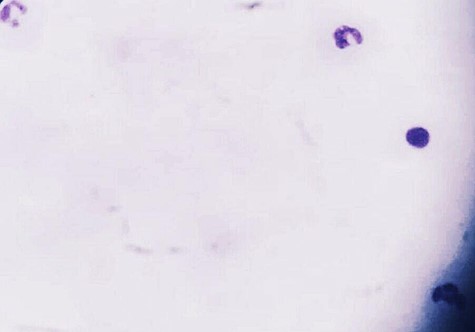
Blood film took before discharging the patient to ensure the parasitological clearance of malaria.
DISCUSSION
The major complications of falciparum malaria include cerebral malaria, severe anaemia, jaundice, circulatory collapse, pulmonary oedema, blackwater fever, lactic acidosis, acute kidney injury and hypoglycaemia [6]. Bowel obstruction due to malaria has been reported very rarely in the medical literature (Table 1). However, some cases may have been passed unnoticed. Vascular affection at the intestinal level that has resulted in intestinal ischemia without the clinical picture of bowel obstruction has also been reported [7].
The exact mechanism that results in functional bowel obstruction due to malaria remains obscured, but many theories have been postulated [8–10]. Infection of the red blood cells by P. falciparum results in sequestration of P. falciparum-infected erythrocytes (IRBC) in the microcirculation including the bowel, resulting in impairment of blood flow, hypoxia and bowel wall ischemia [7]. Sequestration results from the cytoadherence of IRBC to the vascular endothelial cells. This process is mediated by the variant parasite ligand P. falciparum erythrocyte membrane protein 1 (PfEMP1) and endothelial receptors, of which a number have been linked with severe malaria [8]. Besides, it has been reported that symptomatic P. falciparum infection was associated with a significant increase in von Willebrand factor (VWF) level and activity and a decrease in ADAMTS13 activity, resulting in the presence of circulating prothrombogenic unusually large VWF multimers in the plasma. The presence of reduced ADAMTS13 activity might be attributable to the microvascular disorders observed in severe malaria. In addition, it has been hypothesized that P. falciparum infection results in alterations in the erythrocyte membranes, resulting in stimulating the coagulation cascade and releasing of inflammatory cytokines, leading to thrombin formation [8]. Taken together, all of these may lead to prothrombotic state and bowel wall ischemia in this patient.
In the case of Divine Tim et al., the patient passed a small amount of faeces 48 hours after initiation of quinine base infusion, with complete resolution of the abdominal pain, distension and bowel movements on the fourth day of hospital stay [1]. In our case, the patient passed flatus about 36 hours after starting the intravenous artesunate and he passed faeces around 48 hours with the resolution of the abdominal pain and distension. However, in other reported cases of functional bowel obstruction due to malaria, it was not mentioned when the bowel obstruction has resolved (Table 1).
In conclusion, malaria should be suspected in any febrile patient with the features of bowel obstruction especially in an endemic area or if the patient has recently come from an endemic area with malaria. Treatment of malaria will result in the resolution of symptoms of the functional bowel obstruction. Many theories have postulated to explain the mechanism of functional bowel obstruction in falciparum malaria.
ACKNOWLEDGEMENT
I sincerely express my deep gratitude to the Education Development and Research Center, University of Gezira, Sudan for supporting the article.
CONFLICT OF INTEREST STATEMENT
None.
FUNDING
None.
ETHICS APPROVAL
The article is accepted by the Research Ethics Committee, University of Gezira, Faculty of Medicine, Sudan.
CONSENT
A written consent for publication has been obtained from the patient.
GUARANTOR
The University of Gezira, Faculty of Medicine, Sudan.
ABBREVIATIONS
TSS: tropical splenomegaly syndrome
FDA: Food and Drug Administration
PfEMP1: Plasmodium falciparum erythrocyte membrane protein 1
ADAMTS13: a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13



